Back to Journals » Risk Management and Healthcare Policy » Volume 17
Link of Infection Prevention Climate to Patient-Centered Care: Role of Workplace Safety and Risk Mitigation
Authors Rumintang Marito D, Widianto S
Received 12 September 2023
Accepted for publication 1 February 2024
Published 9 February 2024 Volume 2024:17 Pages 329—340
DOI https://doi.org/10.2147/RMHP.S439907
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Gulsum Kubra Kaya
Debora Rumintang Marito, Sunu Widianto
Department of Management and Business, Universitas Padjadjaran, Bandung, Indonesia
Correspondence: Debora Rumintang Marito, Department of Management and Business, Universitas Padjadjar, Jl. Dipati Ukur No. 46, Bandung, Jawa Barat, 45363, Indonesia, Email [email protected]
Background: Healthcare-associated infections pose a substantial threat to the quality of healthcare services. Consequently, it is imperative for hospital organizations to actively support an infection prevention climate, fostering workplace safety and risk mitigation, thereby promoting patient-centered care.
Purpose: This study aims to explore the interconnectedness between the infection prevention climate, workplace safety, risk mitigation, and patient-centered care.
Methods: A cross-sectional study design was employed, utilizing a questionnaire administered to 235 healthcare professionals in intensive care and inpatient units at Bandung Kiwari Regional General Hospital. Data analysis was conducted using partial least squares structural equation modeling (PLS-SEM) with SmartPLS 4 and SPSS 25.
Results: The study revealed several significant relationships, including (1) between infection prevention climate and patient-centered care; (2) infection prevention climate and workplace safety; (3) workplace safety and patient-centered care; (4) infection prevention climate and patient-centered care mediated by workplace safety; (5) infection prevention climate and risk mitigation; (6) risk mitigation and patient-centered care; (7) and the relationship between infection prevention climate and patient-centered care mediated by risk mitigation.
Conclusion: Infection prevention climate emerges as a crucial intangible value that hospital organizations can cultivate to shape workplace safety. This, in turn, encourages healthcare workers’ compliance in implementing infection prevention controls as a form of risk mitigation, ultimately contributing to the provision of patient-centered care.
Keywords: healthcare-associated infections, infection prevention climate, patient-centered care, workplace safety, risk mitigation
Introduction
Healthcare-associated infections (HAIs) pose a significant threat to the quality of health services.1 They not only contribute to heightened morbidity and mortality rates but also result in prolonged hospital stays and increased healthcare costs.2 Beyond jeopardizing patient safety, HAIs also compromise the well-being of health workers, communities, and the overall health system.3
The implementation of infection prevention control (IPC) represents a pivotal endeavor aligned with patient-centered care—one of the World Health Organization’s (WHO) dimensions of healthcare quality.4,5 Involving patients and families in IPC practices facilitates their engagement in assessing healthcare workers’ IPC performance, participating in medical decisions, fostering a sense of security, and promoting the implementation of patient-centered care.4,6,7
However, not all healthcare workers incorporate infection prevention as a component of patient-centered care.8 As a risk mitigation strategy, IPC aims to safeguard both healthcare workers and patients from potential infections within healthcare facilities.9,10 Observing health workers perform infection prevention procedures, such as hand hygiene before patient contact, instills a sense of security in patients.11 Nevertheless, adherence to hand hygiene is lower before patient contact (58%) compared to after contact with patient body fluids (73.6%) or after patient contact (73.6%).12 This discrepancy stems from health workers’ concerns about the cross-transmission of infections from patients, overlooking the fact that the hands of health workers pose the highest risk of transmitting microorganisms.12,13 Consequently, health workers inadvertently neglect patient-centered care by inadequately minimizing infection risks to patients.7,13
Beyond risk mitigation, IPC practices also aim to enhance the quality of patient-centered care. Organizational comprehension of IPC and patient-centered care has the potential to elevate patient satisfaction.10,14 However, not all hospitals provide IPC facilities that guarantee workplace safety due to resource constraints.15
Research on the infection prevention climate’s impact on patient-centered care is scant in Indonesia. This study seeks to guide hospital management in assessing and enhancing organizational support for IPC practices related to patient-centered care. By addressing existing gaps in research on the interconnectedness of infection prevention climate, workplace safety, and risk mitigation for patient-centered care, this research aims to elucidate how organizational climate influences workplace safety and healthcare workers’ adherence to patient-centered infection control prevention. The study specifically endeavors to determine whether the infection prevention climate correlates with patient-centered care through risk mitigation and workplace safety.
