Back to Journals » Patient Preference and Adherence » Volume 18
Mediating the Role of Perceived Social Support Between Frailty and Self-Perceived Burden in Elderly Patients with Diabetes
Authors Chen MZ, Chen XL, Xu Q, Cao XD, Wang MY, Cao R
Received 30 November 2023
Accepted for publication 16 February 2024
Published 25 March 2024 Volume 2024:18 Pages 745—752
DOI https://doi.org/10.2147/PPA.S452648
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Ming-Zhu Chen,1,* Xiao-Lei Chen,2,* Qin Xu,3 Xiao-Dong Cao,2 Meng-Yu Wang,1 Rong Cao1
1Department of Endocrinology, The Affiliated Wuxi People’s Hospital to Nanjing Medical University, Wuxi, 214001, People’s Republic of China; 2Nursing Department, The Affiliated Wuxi People’s Hospital to Nanjing Medical University, Wuxi, 214001, People’s Republic of China; 3School of Nursing, Nanjing Medical University, Nanjing, 211166, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Qin Xu, School of Nursing, Nanjing Medical University, No. 101 of Longmian Road, Jiangning District, Nanijing, 211166, People’s Republic of China, Tel +86 25-86869553, Fax +86 25-86869555, Email [email protected] Xiao-Dong Cao, Email [email protected]
Objective: To explore the mediating effects of perceived social support between frailty and self-perceived burden (SPB) in elderly patients with diabetes and to provide a theoretical basis for reducing that burden.
Methods: A total of 169 elderly patients with diabetes who were hospitalised in the endocrinology department of a third-class hospital in Wuxi between May 2020 and July 2022 were included in this study using the convenience sampling method. Patients were assessed by the general information questionnaire, the Chinese version of the Tilburg frailty inventory (TFI), the Self-Perceived Burden Scale (SPBS) and the Perceived Social Support Scale (PSSS). The SPSS 22.0 software was used for Pearson’s correlation analysis and multiple linear regression analysis. Model four of the SPSS PROCESS was used for mediating the effect analysis.
Results: The SPBS of elderly patients with diabetes was positively correlated with the TFI (P < 0.01) and negatively correlated with the PSSS (P < 0.01). The results of the Bootstrap test showed that the mediating effect of the PSSS on the relationship between the TFI and the SPBS in elderly patients with diabetes was 0.296 (95% CI: 0.007, 0.066), and the mesomeric effect accounted for 17.3% of the total effect.
Conclusion: The debilitation of elderly patients with diabetes can be reduced by decreasing their SPB through perceived social support. This can be achieved through comprehensive interventions by nurses.
Keywords: elderly patients with diabetes, frailty, self-perceived burden, mediating effects
Introduction
Featuring a long course of disease, diabetes is a risk factor for multiple chronic diseases and may result in a variety of complications.1 Controlling diabetes is influenced by several factors, such as medication, follow-up management and emotional and social support, as physiological and social functions have a serious negative impact on the mental states of patients with diabetes.2 Self-perceived burden (SPB) refers to negative emotions such as anxiety, depression and loneliness, which are caused by physical worries about the illness and psychological stress that encompasses feelings of guilt, dependence and fear of imposing a burden on others during the care-receiving process.3 Recent studies4 have shown that the frailty arising from chronic diseases among elderly patients is in close connection with SPB. Frailty is a senile syndrome mainly characterised by decreased physiological reserve function, multiple organ dysfunction, increased organismal vulnerability and declining anti-stress ability.5 Hyperglycaemia, multiple complications and defects in islet function6 increase the frailty of hospitalised elderly patients with diabetes. The disease progression further restrains their self-care ability and mobility. Their role change in their families and society hinders their recovery and worsens their SPB, which, in turn, further enhances their frailty, causing a vicious cycle. Therefore, it is crucial to remedy the frailty of elderly patients with diabetes to relieve their SPB. Current intervention studies on frailty are weighted in external behaviours, including physical exercise, medication and cognitive training.7 Little emphasis is placed on the subjective perspective of patients, namely, their effective psychological response to their illness and condition.
According to Roy’s Adaptation Model,8 a person is a bio–psycho–social being in constant interaction with a changing environment in which perception and emotions are important psychological adaptation mechanisms. Perceived social support (PSS) is the individual’s subjective experience of being supported, respected and understood. It is an effective way to gain positive emotions and assistance, and it plays an important role in psychological responses.9 The changes in physiological function affect a person’s perceptions, experiences and adaptation levels, which means that frailty levels may also influence PSS. Therefore, this study made the hypothesis that PSS is correlated with frailty and SPB. The mediating factors of PSS were analysed to provide practical enlightenment for alleviating SPB among elderly patients with diabetes.
