Back to Journals » Medical Devices: Evidence and Research » Volume 16
Medical Equipment Management in General Hospitals: Experience of Tulu Bolo General Hospital, South West Shoa Zone, Central Ethiopia
Authors Kabeta SH , Chala TK , Tafese F
Received 6 January 2023
Accepted for publication 10 March 2023
Published 17 March 2023 Volume 2023:16 Pages 57—70
DOI https://doi.org/10.2147/MDER.S398933
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Sirnan Humnesa Kabeta,1 Temesgen Kabeta Chala,2 Fikru Tafese2
1Oromia Regional Health Bureau, Finfinne, Ethiopia; 2Health Policy and Management Department, Jimma University, Jimma, Ethiopia
Correspondence: Temesgen Kabeta Chala, Email [email protected]
Background: Medical equipment are vital items to deliver quality services in health facilities and the role of medical equipment is a well-founded reality. It is mainly used in many diverse settings in hospitals to diagnose, treat illnesses; support disabled and intervened acute and chronic cases. Effective maintenance and proper management are major utilization issues to provide quality services while saving scarce resources. However, managing medical equipment, especially, the utilization phase of medical equipment, was not well studied in this general hospital.
Objective: This study aims to assess the utilization of medical devices in Tulu Bolo General Hospital.
Methods: The study was conducted from December 25, 2021 to February 9, 2022. Data sources included health professionals and document archives in the hospital. Data collection method includes questionnaires and observations checklists. A census of 165 health workers was conducted, with a response rate 94.5%. Data was entered into epi-data; version 3.1, then analyzed by SPSS version 23 and presented using descriptive statistics.
Results: Procurement, storage, and utilization were found to be 53.47%, 56.57%, and 45.88%, respectively. Only 114 (57.3%) of the 199 pieces of medical equipment discovered were functional. Pearson correlation indicated that procurement and utilization of medical equipment are related to a higher proportion of non-functional devices (P = 0.000, B1 = 1.47, OR = 4.349, and CI 95% = 2.047– 9.241) and nonfunctional medical equipment (B2 = 0.790, OR = 2.203, and CI 95% = 1.065– 4.556) for procurement and utilization, respectively.
Conclusion: Procurement, storage, and utilization of available medical equipment in Tulu Bolo Hospital were low. While health sectors operating in a resource-limited were assumed to have a big shortage of medical technologies, procurement, storage, and utilization of the limited available medical equipment need the attention of health program managers.
Keywords: utilization, medical equipment management, procurement, the functionality of medical equipment
Introduction
Medical Equipment Management (MEM) is how medical equipment is acquired, utilized, conserved, and assisted by internet technology for documentation. MEM practices are important in the management of human resources to successfully operate in health care. It has several domains, such as procurement, effective utilization, maintenance service, storage, and decommissioning or disposal.1
The procurement of ME includes medical device assessment, prioritization, purchase, installation, and commissioning in sequential order. This process begins in the health facility with organizing the purchase order and is summarized with receiving the commodity. Completing these steps, the equipment begins its life of services.2,3 The effective use of ME is the most important and gets health-care providers and communities concerned. Inefficient use of medical equipment in different health-care structures compromises the quality of care and costs more.4 Another important practice in medical equipment management is the storage of medical equipment. The goal of medical equipment store management is to properly handle the equipment and avail it for the intended purpose only without any dissipation.5
Proper management of medical equipment protects the patients and health-care givers from unnecessary injuries from defective medical equipment.6 From the side of the health system, Sustainable Development Goal (SDG) felt a challenge from the weaknesses in the health-care system to deliver health services at different levels nationally and globally.7
Currently, medical technology attracts attention due to its critical role in minimizing the complication to the health of the patients and reduction of the time of treatment. The primary step in managing medical equipment is understanding what commodities are to be handled and performing inspections of the items.8 The hospital inventory management is the working file, as it is performed on a regular basis to conserve the assets of the facility. Properly used inventories improve the handling of the most important medical devices.7,9
