Back to Journals » Open Access Emergency Medicine » Volume 15
Paramedic To Provider Consultation Challenges in the Emergency Department in Kazakhstan: An Online Survey
Authors Ygiyeva D , Pivina L , Messova A, Urazalina Z, Semenova Y, Dyussupov A, Dyussupov A, Belikhina T, Syzdykbayev M, Batenova G , Akhmetova A, Adams A
Received 15 December 2022
Accepted for publication 28 February 2023
Published 9 March 2023 Volume 2023:15 Pages 69—77
DOI https://doi.org/10.2147/OAEM.S401331
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Diana Ygiyeva,1 Lyudmila Pivina,1 Assylzhan Messova,1 Zhanar Urazalina,1 Yuliya Semenova,1 Almas Dyussupov,1 Altay Dyussupov,1 Tatyana Belikhina,2 Marat Syzdykbayev,1 Gulnara Batenova,1 Ayaulym Akhmetova,1 Amber Adams3
1Department of Emergency Medicine, Semey Medical University, Semey, Abay Region, Kazakhstan; 2Nuclear Medicine Department, Center of Nuclear Medicine and Oncology, Semey, Abay Region, Kazakhstan; 3JoAnne Gay Dishman School of Nursing, Lamar University, Beaumont, TX, USA
Correspondence: Assylzhan Messova; Lyudmila Pivina, Department of Emergency Medicine, Semey Medical University, Abay str. 103, Semey, Abay Region, Kazakhstan, Tel +7 777 2138307 ; +77055227300, Email [email protected]; [email protected]
Objective: Consultation is an important and necessary aspect of patient care in the emergency department. We prospectively examined difficulties during the consultation process between paramedics and providers in emergency departments in Kazakhstan.
Methods: The paramedics were interviewed using various platforms and face-to-face meetings. Questionnaires were administered to paramedics to gather feedback on the current consultation process. In our survey, 202 paramedics of ambulance from the cities of Semey, Pavlodar, and Ust-Kamenogorsk, located in the North and East of Kazakhstan took part.
Results: Serious barriers to effective consultation were identified during consultations with cardiologists, pediatricians, and traumatologists. Weekends, as well as nighttime, are associated with more consultation difficulties. The most common problems for paramedics are non-attendance of the consultant, refusal of hospitalization by the consultant, and referral to other specialists and departments. More than 40% of the respondents noted the desire to share responsibility for the patient with medical consultants, which indicates uncertainty in their own knowledge due to the limited work experience of the majority of respondents.
Conclusion: Barriers that arise during the consultation process of patients with emergency conditions can lead to unfavorable outcomes. Strategies to address these barriers are needed to improve the quality of patient care. This review aims to understand and evaluate the issues that arise during the consultation process.
Keywords: emergency department, consultation, paramedics, prehospital medical care
Introduction
Paramedic provides emergency medical care in a variety of settings and ultimately determines the need for further treatment within the emergency department. Emergency departments are known to have the highest mortality rates due to the overload of doctors and nurses.1 Providers in the emergency department are often busy addressing issues and managing various clinical situations. Providers must make vital decisions quickly, which makes communication with the paramedic difficult. In the emergency department, it is often necessary to consult with doctors of different specialties to decide on the scope of diagnostic examination and treatment, and the need for hospitalization.20
Consultation is one of the most critical aspects of patient care in emergency medicine, as the patient needs an urgent examination with the optimal use of diagnostic tools and correct treatment.2 It is one of the most important stages in the provision of emergency medical care to the patient. Consultants are called, based on a preliminary diagnosis, and they decide on the issues of further patient management.3 The provider responsible for the patient determines the areas for the differential diagnosis of the disease, the number of specialists necessary for making a decision, consults with colleagues, takes into account their conclusions, and continues the observation and treatment of the patient. Even in transit, the paramedic may request the need for certain consultations to provide the patient with the necessary treatment interventions.4 The communication links between the consultant and the emergency medicine provider or paramedic determine the success of the consultative process and, accordingly, the quality and timeliness of medical care for the patient. Barriers arising during the consultation process can lead to an increase in the patient’s wait time, delayed treatment interventions, and a decrease in patient satisfaction.5
During the consultation, the provider must adhere to the following rules:
- Clearly define the specific problem in the patient’s health;
- Quickly determine the urgency/criticalness of the consultation by discussing this issue with the consultant (team of consultants) face to face or by telephone, to prevent negative consequences or delay the necessary treatment for patients with severe diseases;
- Independently collect the missing information, communicating with other specialists from other medical institutions, requesting medical documents and the results of visual diagnostics;
- Should be brief and make specific recommendations; must be kind and tactful when communicating with the patient, the emergency medicine doctor and the paramedics;
- Should make recommendations to the paramedic who has applied for consultation.6
In the process of consulting with a patient at the place of residency or in the emergency department, the paramedic may encounter some difficulties and problems. One major issue is overcrowding which leads to a deterioration in the quality of medical care, and an increase in the waiting time for consultations. It can cause delays in making decisions about the diagnosis and treatment of patients, treatment of seriously ill patients, increased costs, and decreased patient satisfaction.7
The purpose of this study is to identify and evaluate the barriers faced by paramedics during consultations in the emergency department.
