Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 15
Non-Disclosure of HIV-Positive Serostatus: Unmatched Case–Control Study in People Living with HIV in Public Health Facilities of Gedeo Zone, Southern Ethiopia
Authors Tessema BT, Bune GT, Mamo ZB
Received 29 January 2023
Accepted for publication 25 May 2023
Published 9 June 2023 Volume 2023:15 Pages 313—324
DOI https://doi.org/10.2147/HIV.S405818
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Olubunmi Akindele Ogunrin
Betelhem Tadesse Tessema,1,* Girma Tenkolu Bune,2,* Zerihun Berhanu Mamo1,*
1Reproductive Health, School of Public Health, College of Health Science and Medicine, Dilla University, Dilla, Ethiopia; 2School of Public Health, College of Health Science and Medicine, Dilla University, Dilla, Ethiopia
*These authors contributed equally to this work
Correspondence: Girma Tenkolu Bune, Tel +251911356214, Email [email protected]; [email protected]
Background: Non-disclosure of HIV-positive status (NDHPSS) is the individual’s experience of hiding their HIV status from other people or groups. People who fail to reveal their HIV-positive serostatus risk contracting the virus again, not receiving the best possible care, and even dying.
Purpose: To assess predictors of NDHPSS in people living with HIV in public health facilities in Gedeo-Zone, Southern-Ethiopia.
Methods: In Gedeo-Zone, Southern Ethiopia, a facility-based, unmatched, case–control study was carried out from the first of February to March 30, 2022GC. With a case-to-control ratio of 1:1, a total of 360 respondents (89 cases and 271 controls) were involved. The respondents were chosen using a sequential sampling technique. EpiData-V-3.1 was used to enter the data, and SPSS-V-25 was used to analyse it. To determine the factors that were connected to the result, a binary logistic regression analysis was performed. AOR at the 95% confidence interval and p-values under 0.05 were utilised to explain their statistical significance.
Results: The study had 360 participants in total— 271 controls and 89 cases—resulting in a response rate of 97.6%. The average age of the participants was 35.6 years (SD: 8.3). After adjusting the possible confounders, sex (AOR = 2.8, 95% CI: 1.04– 7.56), residence (AORs = 3.52, 95% CI: 2.83– 9.39), WHO clinical stage I (AORs = 4.68, 95% CI: 1.9– 22.1), short duration of ART follow-up care (AOR = 4.21, 95% CI: 1.65– 10.73), and number of lifetime sexual partners (AOR = 6.9, 95% CI: 1.86– 26.3) were significantly associated factors with the outcome.
Conclusion: According to this study, living in a rural area and being in WHO clinical stage one, in addition to being a woman and having multiple sexual partners during one’s lifetime, were predictors of non-disclosure of an HIV-positive serostatus. As a result, encouraging people with HIV in WHO stage I and those who have had more than one sexual partner in their lifetime to disclose their status and expanding counselling services for rural residents and women have a substantial impact on reducing the HIV load.
Keywords: non-disclosure, NDHPSS, determinants, Gedeo-Zone, Southern-Ethiopia, HIV-positive serostatus
Introduction
HIV/AIDS affects 37.6 million people globally, endangering public health on a large scale.1 The treatment of those who are already ill and the prevention of new infections are essential to the prevention and control of HIV infection.2 One of the most crucial actions in avoiding and controlling HIV growth, according to the Centres for Disease Control (CDC) and World Health Organization (WHO),3,4 is revealing an HIV positive serostatus to a sexual partner and other family members.