Equitable access to essential medical equipment, pharmaceuticals, and vaccines of assured quality, safety, efficacy, and their scientifically sound and cost-effective use was very important.10 In certain resource-limited countries like Ethiopia, a variety of medical equipment are not functional. Of the total donated medical equipment, up to 96% are out of service at any time in the developing world. Around 50% of capital medical equipment like laboratory machinery was not in use in lower economic countries.11 To improve universal health coverage, address health emergencies, and promote healthier communities, access to good quality, affordable and appropriate health-care products is the most essential.12
Biomedical equipment management thus presents a challenge for many countries, especially those with low technical resources like Ethiopia, both human and infrastructural. Biomedical Engineers and pharmacists play a great role in managing medical equipment especially to provide electrically safe, calibrated, and well-functioning equipment to deliver the best healthcare for patients and to present the most cost-effective manner of maintaining equipment in a hospital.13
In a health-care setting, human power issues, staff training, and motivation were full filled by proper utilization of medical devices.13 Procurement, utilization, and decommissioning of medical equipment have a high influence on the quality of health services given to patients.14
The regulation and policy of medical equipment management incorporating procurement, sale, maintenance, and utilization of medical equipment and provision of guidelines manual for its operation or performance; capacitating of biomedical professionals and availing of spare parts.15 Recently, WHO has continuously identified and advised that policies regarding medical equipment be revised to enable health systems. Quality Assurance has strictly stressed the need to adopt standards and best practices in the utilization of medical equipment to enhance patient safety and Medicare management.16
Ethiopia is now dealing with massive problems like communicable diseases (CD), non-communicable diseases (NCDs), and injuries, which affect all age groups but disproportionately affect children and women of reproductive age, as well as cyclical hazards that affect households, infrastructure, and system resilience.17 Poor health service quality is due to shortages of medical equipment, drugs, and medical supplies and a lack of modern and improved health-care services.18
Well-managed medical equipment needs complete and accurate data. A cyclic phase of medical equipment management contains several domains like procurement, acceptance, inspection, installation, ensuring performance within the accepted standards, safe and effective utilization, maintenance service, storage, and disposal. Proper management of medical equipment protects the patients and health-care givers from unnecessary injuries from defective medical equipment.6 Global MEM practices were a major issue in the current state of health-care services. On the other hand, as the population grew older, so did the demand for medical equipment.19
In developing countries, about forty to seventy percent of medical equipment is damaged or not fit for the intended purposes and impairs the service given to the clients.20 Generally, improper handling of medical equipment limits the capacity of health institutions to give adequate health care. In Ethiopian public hospitals and other health-care settings, more than 61% of medical equipment is functional at any one time. In Ethiopia, only a few studies reported the status of medical equipment, and most of them indicated that greater than 33% of the medical equipment in higher health-care institutions was not functional and not in use.21
In this study, we aimed at assessing the procurement, storage, and utilization of medical equipment in Tulu Bolo General Hospital, central Oromia and propose comprehensive frame work and recommendations. Considering the importance of the subject, the goal of this paper is to assess medical equipment management practices using a qualitative and quantitative approach to provide good health services and saving limited resources.
Methods
The Study Setting
This facility-based cross-sectional study was conducted at Tulu Bolo General Hospital. The hospital is found 81 kilometers far from Finfinne. The hospital was constructed by the Oromia Regional Health Bureau in 2010 GC. The hospital is expected to give services to the population estimated at 1,000,000 people living in Tulu Bolo and the surrounding area. Tulu bolo general hospital gives services like outpatient, in patients having different departments (medical, surgical, gynecology, NICU, pediatrics) and has around 115 beds during the data collection. This hospital has laboratory services; new initiative auditable pharmacy services (APTS).
