Back to Journals » Pragmatic and Observational Research » Volume 15
Obesity Paradox in Heart Failure with Mildly Reduced Ejection Fraction
Authors Reinhardt M, Schupp T, Abumayyaleh M, Lau F, Schmitt A, Abel N, Akin M, Rusnak J, Akin I, Behnes M
Received 12 October 2023
Accepted for publication 10 January 2024
Published 5 March 2024 Volume 2024:15 Pages 31—43
DOI https://doi.org/10.2147/POR.S444361
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor David Price
Marielen Reinhardt,1,* Tobias Schupp,1,* Mohammad Abumayyaleh,1 Felix Lau,1,2 Alexander Schmitt,1 Noah Abel,1 Muharrem Akin,2 Jonas Rusnak,3 Ibrahim Akin,1 Michael Behnes1
1Department of Cardiology, Angiology, Haemostaseology and Medical Intensive Care, University Medical Centre Mannheim, Medical Faculty Mannheim, Heidelberg University, Mannheim, Germany; 2Department of Cardiology, Angiology, Hannover Medical School, Hannover, Germany; 3Department of Cardiology, Angiology and Pneumology, University Hospital Heidelberg, Heidelberg, Germany
*These authors contributed equally to this work
Correspondence: Tobias Schupp, First Department of Medicine, University Medical Center Mannheim (UMM), Theodor-Kutzer-Ufer 1-3, Mannheim, 68167, Germany, Tel +49 621-383-2204, Email [email protected]
Objective: The study investigates the prognostic impact of body mass index (BMI) in patients hospitalized with heart failure with mildly reduced ejection fraction (HFmrEF).
Background: Limited data regarding the prognostic impact of BMI in patients with HFmrEF is available.
Methods: Consecutive patients with HFmrEF (ie, left ventricular ejection fraction 41– 49% and signs and/or symptoms of HF) were retrospectively included at one institution from 2016 to 2022. Risk stratification was performed according to WHO-defined BMI groups. The primary endpoint was all-cause mortality at 30 months (median follow-up). Kaplan-Meier, uni- and multivariable Cox proportional regression analyses were applied for statistics.
Results: 1832 consecutive patients with HFmrEF were included with a median BMI of 26.7 kg/m2 (IQR 24.0– 30.8 kg/m2). Patients with lowest BMI (ie, 18.5– 24.9 kg/m2) were associated with highest risk of all-cause mortality at 30 months compared to patients with higher BMI values (40.0% vs 29.0% vs 21.4% vs 20.9%; log rank p = 0.001; HR = 0.721; 95% CI 0.656– 0.793; p = 0.001). Even after multivariable adjustment, higher BMI values were associated with improved survival at 30 months (HR = 0.963; 95% CI 0.943– 0.985; p = 0.001). In contrast, the risk of HF- related rehospitalization at 30 months was not affected by BMI (log rank p = 0.064).
Conclusion: In patients hospitalized with HFmrEF, lower BMI was associated with increased risk of all-cause mortality at 30 months, suggesting an obesity paradox in HFmrEF.
Keywords: heart failure with mildly reduced ejection fraction, HFmrEF, body mass index, BMI, obesity, mortality
Introduction
The incidence of chronic heart failure (HF) has reached a stable level due to improved treatment of primary causes and evidence-based therapies such as the use of invasive cardiac devices and HF-related pharmacotherapies. However the overall prevalence of HF is increasing as a result of the ageing of the general population.1–3 HF affects over 64 million individuals worldwide and is associated with a 5-year mortality rate of 50–75%.1,4 Traditionally, HF has been categorized into two groups based on the left ventricular ejection fraction (LVEF): HF with reduced LVEF (ie, HFrEF) and preserved LVEF (ie, HFpEF). In 2016 and 2021, the ESC HF guidelines have been revised and HF with mildly reduced ejection fraction (ie, HFmrEF), characterized by a LVEF of 41–49%5 was introduced as third and independent category of HF. This category remains largely unexplored, as patients with HFmrEF have been excluded from most heart failure registries and randomized controlled trials (RCT).6–8 Since HFmrEF accounts for 10–25% of all HF patients,9 it is crucial to conduct focused research to understand its underlying characteristics, pathophysiology, treatment, and the prognostic value of comorbidities within this subgroup.10
Obesity has become a worldwide burden reaching pandemic dimensions. According to the World Health Organization (WHO), the prevalence of obesity has nearly tripled in the last four decades and is expected to rise further.11 Obesity is associated with various comorbidities such as type 2 diabetes mellitus, hyperlipidemia, sleep disorders, and hypertension, leading to the development of cardiovascular diseases.12–14 Although obesity was shown to be an independent risk factor for cardiovascular mortality and morbidity, several studies reported that a higher body mass index (BMI) is linked to a better prognosis for various chronic diseases, a phenomenon known as the “obesity paradox”.15–17 Specifically, overweight and obese patients with chronic heart failure have been found to have a lower risk of death compared to those with normal BMI.18 In fact, a U-shaped association was found between the BMI and mortality in patients with chronic HF19,20 and the paradox was observed in patients with HF with preserved ejection fraction (HFpEF) as well as HF with reduced ejection fraction (HFrEF).21–23 While the rates of overweight and obese patients is commonly high in HFpEF, it seems that the obese phenotype is also typically found in patients with HFmrEF, whereas 38% to 76% of patients with HFmrEF were obese in contemporary studies.8,24
The study investigates the prognostic impact of BMI in consecutive patients hospitalized with HFmrEF, aiming to determine whether there is an obesity paradox in patients with HFmrEF.