Methods
Objectives
A total of 169 elderly patients with diabetes who were hospitalised in the endocrinology department of a Grade-A hospital in Wuxi between May 2020 and July 2022 were included in this study. The inclusion criteria were as follows: (1) aged ≥60, according to the United Nations’ definition for elderly people; (2) diagnosed with diabetes;10 (3) did not have mental illnesses or cognitive impairment; (4) were partially self-reliant or completely unable to take care of themselves; (5) voluntarily signed the informed consent form. The exclusion criteria were as follows: (1) were in critical condition and unable to cooperate during this study; (2) were unable to communicate normally. This study was approved by the Ethics Committee of our hospital (No. KY23160). Written informed consent was obtained from all participants or their legal representatives.
According to Kendall’s Tau,11 the sample size should be 5–10 times the number of variables. Considering the invalid sample size, the sample size was increased by 20%, with at least 78–156 candidates.
Applied Tools
- General information questionnaire:The general information questionnaire covered entries such as age, gender, education, medical expenses, living status, primary caregivers, etc.
- Tilburg frailty indicator:Localised by Zamora-Sánchez et al,12 the Tilburg frailty indicator (TFI) involved 15 entries concerning physical, psychological and social frailty, and the binary “yes or no” scoring system was applied. Scores equal to or higher than five points were defined as frailty, and the higher the score was, the more severe the frailty degree was. Cronbach’s alpha coefficient was 0.73.
- Self-Perceived Burden Scale:Introduced by Saji et al,13 the Self-Perceived Burden Scale (SPBS) featured 10 entries from 3 dimensions: economic, physical and emotional burdens, and the five-point Likert scale was applied. According to their scores, the patients were classified as having no SPB when they had a score of 10–19 points, having a light SPB when they had a score of 20–29 points, having a moderate SPB when they had a score of 30–39 points and as having a heavy SPB when they had a score of 40–50 points. Cronbach’s alpha coefficient was 0.9.
- Perceived Social Support Scale:Modified by Lin et al,14 the Perceived Social Support Scale (PSSS) included 12 items in 3 dimensions: family support (4 items), friend support (4 items) and social support (4 items). Each item was scored on a scale of 1–7, with a total score of 12–84 points. Cronbach’s alpha coefficient for each dimension and total dimensions were 0.82, 0.83, 0.79 and 0.90, respectively.
Quality Control
Unified training for the investigators was conducted prior to the study. Before the survey, the purpose of the questionnaire was disclosed to the patients, and informed consent was provided by them. During the survey, the patients were encouraged to fill in the questionnaire independently, and standard guidance language was adopted for any questions. After completion, the questionnaires were collected immediately and checked for any errors or missing information, which were confirmed with the respondents and then corrected to ensure quality.
Statistical methods
The EpiData3.1 software was used for data entry, and the SPSS 22.0 software was used for statistical analysis. The measurement data applied the mean ± standard deviation, and the enumeration data adopted the number of cases and percentages. To evaluate the relationship between SPB, frailty and PSS, Pearson’s correlation and multiple linear regression were used for correlation analysis and multiple linear regression analysis, respectively. The mediating effect was tested using the SPSS PROCESS Macro (Model 4), and a value of P < 0.05 was considered statistically significant. To avoid homological errors, the Harman single-factor test was used to assess common method bias.15
Results
General Information
A total of 176 questionnaires were sent out, 170 were collected and 169 were deemed valid, with an effective return rate of 96.1%. The patients had an average age of 75.74 ± 6.10 years old, comprising 101 men and 68 women (Table 1).
 |
Table 1 General Information of Survey Subjects (n=169) |
Scores of the Tilburg Frailty Indicator, Self-Perceived Burden Scale and Perceived Social Support Scale in Elderly Patients with Diabetes
The total score of the TFI was 7.34 ± 2.13 points, and the scores in each dimension were as follows: physical frailty, 4.54 ± 1.40 points; psychological frailty, 2.21 ± 1.00 points; social frailty, 0.60 ± 2.13 points. The total score of the SPBS was 30.22 ± 7.00 points, and the scores in each dimension were as follows: physical burden, 15.44 ± 4.85 points; emotional burden, 11.46 ± 4.11 points; economic burden, 3.30 ± 1.27 points. The total score of the PSSS was 54.94 ± 12.63, and the scores in each dimension were as follows: family support, 23.00 ± 4.71 points; friend support, 16.73 ± 4.99 points; other support, 15.18 ± 5.58 points.