Disclosure of HIV status, or revealing one’s HIV-positive diagnosis to others, is a complex and multifaceted issue that is influenced by various factors.3,5,6 Experts generally recommend disclosure as a key strategy for reducing stigma, improving access to care and support, and promoting positive health outcomes for people living with HIV.1 However, HIV-positive individuals who conceal their HIV positive status often experience stigma, drug use, social marginalisation, and self-blame.7,8 Non-disclosure of HIV serostatus (NDHSS) raises the risk of HIV infection for intimate partners, kids, and members of the same close family. Furthermore, hiding an HIV-positive spouse’s serostatus increases the risk of mother-to-child transmission of AIDS.1
Global studies have shown that HIV serostatus disclosure is predicted by pre- and post-test counselling, WHO stage, viral load, partner’s HIV status, number of lifelong sexual partners, membership in an HIV support group, marital status, age, gender, known stigma and discrimination, and intimate partner violence.1 Prevalence of HIV serostatus disclosure ranges from 16.7% to 100%.2,9 In developed countries, an average of 71%+ (42–100%), compared to 52%+ (16.7–86%) in developing countries.2,10 In Thailand, disclosure of HIV serostatus to partners varies from 26% to 95% depending on whether they have sex with other men or pregnant HIV-positive women.10
In Sub-Saharan Africa (SSA), HIV is a major public health challenge, with an estimated 20.6 million people living with HIV in the region.1 HIV disclosure in SSA ranges from 16.7% to 86%. Despite the significant efforts made in the region to combat the epidemic, stigma and discrimination remain major barriers to HIV testing, treatment, and care.11
Ethiopia is one of the SSA countries that has made notable progress in the HIV response, with HIV prevalence estimated at 0.9%, with 690,000 people living with the virus.12–14 The Ethiopian Ministry of Health emphasizes the importance of swiftly informing intimate partners and close contacts about HIV-positive serostatus in order to lower viral load and reach zero new HIV infections by 2030.15 However, HIV disclosure in Ethiopia is reported to be between 51.7% and 89.7%, which may be due to stigma and discrimination in rural areas.16
The Southern Nations, Nationalities, and Peoples’ Region (SNNPR) is one of the regional states in Ethiopia and has a high prevalence of HIV, with an estimated adult prevalence of 2.5%. The Gedeo Zone is located in SNNPR and has an estimated HIV prevalence of 2.1%.14 In the SNNPR of Ethiopia, the magnitude of HIV serostatus disclosure is unknown. However, evidences revealed that HIV disclosure in SNNPR is influenced by cultural norms and beliefs, fear of discrimination, and concerns related to confidentiality and privacy. Additionally, HIV-disclosure extents in the Gedeo Zone are not largely known. This zone has a predominantly rural population, with limited access to healthcare services, which can also affect HIV disclosure and access to care.17
Therefore, this study aimed to predict the factors which contributed to the non-disclosure of HIV Serostatus in People Living with HIV in Public Health Facilities of Gedeo Zone, Southern Ethiopia. Understanding the predictors of HIV disclosure can help researchers and policymakers develop effective interventions to reduce HIV transmission and improve the quality of life for people living with HIV.
Materials and Methods
Study Area, Period, and Design
Gedeo-Zone public health facilities are where the study was carried out. The Gedeo Zone is located in Ethiopia’s Southern Nations, Nationalities, and Peoples’ Region (SNNPR), bordered to the north and east by Oromia Region, to the west by Sidama Region, and to the south by Guji Zone. It has 1.3 million inhabitants and a land area of 5861 square kilometers. It is distinguished by its high hills, valleys, and rugged landscape. Agriculture and trade are the primary economic activities in the zone, with coffee production being a key source of wealth. The Gedeo people are largely Christian, with the Ethiopian Orthodox Church constituting the majority of the population. Despite its economic potential, the zone suffers from socioeconomic obstacles such as poverty, low education levels, and limited access to healthcare services, as well as environmental issues such as deforestation.
