Back to Journals » Clinical Ophthalmology » Volume 18
Long Term Evaluation of Surgically Induced Astigmatism and Corneal Higher-Order Aberrations After 2.2 Mm Clear Corneal Incisions in Femtosecond Laser-Assisted Cataract Surgery: Temporal versus Superior Approach
Authors Cao X, Shao J, Zhang Y, Zheng L, Zhang J
Received 21 December 2023
Accepted for publication 16 April 2024
Published 20 April 2024 Volume 2024:18 Pages 1067—1082
DOI https://doi.org/10.2147/OPTH.S456110
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Xinfang Cao, Jie Shao, Yonggang Zhang, Li Zheng, Jun Zhang
Department of Ophthalmology, Hangzhou MSK Eye Hospital, Hangzhou, Zhejiang Province, People’s Republic of China
Correspondence: Jun Zhang, Department of Ophthalmology, Hangzhou MSK Eye Hospital, Hangzhou, Zhejiang Province, People’s Republic of China, Tel +86 571 85068587, Email [email protected]
Purpose: To assess long term changes of the surgically induced astigmatism (SIA) and corneal higher-order aberrations (HOAs) after 2.2 mm clear corneal incisions (CCIs) in femtosecond laser-assisted cataract surgery and compare them between 2 types of CCIs: temporal and superior approach.
Patients and Methods: Patients received the temporal CCIs (Group A) or the superior CCIs (Group B). Outcome measures included visual acuity, manifest refraction, corneal astigmatism, SIA, flattening effect, and corneal HOAs. Correlation between postoperative corneal HOA and SIA at each follow-up were analysed.
Results: This study assessed data from 106 eyes, of which 64 in Group A and 42 in Group B. The two groups had similar postoperative visual acuity of distance, intermediate and near (all P > 0.05). SIA and corneal HOAs were significantly lower in Group A than Group B in the early postoperative period, while there was no significant difference in the late postoperative period. At 6 months after surgery, the arithmetic mean of SIA over corneal 4mm zone was 0.33 ± 0.19D for temporal incision, and 0.37 ± 0.25D for superior incision. For Group A, the correlations of HOAs and SIA persisted from 1 week to 6 months after surgery. For Group B, the changes in corneal HOAs were significantly related to the SIA at 1 week and 1 month postoperatively.
Conclusion: This study suggested the consistency of increasing and recovering process of corneal HOAs and SIA after surgery. Compared to the superior incisions, temporal incisions might induce quicker corneal recovery and less change in SIA and corneal HOAs.
Keywords: surgically induced astigmatism, higher-order aberrations, clear corneal incision, femtosecond laser-assisted, cataract surgery
Introduction
Surgically induced astigmatism (SIA) is defined as the difference between the postoperative and preoperative astigmatism, which is a form of astigmatism related to the process of healing and scar reshuffling that takes place at the surgical incision.1,2 The presence of corneal astigmatism may lead to suboptimum refractive outcomes and patient dissatisfaction after cataract surgery. Considering this, controlling surgically induced astigmatism (SIA) during cataract surgery plays a significant role in this surgery to reduce astigmatism to emmetropia, improve uncorrected visual acuity, and thereby increase patient satisfaction.3
To optimize visual performance with intraocular lens (IOLs), SIA should be one of the factors taken into account for IOL power selection. Nowadays, with the improvement of people’s living standards and the extension of working age, the demand for eye use is increasing. When people develop cataracts or presbyopia, they expect to achieve good vision both in the far and near distances with spectacle independence after surgery. Cataract surgery has evolved from vision restoration surgery to a refractive procedure.4 In addition, an increasing number of younger patients decide to undergo refractive lens exchange to treat presbyopia and refractive errors such as myopia, hyperopia and astigmatism.5 The goal of cataract surgery is not limited to improving visual acuity only, but also to increase visual quality.6 However, the visual performance of MIOLs is more sensitive to even very small magnitudes of refractive error than monofocal IOLs, including spherical refractive error, preexisting astigmatism, and surgically induced astigmatism (SIA).7 Garzón’s study showed that a given refractive error results in a more pronounced drop in visual acuity and a worsening of visual quality for multifocal IOLs wearers than for those people implanted with monofocal IOLs.8 So, optimum management of SIA is important in today’s surgical practice of cataract extraction, especially in cases of multifocal IOL implantation.4
Now, the use of femtosecond lasers in cataract surgery is becoming more and more common. As we know, femtosecond lasers can control the parameters of clear corneal incisions (CCIs) including width, length, site, and incision architecture.9,10 It may potentially provide predictable and reproducible outcomes, inducing a predictable degree of astigmatism through CCIs.4 Previous studies about SIA of manually created clear corneal incisions (CCIs) demonstrate that temporal placement of the primary incision induces less corneal astigmatism in comparison to superior wounds since these incisions are usually farther from the visual axis (the horizontal axis of the cornea is larger than the vertical).11 It is necessary to study the SIA of CCIs created by femtosecond laser at different meridians.