Methods
Data Collection
The survey was conducted during April 2022 on the sample consisted of paramedics from Semey, Pavlodar, and Ust-Kamenogorsk cities, located in the North and East of Kazakhstan. Paramedics were interviewed anonymously after face-to-face meetings at emergency medical stations. After agreeing and approving the meeting with the emergency medical station managers, we explained to the paramedics the goals and main questions that arise during the survey and received informed consent for participating in our study. The paramedics then completed the survey on their own through the platform Google Forms. We have sent the link to the questionnaire via social media.
The design of the study is a cross-sectional, the sample is full population survey due to the small number of paramedics in the ambulance service in these regions. The study has approval of the Local Ethics Commission of the Semey Medical University on March 16, 2022 (Protocol #7). The study was conducted for the first time in Kazakhstan.
The questionnaire was created based on a survey developed and validated by Turkish researchers.8 It included nineteen questions:
- Three questions related to personal data (age, gender, work experience).
- Three questions about the difficulties associated with the temporary period of work (day of the week, time of day) and the most difficult medical specialties for paramedics in the process of consulting.
- The rest of the questions were related to communication between the paramedic and the patient (conflict with the patient or his relatives, communication difficulties associated with the patient’s gender); the communication between consultant and paramedic (difficulties in communication related to the gender of the consultant, errors in consultations, untimely or unreasonable refusal to consult, unreasonable consultations, conflict situations, use of modern means of communication for consultations, compliance with the recommendations of the consultant, overload of consultants); the communication between consultant and patient (adequate feedback with the patient), issues of management of the consultative process.
In our survey, 101 paramedics in ambulance stations in Semey city, 61 paramedics in Pavlodar city, and 40 paramedics in Ust-Kamenogorsk city took part. Demographic characteristics of the interviewed paramedics are presented in Table 1.
 |
Table 1 Demographic Characteristics of the Interviewed Paramedics |
Statistical Analysis
Was carried out using IBM SPSS Statistics 20 for Windows software. Descriptive statistics were conducted to summarize the demographic characteristics of the interviewed paramedics. For quantitative data, normality of distribution and mean values were checked. Differences in groups were assessed by constructing contingency tables, calculating Pearson’s chi-squared test.
Results
The specialties that presented the most difficulties during consultations for paramedics are shown in Figure 1. Cardiology was associated with the most difficulty (56.4%, n=114). Consultations with pediatricians and traumatologists were also associated with a high level of difficulty (13% and 7%, respectively). For other specialties, the answers were evenly distributed.