The epidemiological situation of Gedeo Zone, Southern Ethiopia, regarding HIV/AIDS and HIV serostatus disclosure is largely unknown. However, according to the Southern Nations, Nationalities and Peoples’ Regional Health Bureau, there are several public institutions in Gedeo Zone that provide HIV prevention and awareness campaigns, including the Gedeo Zone Health Office, the Gedeo Zone Health Bureau, and the Gedeo Zone Health Department. As this report revealed, there are a total of 15 health centers and 2 hospitals in Gedeo Zone that provide HIV/AIDS care and treatment services. These facilities provide services such as HIV testing, counseling, antiretroviral therapy (ART), and management of opportunistic infections. According to the 2019 UNAIDS Report, in Gedeo Zone, Southern Region of Ethiopia, the HIV prevalence among adults aged 15–49 was estimated to be 0.3% in 2019.18 A facility-based unmatched case–control research was conducted from February 1 to March 30, 2022.
Sample Size Determination
When estimating the sample size for an unmatched case–control research with OpenEpi303 statistical software, which is part of the OpenEpi software package, the following assumptions were taken. Using a 5% threshold of significance, a power of 80% at a 95% confidence interval, and a factoring in 2.8 OR of not having a stable partner,18 a total of 334 samples are obtained. After accounting for a 10% nonresponse rate, the total sample size was 367, which comprised 275 controls and 92 cases.
Sampling Technique and Procedure
Gedeo Zone has eight health institutions that offer ART (4 hospitals and four health centers). Using a simple random selection approach, two hospitals and two healthcare centers were chosen from among these institutions, and the sample size was allotted proportionately to the number of patients they had. Respondents were chosen using a process known as sequential sampling. All affirmative instances and their associated controls, which arrived one after the other, were documented at each institution until all cases and controls were closed. As a result, when HIV-positive patients arrived for their appointment, they were recruited in the trial in a 1:3 case–control ratio.
Population
Source Population
All confirmed HIV positive patients attending ART clinics of public health institutions in Gedeo Zone, southern Ethiopia.
Study Population
Case: HIV-infected patients who did not reveal their serostatus to anybody, attended the Gedeo Zone Health Facility’s selected ART clinics throughout the research period, and satisfied the eligibility requirements stated for the study case. Control: HIV-infected patients who reported their serostatus to their sexual partner or one of their close contacts or family members who attended the Gedeo Zone Health Facility’s designated ART clinics throughout the study period and satisfied the study control eligibility requirements.
Eligibility Criteria
Inclusion Criteria
Case: aged 18 and above, taking ART for at least one month throughout the data collection period, and who did not reveal their HIV status.
Control: Age 18+, on ART for at least one month throughout the data collection period, and who revealed their HIV status.
Exclusion Criteria
Case and Controls
Patients who were newly HIV positive and entered the ART clinic for the first time, patients who had tested positive in a pair, and persons who were critically unwell were excluded from the study.
Operational Definitions
Non-Disclosure
In this study, non-disclosure refers to HIV seropositive persons who did not reveal their HIV sero status to anybody else. It was assessed by asking yes/no questions. This was determined by asking individuals if they had told at least one person about their serostatus. Responses were classified as “yes” or “no”, with 1 for “yes” and 2 for “no”. HIV-related stigma and discrimination refer to prejudice, unfavorable attitudes, and abuse aimed against persons living with HIV/AIDS after their diagnosis. Partner violence is defined as physical and/or sexual assault or threats of physical and/or sexual assault between married, romantically engaged partners, or former partners following HIV positive serostatus disclosure. The concept of blame refers to being held accountable for another person’s HIV-positive status. Confidentiality violation: the revealing of HIV sero positive status to someone without the owner’s authorization. In other words, failing to respect a person’s privacy or the trust with which they provided the information to the other person by passing it on to someone else.
Data Collection Procedure
Data Collection Instrument
The data was collected using structured, standardized questions delivered by the interviewer and a record review checklist (for some health-related factors). The instruments were modified and created from various literature utilized in various investigations done both in and outside of Ethiopia.
Data Collectors and Supervisors
Four case managers who have had ART adherence counseling training, have a history of HIV seropositivity, and are proficient in Gedeoffa and Amharic were chosen and underwent two days of training on data collection methodologies and instruments. A BSC nurse was also recruited from another working unit for supervision.
