Back to Journals » Clinical Ophthalmology » Volume 16
Low Diopter Phakic Implantable Collamer Lens: Refractive and Visual Outcomes in Low Myopia and Myopic Astigmatism
Authors Alonso-Juárez E, Velázquez-Villoria D
Received 27 May 2022
Accepted for publication 23 August 2022
Published 2 September 2022 Volume 2022:16 Pages 2969—2977
DOI https://doi.org/10.2147/OPTH.S373378
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Ernesto Alonso-Juárez,1 Daniel Velázquez-Villoria2
1INSADOF Clinic, Salamanca, Spain; 2Villoria Clinic, Vigo & Pontevedra, Spain
Correspondence: Ernesto Alonso-Juárez, INSADOF, Calle Doctrinos, 4, 1, Salamanca, 37002, Spain, Email [email protected]
Purpose: Nowadays the Implantable Collamer Lens (ICL – STAAR Surgical. Monrovia. CA) is a refractive surgical technique offered not only when laser corneal correction is not possible but also when the patient requires premium quality indexes and when dry eye is a concern. The use of ICL phakic lenses in low myopic patients is an emanate factor to study and analyze in order to determine treatment predictability and stability in such patients. In this paper, we conducted a 1-year follow-up study on patients with myopia below − 3.5D implanted with ICL lenses.
Methods: This was a retrospective analytical study that includes patients with phakic ICL implantation from 2 independent clinics with a minimum follow-up of 12 months. Visual acuity, refractive outcomes, vault, and intraocular pressure (IOP) were assessed at 1, 6 and 12 months.
Results: Eighty-two eyes from 82 patients were included in this analysis. Mean spherical equivalent was − 2.34 ± 0.82 (Range − 5.50 to − 1.00 D). Mean spherical implanted ICL power was − 3.04 ± 0.78 D. In 25 eyes (30.5%) a Toric-ICL (TICL) was implanted with a mean TICL cylinder power of +1.64± 0.64. Efficacy and security index remained stable for 12 months at 1.07 and 1.09, respectively. Mean vault at 12 months was 513.78 ± 262.87 μm and IOP was 15.63 ± 2.17 mmHg.
Conclusion: Phakic Implantable Collamer Lens implantation in very low myopia is a predictable, stable, safe, and effective technique with high efficacy and security indexes. Low diopter Toric ICL is also an excellent option for refractive surgery in cases of low diopter astigmatism.
Keywords: low myopia, phakic intraocular low power lens, refractive surgery
Introduction
Refractive surgery is defined as a set of techniques that modify the eye’s refractive state and may be considered when a patient wishes to reduce dependence on glasses or contact lenses.1 When the procedure permanently alters the corneal shape and anatomy, it is defined as corneal refractive surgery; another technique is to implant an intraocular lens (IOL) into the anterior or posterior chamber without removing the crystalline lens (phakic intraocular lens – pIOL) or replacing the crystalline lens with an intraocular lens with the necessary power to reduce ametropia (refractive lensectomy).1 Since retinal detachment is a well-known risk in young patients with high myopia,2,3 the use of refractive lensectomy is limited to patients over 50–55 years. Therefore, laser vision correction (LVC) or pIOL implantation are the most commonly used refractive surgery techniques in young myopic patients.
