Back to Journals » Clinical Ophthalmology » Volume 17
Online Questionnaire-Based Study on the Knowledge, Attitude, and Practices of Non-Ophthalmic Physicians-in-Training Regarding Exposure Keratopathy Among Patients Admitted in a Tertiary Referral Hospital
Authors Sosuan GMN , Sandoval PF Jr, Torrefranca AB Jr , Tan RRG, Lim Bon Siong R
Received 6 December 2022
Accepted for publication 11 January 2023
Published 21 January 2023 Volume 2023:17 Pages 303—312
DOI https://doi.org/10.2147/OPTH.S399665
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
George Michael N Sosuan,1 Pablito F Sandoval Jr,1 Aramis B Torrefranca Jr,1 Reginald Robert G Tan,1,2 Ruben Lim Bon Siong1,2
1Department of Ophthalmology and Visual Sciences, Philippine General Hospital, University of the Philippines Manila, Manila, Philippines; 2Eye Institute, St. Luke’s Medical Center, Quezon City, Philippines
Correspondence: George Michael N Sosuan, Email [email protected]
Objective: This study aimed to determine the knowledge, attitude, and practices of non-ophthalmic physicians-in-training regarding recognition and prevention of exposure keratopathy among patients admitted in a tertiary referral hospital.
Methods: This study was a single-center cross-sectional study. An anonymous self-administered online questionnaire was distributed among non-ophthalmic physicians-in-training at the Philippine General Hospital (PGH) using convenience and snowball sampling.
Results: A total of 77 responses were recorded with a response rate of 37%. The majority of the respondents uniformly reported the absence of an established eye care protocol or policy being implemented for different subsets of patients at risk for developing exposure keratopathy. Ninety-six percent (96%) was aware of exposure keratopathy. The most urgent reason for referral to the ophthalmology service was the presence of whitish of opacity at 46.8%, while the least urgent reason was the presence of eye redness at 36.4%. Only 43% of the patients with incomplete eyelid closure was referred to the ophthalmology service. The most frequently used modality of prophylactic eye protection treatment was eyelid taping (84.4%) followed by lubricants (drops and gels, 79.1%). The most common reason for not referring was the absence of an established protocol on the appropriate indication for referral to the ophthalmology service.
Conclusion: This study showed that the majority of non-ophthalmic physicians-in-training had adequate knowledge and favorable attitude regarding recognition and prevention of exposure keratopathy among patient admitted at the PGH; however, the absence or the unavailability of an eye care protocol among patients with inadequate eyelid closure in our institution on the prevention of exposure keratopathy and its early treatment and appropriate indications for ophthalmology referral resulted in non-uniformity and varied practice patterns on its management.
Keywords: exposure keratopathy, practice pattern, tertiary referral hospital, online questionnaire
Introduction
Exposure keratopathy (EK) is a clinical syndrome that includes varying severity of corneal damage due to incomplete eyelid closure and tear film defects, subsequently leading to significant visual loss.1 EK, commonly found in hospital in-patients, can occur at a rate as low as 10% to as high as 60% among the critically ill and mechanically ventilated.2
The pathophysiology of the EK involves incomplete eyelid closure or lagophthalmos, leaving the ocular surface and cornea unprotected. The exposure will cause drying or desiccation of the cornea and may lead to erosions on the corneal epithelium.3,4 EK usually resolves as the patient recovers; however, in neglected cases, it causes microbial keratitis leading to corneal perforation or scarring, and eventual permanent visual loss.5
Increased risk of developing EK has been documented among patients in the intensive care unit (ICU),2 and this has been due to the higher incidence of lagophthalmos with the use of sedative and neuromuscular blocking agents in this setting. In addition to their negative effects on eyelid closure, these medications interfere with the normal blink reflex that is responsible for adequate distribution of the tear film over the cornea and also negatively affect the Bell’s phenomenon.6 Other risk factors that may contribute to EK include positive pressure ventilation, high-flow oxygen rates, and fluid imbalances and increase vascular permeability. Positive pressure ventilation raises the patient’s venous pressure, and indirectly causes conjunctival edema and lagophthalmos. High-flow oxygen rates through nebulizers or face masks may desiccate the cornea from increased evaporation. Fluid imbalances and increased vascular permeability can lead to conjunctival edema and subsequent lagophthalmos.7
With the COVID-19 outbreak being declared as a pandemic and a global health emergency by the World Health Organization on March 11, 2020. There was a continuous surge in patients admitted to critical care units across the world, including the Philippines.8 Due to the rapid spread of this life-threatening disease requiring hospital admissions and the lack of healthcare workers, eye care for these patients, especially prevention of corneal complications such as EK, was less of a priority. In addition, the absence of a universally accepted protocol for the protection of eyes in the ICU augments this problem.9
In recent years, there has been a significant rise in referred cases of exposure keratopathy to the External Disease and Cornea Clinic in our institution. All cases were referred when the corneal complications were already present. Currently, there are no local published data on the awareness of non-ophthalmic physicians-in-training on this visually disabling yet preventable disease. The authors aimed to determine the knowledge, attitude, and practices of non-ophthalmic physicians-in-training regarding recognition and prevention of exposure keratopathy among patients admitted at the Philippine General Hospital (PGH). Although with no direct benefit to the respondents, the authors hoped to use the data gathered from this study to help formulate hospital guidelines for the prevention of this visually-disabling disease.