Methods
Study Patients, Design and Data Collection
For the present study, all consecutive patients hospitalized with HFmrEF at one University Medical Centre were included from January 2016 to December 2022. Using the electronic hospital information system, all relevant clinical data related to the index event were documented, such as baseline characteristics, vital signs on admission, prior medical history, prior medical treatment, length of index hospital and intensive care unit (ICU) stay, laboratory values, data derived from all non-invasive or invasive cardiac diagnostics and device therapies, such as echocardiographic data, coronary angiography and data being derived from prior or newly implanted cardiac devices. The University Medical Centre covers a general emergency department for emergency admission of traumatic, surgical, neurological and cardiovascular conditions. Interdisciplinary consultation is an inbuilt feature of this 24/7 service and connects to a stroke unit, four ICUs with extracorporeal life support and a chest pain unit to alleviate rapid triage of patients. The cardiologic department itself includes a 24-h catheterization laboratory, an electrophysiologic laboratory, a hybrid operating room and telemetry units. Furthermore, the medical centre is a certified HF unit.
The present study derived from the “Heart Failure With Mildly Reduced Ejection Fraction Registry” (HARMER), representing a retrospective single-centre all-comers registry including consecutive patients with HFmrEF hospitalized at the University Medical Centre Mannheim (UMM), Germany (clinicaltrials.gov identifier: NCT05603390). The registry was carried out according to the principles of the declaration of Helsinki and was approved by the medical ethics committee II of the Medical Faculty Mannheim, University of Heidelberg, Germany (ethical approval code: 2022–818). No written informed consent was necessary for the present study.
Inclusion and Exclusion Criteria
All consecutive patients with ≥18 years of age hospitalized with HFmrEF at one institution were included. All included patients underwent at least one standardized transthoracic echocardiography at the cardiologic department at index hospitalization, where the diagnosis of HFmrEF was assessed. The diagnosis of HFmrEF was determined retrospectively according to the “2021 European Society of Cardiology (ESC) guidelines for the diagnosis and treatment of acute and chronic HF”.25 Accordingly, all patients with LVEF 41–49% and symptoms and/or signs of HF were included. The presence of elevated amino-terminal prohormone of brain natriuretic peptide (NT-proBNP) levels and other evidence of structural heart disease were considered to make the diagnosis more likely but were not mandatory for diagnosis of HFmrEF. The presence of right ventricular dysfunction was defined as a tricuspid annular plane systolic excursion (TAPSE) <18 mm. Standardized transthoracic echocardiography was performed by cardiologists during routine clinical care in accordance with current European guidelines.26,27 Finally, all echocardiographic examinations and reports were re-assessed post-hoc by two independent cardiologists blinded to the final data analysis. In cases of ambiguous findings or documentation, echocardiographic source data was re-assessed in individual cases based on the available Digital Imaging and Communications in Medicine (DICOM) files.
For the present study, patients with <18 years of age were excluded. Patients with no evidence on weight and/or hight were excluded. Related to the low proportion of patients with BMI <18.5 kg/m2, these patients were excluded from the present study. No further exclusion criteria were applied for the present study.