Corneal techniques have limitations in their use for high refractive errors leading to less biomechanical stability, worse refractive predictability and stability, poorer visual quality and risk of corneal ectasia.4 Nowadays, the use of corneal surface LVC is recommended for low-to-moderate myopias up to −7.50D and −5.00D in spherical equivalent for LASIK and PRK, respectively.5 It has also been shown that laser assisted keratomileusis (LASIK), and to a lesser extent photorefractive keratectomy (PRK), can induce dry-eye symptoms.6–8 Despite this, corneal surface laser vision correction (LASIK, PRK) has an extensive track record and scientific evidence has proven its effectiveness and safety as a refractive treatment offering reliable and predictable results over the last 20 years of follow-up.9–11
On the other hand, it is well known that pIOL implantation is an effective and safe technique for moderate-to-high myopias.4 EVO Visian Implantable collamer lens (ICL) (STAAR Surgical, Monrovia, CA) is the leading and most widely used option today with more than 2 million implants worldwide (Staar surgical, press release June 7th 2022). There are numerous papers confirming the ICL implantation efficacy and safety with long-term follow-up.12–15 The ICL implant technique offers several benefits including reversibility, cornea preservation, retreatment option, lens interchangeability and the upgradeable option without altering the corneal anatomy or introducing high order optical aberrations.4,13,36 These features, in addition to improving visual quality in high myopes, led us to consider using this technique for all suitable diopter ranges rather than limiting these benefits only to patients who are not candidates for corneal laser surgery. Myopia correction with phakic intraocular lenses in moderate-to-high myopia has been a topic of interest throughout the evolution of ICLs with excellent results in predictability, safety, efficacy, and stability. In view of these results, few articles have been published on the use of phakic lenses as a surgical option for the correction of low myopia. To our knowledge, there is no research that has exclusively analyzed the results of ICL implantation in myopia lower than −3.50 D. Using pIOL in low diopter patients (up to −6.00D) has shown positive results. The pIOL predictability and visual outcomes for low myopias are comparable to pIOL implantations in moderate or high myopia.16–18
ICL optical quality is also very good, regardless of lens power (even better at low powers).19 Recently, other authors compared visual and refractive results of ICL implants versus LASIK in low myopia (−4.00 to −7.88D), concluding that ICL was safer and more effective than LASIK.20 However, to our knowledge, no results have been published to date evaluating the ICL lens implantation predictability, safety and efficacy in patients with very low myopia (below −4.00D). So, this is the first paper to evaluate the refractive and visual outcomes of EVO ICL implantation in patients with very low myopia.
Patients and Method
This was a retrospective analytical observational study. Patients undergoing refractive surgery with EVO Visian ICL lens implants at the Instituto Salmantino de Oftalmología (INSADOF – Salamanca, Spain) and at Clínica Villoria (Vigo – Pontevedra, Spain) between 2016 and 2020 were included. Patients showed a preoperative myopia refraction or myopic astigmatism lower than −4.00D sphere, they were suitable for laser corneal refractive surgery or intraocular surgery with phakic lens and had a minimum follow-up of 12 months. As all subjects were candidates for laser corneal refractive surgery and phakic lens implantation, the surgeon explained both techniques detailing their corresponding pros and cons. Patients chose the phakic lens implantation mainly to preserve their cornea and because the ICL is removable facilitating any future ophthalmology procedure. Only one eye per patient was included in the analysis, with random selection.
Patients should have a minimum anterior chamber depth (ACD) measurement of 2.8mm, measured from the corneal endothelium to the anterior crystalline capsule, without ophthalmological alterations contraindicating refractive surgery with phakic lens implantation. Subjective refraction should be stable at least for last 12 months (a variation of <0.50 D), without ocular pathologies or other intraocular ophthalmic surgeries.
The exclusion criteria included shallow anterior chamber depth <2.8mm, refractive error higher than −3.50D sphere, cataract, glaucoma or retinal detachment, macular degeneration, unilateral vision and history of ocular inflammation.
Objectives
- To analyze the refractive predictability and visual outcomes of EVO Visian ICL lens implantation in subjects with myopia lower than −3.50 D.
- To establish the safety and efficacy indices of the procedure, and to analyze the refractive, vault and intraocular pressure stability at 12-month follow-up.
