Back to Journals » Clinical Ophthalmology » Volume 16
Outcomes in Patients with Suprachoroidal Hemorrhage After Anterior Segment Surgery
Authors Fan J , Hudson JL, Pakravan P, Lazzarini TA , Lin BR, Fan KC, Yannuzzi NA, Sridhar J, Townsend JH , Berrocal AM, Smiddy WE , Vanner EA, Flynn HW Jr
Received 29 June 2022
Accepted for publication 7 November 2022
Published 15 December 2022 Volume 2022:16 Pages 4199—4205
DOI https://doi.org/10.2147/OPTH.S379557
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Supplementary video of "SCH after anterior segment surgery" [ID 379557].
Views: 244
Jason Fan, Julia L Hudson, Parastou Pakravan, Thomas A Lazzarini, Benjamin R Lin, Kenneth C Fan, Nicolas A Yannuzzi, Jayanth Sridhar, Justin H Townsend, Audina M Berrocal, William E Smiddy, Elizabeth A Vanner, Harry W Flynn Jr
Department of Ophthalmology, Bascom Palmer Eye Institute, University of Miami, Miami, FL, USA
Correspondence: Harry W Flynn Jr, Bascom Palmer Eye Institute, 900 NW 17th St, Miami, FL, 33136, USA, Email [email protected]
Objective: The purpose of the current study is to report outcomes of suprachoroidal hemorrhage (SCH) after anterior segment surgery at a single institution, and to identify clinical features associated with visual prognosis.
Methods and Analysis: Retrospective consecutive case series of patients with SCH occurring after anterior segment surgery.
Results: The study includes 112 eyes of 112 patients between 2014 and 2020. There were 76 cases of non-appositional SCH versus 36 cases of appositional SCH. The mean presenting visual acuity for patients with non-appositional versus appositional SCH was 2.03 logMAR (SD 0.78) versus 2.39 logMAR (SD 0.43), respectively. Visual acuity outcomes generally remained poor at last follow-up: 64 (58%) patients had a visual acuity (VA) of ≤ 20/200, including 19 (17%) with light perception (LP), and 11 (10%) with no light perception (NLP). Regarding management of non-appositional versus appositional SCH, observation was selected in 46 (61%) vs 12 (33%), delayed drainage in 14 (18%) vs 15 (42%), delayed pars plana vitrectomy in 16 (21%) vs 13 (36%), and VA at last follow-up was 1.2 versus 1.86 logMAR (p=0.002). In patients that were observed, both appositional SCH (p=0.01) and duration of apposition (p=0.04) were correlated with worse outcome.
Conclusion: Appositional SCH was associated with poorer visual outcomes compared to non-appositional SCH. Observation remains a reasonable management strategy for non-appositional SCH.
Keywords: suprachoroidal hemorrhage, non-appositional, appositional, anterior segment surgery
Introduction
Suprachoroidal hemorrhage (SCH) occurs when blood from the short or long ciliary arteries accumulates in the potential space between the choroid and sclera. It is usually precipitated by intraocular surgery or trauma. Mechanistically, SCH is theorized to occur in the setting of hypotony or sudden decrease in intraocular pressure (IOP), which leads to choroidal effusion, stretching of ciliary arteries, and then rupture of an artery with hemorrhage into the suprachoroidal space. Patients may present with symptoms of sudden onset severe pain, nausea, vomiting, and decreased vision, as well as signs of anterior chamber shallowing with elevated IOP. Onset may be delayed after surgery, and atypical presentations, such as SCH mimicking a choroidal mass, have been reported.1,2
The incidence of SCH differs depending on the type of ocular surgery. Glaucoma surgery has the highest incidence of SCH, ranging from 0.15 to 6.1%.3 The incidence of SCH secondary to cataract surgery has decreased to 0.03–0.06% with the adoption of phacoemulsification techniques, presumably due to better maintenance of intraoperative IOP.4 Risk factors for the development of SCH include advanced age, anticoagulation, uncontrolled hypertension, atherosclerotic disease, diabetes, history of glaucoma, hypotony, high myopia, aphakia, previous intraocular surgery/trauma, elevated perioperative IOP, Valsalva maneuvers, and prolonged surgical time.3,5–19
SCH can be classified in several ways: by etiology, extent of hemorrhage (ie in terms of quadrants), or by degree of elevation. Appositional or “kissing” SCH occurs when the degree of elevation of two opposing sides is so great that it causes inner retinal touch (Figure 1). Ultrasonography is helpful in identifying and defining the features of SCH; there is typically a dome-shaped elevation of the choroid filled with hyperechoic material, which becomes hypoechoic over time as the blood clot liquifies. Ultrasonography can thus also aid in determining the need for and optimal timing of surgical drainage (Figure 1A and B).