Even though the hospital was serving all these services in inadequate infrastructures, by now different blocks were constructed with around 78 million birr. One block was constructed for the implantation of CT scan by the support of the hospital catchment voluntaries to solve the problems of the community. A total of 249 staffers are reported to be active employees. Of these, 165 are health professionals of different disciplines. The health professional included medical doctors, nurses, Medical Laboratory professionals, radiographers, midwifery professionals, pharmacy professions, biomedical engineers and public health professionals.
This study takes place from December 25, 2021–February 9, 2022.
Study Design
A facility-based cross-sectional study design was performed.
Data Sources and Collection
The data sources include health professionals and documents archives in the hospital. The data collection method includes questionnaires, checklists, and observations using checklists.
Data Collections
The questionnaire was modified from the checklist for MEM practice and double-checked by the principal author and co-authors to make it fit for this study’s purpose. Here, the research instruments had been in use before by other researchers for other similar studies and they were found to be valid instruments by the researchers. The questionnaires used in this study were double checked with two Jimma University researchers. To test the validity of the questionnaire, a pilot study was conducted on 10% of the sample, that is 16 persons from different departments.
To assure the quality of the data collected two professionals (one chief pharmacist and one biomedical engineer) were assigned as supervisors from woliso zonal health department. Four experienced data collectors from woliso general hospital who have no relation to the study facility were participated. The study participants were health professionals and biomedical engineers who are familiars with medical equipment and know the medical equipment management check list as it is one of the key performance indicator in hospital setting.
Document review, observation of medical equipment, and interviewing were utilized in the data collection from the study health facility. The documents like bin cards, models and elective surgery registration books were reviewed by the principal investigator. We converted the open-ended questionnaires into dichotomous (yes/no) questions and distributed them to all Tulu Bolo Hospital employees. Four health professionals were recruited for the data collection from another hospital.
Data was collected through a self-administered questionnaire, document review, an in-depth interview, and observation of the medical devices.
Procurement, utilization, and storage practices were outcome variables. Additionally, all equipment was checked for functionality.
Analysis Procedures
The data was cleaned, coded, and entered into epi data version 3.1. The processed data were transferred to SPSS version 23 software for analysis. Following analysis, descriptive statistics like tables, percentages, averages, and charts were used. The result score of p-value below 0.05 is considered significant. The odds ratio was also calculated and used to present the results.
Finally, the fit model used in the analysis provides the extent to which the independent variables affect the outcome presented as the following equation.
The available data were reliable results for a valid hypothesis when tested. Simple linear regression was not appropriate when the value of the dependent variable is binary as the expected value of Y had the probability of either 1 or 0.22
Ethical Clearance
Ethical approval was obtained from the Jimma University Institutional review board (IRB) on the date 23/22/2021 with reference number of IHRPGn/71/21. Permission for the study was also guaranteed from Oromia regional health bureau and South West Shoa Zonal Health Department and official letter was written to Tulu bolo general hospital to conduct a research. After getting permission from the hospital, data collection was started after informed consent was obtained from all participants.
In this study, the researcher is ethical enough. The dignity, right and secrecy of individuals and institutions were respected. The researcher clarified the reasons and objectives of undertaking this research to respondents. Any person involved should be assured as nothing will happen on their right, security and psychology. At the beginning of the survey, the enumerators were trained and instructed to explain the purpose of the research to the respondents and to request their verbal consent before conducting the questionnaire.
Confidentiality of the information that respondents provided was ensured and their freedom of terminating the questionnaire/interview at any point and skipping any questions that they would not wish to respond to. Lastly, respondents were informed that any data they provide was kept confidential. The analysis was undergone without mentioning names and the information they provide was not used for anything other than research purpose. All other sources of data and ideas were fully acknowledged.
Results
Socio-Demographic Characteristics of Respondents
In this study, census survey was the suitable sampling technique for as the number of selected hospital health professionals who had direct contact with medical equipment were less than two hundreds and minimizes sampling error. Thirteen study participants for in-depth interviews were selected purposely due to their knowledge for the subject matter of this study. To capture a wide range of perspectives and gain greater insights into this study the participants were grouped based on their expertise. About 199 medical equipment which are thirteen in type were selected from the hospital inventory list.