Pre-Op and IOL Calculation
A complete ophthalmology examination was performed in the preop, including subjective and cycloplegic refraction, uncorrected and corrected distance visual acuity (UDVA and CDVA), corneal topography with a Scheimpflug-based device (Pentacam HR – Oculus Optikgeräte GmbH, Wetzlar, Germany) obtaining horizontal corneal diameter (WTW), anterior chamber depth (ACD) measured from corneal endothelium to anterior capsule of crystalline lens and central corneal thickness (CCT), optical biometry (IOLMaster – Zeiss Humphrey, Carl Zeiss Meditec, Inc., Dublin, CA) obtaining axial length (AL) and simulated keratometry (K) and anterior segment optical coherence tomography (AS-OCT) (Visante – Zeiss Humphrey, Carl Zeiss Meditec, Inc., Dublin, CA) obtaining angle-to-angle distance (ATA), and intraocular pressure (IOP) with Goldman tonometer. ICL power and sizing was calculated using the manufacturer's online software (Online Calculation and Ordering System – OCOS. STAAR Surgical AG. Monrovia, CA). Toric-ICL was implanted when refractive cylinder was greater than 1.00 D.
Surgical Technique
Patients underwent ICL implantation surgery under local and intracamerular anaesthesia (oxybuprocaine chlorhydrate and lidocaine). Surgical technique has been previously described by other authors.15,21 In all cases, a 3.2 mm incision was performed on clear corneal, at temporal meridian. Anterior chamber was filled with methylcellulose or cohesive ophthalmic viscoelastic device (OVD). Lens was injected through the main corneal incision and haptics were situated under the iris, and finally an OVD wash was performed with BSS injected in the anterior chamber.
Follow-Up
Follow-up visits were established after 24 hours, 1 week, 1, 3, 6 and 12 months. Only data from 1, 6 and 12 months were included in the analysis. During each visit, a similar protocol was performed obtaining UDVA, CDVA, subjective refraction, IOP, and vault distance measured with AS-OCT (as the distance between the central posterior surface of the phakic lens and the anterior capsule of the crystalline lens). All this data was included in a spreadsheet created for this study for posterior statistical analysis.
Statistics
The sample size, calculated according to the standard deviation of the corrected spherical equivalent from a pilot analysis, indicated that a minimum of 71 subjects would be needed for a minimum detectable difference of 0.05D (1/3 SD), accepting an alpha risk of 0.05 and a beta risk of 0.2 in bilateral contrast. This sample size was calculated using Granmo software (ver. 7.12 – Institut Municipal d’Investigació Mèdica, Barcelona, Spain). Kolmogorov Smirnov normality test was performed to describe the sample normality, while paired means t-student tests were performed to compare means and R Pearson linear correlation was used to analyze procedure predictability.
Database was analyzed using SPSS software (IBM Corp., version 22.0) with descriptive statistics, paired means analysis and linear correlation for predictability analysis.
Results
Eighty-two eyes from 82 subjects were finally included in this analysis. Descriptive statistics data is described in Table 1. Mean age was 35.06 ± 8.46 (range 21 to 56 years) and mean spherical equivalent was −2.34 ± 0.82 (Range −5.50 to −1.00D). There were 2 subjects who underwent ICL implantation for a refractive error correction after laser corneal surgery (LASIK), and they had mean keratometry under 40D.
 |
Table 1 Descriptive Statistics of Sample |
Mean spherical implanted ICL power was −3.04D (range −1.25 to −4.50, median −3.00). In 25 eyes (30.5%) a Toric-ICL (TICL) was implanted, mean TICL cylinder power was +1.64D (range +0.50 to +3.00, median +1.50). The most implanted ICL size was 13.2mm (n = 50, 61.0%), followed by 12.6 mm (n = 20, 24.4%), 13.7 mm (n = 11, 13.4%) and 12.1 mm (n = 1, 1.2.%).
Refractive and visual outcomes, vault and IOP evolution after 1, 6 and 12 months are described in Table 2. UDVA and CDVA did not suffer statistical differences in any of the follow-up; therefore, the efficacy and security index remain stable for 12 months, around 1.07 and 1.09, respectively.
 |
Table 2 Refractive and Visual Outcomes at 1, 6 and 12 Months after Surgery |
SEQ and cylinder predictability are shown in Figure 1. Linear correlation between preop SEQ & cylinder and achieved SEQ & cylinder at 12-month follow-up was positive and statistically significant in both cases (Pearson R = 0.965; R2 = 0.965 p < 0.001 for SEQ and R = 0.963; R2 = 0.928; p > 0.001 for cylinder).