There have been many advances in vitreoretinal surgical technology. However, whether these advances have improved outcomes after suprachoroidal hemorrhage remains unclear. This study seeks to investigate visual acuity (VA) outcomes in patients with SCH after anterior segment surgery.
Materials and Methods
The institutional review board of the University of Miami approved the study protocol, and the study was conducted in accordance with the Declarations of Helsinki. This study involved the retrospective review of medical records and did not have prospective contact with potential study subjects prior to acquisition of the requested data. As a result, the University of Miami approved a waiver of consent in accordance with US Code of Federal Regulations guidelines. The study design was a retrospective case series of patients with suprachoroidal hemorrhage occurring after anterior segment surgery. SCH after trauma, PPV, or retinal detachment (RD) surgery were not included. Diagnosis of suprachoroidal hemorrhage was made clinically and followed by confirmation on B-scan ultrasonography. Images were individually reviewed by the physicians. Serous choroidals were ruled out by analysis of the B-scan images. Measured preoperative variables included age, sex, hypertension, anticoagulation status, lens status, surgery type causing SCH, presenting VA, presenting intraocular pressure (with hypotony defined as IOP <8mmHg), concurrent pathology on presentation (including flat anterior chamber, vitreous hemorrhage, retinal detachment), and duration of apposition. Intraoperative variables included management of SCH (observation, delayed drainage, or delayed vitrectomy (PPV)), while post-operative variables included VA and IOP on follow-up. Observation was defined as treatment limited to non-surgical interventions. Delayed drainage and PPV were not defined by a given number of days, but rather by the surgeon’s decision to observe/monitor with serial ultrasonography, and then to intervene surgically once there was evidence of liquefaction of the clot. Management decisions were surgeon preference and did not follow a prospective protocol. The following logMAR assignments were utilized: counting fingers = 2.0, hand motion = 2.3, light perception = 2.6, and no light perception = 3. VA and IOP “at last follow-up” were determined only from patients with greater than 3 months of follow-up (101 and 94 patients, respectively). Student’s t-test and Wilcoxon-Mann–Whitney u-test were used for parametric and non-parametric data, respectively. Spearman’s rank order correlation was used for continuous data. Patients and the public were not involved in the design, conduct, reporting, or dissemination plans of this research.
Results
The current study included 112 eyes from 112 patients diagnosed with SCH after cataract, corneal, or glaucoma surgery between January 1, 2014 and October 31, 2020. The mean patient age was 79.9 years, and 51 (46%) patients were female (Table 1). Regarding systemic factors, 85 (76%) patients were hypertensive, 30 (26.8%) were diabetic, and 42 (38%) were taking anticoagulant medications. The majority of patients were pseudophakic (n=85, 76%).
 |
Table 1 Clinical Characteristics in Patients with SCH Associated with Anterior Segment Surgery (n=112) |
The mean presenting VA was hand motion (HM) (logMAR 2.15, SD 0.703) and ranged from 20/70 to NLP (Table 1). The mean presenting IOP was 19.2 (SD 14.9). There were 76 cases of non-appositional SCH and 36 cases of appositional SCH. The mean presenting visual acuity for patients with non-appositional SCH was 2.03 logMAR (SD 0.78) versus 2.39 logMAR (SD 0.43) for appositional SCH.