The ages of most of the respondents were between 26 and 30 years. More than 55% of the respondents were nurses in their profession. The majority of the respondents had work experience of more than six years. Out of a total of 165 health workers 156 (94.5%) completed and returned the questionnaire among which more than half (64.1%) were males (Table 1).
 |
Table 1 Summary of Socio-Demography of the Respondents |
Medical Equipment Procurement, Storage and Utilization
Procurement Practice
The majority of medical equipment in Tulu bolo general hospital was from the donation (64.7%). A slightly higher proportion (50.6%) responded that medical equipment was not requested and delivered on time. Again, a higher proportion (51.3%) of responded received did not consider the hospital setting. Moreover, most of the received medical equipment was not installed according to the equipment’s manufacturer’s instructions (Table 2).
 |
Table 2 Medical Equipment Procurement, Storage and Utilization in Tulu Bolo Hospital, 2022 |
This finding was supported by the qualitative finding. According to KII the medical equipment procurement practice in Tulu Bolo general hospital is not based on demand.
… medical equipment procurement practices were not based on a schedule to buy medical equipment, but undergo the procurement based on the need most of the medical equipment was received by donation and they did not have enough spare parts (KII, female 26 age, 2022) and here one KII added… there is no involvement of hospital in decision making to receive the medical equipment (KII, male 26 ages, 2022)…
Another KII added,
… the hospital has no adequate budget for medical equipment as pharmaceuticals and this was why medical equipment was not availed in quality and quantity, and the purchase of medical equipment has much higher regulatory registration than medicines. Regulations like pre-procure agreement with the supplier that is EPSA. (KII, male 39 ages, 2022)
A similar idea was added by a key informant from finance,
… EPSA was not interested to give us the stock out in a reasonable time and if we request medical equipment through an agreement, it may take a long period even from 6 months to one-year duration added by. (KII, male 33 ages, 2022)
Utilization Practice
Regarding the utilization of medical equipment, more than half (58.3%) of the medical equipment’s end users did not report immediately to the responsible office. For 51 medical equipment (41%) neither preventative nor curative maintenance was scheduled. On average medical equipment utilization practice was 56.57% (Table 3).
 |
Table 3 Medical Equipment Utilization Practices at Tulu Bolo Hospital, 2022 |
Medical equipment was the key element in the health-care system and needs care; the majority of the respondents replied that there was no proper hand covering system and one of the key informants mentioned:
… medical equipment users did not care for the medical equipment they used, and even if they did not hander the medical equipment most of the service units didn’t report the medical equipment, and different non-functional medical equipment are seen during the inventory. If vital medical equipment stops functioning, they bring it to the store and take the new one rather than consulting biomedical engineers through a work order sheet. (KII, male 27 ages, 2022)
Similarly, this idea was supported by one physician from a dental clinic explained:
There is no sufficient training about medical equipment for storekeepers, technicians, and users. Sometimes they didn’t know the name of the medical equipment stored there and the arrangement is not attractive (KII, male 33 ages, 2022). A key informant interview from a pharmacy added…, biomedical engineers do not have enough training to do preventive maintenance for most and to fix when impaired especially not consider inspection and preventive maintenance. (KII, Male 35 ages, 2022)
In addition, even though the procurement was the basis in measuring the quality of medical equipment, it did not get sufficient attention, one key informant stated:
… the challenge in MEM starts at procurement, they didn’t involve us in setting specifications due to this some medical equipment are not working from the beginning, some impaired when they start to use due to inappropriate electric power, and most equipment become out of use due to careless handling by professionals, and lack of preventive maintenance, overload above the capacity of the equipment. (KII, male 36 ages, 2022)