Apart from astigmatism, the higher-order aberrations (HOAs) are also important for visual quality.12 The surgical procedures, including clear corneal incision (CCI), phacoemulsification, stromal hydration and intraoperative flushing, may all affect corneal regularity and consequently induce the HOAs.12 The effect of femtosecond laser CCIs on corneal HOAs is less well know and long-term changes of corneal HOAs has not been studied so far.
The objective of this study was to compare SIA and corneal HOA in patients who underwent phacoemulsification with CCIs created by femtosecond laser at two different meridians and to observe time-related changes of them. We hope our findings contribute to a better understanding of the effect of femtosecond laser CCIs on SIA and corneal HOAs. This work could contribute to the optimization of the CCI design.
Patients and Methods
This retrospective study included patients who underwent femtosecond laser-assisted cataract surgery between March 2021 and March 2023 at Hangzhou MSK Eye Hospital, Hangzhou, China. The study was performed according to the tenets of the Declaration of Helsinki, and approved by the Medical Ethics Committee of Hangzhou MSK Eye Hospital.
Patients who met the following criteria were included: (1) a history of femtosecond laser-assisted cataract surgery; (2) preoperative corneal astigmatism less than 1.25 D; (3) pupil diameter >2.5 mm (Photopic) and <6 mm (Mesopic); (4) total corneal HOA ≤ 0.5 μm (undilated pupil, 4mm diameter). The exclusion criteria were as follows: (1) ocular surface disorders (severe dry eye, ectropion, entropion, trichiasis); (2) corneal disease, uveitis, glaucoma, retinopathy, neurological lesions; (3) history of trauma or ocular surgery; (4) lack of 6 months follow-up data.
All patients were divided into group A and group B. Group A included 64 cases who had corneal astigmatism against the rule and underwent femtosecond laser-assisted phacoemulsification through temporal clear corneal approach, and group B had 42 cases who had corneal astigmatism with the rule and underwent the procedure through superior clear corneal approach. Patients with corneal oblique astigmatism were not studied due to their scarcity.
Clinical Data Measurement
All patients received a comprehensive ophthalmologic evaluation within 2 weeks before surgery, which included measurement of uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), manifest and cycloplegic refractions, keratometry, slit-lamp microscopy, intraocular pressure (IOP) measurement, endothelial cell density (ECD) assessment, ultrasound A and B scan, dilated indirect fundoscopy, anterior segment tomography (Sirius; CSO, Florence, Italy), biometry (IOL Master 700; Carl Zeiss, Jena, Germany), and optical coherence tomography (OCT) (Cirrus HD-OCT 5000; Carl Zeiss, Jena, Germany).
Follow-up examinations were scheduled at 1 week, 1 month, 3 months and 6 months postoperatively. The study assessed the following outcome measures: (1) uncorrected distance visual acuity (UDVA) at 5 meters, uncorrected intermediate visual acuity (UIVA) at 60 centimeters, and uncorrected near visual acuity (UNVA) at 40 centimeters; (2) corrected distance visual acuity (CDVA) at 5 meters, distance-corrected intermediate visual acuity (DCIVA) at 60 centimeters, and distance-corrected near visual acuity (DCNVA) at 40 centimeters; (3) manifest refraction spherical equivalent (MRSE) and refractive astigmatism.