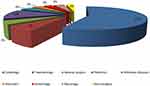 |
Figure 1 Specialties in which paramedics experienced difficulties during consultation. |
For male paramedics, difficulties in consulting with pediatricians occurred twice as often compared with women (16.7% and 8.5%, respectively, p=0.005). The majority of paramedics (53.5%, n=108) noted that it is more difficult to work on weekends. As for the time of day, for 52.5% (n=106) of paramedics the most difficulties occur at the time from 24:00 until 08:00, for 38.6% (n=78) at the time of 16:00–24:00, for 8.9% (n=18) at 08:00–16:00. To the question, “Which gender is more difficult to work with?” many paramedics (83.2%, n=168) responded that female consultants are more difficult to work with, and 16.8% (n=34) responded that it was male physicians. 75.2% (n =152) of participants reported that working with men and women is equally difficult; 5% (n=10) reported that male patients are more difficult to counsel; and 19.8% (n=40) reported that working with women is more difficult. In response to the question “In the process of consultations, what difficulties do you most often encounter?” 32.7% (n=66) answered “doctor consultant does not come for consultation”; 5% (n=10) answered that the consultant recommends additional, optional diagnostic methods; 23.8% (n=48) answered that the consultant suggested consulting in another department or hospital; 5% (n=10) answered that the consultant unreasonably referred the patient to another medical institution; 28.7% (n=58) said that the consultant does not hospitalize a patient who needs it; 5% (n=10) responded that they face the need to convince an emergency physician to consult a specialist. At the same time, a large number of participants (62.4%) answered that the consulting doctor complies with the consultation process rules established by the institution/hospital.
24.8% of paramedics noted that they never use technologies in the process of consulting with a doctor; 50.5% use them rarely; 13.9% use frequently; 10.9% always use these technologies (Figure 2).
 |
Figure 2 Analysis of answers about the use of communication tools (Whats App, Facebook, etc.). |
To the question, “Does the consultant doctor give adequate feedback to the patient or relatives during the consultation?” 15.8% of paramedics answered «never», 40.6% «rarely», 26.7% «often», 16.8 «always».
It was revealed that 58.4% of paramedics had no conflicts with consultant doctors; 40.6% had a verbal conflict with a consultant physician; and only 1% had a physical conflict with a consultant physician. Regarding conflicts with patients, the answers were distributed as follows: 59.4% (n=120) never had a conflict with a patient, 39.6% had a verbal conflict, and only 1% had a physical conflict with the patient.
When the reason for too many consultations in the emergency department was considered, the most common response was “the desire to share responsibility for the patient with the consulting physicians” (41.6%) (Table 2). However, 62.4% of the respondents had never been trained in counseling.
 |
Table 2 Possible Reasons of the High Number of Consultations in the Emergency Department |
To the question “Do you follow all the recommendations of the consultant doctor?” participants responded: 7.9% never followed the recommendations; 7.9% rarely follow the recommendations; 35.6% usually follow the recommendations; 48.5% always follow the recommendations. Paramedics were asked if there were situations when they had to go to a consultant doctor without indications: 76.2% answered “no”.
Answers to the question “Who solves the problems associated with consulting a patient in a hospital?” were distributed as follows: 12.9% answered “patients”, 18.8% answered “paramedic”, 31.7% answered ‘head of department’, 21.8% answered ‘hospital administration’. The results are shown in Table 3.
 |
Table 3 Difficulties in the Work of Paramedics |
For both male and female paramedics, they perceived more difficulty working with female physician consultants (p<0.05), but the gender variable did not affect the variable for the occurrence of conflict situations between the paramedic and the consultant (p=0.405) (Table 4). Female paramedics found it more difficult to work at night than male paramedics, but no statistical significance was found (p=0.059).
 |
Table 4 Analysis of the Relationship Between the Sex of Paramedics and Counseling Problems |
Statistical analysis showed that paramedics with less than 10 years of experience perceive more difficulty with female consultants than more experienced colleagues (p<0.05). Paramedics with more than 10 years of experience more often use communication tools to consult patients (p=0.033) and more often follow the recommendations of consultant doctors (p=0.037) (Table 5).