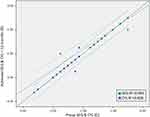 |
Figure 1 Mean spherical equivalent and cylinder predictability at 12 months. R2 = 0.965 and 0.928 for SEQ and CYL, respectably. |
Vault evolution showed a positive and statistically significant linear correlation with a reduction of 39.21 ± 81.35 µm at 12 months (Pearson R = 0.949; R2= 0.901; p < 0.001) (Figure 2). At one month, mean vault was 573.33 ± 239.77 µm, at 6 months 544.67 ± 260.98 µm and at 12 months 513.78 ± 262.87 µm. Paired mean analysis showed statistically significant differences from 1 to 6 months (p = 0.009), 1–12 months (p = 0.010); however, 6–12 month means did not show statistically significance differences (p = 0.191).
 |
Figure 2 Vault evolution, and vault correlation between vault measurement at 1 month and at 12 months. |
Mean IOP did not suffer significant changes in the follow-up, and the difference between preop IOP and IOP after 12 months did not show statistical significance (p = 0.587).
Refractive stability is described in Figure 3. There was a statistical difference between pre- and post-surgical refraction in SEQ and cylinder (p < 0.001 in both cases), and the refractive outcomes remain stable in the rest of measurements up to 12 months, in SEQ and cylinder (p > 0.05 in all cases).
 |
Figure 3 Refractive stability at 12-month follow-up. |
Discussion
The phakic collamer lens implantation in patients with moderate-to-high myopia has been previously described as a safe and effective technique,22 and up to 10-year follow-ups have been published in this population group with very good refractive and visual outcomes.12,15,23,24 Similarly, refractive surgery with laser corneal ablation in low-to-moderate myopia (LASIK, PRK or SMILE) has also shown a high level of safety in long-term follow-ups.25 However, it has also been confirmed that corneal shape modification produces a certain degree of high-order aberrations (HOAs) since the cornea is the first element in the optical system.26 Even the topography-guided laser treatments induce HOAs that could affect visual quality.26,27 Dry-eye disease (DED) has also been described as a side effect after LVC, mainly after LASIK, where corneal innervation damage induces a reduction of corneal sensitivity and other mechanisms with a neurotrophic effect.6–8,28 Pre-existing dry eye has been reported as a risk factor for severe postoperative dry eye with staining of the ocular surface and severe symptoms.6 Despite these side effects, laser vision correction offers an improvement in quality of life when compared to using glasses or contact lenses.29–31
Since life expectancy in developed countries far exceeds age-related cataract formation, all subjects will most likely have to consider an ophthalmologic surgery over the course of their lifetime. Corneal shape and HOAs are a decisive factor for intraocular lens (IOL) selection in presbyopia-correction crystalline surgery related to visual function and optical quality.32 HOAs can reduce contrast sensitivity (SC) and dysphotopsia phenomena. In addition, corneal refractive surgery alters the relation between anterior and posterior corneal curvature making the standardized keratometric index inappropriate. This requires additional evaluation to be made in the lens power calculation process, which may reduce the biometric calculation accuracy.32
Therefore, if phakic IOL (pIOL) implantation with the most recent ICL model is a safe and effective procedure in moderate-to-high myopic patients and offers the associated advantages of maintaining corneal integrity and easy lens explantation while facilitating future ophthalmology-related surgeries, why limit phakic IOL implantation exclusively to those patients who are not candidates for laser corneal surgery?