Methods
The study was a single-center, cross-sectional study. The study was an anonymous self-administered online questionnaire via Google Forms of non-ophthalmic physicians-in-training of the Philippine General Hospital. The link to the online questionnaire was sent to the chief residents of the Departments of Surgery, Medicine, Otorhinolaryngology-Head and Neck Surgery, Pediatrics, Neuroscience (Neurology and Neurosurgery), and Rehabilitation Medicine to disseminate to the physicians-in-training of their respective departments. Convenience and snowball sampling were used. A target minimum sample size of 75 respondents was needed based on an error rate of 5% and a confidence interval of 95%, and an assumed response rate of 42% referenced from the response rate of the survey study conducted by Bromeo et al.10
For the inclusion criteria, the respondents should be enrolled as a resident or fellow in any of the Departments of Surgery, Medicine, Otorhinolaryngology-Head and Neck Surgery, Pediatrics, Neuroscience (Neurology and Neurosurgery), and Rehabilitation Medicine of the Philippine General Hospital. Respondents who were not formally recognized as either a resident or fellow in their departments such as hospitalists, adjuncts, medical specialists, or those on observership would be excluded from the study.
The Exposure Keratopathy Questionnaire
The online questionnaire can be accessed through the provided link: https://forms.gle/B1d7szmw6rii6X5J7. Prior to the commencement of the anonymous self-administered online questionnaire, each respondent was required to give his/her informed consent electronically by clicking on a tick box signifying their approval to voluntarily participate in the study for which no compensations/reimbursements were offered by the researcher. The online questionnaire was divided into four sections, namely general demographic questions, presence of an eye care protocol, awareness of exposure keratopathy, and prevention and treatment of exposure keratopathy, and would take approximately 10–15 minutes to answer. A submission was considered only upon completion of all the questions. The online questionnaire comprised of 28 multiple-choice questions with an option of filling-in if the answer was not available among the given choices. The questionnaire that was used was adapted and modified from the studies of Vidha11 and Kam,12 and was then reviewed by three External Disease and Cornea Specialists for its content validity and by seven non-ophthalmic physicians for its face validity.
The online questionnaire did not ask for any identifiable personal details from the respondents. Also, the completed questionnaires were stored in password-protected hard drives, can only be accessible to the investigators, and would be permanently deleted after a minimum of 3 years as recommended by the National Ethical Guidelines for Health and Health-Related Research (NEGHHR) 2017.
The data were generated and obtained in proportions based on the answers to the online questions via the Google Forms platform and were collected by the primary investigator. A descriptive analysis using frequency and percentage was used for each of the responses for each question with no subgroup analysis.
Results
A total of 77 responses were recorded out of 210 to whom the survey link was sent (response rate of 37%) in a 5-month period (May to September 2022) of data collection. Since all respondents who completed the questionnaire gave consent, all answers were included in the analysis. The demographic characteristics of the respondents are shown in Table 1. Nearly two-thirds of the respondents were in their residency training, and the other one-third were in their fellowship training. The majority of the residents who responded were on their second-and-third-year level of training, while the majority of the fellows who responded were on their second-and-first year level of training. Most of the respondents (35.1%) came from the Department of Medicine, followed by the Department of Pediatrics at 21%.
 |
Table 1 Demographic Characteristics of the Respondents |
Presence of Eye Care Protocol
Among non-ophthalmic physicians-in-training seeing patients in the intensive care unit, only 10.4% reported for the availability of an eye care protocol or policy among patients admitted. More than half (54.5%) reported the absence of an eye care protocol or policy, and nearly one-third (28.6%) of the respondents did not know whether an eye care protocol or policy was available or not (Table 2).