Presenting features included relative afferent pupillary defect (rAPD) (n=8, 7%), hypotony (n=43, 44%), vitreous hemorrhage (n=32, 31%), and concurrent or delayed retinal detachment (n=30, 29%) (Table 2). SCH after glaucoma surgery accounted for 59 (53%) of cases, while SCH after cataract surgery accounted for 37 (33%) of cases. The remainder of cases occurred after non-traumatic corneal perforation or other corneal surgery (ie penetrating keratoplasty). SCH occurred intraoperatively (n=38, 35%) versus post-operatively (n=70, 65%).
 |
Table 2 Clinical Features of SCH Associated with Anterior Segment Surgery |
Management decisions were made by the individual physician, but observation was usually selected when SCH involved <2 quadrants or vision was NLP on presentation. Additionally, at this institution, timing of surgical intervention was usually based on echographic findings of clot lysis, which generally occurred 10 to 14 days after onset of hemorrhage. In cases of non-appositional SCH, 46 (61%) patients were observed (mean final VA 0.92, SD 0.88), 14 (18%) underwent delayed drainage (mean final VA 1.66, SD 1.08), and 16 (21%) underwent PPV (mean final VA 1.66, SD 0.92) (Table 3). In cases of appositional SCH, 12 (33%) patients were observed (mean final VA 1.78, SD 1.16), 15 (42%) underwent delayed drainage (mean final VA 1.951, SD 0.73), and 13 (36%) underwent PPV (mean final VA 1.89, SD 0.73). A significant number of patients with appositional SCH were treated with combined delayed drainage and PPV (n=7). Therefore, comparison of visual outcome between the interventions would not be meaningful. A representative surgical video showing delayed drainage by the scleral cutdown method is shown in the Supplementary video.
 |
Table 3 Management as Selected by Treating Physician and VA Outcome |
Mean VA at last follow-up was better in non-appositional versus appositional SCH (1.20 logMAR (SD 0.97) vs 1.86 logMAR (SD 0.89), respectively (p=0.002)) (Figure 2). Overall, 47 (42%) patients had final VA of 20/200 or better, and 64 (58%) had a VA ≤ 20/200, including 6 (5%) with counting fingers, 11 (10%) with hand motions, 19 (17%) with light perception (LP), and 11 (10%) with no light perception (NLP). Patients who were observed had the best mean final VA (logMAR 1.21, SD 1.03, p=0.0017), while those with delayed drainage (logMAR 1.87, SD 0.90) or delayed PPV with or without scleral buckle (logMAR 1.73, SD 0.84) had worse outcomes. Within each intervention type, appositional SCH (p=0.04) and duration of apposition >7 days (p=0.002) were associated with worse outcomes only in the observation group.
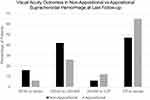 |
Figure 2 Visual acuity at last follow-up in non-appositional vs appositional suprachoroidal hemorrhage. The percentage of patients in each visual acuity group is shown. |
Discussion
The current study reports the largest series of suprachoroidal hemorrhage and demonstrates that despite advances in ocular surgery, outcomes after SCH generally remain poor. Several previously identified factors were associated with poorer VA outcome: APD, retinal detachment, appositional SCH, and duration of apposition >7 days.20 In the current study, duration of apposition >7 days was associated with poorer VA outcome only in cases that were managed by observation. This suggests that surgical intervention to relieve retinal apposition may be considered in eyes with appositional SCH if there is at least light perception vision. Appositional SCH may be associated with poorer visual outcome for multiple reasons, including greater degree of choroidal detachment, greater volume of suprachoroidal blood, and higher intraocular pressures. Furthermore, retina-to-retina adhesions have been reported in cases of appositional SCH and are generally considered an indicator of poor prognosis.21,22
Prior retrospective studies at this institution also included traumatic SCH, or only assessed appositional SCH, and are therefore not directly comparable to the current study.20,23 With these caveats in mind, however, the cohort in this study did demonstrate superior visual outcomes. Scott et al, studied only appositional SCH, reporting that 29% with appositional SCH achieved a VA better than counting fingers,20 while 60% of patients in the current study had this outcome. In the study by Reynolds et al, which included traumatic SCH, 24% (25/106) of patients achieved a final VA of 20/200 or better,23 while 38% (43/112) of patients in the current study had this outcome. In contrast to these prior studies, a higher proportion of patients in the current study were observed (52.8% vs 21.6% in Scott et al vs 46.2% in Reynolds et al). Future studies with comparable cohorts are needed to assess for changes in management outcomes.