AS-OCT Assessments
The AS-OCT assessments were performed by the same experienced physician. Patients received measurements preoperatively and postoperatively at 1 week, 1 month, 3 months and 6 months, and the following data were extracted: (1) central corneal thickness (CCT), (2) central ketatomtry, (3) corneal astigmatism, (4) coefficients of Zernike polynomials on total corneal surface. Each eye had at least three measurements with good reproducibility.
Surgically induced astigmatism (SIA) vectors were calculated with the method described by Alpins & Goggin.13 The flattening effect was calculated with the method described by Alpins.14 The root-mean-square (RMS) of corneal HOAs were also calculated.
Surgical Procedures
Following topical anesthesia (Alcaine; Alcon, Fort Worth, TX, USA), femtosecond laser (LenSx; Alcon, Fort Worth, TX, USA) was used to perform capsulorhexis, lens fragmentation, and double incisions (main incision and lateral incision). Femtosecond Laser Clear Corneal Incisions After the suction ring was precisely docked onto the patient’s eye and centered over the limbus, the arc cuts of the primary incision and side-port incision were adjusted toward the limbus, just anterior to the conjunctival vascular arcades, guided by the femtosecond laser real-time imaging system. The 3-planar primary incision of 2.2mm was made at temporal in the eye of Group A (180° for right eye, 0° for left eyes) and at superior in the eye of Group B (90° for right eye and left eye). Subsequently, the surgeon opened two incisions with a bladeless hook and injected ophthalmic viscoelastic devices (OVDs) (DisCoVisc; Alcon, Fort Worth, TX, USA) to maintain the anterior chamber. Following this, free-floating anterior capsule removal was carried out, followed by cortical-cleaving hydrodissection and the stop-and-chop technique for phacoemulsification. The irrigation-aspiration (I/A) probe was used for cortical removal and polishing, and a multifocal IOL (AcrySof IQ PanOptix, TNFT00, Alcon, Fort Worth, TX, USA) was implanted into the capsular pouch directly via the 2.2-mm main incision (Centurion; Alcon, Fort Worth, TX, USA). After OVDs removal with the I/A probe, stromal hydration was utilized to close the incisions. Postoperative eyedrops including topical antibiotics and corticosteroids (levofloxacin, Santen, Japan, and Tobradex, Alcon, Fort Worth, TX, USA) were used.
Statistical Analysis
Statistical analysis was conducted using SPSS software (version 22.0, SPSS, Inc, USA). Data with a normal distribution were presented as means ± standard deviations (SD). Visual acuity data were converted to logMAR values. Categorical variables were presented as numbers and percentages. A Kolmogorov–Smirnov test was used to test the normality of the data. The independent-sample t test was used to compare the data between Group A and Group B if the data had a normal distribution; otherwise, the Mann–Whitney U-test was applied. The One-way ANOVA test was used to compare one data with every other data within the same group. Spearman analysis was performed to determine the correlation between corneal total HOAs and SIA. A P value less than 0.05 was considered statistically significant.
Results
This study assessed data from 106 eyes, of which 64 had temporal clear corneal incision (Group A) and 42 had superior clear corneal incision (Group B). The patients’ baseline data were comparable between the two groups (P > 0.05) (Table 1). All surgical procedures were uneventful, and there were no serious intraoperative or postoperative complications.