Risk Stratification
For the present study, patients were divided into four BMI categories in agreement with the CDC and WHO guidelines as follows: Normal weight was defined as BMI from 18.5 to <25.0 kg/m2. Overweight was defined as BMI from 25.0 to <30.0 kg/m2. Obesity class I was defined as BMI from 30.0 to <35.0 kg/m2. BMI ≥35.0 kg/m2 included patients with obesity classes II and III. Documentation of height and body weight was derived from documented medical records within the electronic hospital information system. Patients with BMI < 18.5 kg/m2 (n = 35) were excluded.
Study Endpoints
The primary endpoint was long-term all-cause mortality. Long-term was defined as the median time of clinical follow-up in months. Secondary endpoints comprised in-hospital all-cause mortality (defined as all-cause mortality during the index hospitalization) and all-cause mortality at 12 months of follow-up. Further secondary endpoints included rehospitalization for worsening HF, cardiac rehospitalization, acute myocardial infarction (AMI), stroke, coronary revascularization, and major adverse cardiac and cerebrovascular events (MACCE) at long term follow-up. All-cause mortality was documented using the electronic hospital information system and by directly contacting state resident registration offices (“Bureau of Mortality Statistics”). Identification of patients was verified by place of name, surname, date of birth, and registered living address. HF-related hospitalization was defined as a rehospitalization due to worsening HF requiring intravenous diuretic therapy. HF-related rehospitalization comprised patients with hospitalization due to worsening HF as the primary cause or as a result of another cause but associated with worsening HF at the time of admission, or as a result of another cause but complicated by worsening HF during its cause. Cardiac rehospitalization was defined as rehospitalization due to a primary cardiac condition, including worsening HF, AMI, coronary revascularization and symptomatic atrial or ventricular arrhythmias. MACCE was defined as the composite of all-cause mortality, coronary re-vascularization, non-fatal AMI and non-fatal stroke.
Statistical Methods
Quantitative-data is presented as mean ± standard error of mean (SEM), median and interquartile range (IQR), and ranges depending on the distribution of the data. They were compared using the Student’s t-test for normally distributed data or the Mann–Whitney U-test for non-parametric data. Deviations from a Gaussian distribution were tested by the Kolmogorov–Smirnov test. Qualitative data is presented as absolute and relative frequencies and were compared using the chi-square test or the Fisher’s exact test, as appropriate.
Kaplan–Meier analyses were performed stratified by BMI and univariable hazard ratios (HRs) were given together with 95% confidence intervals (Cis). The prognostic impact of BMI was then investigated within multivariable Cox regression models using the “forward selection” option.
Results of all statistical tests were considered significant for p ≤ 0.05. SPSS (Version 28, IBM, Armonk, New York) was used for statistics.
Results
Study Population
A total of 2228 patients with HFmrEF were hospitalized at our institution from 2016 to 2022. 1.97% (n = 44) with incomplete follow-up data, 14.2% (n = 317) with missing data on weight and/or height and 1.57% (n = 35) with BMI <18.5 kg/m2 were excluded (Figure 1; Flow Chart). The final study comprised 1832 patients hospitalized with HFmrEF with a median BMI of 26.7 kg/m2 (mean 27.7 kg/m2; IQR 24.0–30.8 kg/m2).
 |
Figure 1 Flow chart of the study population. |
When stratified by different BMI categories, patients with BMI 18.5 - <25 kg/m2 were older (median age 78 vs 77 vs 72 vs 68 years; p = 0.001), presented with higher rates of peripheral artery disease (14.9% vs 11.1% vs 8.5% vs 8.5%; p = 0.008) and malignancies (19.9% vs 13.5% vs 12.1% vs 11.4%; p = 0.001) (Table 1). In contrast, patients with the highest BMI (ie, BMI ≥ 35 kg/m2) presented with higher rates of cardiovascular risk factors, such as arterial hypertension (87.1% vs 82.5% vs 77.4% vs 72.2%; p = 0.001) and diabetes mellitus (55.2% vs 47.7% vs 35.9% vs 24.4%; p = 0.001). The highest rate of pre-existent coronary artery disease (CAD) was shown in patients with BMI 30 - <35 kg/m2 (47.9%; p = 0.016). In contrast, the rates of pre-existent congestive HF (35.1% vs 32.0% vs 33.4% vs 37.8%; p = 0.403) and the proportion of patients with HF-related hospitalization within the last 12 months (10.3% vs 8.9% vs 11.0% vs 14.9%; p = 0.106) did not significantly differ across the BMI groups. With regard to comorbidities at index hospitalization, patients with BMI ≥ 35 kg/m2 had higher rates of acute decompensated heart failure (29.4%; p = 0.007). The rates of ST-segment AMI (STEMI) (7.7% vs 9.5% vs 9.3% vs 7.0; p = 0.511) and non-ST-segment AMI (NSTEMI) (11.4% vs 13.1% vs 14.0% vs 11.4%; p = 0.624) did not differ significantly across the BMI groups.