To date, several papers have been published evaluating low-moderate myopia and ICL implantations,16–18,20 but none of them included very low myopic subjects with less than −3.50 D in spherical equivalent (SEQ). Sanders and Vukich published another paper comparing ICL implantation versus LASIK in low myopia.20 They describe a mean SEQ of −6.4 D in ICL group and −5.6 in LASIK group, concluding that ICL was more predictable and stable than LASIK. Therefore, they determined it would be an alternative to corneal refractive surgery in the treatment of low myopia.20 Regarding ICL implantation results in low myopia as a proprietary technique, Dougherty and Priver described their results in low myopic patients (mean SEQ −6.96 D) with up to 50 months of follow-up.16
The most recent study on low myopia and ICL implantation was written by Pinto, Monteiro et al.18 In this research, the authors compared visual and refractive outcomes of ICL implantation in 2 groups of subjects, with low (<-6.00 D) and high myopia (>−6.00 D). The low myopia group had a mean SEQ of –4.89 D like the Kamiya study, but with a follow-up of at least one year. Our research presents even lower refractive data with a mean SEQ of −2.34 ± 0.82 D making it the first paper to evaluate ICL outcomes in very low myopia subjects with less than −3.50 D.
Regarding astigmatism correction, in this research TICL was implanted when refractive cylinder was >0.75D or clinically significant (30.5% of cases), ie the patient improves CDVA by 1 or more lines by refractively compensating the cylinder when compared to correction with SEQ. Mean TICL Cyl power was +1.64 D, which corresponds to a mean preop refractive cylinder of −1.21 D (Table 1). Our astigmatism correction with TICL results are very good, with a residual cylinder at 12 months of −0.02D. Correlation between target and achieved cylinder also shows very good behavior (R2= 0.928). This is in line with the results described by Cano-Ortiz et al in their recent publication on low power astigmatism correction with TICL lenses.33 In their article, Cano indicates a mean preop power of −1.50D Cyl, which is in line with our preop data. They obtained a cylinder correction accuracy equivalent to ours (R2= 0.942) confirming the stability and predictability of the procedure.
To assess the safety and efficacy of the treatment we used the efficacy and safety indices. The efficacy index is described as the ratio of post-operative UDVA to pre-operative CDVA. If the treatment is equal to or greater than 1, the patient achieves a post-operative UDVA equal to or greater than the pre-operative CDVA. In this scenario, the refractive surgery is effective. Safety refers to the certainty that the patient does not lose lines of CDVA in surgery. The procedure is considered safe if post-op CDVA is equal to or better than the pre-op CDVA, even if the refractive error is not completely corrected. Finally, the change in SEQ indicates the stability of the refractive procedure during the 12-month follow-up. If there are changes in refraction, either by refractive enhancement, stabilization of the procedure or refractive regressions, there will be a significant change in SEQ at follow-up.
At 12 months, mean Efficacy Index in the Pinto & Monteiro’s paper was 1.05 ± 0.17, very similar to the efficacy index obtained in our study at the 12-month follow-up (1.07 ± 0.15). Regarding the Security Index, Pinto & Monteiro reported an index of 1.13 ± 0.18, compared to ours at 1.09 ± 0.13, confirming the strength of our data. Pinto & Monteiro’s data are similar to ours when observing refractive stability after treatment. In our case, mean SEQ after surgery changed from −0.04 ± 0.15 at 1 month to −0.07 ± 0.16 at 6 months and −0.03 ± 0.16 D at 12 months, without significant differences between them (p > 0.05 in all cases). Pinto & Monteiro reported changes of −0.07 ± 0.25 D from 1 to 12 months (p = 0.74), showing our data to be even more stable.
Our results support the idea that ICL implantation in very low myopia (<-3.50 D) is equivalent to ICL implantation in low myopia (<-6.00 D) in terms of safety, efficacy and SEQ change. Our study confirms that ICL implantation is a very good alternative to LVC for low myopia patients while also offering the previously mentioned advantages: reversibility, corneal compliance, non-induction of dry eye and excellent visual quality.
Compared with results described in low myopia refractive surgery with LVC, our outcomes show very good results. Gershoni et al compared trans-PRK and femtosecond assisted LASIK in low myopia and described their results with preop SEQ of −3.43 ± 1.27 D in the PRK group and −3.18 ± 1.34 D in the LASIK group. Efficacy and safety index were 0.95 ± 0.14 and 0.96 ± 0.13, respectively, in the PRK group and 0.98 ± 0.12 and 0.99 ± 0.12, respectively, in the LASIK group.35
Regarding intraocular pressure (IOP), our results show stability without significant changes along the entire follow-up, without significant differences between preop and follow-up in 1, 6 and 12 months (p value >0.05 in all cases). This is also in line with results described by Pinto & Monteiro, as they reported a mean IOP of 15.2 and 15.1 for preop and 12-month revision. Our data show similar results with mean IOP 15.68 ± 2.68 and 15.63 ± 2.17 in preop and 12 months.