Literature Review and Hypotheses
Infection Prevention Climate and Patient-Centered Care
The infection prevention climate denotes healthcare workers’ perceived value of organizational factors related to infection prevention, influencing the implementation of infection prevention measures. It encompasses psychological safety, prioritization of quality, a supportive work environment, and improvement orientation.14,16–19 Patient-centered care, characterized by holistic patient care and involvement in medical decisions, aligns with the four essential aspects of respecting patients’ perspectives, promoting patient involvement, providing comfort, and advocating for patients.19 An optimal infection prevention climate is expected to foster quality patient-centered care.20 Hence, the first hypothesis posits a relationship between infection prevention climate and patient-centered care:
H1: There is a relationship between infection prevention climate and patient-centered care.
Infection Prevention Climate, Workplace Safety, and Patient-Centered Care
An optimal infection prevention climate is believed to drive workplace safety, representing the shared perception built by management to support safety regarding IPC in hospitals.21 Workplace safety, influenced by the availability of zoning divisions, supply of quality personal protective equipment (PPE), and management of isolation for infectious patients, contributes to healthcare workers’ adherence to standard precautions, thereby safeguarding patients from HAIs.10,21 Thus, workplace safety is posited to be related to patient-centered care. Consequently, the following hypotheses are presented:
H2: There is a relationship between infection prevention climate and workplace safety. H3: There is a relationship between workplace safety and patient-centered care. H4: There is a relationship between infection prevention climate and patient-centered care through workplace safety.
Risk Mitigation, Infection Prevention Climate, and Patient-Centered Care
An optimal infection prevention climate is anticipated to drive healthcare workers’ adherence to IPC as a concrete risk mitigation strategy, protecting both healthcare workers and patients from HAIs.9,10 Risk mitigation, aimed at minimizing the risk of exposure and the occurrence of unwanted events, is associated with patient-centered care by ensuring a sense of security, quality, and patient satisfaction with medical services.7 Thus, the following hypotheses are presented:
H5: There is a relationship between infection prevention climate and risk mitigation. H6: There is a relationship between risk mitigation and patient-centered care. H7: There is a relationship between infection prevention climate and patient-centered care through risk mitigation.
Based on the aforementioned theoretical framework, a conceptual model of the study is illustrated in Figure 1. The study is designed to test hypotheses H1 through H7, examining the relationships between infection prevention climate, workplace safety, risk mitigation, and patient-centered care as depicted in the conceptual model of the study in Figure 1.
 |
Figure 1 Conceptual model of the study. |
Materials and Methodology
Ethics
Approval for this study was obtained from the ethics committee of Bandung Kiwari Regional General Hospital (Approval Number: PP.09.01/715_RSUDBK/III/2023). Additionally, approvals were obtained from the National Unity and Politics Agency of West Java (Approval Number: 0515/KB.01.04.03/WASDA) and Universitas Padjadjaran (Approval Number: 3565/UN6.B.4.14/PT.02/2023). Participants provided informed consent electronically through a Google form, where voluntary participation was confirmed by clicking the “I agree” button.
Design
This study employed a quantitative explanatory research design with a cross-sectional approach. Data were collected using a questionnaire as the primary research instrument.