 |
Table 1 Baseline Characteristics |
As outlined in Table 2, the most common aetiology of HF across all groups was ischemic cardiomyopathy (BMI 18.5 – <25 kg/m2, 53.2%; BMI 25 - <30 kg/m2, 60.8%; BMI 30 - <35 kg/m2, 64.9%; BMI ≥ 35 kg/m2, 54.7%; p = 0.002). Compared to patients with BMI 18.5 - <25 kg/m2, patients with BMI ≥ 35 kg/m2 showed higher values of interventricular septal end diastole (IVSd) (12 vs 11 mm; p = 0.001), left ventricular end-diastolic diameter (LVEDD) (52 vs 47 mm; p = 0.001) and TAPSE (21 vs 20 mm; p = 0.001). On the contrary, the rates of valvular heart diseases, including moderate-to-severe aortic valve regurgitation (6.9% vs 2.5%; p = 0.001), moderate-to-severe mitral regurgitation (16.7% vs 6.0%; p = 0.001) and moderate-to-severe tricuspid regurgitation (22.8% vs 8.0%) were higher in patients with BMI 18.5 - <25 kg/m2 compared to patients with BMI ≥ 35 kg/m2. A higher proportion of patients with BMI 30 - <35 kg/m2 underwent invasive coronary angiography during index hospitalization compared to patients with the lowest BMI (47.1% vs 33.5%; p = 0.001). However, no significant difference was found in the distribution of CAD type or percutaneous coronary intervention (PCI) rates across the BMI categories (p = 0.271 and p = 0.180 respectively). Levels of NT-pro-BNP were significantly higher in patients with lowest BMI compared to patients with BMI ≥ 35 kg/m2 (3874 vs 1602 pg/mL; p = 0.001).
 |
Table 2 Heart-Failure Related and Procedural Data |
Finally, patients with BMI ≥ 35 kg/m2 were more frequently discharged with an angiotensin receptor blocker (ARB) (28.9% vs 20.1%; p = 0.016), sodium-glucose cotransporter 2 (SGLT2) inhibitor (11.9% vs 1.9%; p = 0.001) or loop diuretics (57.7% vs 46.8%; p = 0.032) compared to patients with BMI 18.5 - <25 kg/m2.
Prognostic Impact of BMI in Patients with HFmrEF
During a median follow-up of 30 months (IQR 390–1634 days), the primary endpoint all-cause mortality occurred in 40.0% of patients with BMI 18.5 - <25 kg/m2, 29.0% of patients with BMI 25 - <30 kg/m2, 21.4% of patients with BMI 30 - <35 kg/m2, and 20.9% of patients with BMI ≥ 35 kg/m2 (p = 0.001) (Figure 2). Accordingly, a higher BMI was associated with a lower risk of 30-months all-cause mortality (HR = 0.721; 95% CI 0.656–0.793; p = 0.001). The risk of HF-related rehospitalization at 30 months did not differ across the BMI groups (12.9% vs 12.7% vs 15.0% vs 18.0%; log rank p = 0.219; HR = 1.116; 95% CI 0.983–1.268; p = 0.093).
 |
Figure 2 Kaplan-Meier analyses comparing the prognostic impact of BMI on the risk of all-cause mortality (left panel) and hospitalization for worsening HF (right panel) in patients with HFmrEF. |
Regarding key secondary endpoints, the rates of coronary revascularization were higher in patients with BMI 30 - <35 kg/m2 compared to patients with BMI 18.5 - <25 kg/m2 (10% vs 4.9%; log rank p = 0.032; HR = 1.200; 95% CI 1.007–1.430; p = 0.041) (Table 3), whereas the rates of MACCE were higher in patients with BMI 18.5 - <25 kg/m2 compared to patients with BMI ≥ 35 kg/m2 (44.8% vs 29.9%; log rank p = 0.001; HR = 0.818; 95% CI 0.754–0.887; p = 0.001).