 |
Table 5 Analysis of the Relationship Between the Work Experience of Paramedics and Counseling Problems |
Discussion
We present the results of a survey of paramedics regarding the main difficulties they encounter in the process of counseling patients with emergency conditions. About half of the paramedics had work experience of up to five years, which indicates the lack of the necessary experience and, accordingly, the level of communication skills. This could lead to barriers in communication, both with patients and their relatives, and with consultants, as well as more frequent seeking advice due to lack of knowledge. Increased work experience helps develop stress resistance, acquire communication skills, and improve self-confidence. On the other hand, with increasing age and length of service, paramedics are exposed to an increasing number of stress factors.9 There is conflicting data in the literature regarding the dependence of stress resistance on the age and work experience of paramedics. Thus, young paramedics were less likely to show symptoms of mental disorders, which may be due to shorter exposure to stress factors, but the difference was statistically significant only between the age groups from 19 to 29 and from 40 to 49 years. Women were 1.54 times more likely to experience stress disorder than men.10 In a study of the perception and impact of critical stress among paramedics conducted in Canada, more than 75% had an experience of 10 years or more. The majority of employees were in the age range from 31 to 50 years. Psychiatric disorders (eg, alcohol abuse, generalized anxiety disorder, major depressive disorder, panic disorder, post-traumatic stress disorder, social anxiety disorder) are common among paramedics who encounter severe stressful situations, death of patients (especially children), regardless of gender, age and length of service.11
Internal diseases require more careful differential diagnosis; the counseling process here can cause significant difficulties, sometimes leading to conflict situations.12 It is known that conflicts with providers in the emergency care system can increase the number of medical errors, lead to poor patient outcomes, and dissatisfaction with doctors. Conflict situations are often associated with unprofessional and unethical behavior of medical staff. Thus, a study published in 2022 showed that among emergency physicians, the most common causes of unprofessional behavior were condescension (82.1%), dismissive attitude (60.7%) and rudeness (50.0%). Among internal medicine consultation doctors, the most frequently noted disregard for paramedics (50.0%) and unwillingness to help them (38.5%). The two behaviors that underlay occupational conflicts in the emergency department were condescension towards paramedics (p < 0.0001), and rudeness (p-value = 0.0041).13
As the main reason for the large number of consultations in the emergency department, more than 40% of the respondents noted the desire to share responsibility for the patient with medical consultants, which indicates uncertainty in their own knowledge due to the short work experience of the majority of respondents. These data are consistent with the results of a number of studies. Thus, there are three most significant problems in the process of consulting patients with emergency conditions: the patient was not adequately examined before the start of the consultation; his medical records lack the necessary information, and calling a consultant is unreasonable. At the same time, doctors in the emergency medicine department consider the consultant’s desire to complete the entire diagnostic process within the emergency medicine department, the reluctance to hospitalize patients with emergency conditions to specialized departments, and the incompleteness of the consultants’ conclusions, which leads to the need for repeated consultations, as the main problems of counseling.14
Analysis and evaluation of other problems that arise during the consultation process showed that it is more difficult for paramedics to work on weekends. Perhaps this is due to the lack of outpatient services on weekends. In addition, problems were more likely to occur between 24:00 and 08:00. Studies in other countries have shown that admissions to the emergency department were more frequent between 4 pm and 6 pm, and the number of patients decreased markedly after 10 pm. The reason why paramedics find it more difficult to work at night may be fatigue, which makes doctors reluctant to see a patient at night.
For paramedics who took part in our survey, there were more barriers associated with consultation with certain specialties, including cardiology 56.4% (n=114) and pediatrics 12.8% (n=26). We think that this is due to the fact that the vast majority of calls are due to diseases of the circulatory system (arterial hypertension, acute coronary syndrome, etc.). In addition, the Republic of Kazakhstan is still one of the world leaders in terms of morbidity and mortality from diseases of the circulatory system, and adherence to treatment in this category of patients remains extremely low.15–17 Experts believe that the way out of this situation is to implement an individualized educational approach to the patient, constantly improve the skills of the staff of the emergency medicine department, reduce the impact of risk factors on the health of patients, as well as the development and implementation of emergency medical care algorithms that can be adapted for wide use.18,19
Another approach for optimizing the provision of emergency medical care is the use of telephone communication by paramedics for preliminary consultation with emergency department providers and notification of the need to involve consultants in examining a patient. This practice is widely used in developed countries and brings significant benefits in terms of reducing the time to make decisions about patient management and improving outcomes.20 Paramedics with more experience more often use communication tools to consult patients and more often follow the recommendations of consultant doctors, perhaps this is due to the fact that experienced paramedics have the phone numbers of doctors, to whom they turn for advice if necessary.