Central Vault measurement also show similar behavior: in our case vault changed from 559 ± 228 in the first month after surgery to 545 ± 261 at 6 months (p = 0.009) and 514 ± 263 at 12 months (p = 0.001). This indicates a mean difference of −39 ± 81 µm in the first 12 months of follow-up. This vault evolution over time is similar to the results described by Alfonso et al, reporting that most cases showed higher vault reduction in the first 6 months after the surgery, but with a mean difference in the vault of −41 ± 64 µm in 12 months, equivalent to our data.34 It is worth noting the methodical difference in these studies. In our case, the follow-up was linear from preoperative to 12 months while in Alfonso’s study independent measurements were made throughout the follow-up without considering the linear evolution.
In conclusion, Visian ICL implantation in very low myopia is a predictable, stable, safe, and effective technique with high efficacy and security indexes. Low diopter Toric ICL is also an excellent option for refractive surgery in cases of low diopter astigmatism.
Data Sharing Statement
The datasets during and/or analyzed during the current study available from the corresponding author on reasonable request.
Ethics Approval
This work is exempt from evaluation by an ethics committee since it is a retrospective analysis of results, according to the secretariat of the clinical research ethics committee CEIm – Área de salud de Salamanca – Complejo asistencial Universitario de Salamanca – Spain. All data accessed in this analysis complied with relevant data protection and privacy regulation.
Signed informed consent to analyze refractive and visual data was obtained from every subject participating in this study. Institutional consent form is attached.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
No funding sources were available for this work.
Disclosure
The authors declare that they have no competing interests. The authors did not receive any financial support from any public or private sources.
References
1. Chuck RS, Jacobs DS, Lee JK, et al. Refractive errors & refractive surgery preferred practice pattern. Am Acad Ophthalmol. 2017;125(1):P1–P104. doi:10.1016/j.ophtha.2017.10.003
2. Javaloy J, Druchkiv V, Beltrán J, et al. Retinal detachment after phacoemulsification in refractive surgery clinics: a large series analysis with variable follow-up during 16 years. Graefe’s Arch Clin Exp Ophthalmol. 2021;259(6):1555–1567. doi:10.1007/s00417-021-05160-w
3. Laube T, Brockmann C, Lehmann N, Bornfeld N, Wedrich A. Pseudophakic retinal detachment in young-aged patients. PLoS One. 2017;12(8):1–19. doi:10.1371/journal.pone.0184187
4. Huang D, Schallhorn SC, Sugar A, et al. Phakic intraocular lens implantation for the correction of myopia. Ophthalmology. 2009;116(11):2244–2258. doi:10.1016/j.ophtha.2009.08.018
5. Gil JQ, Lobo C, Tavares C, et al. Guidelines for excimer laser refractive surgery on cornea. Rev Soc Port Oftalmol. 2015;39(1):2–16. doi:10.48560/rspo.6907
6. Toda I. Dry Eye After LASIK. Investig Opthalmology Vis Sci. 2018;59(14):DES109. doi:10.1167/iovs.17-23538
7. Wilkinson JM, Cozine EW, Kahn AR. Refractive eye surgery: helping patients make informed decisions about LASIK. Am Fam Physician. 2017;95(10):637–644.