The Correlation of Self-Perceived Burden, Frailty and Perceived Social Support in Elderly Patients with Diabetes
Pearson’s correlation analysis showed that frailty was positively correlated with SPB (r = 0.388, P < 0.01) and negatively correlated with PSS (r = −0.393, P < 0.01), and PSS was negatively correlated with SPB (r = −0.297, P < 0.01) (Table 2).
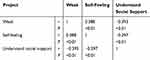 |
Table 2 The Correlation Between Self Perceived Burden and Weakness, Perceived Social Support |
Multiple Linear Regression Analysis of Self-Perceived Burden, Frailty and Perceived Social Support in Elderly Patients with Diabetes
Controlling for potential variables, this study conducted multiple linear regression with the SPBS as the dependent variable. The independent variables included the total statistically significant scores from the TFI and the PSSS, as determined through correlation analysis. The results show that the TFI can positively predict the value of the SPBS and that the PSSS can positively predict the value of the SPBS (Table 3).
 |
Table 3 Multivariate Linear Regression Analysis of Senile Diabetes Weakness, Self Perceived Burden and Perceived Social Support |
The Mediating Effect Analysis of Perceived Social Support
The results showed that there were three factors with characteristic roots >1, and the total variation explained by the first factor was 37.21%, which was lower than the 40% critical standard, indicating no serious common method bias.
The SPSS PROCESS Macro (Model 4) was used to test the mediating effect, with the frailty of elderly patients with diabetes as the independent variable, PSS as the mediating variable and SPB as the dependent variable. The results indicated that frailty could predict PSS (a = −2.326, standard error (SE) = 0.421, P < 0.05). The regression analysis of frailty and PSS was conducted, and the results showed that frailty could predict SPB (c’ = 1.413, SE = 0.337, P < 0.05) and that PSS could predict SPB (b = −0.127, SE = 0.057, P < 0.05). The bias-corrected percentile Bootstrap test indicated a significant mediating effect of PSS on frailty and SPB, with an indirect effect (ab) of 0.296, a Bootstrap SE of 0.163 and a 95% confidence interval of (0.007, 0.066). The mediating effect accounted for ab/(ab + c’) = 17.3% of the total effect, indicating that PSS played a partial mediating role between frailty and SPB (Table 4 and Figure 1).
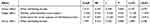 |
Table 4 Analysis of the Mediating Effect of Social Support Between Frailty and Self Perceived Burden |
Discussion
This study analysed the relationship between frailty, SPB and PSS in elderly patients with diabetes, and the results showed that significant pairwise correlations were found among the three factors. Frailty was significantly correlated with SPB (r = 0.388, P < 0.01), and its generating mechanism was related to physical, psychological and social frailty. Social frailty refers to low levels of important social resources, social activities and self-management ability to meet basic social needs. It is a key factor accelerating declines in physical and mental functions. Increasing evidence shows that social frailty has serious consequences for the physical, psychological and spiritual health of elderly patients with diabetes.16 All factors interact with and influence each other. Elderly patients suffering from severe social and psychological frailty often experience more serious physical frailty, which has always been the focus of research on the ageing population problem. This interconnectedness inevitably leads to SPB, where psychological frailty plays a direct role in its manifestation When physical and psychological frailty were controlled, social frailty was still significantly related to SPB.17 Because social frailty is a dynamic process, slowing it down is an important method of alleviating the SPB of elderly patients with diabetes, raising their quality of life and realising a proactive response to ageing.
This study revealed a close relationship between frailty and PSS (r = −0.393, P < 0.01). The more severe the frailty was, the lower the PSS level was. Moreover, PSS remains an important way for elderly patients with diabetes to relieve pressure, gain support and experience positive emotions, which originate from individual cognitive functions.18–20 Diabetes affects neurocognitive areas such as attention, memory, executive ability, mobility and processing ability.21 Patients with diabetes deal with their frailty through common perceptions and past experiences, which create cognitive biases, hindered perceived ability and lowered perception of social support. Consequently, different measures should be taken, such as conducting disease–health education to change patients’ perceptions of their condition, which is a critical approach to enhancing PSS.
In addition, this study indicated that the lower the PSS level was, the heavier the SPB was (r = −0.297, P < 0.01), which was consistent with the research results of Du et al.22 This suggests that the capacity for social cognition, encompassing the ability to contemplate one’s own and others’ mental states for understanding and predicting behaviours, is also deemed a significant predictor of mental health.23 According to sociological theories, people interact with each other through certain expectations, and when their expectations for themselves, other people and the context they are in cannot be met during the interaction, one or more negative emotions arise. Such negative emotions can further grow and eventually produce adverse consequences24 if the interactors cannot obtain support and affirmation from others in time. Self-satisfaction and affirmation for elderly patients with diabetes are effective ways to alleviate their SPB. Narrations of similar stories and the learning and experiencing processes can allow the patients to find their strengths, exercise physiological functions,25,26 raise their living standards and self-management ability and reduce SPB.