Data Quality Management
The questionnaire was written in English, translated into Amharic and Gedeoffa, and then translated back into English by a third person to assure accuracy. The questionnaire was pre-tested on 5% of the Dilla Health Center sample of ART patients, which differed from the actual data collection sites, prior to data collection. As a consequence of the pre-test results, certain questions have been modified. The data collector and supervisor were taught for two days about the equipment and data collection practices. Through supervision and several same-day reviews of the gathered material, the investigators frequently checked the data collection procedure for consistency and completeness.
Data Process and Analysis
Data was entered into the EPI-data version 3.1 program and exported to the SPSS version 25.0 Windows program for additional analysis. The data was cleaned and coded, and it was checked for errors and missing values. The frequency, mean, and standard deviation of the variables were calculated using descriptive statistics. The crude association between the independent variables and the dependent variables was ascertained using binary logistic regression. Variables with P 0.25 in the bivariate analysis were candidates for the multivariate logistic regression models to reduce the impact of confounders. The results were finally presented using crude odds ratios (COR), adjusted odds ratios (AOR), and confidence intervals (95% CI), with a P value of 0.05 being taken as a level of significance for those factors in the multivariate analysis that were statistically significant.
Ethical Consideration
To address the ethical implications of human-initiated research, all ethical norms and principles from the Helsinki Declaration have been taken into account. As a result, the plan was presented to the Dilla University College of Health Science Institutional Review Board (IRB) for ethical approval, and the board approved it and gave an officially written letter of permission. This written approval letter was then presented to the Gedeo Zone Health Department, and another comparable letter was produced and submitted to all designated health institutions to undertake the research. Prior to gathering information from research participants, each respondent provided written consent and was asked if they were willing to participate in the study. The right of participants to decline or interrupt the interview was protected, and the information supplied by each interviewee was kept private. Interviews were done with just the interviewer present to ensure their privacy and confidentiality, and the interviewee and participants were recognized by an identifying number, and the data was utilized solely for the stated purpose.
Results
Socio-Demographic Characteristics of Respondents
A total of 360 (89 cases and 271 controls) subjects were included in the present study, resulting in a response rate of 97.6% (96.7% for cases and 98.5% for controls). The mean age of the participants was 35.6 years (SD 8.3) (34.5 9.2 years for cases and 36.5 8.05 years for controls). Almost a third (76.4%) of the cases were rural residents, while the majority of controls 198 (73.1%) were urban residents. Fifty-nine (30.3%) of the cases and 116 (42.8%) of the controls were female by their sex (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Respondent Among HIV Infected Patients Attending in ART Clinics of Public Health Facilities, in Gedeo Zone, Southern Ethiopia, 2022 |
Health Related Characteristics of Respondent
Approximately 37% of respondents (33 cases and 60 controls) were in the World Health Organization’s category one clinical stage. Regarding the duration of antiretroviral treatment and follow-up, thirty-nine (43.8%) of the cases and ninety-two (33.9%) of the control group remained on antiretroviral treatment. Less than three years. Out of control individuals who had disclosed their HIV status, 156 (57.6%) disclosed their HIV status to their husband or current partner, and the remaining 115 (42.4%) disclosed it to another family member or friend. Regarding the number of lifetime sexual partners, most of them (58.9% of 71 cases and 141 controls) had more than one lifetime sexual partner (Table 2).
 |
Table 2 Health-Related Characteristics of Respondent Among HIV Infected Patients Attending in ART Clinics of Public Health Facilities, in Gedeo Zone, Southern Ethiopia, 2022 |
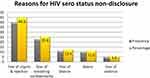
Reasons for Non-Disclosure of Their HIV Positive Status
Among the 89 respondents who did not tell their HIV status to a spouse or other family member, the two most common reasons for not revealing were “fear of stigma and rejection (44.9%) and fear of breaching confidentiality (25.8%)” (Figure 1).