A multidisciplinary approach involving consultants of various profiles is especially necessary for elderly patients with a large number of chronic comorbid diseases and patients with multiple injuries. Conflicts over where patients should be admitted to and a lack of sufficient resources in the hospital result in many patients staying in the emergency department for longer periods of time, delaying the proper management and treatment they should have received.
The importance of consultations in emergency rooms and emergency departments is undeniable. Providers, paramedics, and medical staff need to work together for the benefit of the patient. The consultant physician who examined the patient may need the knowledge or experience of colleagues from different specialties in order to provide better medical care to the patient. This is very important, especially in emergency departments where many complex clinical situations arise.
Limitations
Our study has some limitations. We excluded the question “Which gender of consultants is more difficult to work with?” from the discussion. We thought that this question support a potential gender bias. Another reason for difficulties in building communication with female consultants may have been the large proportion of females among consultants in the field of internal medicine and pediatric consultants.
Conclusion
Thus, the consultation process is one of the main daily activities of a provider. Providers now require consultations more frequently than ever before, both for medico-legal reasons and for evolving medical technologies. In the past, the provider could take full responsibility for the patient they were examining. Today, patient care is not the responsibility of one provider, but is considered a team effort. Consultant physicians are an integral part of this team due to their contributions. While consultation is so important for proper diagnosis and treatment, the consultation process may not always go as planned. The consultation process can cause dissatisfaction. The emergency room staff, consultant, or patient may not be completely satisfied with the performance of the medical team. Both requesting and consulting physicians must continually improve their knowledge in order for the consultation process to be more professional. In addition, problems can be minimized by improving the communication skills of emergency medical professionals.
It should be borne in mind that problems arising in the process of counseling patients with emergency conditions could lead to poor outcomes and even death of patients, which can lead to criminal liability of medical professionals. It is extremely important that paramedics, both emergency and consultation doctors, clearly know their duties and responsibilities.
In order to improve the work of emergency medical care, we consider that regular training in communication skills is necessary for both paramedics and consultants of multidisciplinary hospitals. This could help inexperienced staff avoid conflicts with both patients, their relatives and colleagues. Timely psychological counseling could also be useful for increasing the stress resistance of medical staff and preventing the development of burnout syndrome among them. In addition, an analysis of the results of our study could be useful in scheduling paramedics on duty at different times of the day and on weekends, taking into account their length of service and experience.
Ethical Approval Details
The study has approval of the Local Ethics Commission of the Semey Medical University on March 16, 2022. All participants signed an informed consent form.
Funding
The study is performed in the frame of the Project AP 14871609 “Optimizing the structure and improving the efficiency of the emergency medicine service in Kazakhstan by conducting training for people without medical education (medical technicians)”.
Disclosure
The authors report no competing interests for this work.
References
1. Türkan H, Şener S, Tuğcu H. Improper consultation process in emergency departments and its medico-legal aspects. Tr J Emerg Med. 2005;5(2):138–141.