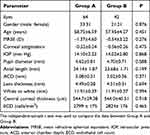 |
Table 1 Patients’ Baseline Demographic Data |
Visual Acuity
Table 2 shows the visual outcomes at each follow-up for the two groups. The UDVA, UIVA, UNVA, CDVA, DCIVA and DCNVA in all cases were significantly better 1 week, 1 month, 3 months and 6 months postoperatively than preoperatively (P < 0.05 for all). There was no significant difference in the postoperative visual acuity for distance, intermediate or near between group A and group B (P > 0.05 for all). Six months after surgery, the percentage of eyes achieving an uncorrected distance visual acuity of 20/20 was 75% for group A and 81% for group B, with all eyes achieved 20/40 or better. For intermediate distance, 92% of patients from group A reached an uncorrected visual acuity of 20/20 and 95% for group B, with all eyes achieved 20/40 or better. For uncorrected near visual acuity, all patients of both groups achieved 20/40 or better; 58% for group A and 62% for group B reached 20/20 (Figure 1).
 |
Table 2 Visual Assessment Results |
 |
Figure 1 Uncorrected visual acuity for distance (A), intermediate (B) and near (C) at postoperative 6 months by group. |
Refraction
Table 3 illustrates the changes in the manifest refraction spherical equivalent (MRSE), refractive astigmatism, and corneal astigmatism over 4mm zone throughout the follow-up. There was no significant difference in MRSE or refractive astigmatism between group A and group B (P > 0.05 for all). For corneal astigmatism, there was a statistically significant difference between group A and group B at postoperative 1 week (p < 0.05), but no significant difference at other visits. Figure 2 shows the refractive accuracy 6 months after surgery. For spherical equivalent refraction, 72% of eyes for group A and 74% of eyes for group B were within ±0.50 D; 93% for group A and 98% for group B were within ±1.0 D of emmetropia. For refractive astigmatism, 56% of eyes were within ±0.50 D and 90% of eyes were within ±1.0 D for group A; 78% of eyes were within ±0.50 D and 98% of eyes were within ±1.0 D for group B. For corneal astigmatism over corneal 4mm zone, 48% of eyes were within ±0.50 D and 93% of eyes were within ±1.0 D for group A; 52% of eyes were within ±0.50 D and 98% of eyes were within ±1.0 D for group B.
 |
Table 3 Assessment of MRSE, Refractive Astigmatism, and Corneal Astigmatism Over 4mm Zone After Surgery |
Surgically Induced Astigmatism
Table 4 shows the values of surgically induced astigmatism over different corneal zones at each follow-up for the two groups. SIAs of group A and group B were significantly different at 1 week and 1 month postoperative follow-up (P < 0.05). While at 3 months and 6 months after surgery, there was no difference between the two groups (P > 0.05). At 6 months after surgery, there was no significant difference between SIAs of every two different corneal zones in group B (P < 0.05). However, comparing SIAs over different corneal zones in group A, SIAs of corneal 3mm and 4mm, 3mm and 5mm were significantly different (P < 0.05); but there was no significant difference among 4mm, 5mm and 6mm zones (P > 0.05). Figure 3 displays SIA over corneal 4 mm at each follow-up time by group. With the extension of time, the SIA values of two groups both gradually decreased (P < 0.05).
 |
Table 4 SIA Assessment Results |
 |
Figure 3 Polar graphical display of SIA over corneal 4 mm at each follow-up time by group. Abbreviations: SIA, surgically induced astigmatism; post-op, postoperative. |
Flattening Effect
The results of flattening effect for each group are presented in Table 5. For right eyes, there was no significant difference between the temporal and superior incisions. However, flattening effect of the superior incision was larger than that of the temporal incision for left eyes (P < 0.05).
 |
Table 5 Flattenting Effects of Temporal and Superior Incisions (Mean ± SD) |
Corneal Higher-Order Aberration
Table 6 shows the values of corneal higher-order aberrations over different corneal zones at each follow-up for the two groups. At 1 week and 1 month after surgery, there were significant difference for HOAs over corneal 4mm, 5mm and 6mm between the two groups (P < 0.05). The corneal HOAs of group A and group B were not different at 3 months and 6 months postoperative follow-up (P > 0.05). At 6 months after surgery, the HOAs of different corneal zones were significantly different among them (P < 0.05). Figure 4 shows corneal high-order aberrations over the 3mm, 4mm, 5mm, and 6 mm corneal zones at each follow-up by Group A and Group B. For group A, the HOAs over corneal 3mm, 4mm and 5mm at postoperative 6 months were significantly different from those of preoperative (P < 0.05). For group B, there were significant difference for HOAs over corneal 3mm, 4mm, 5mm and 6mm between postoperative 6 months and preoperative (P < 0.05).