Concerning medical equipment utilization, two key informants contradicted that:
… we didn’t get the maintenance in a reasonable period and sometimes we rewrite the work order and report to the medical director. When we ask them, they respond us we are searching for spare parts and even they were busy more (KII, male33 ages, 2022) and here one from the biomedical unit complained that … the service unit didn’t report according to the work order format but simply ask us verbally, and this felt us overburden. (KII, male 27ages, 2022)
Similarly, one key informant from the radiological team head added:
… some year one digital x-ray machine stopped working and biomedical engineers couldn’t maintain it and consult the biomedical engineers at the regional level and also they didn’t maintain it. The hospital felt a problem and the imaging stops for around three months and RHB avail one new machine. Because of a lack of space, the previous one was improperly detached and the new one was installed. While the medical equipment professionals came from abroad to maintain them, the machine was already damaged and some spare parts like cable were given to another health facility so at that time four million machines become out of service. (KII, Male 31ages, 2022)
A key informant from the operation room stated,
Most of the received medical equipment was from donation and not gave the intended services, for example, Electrocardiograph (ECG) machine returned to the store due to the software language (only Chinese) even though the hospital has no other ECG machine. Moreover, the language barrier made the utilization of the machine difficult. (KII, male 32 ages, 2022)
Storage Practice
Even though nonfunctional medical equipment were stored, the record was found only for 71 (45.5%) (Table 4).
 |
Table 4 Medical Equipment Storage Practice at Tulu Bolo Hospital, 2022 |
Overall medical equipment status (Observations)
Percentage of functionality = (functional medical equipment/total selected equipment) x100 (Figure 1)
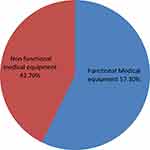 |
Figure 1 Functional status of medical equipment in Tulu Bolo General Hospital, South West Shoa Zone, Central Ethiopia, 2022. |
= (114/199) x100
= 57.3%.
Percentage of the functionality of MEMC = (criteria fulfilled by hospital/total criteria to be fulfilled) x100.
Criteria fulfilled from the check list-11
Total criteria on the check list-20
= (11/20) x100
= 55%.
The correlation between the functionalities of medical equipment and procurement was moderately positive (r = 0.410 and p (0.000) 0.05). On the other hand, the correlation between the functionality of medical equipment and utilization was also positive (r = 0.293 and p = 0.000). Again, the correlation between medical equipment functionality and storage practices was small and positive (r = 0.216 and p = 0.005; 0.05). Generally, all variables were correlated positively with functionality, even though their correlation strength varies. The independent variables do not correlate with each other (Table 5).
 |
Table 5 The Relationship Between Procurement, Utilization, Storage Practices and Functionality of Medical Equipment |
The model that includes the explanatory variables (procurement, utilization, and storage practice) is now correctly classifying the outcome for 70.5% of the cases compared to 51.9% in the null model (Table 6).
 |
Table 6 Functionality Without and with Explanatory Variables (Procurement, Utilization and Storage Practices) |
The output in the Variables in the Equation table provides the regression coefficients (B), the Wald statistic (to test the statistical significance), and the Odds Ratio (Exp (B)) for each variable category. The procurement overall effect (df=1, B1 = 1.470, OR = 4.349 p = 0.0, 95% CI between 2.045 and 9.241). The utilization overall effect (df = 1, B2 = 0.79, OR = 2.203 p = 0.033, 95% CI between 1.075 and 4.618). The storage practice overall effect (df = 1, B3 = 0.313, OR = 1.367 p = 0.423, 95% CI between 0.637 and 2.939) (Table 6).
Generally, the effect of the three independent variables on the functionality of medical equipment is expressed by the logistic regression model as the following equation, the storage practices were not included in the equation as it is not significant.