2. Woods RA, Lee R, Ospina MB. Consultation outcomes in the emergency department: exploring rates and complexity. CJEM. 2008;10(1):25–31. doi:10.1017/S1481803500009970
3. Erenler AK, Akbulut S, Guzel M, et al. Reasons for overcrowding in the emergency department: experiences and suggestions of an education and research hospital. Turk J Emerg Med. 2014;14(2):59–63. doi:10.5505/1304.7361.2014.48802
4. Holiman CJ. The art of dealing with consultants. J Emerg Med. 1993;11(5):633–640. doi:10.1016/0736-4679(93)90323-Y
5. Goyal P, Rustagi N, Belkić K. Physicians’ total burden of occupational stressors: more than threefold increased odds of burnout. South Med J. 2021;114(7):409–415. doi:10.14423/SMJ.0000000000001277
6. Goldman L, Lee T, Rudd P. Ten commandments for effective consultations. Arch Intern Med. 1983;143(9):1753–1755. doi:10.1001/archinte.1983.00350090131022
7. Savioli G, Ceresa IF, Gri N, et al. Emergency department overcrowding: understanding the factors to find corresponding solutions. J Pers Med. 2022;12(2):279. doi:10.3390/jpm12020279
8. Eshikumo IS, Kayipmaz AE, Kavalci C. Difficulties arising from consultation process faced by emergency physicians: a cross-sectional study. Sci Healthcare. 2020;5(22):68–73.
9. Carleton RN, Afifi TO, Turner S, et al. Mental health training, attitudes toward support, and screening positive for mental disorders. Cogn Behav Ther. 2020;49(1):55–73. doi:10.1080/16506073.2019.1575900
10. Carleton RN, Afifi TO, Turner S, et al. Mental disorder symptoms among public safety personnel in Canada. Can J Psychiatry. 2018;63(1):54–64. doi:10.1177/0706743717723825
11. Price JAB, Landry CA, Sych J. Assessing the perceptions and impact of critical incident stress management peer support among firefighters and paramedics in Canada. Int J Environ Res Public Health. 2022;19(9):4976.
12. Cooper A, Carson-Stevens A, Cooke M, et al. Learning from diagnostic errors to improve patient safety when GPs work in or alongside emergency departments: incorporating realist methodology into patient safety incident report analysis. BMC Emerg Med. 2021;21(1):139. doi:10.1186/s12873-021-00537-w
13. Turner A, Adesina A, Pillow MT, Schmidt RM, Lescinskas E, Sekhon N. Perceptions of communication between emergency medicine and internal medicine physicians. Am J Emerg Med. 2022;56:310–311. doi:10.1016/j.ajem.2021.08.020
14. Voaklander B, Gaudet LA, Kirkland SW, Keto-Lambert D, Villa-Roel C, Rowe BH. Interventions to improve consultations in the emergency department: a systematic review. Acad Emerg Med. 2022;29(12):1475–1495. doi:10.1111/acem.14520
15. Dyussenova L, Pivina L, Semenova Y, et al. Associations between depression, anxiety and medication adherence among patients with arterial hypertension: comparison between persons exposed and non-exposed to radiation from the Semipalatinsk Nuclear Test Site. J Environ Radioact. 2018;195:33–39. doi:10.1016/j.jenvrad.2018.09.016
16. Markabayeva A, Bauer S, Pivina L, et al. Increased prevalence of essential hypertension in areas previously exposed to fallout due to nuclear weapons testing at the Semipalatinsk Test Site, Kazakhstan. Environ Res. 2018;167:129–135. doi:10.1016/j.envres.2018.07.016
17. Semenova Y, Rakhimova I, Nurpeissov T, et al. Epidemiology of stroke and transient ischemic attacks in the population of the territories adjacent to the former semipalatinsk nuclear test Site, Kazakhstan. Radiat Environ Biophys. 2022;61(1):17–28. doi:10.1007/s00411-021-00955-1
18. Schofield B, Rolfe U, McClean S, Hoskins R, Voss S, Benger J. What are the barriers and facilitators to effective health promotion in urgent and emergency care? A systematic review. BMC Emerg Med. 2022;22(1):95. doi:10.1186/s12873-022-00651-3
19. Koonce TG, Storrow N, Storrow AB. A. A pilot study to evaluate learning style–tailored information prescriptions for hypertensive emergency department patients. J Med Libr Assoc. 2011;99(4):280–289. doi:10.3163/1536-5050.99.4.005
20. Detollenaere J, Van de Voorde C, Van den Heede K. Van den Heede K. Organisational models at the emergency department to reduce hospital admissions among paediatric patients: a systematic literature review. Eur J Emerg Med. 2022;29(5):329–340. doi:10.1097/MEJ.0000000000000947
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