Determinants Associated with HIV Positive Status Non-Disclosure
To determine the predictors of HIV-positive status non-disclosure, a binary logistic regression model was used. Variables having p-values less than 0.25 in the bivariate analysis were included in the multivariable logistic regression analysis model. After controlling for potential confounders, the variables statistically significantly associated with HIV-positive status secrecy were sex, urban residence, WHO clinical stage of disease, duration of ART follow-up, and number of lifetime sexual partners. Women were 2.8 times more likely than males to keep their HIV status hidden (AOR = 2.8, 95% CI (1.04–7.56)). In terms of domicile, individuals living in rural regions were 3.5 times more likely than those living in urban areas not to reveal HIV-positive status (AOR = 3.52, 95% CI (2nd.83–9.39)). Similarly, non-disclosure of HIV-positive status was 4.6 times more likely in patients with WHO clinical illness stage 1 than in patients with WHO clinical disease stages 3 and 4 (AOR = 4.68, 95% CI (1st.9–22.1)). Furthermore, respondents with fewer than three years of ART follow-up were 4.2 times more likely than those with lengthier ART follow-up not to reveal HIV-positive serostatus (AOR = 4.21, 95% CI (1.65–10.73)). In this study, having a variety of lifetime sexual partners was also an independent factor. Those who had more than one lifelong sex partner were 6.9 times more likely than those who had one lifelong sex partner not to reveal their HIV-positive status (AOR = 6.9, 95% CI (1.86–26.3)) (Table 3).
 |
Table 3 Bivariate and Multivariate Logistic Regression Analysis on Non-Disclosure of HIV Positive Sero Status Among Plhiv, in Public Health Facilities of Gedeo Zone, Southern Ethiopia, 2022 |
Discussion
Non-disclosure of HIV-Positive Serostatus to a sexual partner or close family member is an impediment to HIV testing promotion because it lowers possibilities for social counseling and, in the long run, impedes future plans for safe HIV prevention and control. The gender, location of residence, WHO clinical stage of illness, length of ART follow-up, and number of lifetime sexual partners were revealed to be statistically significant predictors of HIV-positivity status secrecy in this study.
In comparison to males, sex, ie being female, was strongly related with non-disclosure of HIV-positive status, according to the study. A study conducted in the Northern Shewa Zone and South Africa also found similar results in their studies.19,20 This implies that women are more likely to not disclose their HIV-positive status than men. This could be due to a variety of factors, such as fear of stigma, lack of access to healthcare, or lack of knowledge about HIV. Women may also be more likely to be in a position of vulnerability, such as being in an abusive relationship, which could lead to them not disclosing their status. Additionally, cultural norms and expectations may also play a role in women not disclosing their HIV-positive.
The study also found that people living in rural regions were 3.5 times more likely than those living in urban areas to conceal their HIV status. This conclusion is analogous to one from a research conducted in the towns of Debre Markos, Ethiopia, and Tanzania.21,22 This study has far-reaching consequences for public health policy and HIV prevention and treatment programs in rural settings. Community-based education campaigns, home-based counseling and testing services, the engagement of local community leaders, and the integration of HIV care with other health services are all strategies for increasing HIV status disclosure and addressing stigma in rural regions. Furthermore, healthcare clinicians and policymakers must evaluate the influence of socioeconomic variables such as restricted access to healthcare, education, poverty, and cultural norms on HIV status non-disclosure. This study emphasizes the need of rural targeted interventions to promote HIV status disclosure, reduce HIV-related stigma, and improve access to health services. More research is needed to investigate the factors that impact HIV status non-disclosure in rural settings. Evidence-based interventions are critical for lowering the HIV load in rural regions and improving the health outcomes of HIV patients.