8. Sambhi RDS, Sambhi GDS, Mather R, Malvankar-Mehta MS. Dry eye after refractive surgery: a meta-analysis. Can J Ophthalmol. 2019;54(1):1–7. doi:10.1016/j.jcjo.2019.07.005
9. Li S-M, Zhan S, Li S-Y, et al. Laser-assisted subepithelial keratectomy (LASEK) versus photorefractive keratectomy (PRK) for correction of myopia. Cochrane Database Syst Rev. 2016;2(2). doi:10.1002/14651858.CD009799.pub2
10. Shortt AJ, Allan BD, Evans JR. Laser-assisted in-situ keratomileusis (LASIK) versus photorefractive keratectomy (PRK) for myopia. Cochrane Database Syst Rev. 2013;(1). doi:10.1002/14651858.CD005135.pub3
11. Shortt AJ, Allan BD. Photorefractive keratectomy (PRK) versus laser-assisted in-situ keratomileusis (LASIK) for myopia. In: Shortt AJ, editor. Cochrane Database of Systematic Reviews. Chichester, UK: John Wiley & Sons, Ltd; 2006:CD005135. doi:10.1002/14651858.CD005135.pub2
12. Fernández-Vega-Cueto L, Alfonso-Bartolozzi B, Lisa C, Madrid-Costa D, Alfonso JF. Seven-year follow-up of posterior chamber phakic intraocular lens with central port design. Eye Vis. 2021;8(1):1–9. doi:10.1186/s40662-021-00247-1
13. Montes-Mico R, Ruíz-Mesa R, Rodríguez-Prats JL, Tañá P, Posterior-chamber phakic implantable collamer lenses with a central port: a review. Acta Ophthalmol. 2020;99(3):e288–e301. doi:10.1111/aos.14599
14. Nakamura T, Isogai N, Kojima T, Yoshida Y, Sugiyama Y. Posterior chamber phakic intraocular lens implantation for the correction of myopia and myopic astigmatism: a retrospective 10-year follow-up study. Am J Ophthalmol. 2019;206:1–10. doi:10.1016/j.ajo.2019.04.024
15. Alfonso JF, Fernández-Vega-Cueto L, Alfonso-Bartolozzi B, Montés-Micó R, Fernández-Vega L. Five-year follow-up of correction of myopia: posterior chamber phakic intraocular lens with a central port design. J Refract Surg. 2019;35(3):169–176. doi:10.3928/1081597X-20190118-01
16. Dougherty PJ, Priver T. Refractive outcomes and safety of the implantable collamer lens in young low-to-moderate myopes. Clin Ophthalmol. 2017;11:273–277. doi:10.2147/OPTH.S120427
17. Kamiya K, Shimizu K, Igarashi A, et al. Posterior chamber phakic intraocular lens implantation: comparative, multicentre study in 351 eyes with low-to-moderate or high myopia. Br J Ophthalmol. 2018;102(2):177–181. doi:10.1136/bjophthalmol-2017-310164
18. Pinto C, Monteiro T, Franqueira N, Faria-Correia F, Mendes J, Vaz F. Posterior chamber collamer phakic intraocular lens implantation: comparison of efficacy and safety for low and moderate-to-high myopia. Eur J Ophthalmol. 2021;(1):1–8. doi:10.1055/b-0037-142056
19. Pérez-Vives C, Domínguez-Vicent A, Ferrer-Blasco T, Pons ÁM, Montés-Micó R. Optical quality of the Visian implantable collamer lens for different refractive powers. Graefe’s Arch Clin Exp Ophthalmol. 2013;251(5):1423–1429. doi:10.1007/s00417-012-2200-8
20. Sanders D, Vukich JA. Comparison of implantable collamer lens (ICL) and laser-assisted in situ keratomileusis (LASIK) for low myopia. Cornea. 2006;25(10):1139–1146. doi:10.1097/ICO.0b013e31802cbf3c
21. Alfonso JF, Lisa C, Fernández-Vega Cueto L, Belda-Salmerón L, Madrid-Costa D, Montés-Micó R. Clinical outcomes after implantation of a posterior chamber collagen copolymer phakic intraocular lens with a central hole for myopic correction. J Cataract Refract Surg. 2013;39(6):915–921. doi:10.1016/j.jcrs.2013.01.036