FUN = functionality, PROC = procurement practices, UTIL = utilization practices,
Poor storage of Medical equipment was mentioned by one KII,
… Last year I was a member of the inventory team and we found some non-functional medical equipment in the store. The inventory system in our hospital was attractive and we count medical equipment found in the store as well as in the service units and reported to the CEO and finance management. In addition, the bin card was not recorded and only model 19 during receiving and model 22 for issuing were utilized. The stock card is also not used to control the stock. Sometimes medical equipment is left in the service unit without thatching the model simply through verbal transfer, especially during the transfer and change of the unit (KII, male 32 ages, 2022)
Discussions
Medical equipment procurement, storage, and utilization were found to be lower in the context of a resource-limited setting. Such practices were found to be similar across different parts of Ethiopia. Our finding was found to be close to that of the study conducted in Addis Ababa public hospitals (50%)23 and this similarity could be because most of the time, procurement of medical equipment is conducted at the regional or federal level, and most equipment is acquired through donation.
Regarding the utilization of medical equipment, only 56.57% were found to fulfill our utilization measurement tool. This finding was similar to that of the study conducted in eastern Wollega, which was 57.8%.4 The similarity could be uniformity in the donation of medical equipment, a lack of locally available maintenance kits, or the limited number of biomedical engineers in the country.
Medical equipment storage conditions are inadequate. Tulu Bolo Hospital had a storage practice of 45.88%. The observation discovered that medical equipment storage rooms were separate from other supplies and furniture. However, certain laboratory supplies, reagents, and intravenous fluids were stored with medical equipment. Our finding is similar when compared to the study conducted in Addis Ababa (54.55%). Most (54.5%) of the hazardous chemicals were not separately stored in public hospitals in Addis Ababa.24
During this study, a significant number of medical equipment (42.7%, n = 199) were not in use due to non-functionality. This finding was found to be similar to the study conducted in Jimma Zone, where observation and interview showed that 299 medical devices were available in the three hospitals and, on average, about 40.6% were non-functional.21 The similarity could be explained by the severity of the problem across the region. In Tulu bolo general hospital, medical equipment management unit committees met only 55% of medical equipment management criteria from the checklists and considered not fully functional and this may be the reason for the non-functionality of medical equipment.
In contrast to the above finding, the study findings conducted in other countries were: China (77%);25 Costa Rica, and Ghana (86.4% and 74.1%, respectively).26 In eight public hospitals of Australia, around 84% were functional while the left 16% of equipment did not get preventative maintenance on time.27 Compared to sub-Saharan countries medical equipment maintenance practices European countries like Italy were more effective and prevent the sudden failure of critical medical equipment, even though Italy is a mature for medical devices and the fourth largest market in Europe next to Germany, France, and UK, having 42% distributers, 53% producers, and 5% service providers. The availability of medical equipment like orthopedics and dental devices declined in 2020 due to Covid-19 pandemic.28 In Canada, most of the hospitals efficiently utilize their medical equipment as they include all their inventories in their maintenance program and follow manufacturers’ directions for preventative maintenance. From the finding, only around 13.7% is related to inadequate preventive maintenance, set-up and uncategorized repair calls.29 In developing countries like Ethiopia, medical equipment were used until they finish their working time without considering preventive maintenance and this minimizes the effective life time of medical equipment.
The difference in this finding might be due to differences in technologies, the manufacturing capacity of the medical equipment, and the availability of maintenance kits. The other differences were due to our study hospital gives all health-care services like laboratory services, imaging services, inpatient and outpatient services, laundry services, operations and workshops with all types of medical equipment in a single compound compared to some European countries having separate service areas with equipped professionals. In a lower performing countries, medical equipment maintenance costs high. According to the joint commission show medicinal equipment related incidents that related to serious injuries or deaths are typically among the top ten types yearly.29
When triangulating the qualitative response on lack of training, lack of policies and procedures, low testing inspection performance, physical space to install the procured item, and absence of schedule record keeping by the hospitals, the research findings in Jimma University Specialized Hospital were supported in South Sudan, pharmaceutical logistics reveal that 75% of facilities have a separate store assigned, but with inadequate space, and many facilities do not adhere to the proper guidelines.30,31
Limitation of the Study
The limitation of the study was that it was conducted only in Tulu bolo general hospital and did not include suppliers like whole sales and EPSA which do have great potential to identify problems related to medical equipment management practices of the study area. A longer time and enough resources would have helped to come up with more findings, especially with other health-care institutions in other regions of the country. The expected finding may be biased due to self-administered questionnaires. The study did not include the brand or the origin of medical equipment that this may affect the quality and durability of medical equipment.