 |
Table 6 Corneal Higher-Order Aberrations Assessment Results |
Correlation Between Corneal HOA and SIA
Table 7 shows correlation analysis between postoperative corneal HOA and SIA at each follow-up. At corneal 3mm zone, there were positive correlations between HOA and SIA at 1 month, 3 months and 6 months after surgery in group A, whereas in group B the strong correlation was only present at 1 week (P < 0.05). At corneal 4mm zone, there were positive correlations between HOA and SIA at each follow-up in group A, whereas in group B the positive correlations were present at 1 week and 1 month (P < 0.05). At corneal 5mm zone, there were strong positive correlations between HOA and SIA at 1 month, 3 months and 6 months after surgery in group A, whereas in group B the positive correlations were present at 1 week and 1 month (P < 0.05). At corneal 6mm zone, there were strong positive correlations between HOA and SIA at each follow-up in group A, whereas in group B the positive correlations were present at 1 week, 1 month and 3 months (P < 0.05).
 |
Table 7 Correlation Analysis (Spearman Correlation Coefficients) Between Postoperative Corneal HOA and SIA at Each Follow-Up |
Discussion
In this study, we assessed long-term changes of the surgically induced astigmatism (SIA) and corneal higher-order aberrations (HOAs) after 2.2 mm clear corneal incisions (CCIs) in femtosecond laser-assisted cataract surgery and compare them between 2 types of CCIs: temporal and superior approach. SIA and corneal HOAs were significantly lower for temporal incision than superior incision in the early postoperative period, while there was no significant difference in the late postoperative period. At 6 months after surgery, the arithmetic mean of SIA over corneal 4mm zone was 0.33 ± 0.19D for temporal incision, and 0.37 ± 0.25D for superior incision. For Group A, the correlations of HOAs and SIA persisted from 1 week to 6 months after surgery. For Group B, the changes in corneal HOAs were significantly related to the SIA at 1 week and 1 month postoperatively. This suggested the consistency of increasing and recovering process of corneal HOAs and SIA after surgery. Compared to the superior incisions, temporal incisions might induce quicker corneal recovery and less change in SIA and corneal HOAs.
In this study, femtosecond laser was used to make clear corneal incisions, capsulotomy creation and lens fragmentation. Since the femtosecond lasers are unable to cut through opaque tissues, the incisions should be located entirely on the clear corneal.4 Compared with scleral tunnel or limbus incision, clear corneal incision has advantages of increased safety, decreased inflammation and pain, faster postoperative recovery, as well as reduced SIA.15 It is universally accepted that femtosecond lasers are able to create precisely shaped (internal contour: 3-plane incisions), optimally placed (on any axis), and perfectly sized (width and length of the incision) CCIs during femtosecond laser–assisted cataract surgery.4 Therefore, femtosecond laser CCIs are highly precise, reproducible, and stable.2
Clear corneal incisions performed during cataract surgery induce changes on corneal astigmatism, whose magnitude depends on factors like location, width, length or incision shape.16 In this study, we select the same parameters of incision width, length and architecture for all the cases, just compare the two different locations of incision: temporal and superior. At 1 week and 1 month after surgery, SIA was higher in the superior group than in the temporal group with statistical significance. This result is in line with previous studies investigating manual incisions.14,17,18 Two possibilities may explain why temporal incisions induce less astigmatic change than superior incisions. One is the anatomical distance between the visual axis and the limbus, which is greater in the temporal quadrant than in the superior one. The shorter the distance from the center, the greater the effect on SIA.19 The other one is the continuous pressure of the upper eyelid putting on the superior wound.20 While as time goes on, the SIA values decreased gradually in both groups, and there was no significant difference between the two groups at 3 months and 6 months after surgery. This suggests that with the healing of the corneal incision, different incision locations do not result in different magnitude of SIA. Oshika et al19 examined the effect of superior and temporal incisions on regular and irregular astigmatism, and demonstrated that incision site makes no difference in regular and irregular SIA after surgery.