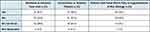 |
Table 2 The Availability of Eye Care Protocol for Different Subsets of Patients at Risk for Developing Exposure Keratopathy |
For unconscious or sedated patients and for patients with facial nerve palsy or lagophthalmos of any etiology, most respondents reported the absence of an eye care protocol or policy at 53.2% and 44.2%, respectively. Nearly a quarter of the respondents did not know whether an eye care protocol or policy was available or not (Table 2).
Eyelid closure (Table 3) among unconscious or sedated patients was assessed by 48.1% of the respondents; while among patients with facial nerve palsy or lagophthalmos of any etiology, eyelid closure was assessed by 61% of the respondents. The results showed that nearly one-third (30%) of respondents were assessing eyelid closure among patients at risk for developing exposure keratopathy, even though they were not aware of the presence or availability of an eye care protocol or policy. More than half (54%) of the respondents assessing patient eyelid closure were doing it once daily.
 |
Table 3 Assessment of Eyelid Closure of Patients at Risk for Developing Exposure Keratopathy |
Awareness of Exposure Keratopathy
Ninety-six percent of the respondents was aware of exposure keratopathy. Eighty-eight percent of them correctly identified its etiopathogenesis which is damage to the cornea that occurs from drying of the outer surface of the eye due to the prolonged contact to the outside environment. Based on the responses, reduced consciousness level (90.9%) and protrusion/bulging of the eye (exophthalmos/proptosis, 90.9%) were the most common risk factors considered for exposure keratopathy (Figure 1). This was subsequently followed by facial nerve palsy (89.6%), pre-existing diseases of the outer surface of the eye (81.8%), and eyelid malposition (76.6%). Only a quarter (26%) of the respondents requested for special precautions to protect the eye of patients undergoing nursing care procedures such as tracheal suctioning and sponge bath. For the signs of exposure keratopathy (Figure 2), conjunctival redness or hyperemia (90.9%) was the most common sign considered followed by whitish corneal opacity (72.7%) and conjunctival edema or chemosis (72.7%). Table 4 shows the reasons for referral to the ophthalmology service. The most urgent reason was the presence of whitish of opacity at 46.8% followed by eye discharge at 27.3%, while the least urgent reason was the presence of eye redness at 36.4% followed by lagophthalmos at 33.8%. At least half (50.6%) of the respondents identified correctly all of the possible complications of exposure keratopathy; moreover, 98.7% of the respondents (Figure 3) was able to identify corneal epithelial defect/ulcer as a complication, which is the earliest corneal complication of exposure keratopathy.
 |
Table 4 Reasons for Referral to the Ophthalmology Service |
 |
Figure 1 Risk factors for exposure keratopathy considered by the respondents. |
 |
Figure 2 Signs of exposure keratopathy considered by the respondents. |
 |
Figure 3 Complications of exposure keratopathy considered by the respondents. |
Prevention and Treatment of Exposure Keratopathy
Among patients with incomplete eyelid closure, 43% was referred to the ophthalmology service by the respondents (Figure 4). Around 52% was managed by the respondents as follows: 40% by starting eye treatment and 12% by observation. In terms of delivery of prophylactic treatments (Figure 5), none of the respondents withheld any treatments. Overall, the single most frequently used modality of prophylactic eye treatment (including use alone or on combination with other treatments) was eyelid taping (84.4%) followed by lubricants (drops and gels, 79.1%). The median interval for delivery of all types of prophylactic treatment for preventing exposure keratopathy was every 4–8 hours.
 |
Figure 4 Frequency distribution of the management among patients with incomplete eyelid closure by the respondents. |
 |
Figure 5 Modes of prophylactic treatments used and the number of respondents employing each method, either alone or in combination with other methods. |
For the practice patterns, only 35% of the respondents were referring all patients with incomplete eyelid closure to the ophthalmology service. The most common reason for not referring was the absence of an established protocol on the appropriate indication for referral to the ophthalmology service. Most of the respondents were initially managing exposure keratopathy with eyelid taping and lubricants by themselves since most patients had far worse medical problems that needed to be addressed first, and would refer only if they saw an urgent indication for referring such as whitish opacity or an infection. Some would refer only if the cause of incomplete eyelid closure was permanent, because of the fear of overburdening the ophthalmology service with referrals. For the disposition of patients with exposure keratopathy seen at the hospital on the year 2021 (Figure 6), 50% was not referred to the ophthalmology service for those respondents who saw 1 to 3 patients, 4 to 6 patients, and more than 6 patients.