Conclusions and Recommendations
Purchasing, utilization, and storage of medical equipment are slightly low in Tulu bolo hospital. While countries in resource-limited countries are assumed to have a big shortage of medical technologies, procurement, storage, and utilization of the limited available medical equipment need the attention of health program managers. A further exploratory study is needed to explore why procurement, storage, and utilization are low. Given the limited resources, hospital managers and health cadres should focus and invest not only in procuring new medical technologies but utilization and storage practices. Wisely utilized medical device saves the hospital from high maintenance costs, serious incident like injuries and deaths. Therefore, health facilities must ensure their critical medical equipment are accurate, safe, reliable and operating at the maximum level of performance. Biomedical engineers and Medical equipment maintenance kits should be arranged for timely maintenance and utilization of medical equipment.
Abbreviations
CCO, Chief Clinical Officer; CEO, Chief Executive Officer; DALYs, Disability Adjusted Life Years; EDP, Equipment Development Plan; EFY, Ethiopian Fiscal Year; EHF, Equipment History File; EHSTG, Ethiopian Hospitals Transformation Guidelines; EU, European Union; HSTP, Health Sector Transformation plan; IHCS, International Healthcare systems; IPM, Inspection and Preventive Maintenance; IT, Information Technology; MDR, Multi Drug Resistance; MEM, Medical Equipment Management; ME, Medical equipment; MEMM, Medical Equipment Maintenance Management; MEMU, Medical Equipment Management Unit; MRI, Magnetic Resonance Imaging; NICU, Neonatal intensive care unit; SOP, Standard Operational Procedure; WHO, World Health Organization; ZHD, Zonal Health Department.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study received approval from the Institutional Review Board of the Institute of Health, Jimma University in Ethiopia.
Consent for Publication
Participants have consented for the anonymous publication of the data.
Acknowledgments
We would like to extend our appreciation and thank our data collectors, and study participants. We also extend our sincere gratitude to health-care professionals, and managers at Tulu Bolo hospital for providing us with necessary data/information, and for their kind cooperation, and assistance throughout the data collection process. Additionally, we would like to express our heartfelt gratitude to the Jimma University for financially supporting us in the ethical approval process and the official communication of our respective offices and health facilities.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by Jimma University, Ethiopia.
Disclosure
All the authors declare that they have no competing interests for this study, be it financial or non-financial.
References
1. Ren W. Application of intelligent medical equipment management. J Healthc Eng. 2022;2022:56.
2. Willson K, Ison K, Tabakov S. Medical equipment management. Med Equip Manag. 2013;2013:1–310.
3. Medicines and Healthcare products Regulatory Agency. Managing medical devices. Health policy (New York); 2015:60. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/421028/Managing_medical_devices_-_Apr_2015.pdf.
4. Geta ET, Rikitu D, Ewunetu A. Medical equipment utilization efficiency and associated factors at public referral hospitals in East Wollega Zone, Oromia Regional State, Ethiopia. 2022:1–17.
5. Locke RH. Management support system. Fall Ind Eng Conf Am Inst Ind Eng. 1983;65:525–536.
6. Batawalage D, Saranga A. Hospital equipment management in district base hospitals in Kalutara district in Sri Lanka. Biomed Stat Inform. 2017;2(1):18–21.
7. World Health Organization (WHO). WHO list of priority medical devices for cancer management; 2017:252. Available from: http://apps.who.int/iris/bitstream/10665/255262/1/9789241565462-eng.pdf?ua=1.