In our study, we assessed the flattening effect as a constituent of SIA acting along the incision meridian. We observed that the flattening effect associated with the superior incision was greater than that of the temporal incision for left eyes, with values of 0.05 ± 0.24D and 0.25 ± 0.33D, respectively. This finding aligns with previous research by Alpins et al14 which reported a flattening effect of 0.17 ± 0.56D for temporal incisions and 0.54 ± 0.55D for superior incisions. Notably, the flattening effects observed in our study were smaller than those reported by Alpins et al. This variance could be attributed to differences in the methodology of incision creation. In our study, femtosecond laser technology was employed for clear corneal incisions, whereas Alpins et al utilized a diamond trapezoidal blade.14 Surgically induced astigmatism comprises two components: flattening effect and torque. Given that flattening effect represents the portion of SIA that mitigates corneal astigmatism, Alpins et al14 proposed incorporating historical flattening effects into toric calculators when determining toric power for intraocular lens selection prior to cataract surgery.
The current study has also evaluated SIAs over different corneal zones. In the early postoperative period, the larger the corneal zones, the higher the SIA values. This illustrates that the impact of clear corneal incision on the peripheral corneal tissue is likely greater than at the central area, especially the zone near the incision. While in the late postoperative period, there was no significant difference between SIAs of different corneal zones. At 6 months after surgery, the arithmetic mean of SIA over corneal 4mm zone was 0.33 ± 0.19D for temporal incision, and 0.37 ± 0.25D for superior incision. Our results in the temporal group seem to be consistent with those of Borasio et al17 (SIA = 0.34D at 7 weeks) and Altan-Yaycioglu et al21 (SIA = 0.34D at 6 months). Our results in the superior group are similar to those obtained by Rho et al22 (SIA = 0.46D at 2 months), although the postoperative period was different. The results in Ferreira’s study2 showed that the SIA was 0.43 ± 0.35D in the temporal incision group, and 0.62 ± 0.46D in the superior incision group at 3 months, which were higher than our results. The reasons are likely to be larger incision (2.4mm vs 2.2 mm) and shorter visit time (3 months vs 6 months).
As we know, HOAs are part of refractive errors, but they are not correctable with sphere or cylinder corrections. They can impair the quality of the retinal image and lead to symptoms such as glare, halos, starbursts, and ghosting, which were commonly called “GASH”. Thus, corneal HOAs have an impact on visual performance after cataract surgery.23 In this study, we found that the corneal HOAs of postoperative were significantly higher than preoperative. Because of the increased corneal HOAs, especially in the superior group, the optical performance of the cornea had deteriorated, compromising visual quality after surgery. There are several reasons inducing these changes. In the early postoperative period, it is reasonable to speculate that changes were associated with significant corneal edema at central cornea and incision site.12 Factors, including the surgical incision, intraoperative flushing, and eyedrop administration, can also cause short-term ocular surface damage and thus affect corneal HOAs.6 Meanwhile, the HOAs of the superior group were higher than those of the temporal group. Except for the different corneal incision position, other intraoperative parameters were the same in both groups. Therefore, the difference in HOA between the two groups is mainly due to the influence of the surgical incision location. In the late postoperative period, with corneal edema dissipating12 and corneal incision healing, corneal HOAs of the two groups became no significantly different. This pattern of change is consistent with the change of SIA. So, we analysed the correlation between corneal HOA and SIA at each follow-up.
We found that there were positive correlations between corneal HOA and posterior SIA. For the temporal group, the correlations persisted from 1 week to 6 months after surgery. For the superior group, the positive correlations between the two were strong at 1 week and 1 month postoperatively. In the study of He Q et al, the changes in posterior surface total HOAs were significantly related to the posterior SIA, especially 1 week postoperatively, suggesting the consistency of increasing and recovering process of total HOAs and SIA after surgery.6 In addition, Hayashi et al found that similar to SIA, corneal aberrations that developed after cataract surgery were closely related to the incision size. Specifically, the aberrations decreased with decreasing incision size.24 Therefore, in order to reduce postoperative corneal HOA, SIA needs to be controlled.