 |
Figure 6 The disposition of patients with exposure keratopathy seen at the hospital (2021). |
As demonstrated in Figure 7, 81% of the patients with exposure keratopathy referred to the ophthalmology service was seen within 24 hours from the time of referral, and 38% of them was seen within 12 hours. For the administration of the prescribed treatment plan for the patient, most were administered by the nurses/nursing attendant (60%). Some were administered by the physicians (21%) or relatives (14%).
 |
Figure 7 Frequency distribution of the time in hours it takes for the ophthalmology service to see referred patients from the time of referral. |
Discussion
This was the first institution-wide online survey examining the knowledge, attitudes, and practices of non-ophthalmic physicians-in-training regarding recognition and prevention of exposure keratopathy among patients admitted at PGH. Our results showed that majority of non-ophthalmic physicians-in-training had adequate knowledge and favorable attitude regarding recognition and prevention of exposure keratopathy among patient admitted at the PGH; however, the absence or the unavailability of an accepted and established eye care protocol among patients with inadequate eyelid closure in our institution on the prevention of exposure keratopathy and its early treatment and appropriate indications for ophthalmology referral resulted to non-uniformity and varied practice patterns on its management. This could have resulted to inadequate prophylactic treatments to prevent exposure keratopathy, and thus late referrals with an increased number of corneal complications among the referred cases to the External Disease and Cornea clinic in our institution.
An adequate number (77) of participants were able to complete the online questionnaire during the 5-month period of data collection. Physician-in-trainings were the chosen population since they were the ones seeing and managing the patients admitted at PGH on a daily basis. In our institution, there is a greater number of residents compared to fellows; hence, a large number of the respondents were residents from the bigger Departments of Medicine and Pediatrics.
Our study demonstrated that the majority (>65%) of the respondents uniformly reported the absence of an established eye care protocol or policy being implemented for different subsets of patients at risk for developing exposure keratopathy. Eyelid closure was assessed in our institution at 48.1% and 61% for unconscious or sedated patients and patients with facial nerve palsy or lagophthalmos of any etiology, respectively. Comparing our data with England, eyelid closure was assessed 66% for patients admitted at their ICUs. Sixty percent of the ICUs in England have already adopted eye care protocols or policy.12 Our results showed that nearly half of our respondents were aware and were able to assess eyelid closure among patients at risk for exposure keratopathy despite the absence of an eye care protocol or policy.
Only 4% of the respondents was not aware of exposure keratopathy. More than 75% of the respondents were able to correctly identify risk factors for exposure keratopathy relating to local factors affecting the blink reflex and the ocular surface; however, only 30–40% of the respondents were able to identify environmental factors that contribute to the development of exposure keratopathy. Only 72.7% of the respondents had identified whitish corneal opacity as a sign of exposure keratopathy, and only 46.8% had identified it as the most urgent reason for referral. Unfortunately, this is already a late-stage finding and has permanent visually disabling complications. In formulating hospital guidelines for the prevention of exposure keratopathy, an emphasis to the environmental risk factors and early signs of exposure keratopathy and its prevention should be made. Many correctly identified the complications of EK, and the authors suggest that an audit record of ocular complications should be started for incidence reporting.
At least 83% of the patients with incomplete eyelid closure were managed by the respondents. Half of these were referred to the ophthalmology service and the other half were treated by the respondents with eyelid taping and lubricants (either alone or in combination with other methods). The authors believe that the current trend and attitude of not referring early in the course of the disease and the varied pattern of prophylactic treatments are mainly due to the absence or the unavailability of an accepted and established eye care protocol. Although a lot of patients at risk for EK have concomitant medical problems that need to be addressed first, a whitish corneal opacity/scar, albeit easily prevented, can be permanently visually disabling. In this day and age where there is a scarcity of corneal tissue for keratoplasty in our country, an emphasis should be made for the prevention of these visually disabling corneal scars. Among patients referred to the ophthalmology service, 81% of the patients was seen timely within recommended 24 hours for non-urgent cases. The prescribed treatment plans were mostly (81%) administered by the health care professionals to ensure correctness and compliance.
The limitations of the study include that the study was conducted in a government tertiary referral hospital. Thus, the results of the study might not be completely generalizable to other hospital settings. The sample population in the study was limited to physicians-in-training. The perspectives of other allied health professionals were not included in the study. Another limitation of the study is the inability if the principal investigator to control the sampling method per department. As with any other survey, the provided answer may differ from actual practices of the respondents from May to September 2022 and do not reflect changes in their attitudes and practice patterns over time. An inherent limitation of online surveys is an inadequate response rate. Although our study attained a good response rate by industry standards, a higher response rate will be better.