More recent retrospective studies performed at other institutions reported differences in their cohort composition, but had comparable findings to the current study.24 Qureshi et al performed a retrospective analysis of 20 patients who underwent drainage with or without vitrectomy for SCH.24 The most common cause of SCH within their cohort was phacoemulsification (35%, 7/20), and the series included 2 cases of traumatic SCH. External drainage alone was performed in 55% (11/20), while 45% (9/20) had combined PPV and drainage. Of patients who underwent external drainage, 72% (8/11) achieved a vision of 20/200 or greater, and 9% (1/11) became NLP, as compared to patients who underwent PPV with external drainage, where only 11% (1/9) of patients achieved a vision of 20/200 or greater. Consistent with the current study, those patients undergoing PPV tended to have poorer outcomes, likely due to the increased complexity of these cases.
The current study is notable for its focus on SCH after anterior segment surgery. Traumatic SCH is highly variable in both its etiology and severity of presentation, and thus should represent a distinct entity.3 Limitations of the study include its retrospective nature, relatively small number of patients, single center focus, and management selected by physician preference.
Conclusion
SCH remains a severe potential complication of intraocular surgery and has a guarded visual prognosis. In eyes with non-appositional SCH, observation remains a reasonable management strategy. However, in eyes with appositional SCH, management remains more challenging and surgical intervention may be indicated.
Ethics Approval Statement
The institutional review board of the University of Miami approved the study protocol (IRB # 20201265), and the study was conducted in accordance with the Declarations of Helsinki.
Acknowledgments
The authors would like to thank Dr. Elizabeth Vanner for performing the statistical analysis for this study. The abstract of this paper was presented at the ARVO 2021 and 2022 conferences as a poster presentation with interim findings. The poster’s abstract was published in “Poster Abstracts” in Investigative Ophthalmology & Visual Science June 2021, Vol.62, 3666 and Investigative Ophthalmology & Visual Science June 2022, Vol.63, 3395 – F0295.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
US National Institutes of Health Center Core Grant P30EY014801; an unrestricted grant to the University of Miami from the National Eye Institute; and Research to Prevent Blindness, New York, NY, USA (GR004596).
Disclosure
Dr Jayanth Sridhar reports personal fees from Alcon, DORC, Genentech, and Regeneron, outside the submitted work. Harry W Flynn Jr reports grants from NIH Center and Research to Prevent Blindness, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. Marous CL, Sioufi K, Shields CL, Mashayekhi A, Shields JA. Coughing-induced suprachoroidal hemorrhage simulating melanoma in two cases. Retin Cases Brief Rep Fall. 2018;12(4):336–341. doi:10.1097/ICB.0000000000000502
2. Oli A, Balakrishnan D. Multimodal imaging in a case of localized suprachoroidal hemorrhage. J Ophthalmic Vis Res. 2020;15(1):104–108. doi:10.18502/jovr.v15i1.5956
3. Chu TG, Green RL. Suprachoroidal hemorrhage. Surv Ophthalmol. 1999;43(6):471–486. doi:10.1016/s0039-6257(99
4. Davison JA. Acute intraoperative suprachoroidal hemorrhage in capsular bag phacoemulsification. J Cataract Refract Surg. 1993;19(4):534–537. doi:10.1016/s0886-3350(13
5. Risk factors for suprachoroidal hemorrhage after filtering surgery. The Fluorouracil Filtering Surgery Study Group. Am J Ophthalmol. 1992;113(5):501–507. doi:10.1016/s0002-9394(14
6. Sharma T, Virdi DS, Parikh S, Gopal L, Badrinath SS, Mukesh BN. A case-control study of suprachoroidal hemorrhage during pars plana vitrectomy. Ophthalmic Surg Lasers. 1997;28(8):640–644. doi:10.3928/1542-8877-19970801-05
7. Ariano ML, Ball SF. Delayed nonexpulsive suprachoroidal hemorrhage after trabeculectomy. Ophthalmic Surg. 1987;18(9):661–666.