The current study has several limitations. First, there were some other often used incision locations not included, such as steep-axis incision and superotemporal incision. Second, corneal biomechanical properties and their changes were not analysed. Third, the same surgeon performed the procedures, and this introduces potential bias. Lastly, the effects and correlations of SIA and HOA on postoperative visual quality require more in-depth study.
Conclusion
In summary, surgical induced astigmatism by femtosecond laser-created clear corneal incisions and corneal higher-order aberrations were significantly lower by the temporal approach than the superior approach in the early postoperative period, while there were no significant differences in the late postoperative period. The changes in corneal HOAs were significantly related to the SIA, especially 1 week and 1 month postoperatively, suggesting the consistency of increasing and recovering process of HOAs and SIA after surgery. Further studies are needed to calculate flattening effects on different incision meridians, which will be useful for surgeons to calculate the toric power when choosing intraocular lens before cataract surgery.
Data Sharing Statement
The data used during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The study was performed according to the tenets of the Declaration of Helsinki, and approved by the Medical Ethics Committee of Hangzhou MSK Eye Hospital. Informed consent was obtained from all individual participants included in the study.
Funding
There is no funding to report.
Disclosure
All authors declare no conflicts of interest in this work.
References
1. Fernández J, Rodríguez-Vallejo M, Martínez J, Tauste A, Piñero DP. Prediction of surgically induced astigmatism in manual and femtosecond laser-assisted clear corneal incisions. Eur J Ophthalmol. 2018;28:398–405. doi:10.1177/1120672117747017
2. Ferreira TB, Ribeiro FJ, Pinheiro J, Ribeiro P, O’Neill JG. Comparison of surgically induced astigmatism and morphologic features resulting from femtosecond laser and manual clear corneal incisions for cataract surgery. J Refract Surg. 2018;34:322–329. doi:10.3928/1081597X-20180301-01
3. Hashemi H, Khabazkhoob M, Soroush S, Shariati R, Miraftab M, Yekta A. The location of incision in cataract surgery and its impact on induced astigmatism. Curr Opin Ophthalmol. 2016;27:58–64. doi:10.1097/ICU.0000000000000223
4. Diakonis VF, Yesilirmak N, Cabot F, et al. Comparison of surgically induced astigmatism between femtosecond laser and manual clear corneal incisions for cataract surgery. J Cataract Refract Surg. 2015;41:2075–2080. doi:10.1016/j.jcrs.2015.11.004
5. Löffler F, Böhm M, Herzog M, Petermann K, Kohnen T. Tomographic analysis of anterior and posterior and total corneal refractive power changes after femtosecond laser-assisted keratotomy. Am J Ophthalmol. 2017;180:102–109. doi:10.1016/j.ajo.2017.05.015
6. He Q, Huang J, Xu Y, Han W. Changes in total, anterior, and posterior corneal surface higher-order aberrations after 1.8 mm incision and 2.8 mm incision cataract surgery. J Cataract Refract Surg. 2019;45:1135–1147. doi:10.1016/j.jcrs.2019.02.038
7. Frings A, Steinberg J, Druchkiv V, Linke SJ, Katz T. Pseudolentogenic astigmatic effect of multifocal intraocular lenses: non-corneal ocular residual astigmatism (N-CORA) as a new parameter in astigmatic change analysis. Int Ophthalmol. 2017;37:957–964. doi:10.1007/s10792-016-0359-4
8. Garzón N, Rodríguez-Vallejo M, Carmona D, et al. Comparing surgically induced astigmatism calculated by means of simulated keratometry versus total corneal refractive power. Eur J Ophthalmol. 2018;28:573–581. doi:10.1177/1120672118757666
9. Nagy ZZ, Kránitz K, Takacs AI, Miháltz K, Kovács I, Knorz MC. Comparison of intraocular lens decentration parameters after femtosecond and manual capsulotomies. J Refract Surg. 2011;27:564–569. doi:10.3928/1081597X-20110607-01
10. Alió JL, Abdou AA, Soria F, et al. Femtosecond laser cataract incision morphology and corneal higher-order aberration analysis. J Refract Surg. 2013;29:590–595. doi:10.3928/1081597X-20130819-01
11. Marek R, Kluś A, Pawlik R. Comparison of surgically induced astigmatism of temporal versus superior clear corneal incisions. Klin Oczna. 2006;108:392–396.