8. Yao L, Shang D, Zhao H, Hu S. Based on cloud computing and internet of things. 2021.
9. Daba H, Mohammed Aliy T, Lingaiah B. Up to date inventory system for effective management of healthcare technology: case study in Jimma University Specialized Hospital (JUSH). Int J Eng Res. 2017;V6(02):4–7.
10. Bahreini R, Doshmangir L, Imani A. Influential factors on medical equipment maintenance management in search of a framework. 2019.
11. Ministry of Health. Medical equipment management guidelines. 2012:1–188.
12. World Health Organization. WHO Compendium of Innovative Health Technologies for Low-Resource Settings 2022. World Health Organization; 2022.
13. Aruna M, Gunasilan U, Naeem S. Efficient equipment management for biomedical engineering department in the hospital. Int Rev Manage Market. 2018;8(3):69–74.
14. Mutia D, Kihiu J, Maranga S. Maintenance management of medical equipment in hospitals. Plos One. 2012;2(3):58.
15. Com LI. WHO global forum medical devices. 2011.
16. Iadanza E, Gonnelli V, Satta F, Gherardelli M. Evidence-based medical equipment management: a convenient implementation. Med Biol Eng Comput. 2019;57:2215–2230. doi:10.1007/s11517-019-02021-x
17. The Federal Democratic of Ethiopia Ministry of Health. Health sector transformation plan II. 2020.
18. Rattan R, Chambers R, Wakley G. The challenges of quality improvement. Clin Gov Gen Dent Pract. 2019;15:233–240.
19. Semegnew BA. Web-based medical equipment management system in seven referral hospitals. 2018.
20. Diaconu K, Chen Y, Cummins C, Moyao GJ, Manaseki-holland S, Lilford R. Methods for medical device and equipment procurement and prioritization within low- and middle-income countries: findings of a systematic literature review. Glob Health. 2017;13:1–16.
21. Ademe BW, Tebeje B, Molla A, Dror D, Bedi A. Availability and utilization of medical devices in Jimma zone hospitals, Southwest Ethiopia: a case study. BMC Health Serv Res. 2016;16:1–10. doi:10.1186/s12913-016-1523-2
22. Daniel WW. Biostatistics: a foundation for analysis in the health sciences. Biometrics. 1988;44:317. doi:10.2307/2531929
23. Tesfaye S. Procurement, utilization and disposal of medical equipment in the public hospitals of Addis Ababa, Ethiopia. 2013.
24. Tesfaw HM, Hussien K. Assessment on storage conditions of medical laboratory commodities and KAP of store managers at government hospitals in Addis Ababa, Ethiopia. J Multidiscip Res Healthc. 2017;4(1):11–21. doi:10.15415/jmrh.2017.41002
25. Chaudhary P, Kaul P. Factors affecting utilization of medical diagnostic equipment: a study at a tertiary healthcare setup of Chandigarh. Chrismed J Heal Res. 2015;2(4):316. doi:10.4103/2348-3334.165741
26. Perry L, Malkin R. Effectiveness of medical equipment donations to improve health systems: how much medical equipment is broken in the developing world? Med Biol Eng Comput. 2011;49(7):719–722. doi:10.1007/s11517-011-0786-3
27. Keil OR. Management of medical equipment. J Clin Eng. 2007;32(4):136–137. doi:10.1097/01.JCE.0000294895.28147.77
28. The Evolving Medical Devices and Consumer Health Regulatory Framework in Italy, 2022 . Available from: https://practiceguides.chambers.com/home.
29. Jamshidi A, Rahimi SA, Ait-Kadi D, Bartolome AR. Medical devices inspection and maintenance; a literature review.
30. Belachew T, Tilahun G. Review article utilization of donated medical equipments and associated factors in Jimma University Specialized Hospital, Oromia, South West Ethiopia of population and family health, Faculty of Public Health, Jimma University Institute of Health. 2017.
31. USAID. Southern Sudan health. Heal (San Fr). 2007:1–73. Available from: https://www.hfgproject.org/wp-content/uploads/2015/02/Southern-Sudan-Health-System-Assessment.pdf.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