 |
Table 3 Follow-Up Data, Primary and Secondary Endpoints |
After multivariable adjustment for patients’ characteristics and comorbidities, higher BMI was associated with lower risk of 30-months all-cause mortality as compared to lower BMI values (HR = 0.963; 95% CI 0.943–0.985; p = 0.001) (Table 4). Furthermore, higher age (HR = 1.050; 95% CI 1.039–1.060; p = 0.001), male sex (HR = 1.347; 95% CI 1.098–1.652; p = 0.004), the presence of diabetes mellitus (HR = 1.243; 95% CI 1.015–1.522; p = 0.035), pre-existent malignancy (HR = 3.045; 95% CI 2.472–3.751; p = 0.001) and acute decompensated HF (HR = 1.994; 95% CI 1.629–2.442; p = 0.001) increased the risk of 30-months all-cause mortality, whereas the presence of hyperlipidaemia (HR = 0.702; 95% CI 0.561–0.880; p = 0.002) and ischemic cardiomyopathy (HR = 0.783; 95% CI 0.645–0.951; p = 0.014) were associated with lower risk of 30-months all-cause mortality.
 |
Table 4 Multivariable Cox Regression Analyses with Regard to All-Cause Mortality and Heart-Failure Related Rehospitalization at 30 Months |
Even when stratified by important pre-selected subgroups, higher BMI levels were associated with lower risk of all-cause mortality in patients >75 years of age (HR = 0.961; 95% CI 0.934–0.988; p = 0.005), males (HR = 0.955; 95% CI 0.927–0.984; p = 0.003) and patients NYHA functional class ≤2 (HR = 0.953; 95% CI 0.925–0.982; p = 0.001) and TAPSE ≥18 mm (HR = 0.967; 95% CI 0.942–0.993; p = 0.014) (Table 5). In contrast, the risk of rehospitalization for worsening HF at 30 months was higher in patients with higher BMIs and NYHA functional class ≤2 (HR 1.044; 95% CI 1.005–1.084; p = 0.027).
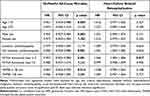 |
Table 5 Hazard Ratios for BMI Within Pre-Specified Subgroups After Multivariable Adjustment |
Discussion
The present study investigates the prognostic impact of BMI in patients hospitalized with HFmrEF using a large registry-based dataset from 2016 to 2022. The data suggests that more than two-thirds (69%) of patients with HFmrEF were overweight or obese. A higher BMI was independently associated with a lower risk of all-cause mortality at 30 months, which was still evident after multivariable Cox regression analyses, suggesting an obesity paradox in patients hospitalized with HFmrEF. Specifically, in older patients and in males, a higher BMI was associated with a lower risk of all-cause death. In contrast, the risk of HF-related rehospitalization was not affected by BMI.
The high metabolic activity of excessive fat tissue and lipotoxicity in obese patients leads to myocardial remodeling and diastolic dysfunction, which may contribute to the development and progression of congestive HF.28 Although epidemiologic data suggest a strong link between obesity and HF, even after adjustment for demographics and commonly prevalent risk factors such diabetes mellitus, hypertension, and hypercholesterolemia, many studies have suggested that patients with higher BMI levels generally had a better prognosis.29,30 The underlying causes of this phenomenon called obesity paradox are still unclear, however several potential explanations exist. From this perspective, obese patients may cope better with the chronic catabolic state of HF due to higher metabolic reserves and attenuated neurohormonal response to stress.15,29,31 Increased production of leptin and soluble receptor of tumor necrosis factor in adipose tissues may reduce the effect of the proinflammatory cytokine.31 Furthermore, obese patients show an attenuated sympathetic nervous system and renin–angiotensin response leading to higher systolic blood pressure, which results in a better prognosis for HF and may permit a higher titration of cardioprotective medication.32 In addition, a positive correlation between higher cholesterol levels and improved survival in HF has been observed.32 Obesity also influences circulating NT-proBNP levels, whereas obese HF patients showed significantly lower levels.33 This phenomenon was observed within the present study including patients with HFmrEF. Finally, patients with higher BMI may manifest symptoms of HF at a younger age with consequent longer survival after diagnosis (lead-time bias),31 however, within the present study, the rates of prior congestive HF and the proportion of patients with hospitalization for acute decompensated HF <12 months did not differ among patients with different BMI categories.