This study revealed that the SPB of elderly patients with diabetes and frailty was affected by their PSS. The frailty level of the patients could directly predict their levels of SPB as well as indirectly affect it via PSS. A high level of PSS meant wider acceptance and recognition by others, bringing in a better self-image. Image maintenance could encourage patients to show higher self-confidence when dealing with their condition and life events. It could allow them to better handle depression, anxiety and other emotions caused by physical, psychological and social frailty.4 If an elderly patient who suffers from high physical frailty due to diabetes remains in a state of stress and seldom receives social support from family, friends and society, they will be unwilling to communicate with others, raising their SPB level. Hence, it is imperative not only to secure the material foundation but also to empower individuals to exercise subjective initiative in alleviating (SPB).
Limitations
This study had several limitations due to the COVID-19 pandemic, quarantine measures, social distancing and other factors arising thereof. Furthermore, most of the patients were urban residents, which means that the results may not reflect patients living in the countryside. Therefore, a wider pool of participants is needed for future studies.
Conclusions
Perceived social support plays a mediating role in the direct correlation between frailty and SPB in elderly patients with diabetes. The results provide a new practical perspective for exploring the influencing mechanism between frailty and SPB in those patients.
Implications
When formulating intervention plans and strategies, medical personnel should take a comprehensive consideration of the special needs of elderly patients, and they should encourage their families and society to participate in raising their PSS. Moreover, medical personnel should encourage elderly patients with diabetes to actively participate in disease self-management to reduce their SPB.
Data Sharing Statement
All data generated or analyzed during this study are included in this article.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Nanjing Medical University. Written informed consent was obtained from all participants.
Funding
This work was supported by Nanjing Medical University Science and Technology development fund project (NMUB2019283).
Disclosure
Ming-Zhu Chen and Xiao-Lei Chen are co-first authors for this study. Qin Xu and Xiao-Dong Cao are co-corresponence authors for this study. The authors declare no conflicts of interest in this work.
References
1. Harreiter J, Roden M. Diabetes mellitus-Definition, classification, diagnosis, screening and prevention (Update 2019). Wiener Klinische Wochenschrift. 2019;131:6–15. doi:10.1007/s00508-019-1450-4
2. Zhang Y, Li X, Bi Y, et al. Effects of family function, depression, and self-perceived burden on loneliness in patients with type 2 diabetes mellitus: a serial multiple mediation model. BMC Psychiatry. 2023;23(1):636. doi:10.1186/s12888-023-05122-y
3. Genelin MP, Helmkamp LJ, Steiner JF, et al. Patient pill organization strategies and adherence measured in a cross-sectional study of hypertension. Patient Prefer Adherence. 2023;17:817–826. doi:10.2147/PPA.S399693
4. Narbutt J, Niedźwiedź M, Lesiak A, Ceryn J, Skibińska M. Secukinumab for the treatment of psoriasis in pediatrics: patient selection and acceptability. Patient Prefer Adherence. 2023;17:421–431. doi:10.2147/PPA.S350753
5. Yang Q, Li J, Shi D, et al. Incidence and risk factors associated with hospital-acquired pressure ulcers following total Hip arthroplasty: a retrospective nationwide inpatient sample database study. J Tissue Viability. 2022;31(2):332–338. doi:10.1016/j.jtv.2022.01.004
6. Zhuo M, Hawley CE, Paik JM, et al. Association of sodium-glucose cotransporter-2 inhibitors with fracture risk in older adults with type 2 diabetes. JAMA Network Open. 2021;4(10):e2130762. doi:10.1001/jamanetworkopen.2021.30762
7. Boye KS, Shinde S, Kennedy-Martin T, Robinson S, Thieu VT. Weight change and the association with adherence and persistence to diabetes therapy: a narrative review. Patient Prefer Adherence. 2022;16:23–39. doi:10.2147/PPA.S328583