Settings
The research was conducted at Bandung Kiwari Regional General Hospital (RSUDBK), West Java, Indonesia. RSUDBK transitioned from being a Mother and Children Hospital to a General Hospital in February 2022, influencing resource prioritization for infection prevention control (IPC) management.22 The hospital experienced an increase in the bed occupancy rate, reaching 85.5% in May 2022, a rise of 12.1% compared to April 2022 (73.4%). Notably, the highest incidence of healthcare-associated infections (HAIs) occurred in May 2022, with central line-associated bloodstream infections (CLABSI) at 15.34‰ and ventilator-associated pneumonia (VAP) at 10.2‰, exceeding IPC quality indicators.23 The research period extended from March 2023 to June 2023 in intensive care and inpatient units, as defined by healthcare-associated infections occurring after 48 hours of hospital treatment.24
Sampling
Following Hair et al and Uzir et al, the research aimed for a sample size of 235 respondents, calculated by multiplying the number of questionnaire items (47 items) by five, ensuring a confidence level of 95%.25,26 A non-probability convenience sampling method was employed, targeting healthcare workers (general practitioners and nurses) in intensive care and inpatient units at RSUDBK. The total number of intensive care unit nurses is 79 people, consisting of 26 ICU nurses (5 beds with a nurse ratio of 1:1), 22 PICU nurses (6 beds with a nurse ratio of 1:1), and 31 NICU nurses (12 beds with a nurse ratio of 1:1). Medical doctors and nurses were the objects of the research as they make direct contact with patients at risk of being exposed to infection and transmitting infection to patients.27
Instruments
Data on infection prevention climate were collected using an adapted version of the Leading a Culture of Quality for Infection Prevention (LCQ-IP) questionnaire from Cruz’s study (2019) regarding Pogorzelska-Maziarz et al.16,20 Information on risk mitigation was obtained through an adapted questionnaire from Lyu et al, enriched by Wilkason et al’s research.9,10 Workplace safety data were collected using an adapted questionnaire from Lyu et al.10 Patient-centered care information was gathered using an adapted questionnaire from Hwang et al, subsequently modified based on research needs related to infection.9,19 The questionnaire items are illustrated in Figure 2a (Questionnaire Items Part 1) and Figure 2b (Questionnaire Items Part 2).
 |
Figure 2 Continued. |
 |
Figure 2 (A) Questionnaire Items (Part 1). (B) Questionnaire Items (Part 2). |
Data Collection
In this study, the authors were responsible for executing the data collection process. Initially, the authors elucidated the questionnaires to a designated representative from each unit, conducting subsequent interviews to clarify any queries the participants might have had. Following this, the questionnaires were disseminated to both intensive care and inpatient units utilizing Google Forms. To enhance data accuracy and streamline the collection process, a purpose-built Google Spreadsheet file was crafted. This file constrained the types of data that could be entered into each column, thereby mitigating data entry errors and ensuring the overall efficiency of the data collection process. Upon completion, the data files underwent a thorough integrity check to confirm that participants had responded to all questions.
Data Analysis
The data, gathered through a questionnaire employing ordinal data with a Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree), underwent further processing using SPSS 25 software software to construct a correlation matrix. PLS-SEM analysis was conducted with the aid of SmartPLS 4 software to scrutinize the research model. Both the outer model (validity and reliability) and the inner model underwent rigorous testing. The assessment of the inner model involved evaluating the relationships between exogenous and endogenous variables through squared multiple correlations (R2) and path coefficients (b), employing the bootstrapping method.28 The coefficient of determination (R2) gauges the explanatory power of the research model by indicating the predictive value of the endogenous construct. Specifically, R2 values were interpreted on a scale from 0 to 0.10 (weak), 0.11 to 0.30 (modest), 0.30 to 0.50 (moderate), and >0.50 (strong). Meanwhile, the path coefficient (β) delineates the strength of relationships between constructs within the structural model, with values ranging from 0 to 0.10 (weak), 0.11 to 0.30 (modest), 0.30 to 0.50 (moderate), and >0.50 (strong).29
Results
Demographic Characteristics of Participants
A total of 235 healthcare workers, including general practitioners and nurses, actively participated in the study. Table 1 presents the participants’ demographic, revealing that the majority of participants fell within the age range of 26 to 35 years (74%) and were predominantly female (77%). The respondents primarily identified as professional nurses (74.47%), holding a Bachelor of Nursing as their highest educational attainment (74.47%). The majority of respondents reported a working period of 1–5 years (67.2%). Furthermore, 73.19% of participants served in inpatient rooms, while the remaining 26.81% worked in the intensive care unit.