Several studies reported the existence of the obesity paradox in HFrEF and HFpEF, underlying the non-linear relation between BMI and mortality, but data regarding the prognostic impact of BMI in patients with HFmrEF is limited.31,34,35 According to Kenchaiah et al, obesity has a high prevalence in patients with HF, regardless of LVEF,31 which was in line with the present study, demonstrating a prevalence of overweight and obesity of 69%. The examination of patients from the CHARM program showed that lower BMI values were associated with increased risk of cardiovascular and non-cardiovascular death, whereas the risk of hospitalization for worsening of heart failure or due to all causes was not affected by baseline BMI.31 Zhang et al suggested an inverse association between BMI and all-cause mortality in patients with HFpEF based on a systematic review including 59,263 patients; the meta-analysis showed a U-shaped association with the lowest mortality at a BMI of 32–33 kg/m2.35 Similar results were found when examining studies of patients with HFrEF, whereas the meta-analysis showed a flatter U-shaped association than for HFpEF with the lowest mortality at a BMI of 32 kg/m2.35 According to the U-shaped association, it was shown that BMI <18.5 kg/m2 is associated with a high risk of mortality, whereas very underweight patients with HF had a higher risk than obese patients.36 This effect was not investigated in our study, due to the low proportion of underweight patients (0.02%) with HFmrEF. It should be noted that the proportion of patients with BMI <18.5 kg/m2 is generally very low in most HFmrEF registries.8
While recent studies showed a strong association of higher BMI with the risk for HFpEF more than for HFrEF, little is known about the prognostic value of BMI in HFmrEF.37 Within the CHARM Program, the BMI of patients with HFmrEF was intermediate betweenHFrEF and HFpEF, while in the TOPCAT, PARAGON-HF and DELIVER trials the BMI of the HFmrEF group resembled more the BMI of the HFpEF group.8,9,31,38 Liu et al demonstrated that obesity increased the 1-year risk for cardiovascular death in female patients with HFmrEF but not in male patients.13 In line with this, our study found a lower risk of all-cause mortality at 30 months in obese male patients compared to females. Furthermore, Liu et al showed that obesity had a 57% overall increased risk of cardiovascular death.13 This was not confirmed in the study based on the DELIVER-Trial, where the risks of all-cause mortality and cardiovascular death were significantly higher in patients with lower BMI.37 Regardless of the obesity paradox, obesity remains a relevant risk factor for heart failure and must not be attributed to a protective effect. Studies should focus on more obesity parameters such as fat distribution and waist-to-hip ratio and consider cardiorespiratory fitness as a modulating factor. While extreme obesity is linked to a negative outcome, it is still unclear how weight loss influences the prognosis of HF and requires further investigation.
Study Limitations
The study has several limitations. Due to the retrospective and single-centre study design, results may be influenced by measured and unmeasured confounding. Related to the retrospective study design, data concerning weight changes after index hospitalization was not available. In line, increased mortality in patients with lower BMI may be attributed to an older age, higher incidence of comorbidities (ie, aortic valve disease, anemia), although this was adjusted within multivariable Cox regression analyses. Furthermore, only BMI was used as a parameter for obesity, without taking into account other valid obesity parameters such as fat distribution and body composition and does not provide information on the nutritional status of patients. HF-related and cardiac rehospitalization were assessed at our institution only. Finally, causes of death beyond during index hospitalization were not available for the present study.
Conclusions
The present study found that most HFmrEF patients are overweight and obese. A lower BMI was associated with an increased risk of all-cause mortality at 30 months, which was still evident after multivariable Cox regression analyses, suggesting an obesity paradox in HFmrEF. This may be further attributed to a higher age and an increased burden with cardiovascular comorbidities in patients with lower BMI.
Data Sharing Statement
The dataset used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Funding
This manuscript did not receive any funding.
Disclosure
The authors declare that they do not have any conflicts of interest for this work.