12. He Q, Huang J, He X, Yu W, Yap M, Han W. Effect of corneal incision features on anterior and posterior corneal astigmatism and higher‐order aberrations after cataract surgery. Acta Ophthalmologica. 2021;99:e1027–e1040.
13. Alpins NA, Goggin M. Practical astigmatism analysis for refractive outcomes in cataract and refractive surgery. Surv Ophthalmol. 2004;49:109–122. doi:10.1016/j.survophthal.2003.10.010
14. Alpins N, Ong JKY, Stamatelatos G. Asymmetric corneal flattening effect after small incision cataract surgery. J Refract Surg. 2016;32:598–603. doi:10.3928/1081597X-20160608-01
15. Nikose AS, Saha D, Laddha PM, Patil M. Surgically induced astigmatism after phacoemulsification by temporal clear corneal and superior clear corneal approach: a comparison. Clin Ophthalmol. 2018;12:65–70. doi:10.2147/OPTH.S149709
16. Koç M, Ilhan Ç, Koban Y, Özülken K, Durukan İ, Yılmazbaş P. Effect of corneal biomechanical properties on surgically-induced astigmatism and higher-order aberrations after cataract surgery. Arq Bras Oftalmol. 2016;79:380–383. doi:10.5935/0004-2749.20160108
17. Borasio E, Mehta JS, Maurino V. Surgically induced astigmatism after phacoemulsification in eyes with mild to moderate corneal astigmatism: temporal versus on-axis clear corneal incisions. J Cataract Refract Surg. 2006;32:565–572. doi:10.1016/j.jcrs.2005.12.104
18. Borasio E, Mehta JS, Maurino V. Torque and flattening effects of clear corneal temporal and on-axis incisions for phacoemulsification. J Cataract Refract Surg. 2006;32:2030–2038. doi:10.1016/j.jcrs.2006.09.010
19. Oshika T, Sugita G, Tanabe T, Tomidokoro A, Amano S. Regular and irregular astigmatism after superior versus temporal scleral incision cataract surgery. Ophthalmology. 2000;107:2049–2053. doi:10.1016/S0161-6420(00)00379-1
20. Cillino S, Morreale D, Mauceri A, Ajovalasit C, Ponte F. Temporal versus superior approach phacoemulsification: short-term postoperative astigmatism. J Cataract Refract Surg. 1997;23:267–271. doi:10.1016/S0886-3350(97)80352-5
21. Altan-Yaycioglu R, Akova YA, Akca S, Gur S, Oktem C. Effect on astigmatism of the location of clear corneal incision in phacoemulsification of cataract. J Refract Surg. 2007;23:515–518. doi:10.3928/1081-597X-20070501-16
22. Rho CR, Joo C-K. Effects of steep meridian incision on corneal astigmatism in phacoemulsification cataract surgery. J Cataract Refract Surg. 2012;38:666–671. doi:10.1016/j.jcrs.2011.11.031
23. Pohlmann D, Pilger D, Bertelmann E, von Sonnleithner C. Corneal higher-order aberrations after cataract surgery: Manual phacoemulsification versus femtosecond-laser assisted technique. Eur J Ophthalmol. 2021;31:2955–2961. doi:10.1177/1120672121990611
24. Hayashi K, Yoshida M, Hayashi H. Postoperative corneal shape changes: microincision versus small-incision coaxial cataract surgery. J Cataract Refract Surg. 2009;35:233–239. doi:10.1016/j.jcrs.2008.10.031
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