Furthermore, respondents with less than three years of ART follow-up were shown to be 4.2 times more likely than those with longer ART follow-up not to declare their HIV-positive serostatus. The findings of this study show that HIV-positive people who have had less than three years of ART follow-up are more likely to hide their HIV-positive serostatus than those who have had longer follow-up. This conclusion is consistent with findings from a study conducted in Ethiopia’s North Shewa Zone and another at Mekele Hospital.13,19 This case–control study underlines the necessity of long-term engagement and focused interventions to increase ART adherence and reduce the risk of HIV transmission. Individuals with shorter follow-up times may not have received appropriate assistance or counseling to help them appreciate the need of ART follow-up and the hazards associated with not revealing their HIV-positive status, according to the research. Furthermore, health care practitioners must offer ongoing assistance and counseling to HIV-positive individuals who are new to ART follow-up. Finally, the study emphasizes the importance of tailored treatments to increase ART adherence in HIV-positive patients with fewer than three years of ART follow-up.
Participants in this study who had more than one lifetime sexual relationship were less likely to report their HIV status than those who had just one lifetime sexual partner. The conclusion that having more than one lifetime sex partner increases the chance of HIV-positive status not being disclosed is consistent with other research done in various contexts. For example, comparable result was also observed in the study conducted in Bangkok,10 and a systematic review of studies conducted in sub-Saharan Africa found that having multiple sexual partners was associated with increased HIV non-disclosure.11 Similarly, a study conducted in south-west, north Shewa Zone of Ethiopia and Amhara region16 and Uganda found that individuals who had more than one sexual partner were less likely to disclose their HIV status.3 This study discovered that individuals in Ethiopia’s Southern area with WHO clinical illness stage 1 are more likely to keep their HIV-positive status hidden than those with higher WHO clinical disease stages. This is problematic since non-disclosure can result in poor drug adherence, untreated diseases, and continued HIV transmission. To address this issue, healthcare practitioners can establish a safe and supportive atmosphere for patients to reveal their HIV status, and community-based activities to minimize HIV stigma and prejudice can be adopted. Furthermore, it is critical to engage with the community and design culturally relevant treatments to address the underlying social and cultural variables that lead to non-disclosure. On the other hands, the study conducted in Addis Ababa contradicts the finding that the WHO stage of the disease is unrelated to the disclosure status of individuals.23 Perhaps, the variations in research design and study subject characteristics can be used to explain the observed variance.
This study used several steps to increase its internal and external validity by utilizing standardized questionnaires to collect both primary and secondary data, proper statistical techniques. Despite the several efforts made to improve internal and external validity, because of the effect of non-matched participants and non-random participant selection, this study has limitations. Although regression analysis was employed to control for potential confounding variables, the inclusion of non-matched study participants and non-random participant selection may have influenced the findings’ generalizability. Participants may have had more or less exposure to certain risk variables than the general population, resulting in selection bias. Furthermore, differences in factors such as age, gender, or socioeconomic status may have impacted the research findings. As a result, the generalizability of the findings should be regarded with caution.
Conclusion
The study identified the following factors as predictors of non-disclosure of HIV serostatus among people living with HIV: sex, residence, WHO clinical stage of disease, length of time on ART follow-up care, and number of lifetime sexual partners. It is vital to promote HIV disclosure and minimize stigma in order to encourage persons living with HIV to reveal their status. This can be helped by public awareness campaigns and community education programs. Healthcare practitioners should consult and assist people who are thinking about disclosing their HIV status. Social and cultural elements should be considered in personalized therapy. A program administrator should participate in community-based efforts aimed at eradicating HIV stigma and empowering women. WHO clinical stage 1 patients who have several sexual partners should get thorough counseling from healthcare professionals. Targeted medications should be created for vulnerable populations such as individuals who live in rural areas, have several sexual partners, and have HIV in the early clinical disease stage. To choose a viable remedy, researchers must do more research to uncover other underlying issues.