8. Cantor LB, Katz LJ, Spaeth GL. Complications of surgery in glaucoma. Suprachoroidal expulsive hemorrhage in glaucoma patients undergoing intraocular surgery. Ophthalmology. 1985;92(9):1266–1270. doi:10.1016/s0161-6420(85)33872-1
9. Chorich LJ, Derick RJ, Chambers RB, et al. Hemorrhagic ocular complications associated with the use of systemic thrombolytic agents. Ophthalmology. 1998;105(3):428–431. doi:10.1016/S0161-6420(98)93023-8
10. Givens K, Shields MB. Suprachoroidal hemorrhage after glaucoma filtering surgery. Am J Ophthalmol. 1987;103(5):689–694. doi:10.1016/s0002-9394(14
11. Chu TG, Cano MR, Green RL, Liggett PE, Lean JS. Massive suprachoroidal hemorrhage with central retinal apposition. A clinical and echographic study. Arch Ophthalmol. 1991;109(11):1575–1581. doi:10.1001/archopht.1991.01080110111047
12. Gressel MG, Parrish RK 2nd, Heuer DK. Delayed nonexpulsive suprachoroidal hemorrhage. Arch Ophthalmol. 1984;102(12):1757–1760. doi:10.1001/archopht.1984.01040031421015
13. Ingraham HJ, Donnenfeld ED, Perry HD. Massive suprachoroidal hemorrhage in penetrating keratoplasty. Am J Ophthalmol. 1989;108(6):670–675. doi:10.1016/0002-9394(89
14. Ruderman JM, Harbin TS
15. Speaker MG, Guerriero PN, Met JA, Coad CT, Berger A, Marmor M. A case-control study of risk factors for intraoperative suprachoroidal expulsive hemorrhage. Ophthalmology. 1991;98(2):202–209. doi:10.1016/s0161-6420(91)32316-9
16. Tabandeh H, Sullivan PM, Smahliuk P, Flynn HW
17. Taylor DM. Expulsive hemorrhage: some observations and comments. Trans Am Ophthalmol Soc. 1974;72:157–169.
18. Mafee MF, Linder B, Peyman GA, Langer BG, Choi KH, Capek V. Choroidal hematoma and effusion: evaluation with MR imaging. Radiology. 1988;168(3):781–786. doi:10.1148/radiology.168.3.3261432
19. Lakhanpal V, Schocket SS, Elman MJ, Dogra MR. Intraoperative massive suprachoroidal hemorrhage during pars plana vitrectomy. Ophthalmology. 1990;97(9):1114–1119. doi:10.1016/S0161-6420(90
20. Scott IU, Flynn HW
21. Berrocal JA. Adhesion of the retina secondary to large choroidal detachment as a cause of failure in retinal detachment surgery. Mod Probl Ophthalmol. 1979;20:51–52.
22. Lakhanpal V. Experimental and clinical observations on massive suprachoroidal hemorrhage. Trans Am Ophthalmol Soc. 1993;91:545–652.
23. Reynolds MG, Haimovici R, Flynn HW
24. Qureshi A, Jalil A, Sousa DC, et al. Outcomes of suprachoroidal haemorrhage drainage with and without vitrectomy: a 10-year study. Eye. 2021;35(7):1879–1885. doi:10.1038/s41433-020-01170-w
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