References
1. Savarese G, Becher PM, Lund LH, et al. Global burden of heart failure: a comprehensive and updated review of epidemiology. Cardiovasc Res. 2023;118(17):3272–3287. doi:10.1093/cvr/cvac013
2. James SL, Abate D, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–1858. doi:10.1016/S0140-6736(18)32279-7
3. Conrad N, Judge A, Tran J, et al. Temporal trends and patterns in heart failure incidence: a population-based study of 4 million individuals. Lancet. 2018;391(10120):572–580. doi:10.1016/S0140-6736(17)32520-5
4. Shah KS, Xu H, Matsouaka RA, et al. Heart failure with preserved, borderline, and reduced ejection fraction: 5-year outcomes. J Am Coll Cardiol. 2017;70(20):2476–2486. doi:10.1016/j.jacc.2017.08.074
5. Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016;18(8):891–975. doi:10.1002/ejhf.592
6. Carbone S, daSilva-deAbreu A, Lavie CJ. The sodium-glucose co-transporter 2 inhibitor dapagliflozin improves prognosis in systolic heart failure independent of the obesity paradox. Eur J Heart Fail. 2021;23(10):1673–1676. doi:10.1002/ejhf.2336
7. Thorvaldsen T, Ferrannini G, Mellbin L, et al. Eligibility for dapagliflozin and empagliflozin in a real-world heart failure population. J Card Fail. 2022;28(7):1050–1062. doi:10.1016/j.cardfail.2022.04.011
8. Solomon SD, Vaduganathan M, Claggett BL, et al. Baseline characteristics of patients with hf with mildly reduced and preserved ejection fraction: DELIVER trial. JACC Heart Fail. 2022;10(3):184–197. doi:10.1016/j.jchf.2021.11.006
9. Savarese G, Stolfo D, Sinagra G, et al. Heart failure with mid-range or mildly reduced ejection fraction. Nat Rev Cardiol. 2022;19(2):100–116. doi:10.1038/s41569-021-00605-5
10. McDonagh TA, McDonagh TA, Metra M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2022;24(1):4–131. doi:10.1002/ejhf.2333
11. Boutari C, Mantzoros CS. A 2022 update on the epidemiology of obesity and a call to action: as its twin COVID-19 pandemic appears to be receding, the obesity and dysmetabolism pandemic continues to rage on. Metabolism. 2022;133:155217. doi:10.1016/j.metabol.2022.155217
12. Powell-Wiley TM, Poirier P, Burke LE, et al. Obesity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2021;143(21):e984–e1010. doi:10.1161/CIR.0000000000000973
13. Liu Z, Peng Y, Zhao W, et al. Obesity increases cardiovascular mortality in patients with HFmrEF. Front Cardiovasc Med. 2022;9:967780. doi:10.3389/fcvm.2022.967780
14. Benn M, Marott SCW, Tybjærg-Hansen A, et al. Obesity increases heart failure incidence and mortality: observational and Mendelian randomization studies totalling over 1 million individuals. Cardiovasc Res. 2023;118(18):3576–3585. doi:10.1093/cvr/cvab368
15. Simati S, Kokkinos A, Dalamaga M, et al. Obesity Paradox: fact or Fiction? Curr Obes Rep. 2023;12(2):75–85. doi:10.1007/s13679-023-00497-1
16. Tutor AW, Lavie CJ, Kachur S, Milani RV, Ventura HO. Updates on obesity and the obesity paradox in cardiovascular diseases. Prog Cardiovasc Dis. 2022;78:2–10.