Abbreviation
AIDS, Acquired immune deficiency syndrome; ART, Antiretroviral therapy, Ratio; DHPSS, Disclosure of one’s HIV serostatus; HAART, Highly active antiretroviral therapy; HIV, Human immunodeficiency virus; MOH, Ministry of health; MTCT, Mother-to-child transmission; NDHPSS, Non-Disclosure of one’s HIV serostatus; PLHIV, People living with human immunodeficiency virus; PMTCT, Prevention of mother to child transmission; SPSS, Statistical package for social science; RNA, Ribonucleic acid; WHO, World Health Organization.
Data Sharing Statement
All the data created and analyzed in the study are incorporated in this manuscript and uploaded tables and figure. Moreover, the data base used for analysis and other information are available currently in the hands of principal investigator (BT) and corresponding author (GB).
Acknowledgment
I would like to acknowledge Dilla University College of health sciences and medicine, school of public health, department of reproductive health for giving me the chance to carry out this study. Finally, my sincere appreciation belongs to Dilla University General Hospital, Yirgacheffe primary Hospital, Wonago and chelelektu Health center ART care provider, supervisor, and data collectors, for their unreserved effort.
Author Contributions
All authors made a substantial contribution to conceptions and design, analysis and interpretation of data. They also took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Global HIV/AIDS overview; 2020. Available from: https://wwwhivgov/federal-response/pepfar-global-aids/global-hivaids-overview.
2. World Health Organization. Gender dimensions of HIV status disclosure to sexual partners: rates, barriers and outcomes. World Health Organization; 2004. Available from: https://apps.who.int/iris/handle/10665/42717.
3. Ngonzi J, Mugyenyi G, Kivunike M, et al. Frequency of HIV status disclosure, associated factors and outcomes among HIV positive pregnant women at Mbarara Regional Referral Hospital, southwestern Uganda. Pan Afr Med J. 2019:32. doi:10.11604/pamj.2019.32.200.12541
4. Makin JD, Forsyth BWC, Visser MJ, et al. Factors affecting disclosure in South African HIV-positive pregnant women. AIDS Patient Care STDS. 2008;22(11):907–916. doi:10.1089/apc.2007.0194
5. Gari T, Habte D, Markos E. HIV positive status disclosure among women attending art clinic at Hawassa University Referral Hospital, South Ethiopia. East Afr J Public Health. 2010;7(1):87–91. PMID: 21413581.
6. Stirratt MJ, Remien RH, Smith A, Copeland OQ, Dolezal C, Krieger D; SMART Couples Study Team. The role of HIV serostatus disclosure in antiretroviral medication adherence. AIDS Behav. 2006;10(5):483–493. PMID: 16721505. doi:10.1007/s10461-006-9106-6
7. Ayish DM. Ramification of status non-disclosure by people living with HIV/AIDS in Alice Eastern Cape. university of forthare; 2016. Available from: http://vital.seals.ac.za:8080/vital/access/manager/Repository/vital:35970?site_name=GlobalView&view=null&f0=sm_creator%3A%22Mavhunga%2C+Ayisha+Dadiso%22&sort=null.
8. Fatoki B. Understanding the causes and effects of stigma and discrimination in the lives of HIV people living with HIV/AIDS: qualitative study. J AIDS Clin Res. 2016;7(12):635. doi:10.4172/2155-6113.1000635
9. Morkphrom E, Ratanasuwan W, Sittironnarit G, Rattanaumpawan P. Non-disclosure of HIV serostatus to sexual partners: prevalence, risk factors and clinical impact in patients with HIV. HIV Med. 2021;22(3):194–200. Epub 2020 Nov 3. PMID: 33145968. doi:10.1111/hiv.13005
10. Edwards-Jackson N, Phanuphak N, Van Tieu H, et al. HIV serostatus disclosure is not associated with safer sexual behavior among HIV-positive men who have sex with men (MSM) and their partners at risk for infection in Bangkok, Thailand. AIDS Res Ther. 2012;9(1):38. PMID: 23259683; PMCID: PMC3537734. doi:10.1186/1742-6405-9-38
11. Mosisa G, Mulisa D, Oluma A, et al. HIV sero-status disclosure and associated factors among HIV positive women in East Africa: systematic review and meta-analysis. Implications for prevention of mother-to-child HIV transmission. Front Public Health. 2022;10:919410. PMID: 36483255; PMCID: PMC9723243. doi:10.3389/fpubh.2022.919410
12. Medley A, Garcia-Moreno C, McGill S, Maman S. Rates, barriers and outcomes of HIV serostatus disclosure among women in developing countries: implications for prevention of mother-to-child transmission programmes. Bull World Health Organ. 2004;82(4):299–307. PMID: 15259260; PMCID: PMC2585956.