In conclusion, the study showed that the majority of non-ophthalmic physicians-in-training had adequate knowledge and favorable attitude regarding recognition and prevention of exposure keratopathy among patients admitted at the PGH. However, the absence or the unavailability of an accepted and established eye care protocol among patients with inadequate eyelid closure in our institution resulted in non-uniformity and varied practice patterns on its management.
The authors recommend that a hospital guideline for the prevention of exposure keratopathy should be carefully formulated with an emphasis to the environmental risk factors and early signs of exposure keratopathy is warranted. Preventive measures addressing exposure keratopathy should be highlighted, especially with very limited supply of corneal tissues. The authors also recommend that timely referral to ophthalmology service be made once corneal erosion is present. Corneal erosion is the earliest corneal complication of exposure keratopathy. Education on proper assessment and recognition of corneal erosion among non-ophthalmic physicians-in-training should be promulgated.
Abbreviations
EK, exposure keratopathy; ICU, intensive care unit; PGH, Philippine General Hospital.
Data Sharing Statement
The datasets used and analyzed in the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The study adhered to the tenets of the Declaration of Helsinki. The study was approved by the University of the Philippines Manila Research Ethics Board (UPMREB 2022-0176-01). The study commenced only upon approval of the study protocol. Informed consent given electronically was required prior to inclusion to the study. Utmost care was dedicated into ensuring the confidentiality of the online questionnaire’s responses. The respondents were advised that they may refuse to participate anytime in the course of the study.
Acknowledgments
The authors thank Dr Josept Mari Poblete, Dr Anna Victoria San Pedro, Dr Ivo John Dualan, Ms Janice Mabanglo and the Department of Ophthalmology and Visual Sciences of the University of the Philippines Manila – Philippine General Hospital for the support in making and completing this paper.
Funding
The primary investigator was the primary financier of the study. There were no additional budget concerns for both the respondents and the institution because of the online nature of the questionnaire.
Disclosure
Dr Ruben Lim Bon Siong reports personal fees from Santen and Allergan, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. American Academy of Ophthalmology. Basic and clinical science course: section 8: external disease and cornea. Am Acad Ophthalmol. 2021;2021:79.
2. Kuruvilla S, Peter J, David S, et al. Incidence and risk factor evaluation of exposure keratopathy in critically ill patients: a cohort study. J Crit Care. 2015;30:400–404. doi:10.1016/j.jcrc.2014.10.009
3. Mercieca F, Suresh P, Morton A, Tullo A. Ocular surface disease in intensive care unit patients. Eye. 1999;13:231–236. doi:10.1038/eye.1999.57
4. Imanaka H, Taenaka N, Nakamura J, et al. Ocular surface disorders in the critically ill. Anesth Analg. 1997;85:343–346. doi:10.1097/00000539-199708000-00018
5. Ti SE, Scott JA, Janardhanan P, Tan DT. Therapeutic keratoplasty for advanced suppurative keratitis. Am J Ophthalmol. 2007;143:755–762. doi:10.1016/j.ajo.2007.01.015
6. Grixti A, Sadri M, Edgar J, Datta AV. Common ocular surface disorders in patients in patients intensive care units. Ocul Surf. 2012;190:26–42. doi:10.1016/j.jtos.2011.10.001
7. Sansome SG, Lin P-F. Eye care in the intensive care unit during the COVID-19 pandemic. Br J Hosp Med. 2020;81(6):1–10. doi:10.12968/hmed.2020.0228
8. World Health Organization. Coronavirus (COVID-19); 2020. Available from: https://covid19.who.int/.
9. Farrell M, Wray F. Eye care for ventilated patients. Intensive Crit Care Nurs. 1993;9:137–141. doi:10.1016/0964-3397(93)90055-3
10. Bromeo AJ, Grulla-Quilendrino P, Lerit SJ, et al. Changes in retina practice patterns during the COVID-19 pandemic in the Philippines. Clin Ophthalmol. 2021;15:3493–3504. doi:10.2147/OPTH.S326594
11. Vidha A, Shambhu R, Jain R, Hegde V. A questionnaire-based study on awareness and practices of nursing staff regarding risk factors and prevention of exposure keratopathy among patients admitted in a multidisciplinary intensive care unit of a medical college hospital. J Med Sci Health. 2020;6(3):27–30.
12. Kam KYR, Haldar S, Papamichael E, et al. Eye care in the critically ill: a national survey and protocol. J Intensive Care Soc. 2013;14(2):150–154. doi:10.1177/175114371301400213
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