17. Zeng S, Cai X, Zheng Y, et al. Associations of body mass index with mortality in heart failure with preserved ejection fraction patients with ischemic versus non-ischemic etiology. Front Cardiovasc Med. 2022;9:966745. doi:10.3389/fcvm.2022.966745
18. Kim SE, Lee CJ. The paradox in defining obesity in patients with heart failure. Int J Heart Fail. 2022;4(2):91–94. doi:10.36628/ijhf.2022.0010
19. Giri Ravindran S, Saha D, Iqbal I, et al. The obesity paradox in chronic heart disease and chronic obstructive pulmonary disease. Cureus. 2022;14(6):e25674. doi:10.7759/cureus.25674
20. Li S, Zheng Y, Huang Y, et al. Association of body mass index and prognosis in patients with HFpEF: a dose-response meta-analysis. Int J Cardiol. 2022;361:40–46. doi:10.1016/j.ijcard.2022.05.018
21. Dong B, Yao Y, Xue R, et al. Distinct implications of body mass index in different subgroups of nonobese patients with heart failure with preserved ejection fraction: a latent class analysis of data from the TOPCAT trial. BMC Med. 2022;20(1):423. doi:10.1186/s12916-022-02626-4
22. Tadic M, Cuspidi C. Obesity and heart failure with preserved ejection fraction: a paradox or something else? Heart Fail Rev. 2019;24(3):379–385. doi:10.1007/s10741-018-09766-x
23. Alrob OA, Sankaralingam S, Alazzam S, et al. Obesity paradox among heart failure with reduced ejection fraction patients: a retrospective cohort study. Medicina. 2022;59(1):60. doi:10.3390/medicina59010060
24. Wenzel JP, Nikorowitsch J, Bei der Kellen R, et al. Heart failure in the general population and impact of the 2021 European Society of Cardiology Heart Failure Guidelines. ESC Heart Fail. 2022;9(4):2157–2169. doi:10.1002/ehf2.13948
25. McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2021;42(36):3599–3726. doi:10.1093/eurheartj/ehab368
26. Popescu BA, Andrade MJ, Badano LP, et al. European Association of Echocardiography recommendations for training, competence, and quality improvement in echocardiography. Eur J Echocardiograp. 2009;10(8):893–905. doi:10.1093/ejechocard/jep151
27. Lancellotti P, Tribouilloy C, Hagendorff A, et al. Recommendations for the echocardiographic assessment of native valvular regurgitation: an executive summary from the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2013;14(7):611–644. doi:10.1093/ehjci/jet105
28. Badimon L, Bugiardini R, Cenko E, et al. Position paper of the European Society of Cardiology-working group of coronary pathophysiology and microcirculation: obesity and heart disease. Eur Heart J. 2017;38(25):1951–1958. doi:10.1093/eurheartj/ehx181
29. Lavie CJ, Milani RV, Ventura HO. Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. J Am Coll Cardiol. 2009;53(21):1925–1932. doi:10.1016/j.jacc.2008.12.068
30. Horwich TB, Fonarow GC, Clark AL. Obesity and the Obesity Paradox in Heart Failure. Prog Cardiovasc Dis. 2018;61(2):151–156. doi:10.1016/j.pcad.2018.05.005
31. Kenchaiah S, Pocock SJ, Wang D, et al. Body mass index and prognosis in patients with chronic heart failure: insights from the Candesartan in Heart failure: assessment of Reduction in Mortality and morbidity (CHARM) program. Circulation. 2007;116(6):627–636. doi:10.1161/CIRCULATIONAHA.106.679779
32. Oreopoulos A, Padwal R, Kalantar-Zadeh K, et al. Body mass index and mortality in heart failure: a meta-analysis. Am Heart J. 2008;156(1):13–22. doi:10.1016/j.ahj.2008.02.014
33. Madamanchi C, Alhosaini H, Sumida A, et al. Obesity and natriuretic peptides, BNP and NT-proBNP: mechanisms and diagnostic implications for heart failure. Int J Cardiol. 2014;176(3):611–617. doi:10.1016/j.ijcard.2014.08.007
34. Padwal R, McAlister FA, McMurray JJV, et al. The obesity paradox in heart failure patients with preserved versus reduced ejection fraction: a meta-analysis of individual patient data. Int J Obes. 2014;38(8):1110–1114. doi:10.1038/ijo.2013.203
35. Zhang J, Begley A, Jackson R, et al. Body mass index and all-cause mortality in heart failure patients with normal and reduced ventricular ejection fraction: a dose-response meta-analysis. Clin Res Cardiol. 2019;108(2):119–132. doi:10.1007/s00392-018-1302-7
36. Milajerdi A, Djafarian K, Shab‐Bidar S, et al. Pre- and post-diagnosis body mass index and heart failure mortality: a dose-response meta-analysis of observational studies reveals greater risk of being underweight than being overweight. Obes Rev. 2018;20(2):252–261. doi:10.1111/obr.12777
37. Adamson C, Kondo T, Jhund PS, et al. Dapagliflozin for heart failure according to body mass index: the DELIVER trial. Eur Heart J. 2022;43(41):4406–4417. doi:10.1093/eurheartj/ehac481
38. Pitt B, Pfeffer MA, Assmann SF, et al. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med. 2014;370(15):1383–1392. doi:10.1056/NEJMoa1313731
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