13. Tam M, Amzel A, Phelps BR. Disclosure of HIV serostatus among pregnant and postpartum women in sub-Saharan Africa: a systematic review. AIDS Care. 2015;27(4):436–450. doi:10.1080/09540121.2014.997662
14. Ethiopian Public Health Institute (EPHI) [Ethiopia] and ICF Ethiopia mini demographic and health survey 2019: final report. Rockville, Maryland, USA: EPHI and ICF; 2021. Available from: https://dhsprogram.com/publications/publication-FR363-DHS-Final-Reports.cfm.
15. Ethiopian Ministry of Health. National comprehensive HIV prevention, care and treatment training for pharmacy professionals: participant manual; 2018. Available from: http://repository.iifphc.org/handle/123456789/1459.
16. Tibebu NS, Rade BK, Kebede AA, Kassie BA. Disclosure of HIV status to sexual partner and its associated factors among pregnant women living with HIV attending prenatal care in Amhara Regional state referral hospitals, Ethiopia. PLoS One. 2023;18(1):e0280045. doi:10.1371/journal.pone.0280045
17. Tadesse M. Assessment of HIV discordance and associated risk factors among couples receiving HIV test in Dilla, Ethiopia. BMC Res Notes. 2014;7(1):893. doi:10.1186/1756-0500-7-893
18. UNAIDS. Joint united nations programme on HIV/AIDS; 2019. Available from: https://www.unaids.org/sites/default/files/media_asset/2019-global-AIDS-update_en.pdf.
19. Alemineh TL, Tsegaye D, Minwuyelet F, et al. Determinants of non-disclosure to sexual partner among human immune virus infected adults on anti-retroviral therapy follow-up care at North Shewa Zone public Hospitals in Oromia Region, Ethiopia, 2020. Int J Africa Nurs Sci. 2022;17:100484. doi:10.1016/j.ijans.2022.100484
20. Adeniyi OV, Ajayi AI, Selanto-Chairman N, et al. Demographic, clinical and behavioural determinants of HIV serostatus non-disclosure to sex partners among HIV-infected pregnant women in the Eastern Cape, South Africa. PLoS One. 2017;12(8):e0181730. doi:10.1371/journal.pone.0181730
21. Benayew Shifraew M, Teshome Shiferaew M, Zeleke Mitiku H, Ayalew AF. HIV-positive status disclosure to sexual partner and associated factors among adult HIV-positive patients in Debre Markos Town, 2019. HIV AIDS. 2021;13:571–579. PMID: 34079384; PMCID: PMC8163629. doi:10.2147/HIV.S293017
22. Charles J, Exavery A, Barankena A, et al. Determinants of undisclosed HIV status to a community-based HIV program: findings from caregivers of orphans and vulnerable children in Tanzania. AIDS Res Ther. 2020;17(1):42. doi:10.1186/s12981-020-00299-8
23. Meseret Y, Dulla D, Nega B. Prevalence and factors affecting disclosure of HIV status among pregnant women attending antenatal care in Addis Ababa public health centres: a cross sectional survey. Obstet Gynecol Int J. 2019;10(4):317–324. doi:10.15406/ogij.2019.10.00460
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.