8. Wang X, Zhang Q, Shao J, Ye Z. Conceptualisation and measurement of adaptation within the Roy adaptation model in chronic care: a scoping review protocol. BMJ Open. 2020;10(e036546). doi:10.1136/bmjopen-2019-036546
9. Yin H, Qian S, Huang F, Zeng H, Zhang CJP, Ming WK. Parent-child attachment and social adaptation behavior in Chinese college students: the mediating role of school bonding. Front Psychol. 2021;12:711669. doi:10.3389/fpsyg.2021.711669
10. Jia W, Weng J, Zhu D, et al. Standards of medical care for type 2 diabetes in China 2019. Diabetes Metab Res Rev. 2019;35(6):e3158. doi:10.1002/dmrr.3158
11. Chang YH, Yang CT, Hsieh S. Social support enhances the mediating effect of psychological resilience on the relationship between life satisfaction and depressive symptom severity. Sci Rep. 2023;13(1):4818. doi:10.1038/s41598-023-31863-7
12. Zamora-Sánchez JJ, Urpí-Fernández AM, Sastre-Rus M, et al. The Tilburg Frailty Indicator: a psychometric systematic review. Ageing Res Rev. 2022;76:101588. doi:10.1016/j.arr.2022.101588
13. Saji A, Oishi A, Harding R. Self-perceived burden for people with life-threatening illness: a qualitative systematic review. J Pain Symptom Manage. 2023;65(3):e207–e217. doi:10.1016/j.jpainsymman.2022.10.016
14. Lin XD, Xu GR, Chen GJ, Xiao HM. Self-perceived burden predicts lower quality of life in advanced cancer patients: the mediating role of existential distress and anxiety. BMC Geriatr. 2022;22(1):803. doi:10.1186/s12877-022-03494-6
15. Yu X, Zhao J. How rumination influences meaning in life among Chinese high school students: the mediating effects of perceived chronic social adversity and coping style. Front Public Health. 2023;11:1280961. doi:10.3389/fpubh.2023.1280961
16. Cordes T, Bischoff LL, Schoene D, et al. A multicomponent exercise intervention to improve physical functioning, cognition and psychosocial well-being in elderly nursing home residents: a study protocol of a randomized controlled trial in the PROCARE project. BMC Geriatr. 2019;19(1):369. doi:10.1186/s12877-019-1386-6
17. Zhang X, Tan SS, Franse CB, et al. Association between physical, psychological and social frailty and health-related quality of life among elderly people. Eur J Public Health. 2019;29(5):936–942. doi:10.1093/eurpub/ckz099
18. Förster K, Danzer L, Redlich R, et al. Social support and hippocampal volume are negatively associated in adults with previous experience of childhood maltreatment. J Psychiatry Neurosci. 2021;46(3):E328–E336. doi:10.1503/jpn.200162
19. Sato W, Kochiyama T, Kubota Y, et al. The association between perceived social support and amygdala structure. Neuropsychologia. 2016;85:237–244. doi:10.1016/j.neuropsychologia.2016.03.036
20. Qi R, Luo Y, Zhang L, et al. Social support modulates the association between PTSD diagnosis and medial frontal volume in Chinese adults who lost their only child. Neurobiol Stress. 2020;13:100227. doi:10.1016/j.ynstr.2020.100227
21. Xu W, Hu X, Zhang X, Ling C, Wang C, Gao L. Cognitive impairment and related factors among middle-aged and elderly patients with type 2 diabetes from a bio-psycho-social perspective. Diabetes Metab Syndr Obes. 2021;14:4361–4369. doi:10.2147/DMSO.S333373
22. Du F. The Effect of Perceived Social Support on Self-Perceived Burden and Life Quality in Elderly Patients with Heart Failure. Gansu Province: Lanzhou University; 2021.
23. Isernia S, Baglio F, d’Arma A, Groppo E, Marchetti A, Massaro D. Social mind and long-lasting disease: focus on affective and cognitive theory of mind in multiple sclerosis. Front Psychol. 2019;10:218. doi:10.3389/fpsyg.2019.00218
24. Wells J, Crilly P, Kayyali R. A systematic analysis of reviews exploring the scope, validity, and reporting of patient-reported outcomes measures of medication adherence in type 2 diabetes. Patient Prefer Adherence. 2022;16:1941–1954. doi:10.2147/PPA.S375745
25. Tang M, Wang D, Guerrien A. A systematic review and meta-analysis on basic psychological need satisfaction, motivation, and well-being in later life: contributions of self-determination theory. Psych J. 2020;9(1):5–33. doi:10.1002/pchj.293
26. Hamilton JE, Blanco E, Selek S, et al. Patient and provider perspectives on medication non-adherence among patients with depression and/or diabetes in diverse community settings - a qualitative analysis. Patient Prefer Adherence. 2022;16:1581–1594. doi:10.2147/PPA.S328785
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