22. Tang Y, Ye J. Phakic posterior chamber intraocular lens with a central hole in treating patients with moderate to high myopia: a meta-analysis. J Ophthalmol. 2019;2019:1–7. doi:10.1155/2019/9496326
23. Choi JH, Lim DH, Nam SW, Yang CM, Chung ES, Chung T-Y. Ten-year clinical outcomes after implantation of a posterior chamber phakic intraocular lens for myopia. J Cataract Refract Surg. 2019;45(11):1555–1561. doi:10.1016/J.JCRS.2019.06.015
24. Fernández-vega- L, Lisa C, Montés-micó R, Alfonso JF, Alfonso J. Implantable collamer lens with central hole: 3-year follow-up. Clin Ophthalmol. 2018;12:2015–2029. doi:10.2147/OPTH.S171576
25. Taneri S, Knepper J, Rost A, Dick HB. Long-term outcomes of PRK, LASIK and SMILE. Ophthalmologe. 2021. doi:10.1007/S00347-021-01449-7
26. Wang J, Ren Y, Liang K, Jiang Z, Tao L. Changes of corneal high-order aberrations after femtosecond laser-assisted in situ keratomileusis. Medicine. 2018;97(18):e0618. doi:10.1097/MD.0000000000010618
27. Al-Zeraid FM, Osuagwu UL. Induced higher-order aberrations after Laser In Situ Keratomileusis (LASIK) performed with wavefront-guided IntraLase femtosecond laser in moderate to high astigmatism. BMC Ophthalmol. 2016;16(1):29. doi:10.1186/s12886-016-0205-5
28. Levitt AE, Galor A, Weiss JS, et al. Chronic dry eye symptoms after LASIK: parallels and lessons to be learned from other persistent post-operative pain disorders. Mol Pain. 2015;11:
29. Klokova OA, Sakhnov SN, Geydenrikh MS, Damashauskas RO. Quality of life after refractive surgery: reLEx SMILE vs Femto-LASIK. Clin Ophthalmol. 2019;13:561–570. doi:10.2147/OPTH.S170277
30. Pesudovs K, Garamendi E, Elliott DB. A quality of life comparison of people wearing spectacles or contact lenses or having undergone refractive surgery. J Refract Surg. 2006;22(1):19–27. doi:10.3928/1081-597x-20060101-07
31. Kobashi H, Kamiya K, Igarashi A, Matsumura K, Komatsu M, Shimizu K. Long-term quality of life after posterior chamber phakic intraocular lens implantation and after wavefront-guided laser in situ keratomileusis for myopia. J Cataract Refract Surg. 2014;40(12):2019–2024. doi:10.1016/j.jcrs.2014.03.028
32. Goto S, Maeda N. Corneal topography for intraocular lens selection in refractive cataract surgery. Ophthalmology. 2020;128(11):e142–e152. doi:10.1016/j.ophtha.2020.11.016
33. Cano-Ortiz A, Sánchez-Ventosa Á, Membrillo A, et al. Astigmatism correction with toric implantable collamer lens in low and high astigmatism groups. Eur J Ophthalmol. 2021;32(1):183–192. doi:10.1177/1120672121999991
34. Alfonso JF, Fernández-Vega L, Lisa C, Fernandes P, González-Meijome J, Montés-Micó R. Long-term evaluation of the central vault after phakic Collamer® lens (ICL) implantation using OCT. Graefe’s Arch Clin Exp Ophthalmol. 2012;250(12):1807–1812. doi:10.1007/s00417-012-1957-0
35. Gershoni A, Reitblat O, Mimouni M, Livny E, Nahum Y, Bahar I. Femtosecond laser assisted in situ keratomileusis (FS-LASIK) yields better results than transepithelial photorefractive keratectomy (Trans-PRK) for correction of low to moderate grade myopia. Eur J Ophthalmol. 2021;31(6):2914–2922.
36. Igarashi A. Posterior chamber phakic IOLs vs. LASIK: benefits and complications. Expert Rev Ophthalmol. 2019;14(1):43–52. doi:10.1080/17469899.2019.1571910
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