 |
Table 1 Descriptive Table of Demographic Variables |
Table 2 provides a summary of descriptive statistics and correlation coefficients (r) for the study variables. The mean values reveal that the infection prevention climate, workplace safety, and patient-centered care at RSUDBK are rated as good (3.40 < x ≤ 4.20), while risk mitigation is considered excellent (4.20 < x < 5.00).
 |
Table 2 Descriptive Statistics |
The findings in Table 2 demonstrate a positive correlation between risk mitigation and infection prevention climate (r = 0.42, p < 0.01). The table indicates a positive correlation between workplace safety and both infection prevention climate (r = 0.54,p < 0.01) and risk mitigation (r = 0.41, p < 0.01). Additionally, descriptive statistics reveal a positive correlation between patient-centered care and infection prevention climate (r = 0.65, p < 0.01), risk mitigation (r = 0.67, p < 0.01), and workplace safety(r = 0.54, p < 0.01).
Figure 3 depicts the PLS-SEM research model. Subsequently, an inner model test, based on the depicted structural model, was conducted to evaluate the hypothesis testing results.
The subsequent phase of the inner model test involved evaluating the squared multiple correlations (R2) to gauge the extent of influence exerted by the independent latent variables on the dependent latent variables.28 Structural research model R-Square values are outlined in Table 3.
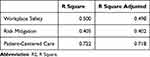 |
Table 3 Structural Research Model R Square (R2) Value |
The results in Table 3 indicate that the infection prevention climate accounts for 50% of the variance in workplace safety, representing a moderate explanatory power. Moreover, the infection prevention climate explains 40.5% of the variance in risk mitigation, also reflecting a moderate level of influence. Collectively, the three variables— infection prevention climate, risk mitigation, and workplace safety—account for a substantial 72.2% of the variance in patient-centered care, denoting a strong explanatory power. It is noteworthy that the remaining variance is attributed to factors not encompassed in this research.
Model Significance Testing
Subsequently, the significance of the model parameters was assessed to validate the study’s hypotheses. Both the measurement and structural models underwent evaluation via a bootstrapping procedure to ascertain the statistical significance of the results. Results regarding the relationship path hypotheses are presented in Table 4.
 |
Table 4 Results Regarding the Relationship Path Hypotheses |
Discussion
H1: Relationship between Infection Prevention Climate and Patient-Centered Care
The results support H1, demonstrating a significant relationship between infection prevention climate (X) and patient-centered care (Y) with a standard coefficient value of 0.374 (p=0.000). This aligns with research by Cruz (2019) and Eygelaar (2018), suggesting that health workers’ perceived values related to infection prevention in hospitals enhance patient-centered care. The four elements of an infection prevention climate—psychological safety, prioritization of quality, supportive work environment, and improvement orientation—aim to enhance service quality.7,20 Organizational climate, influenced by various factors such as leadership, job satisfaction, and cooperation, supports health workers in their duties and responsibilities, ultimately impacting the quality of health services.20 The positive impact of organizational climate on service quality has been corroborated in the literature.30,31
H2: Relationship between Infection Prevention Climate and Workplace Safety
H2 is supported by the findings, indicating a significant relationship between infection prevention climate (X) and workplace safety (W) with a standard coefficient value of 0.707 (p=0.000). This is consistent with Ayele et al, highlighting that an adequate infection prevention climate fosters workplace safety. Frontline nurses perceive workplace safety as including reasonable ward zoning, adequate PPE supply, and effective management of infected patients. Supportive work environments, sufficient infrastructure, and available resources contribute to workplace safety.10,23
H3: Relationship between Workplace Safety and Patient-Centered Care
H3 is validated by the results, demonstrating a significant relationship between workplace safety (W) and patient-centered care (Y) with a standard coefficient value of 0.286 (p=0.000). These findings align with Mull (2017), asserting that work safety is linked to patient-centered care.32 Prioritizing safety in the care environment is essential for improving patient care quality, and the availability of adequate IPC facilities influences patient safety and the quality of health services. Insufficient IPC facilities, environments, and infrastructure pose challenges to staff in executing safety functions and hinder the implementation of IPC for patient safety.33
H4: Relationship between Infection Prevention Climate and Patient-Centered Care through Workplace Safety
H4 is confirmed, as the infection prevention climate (X) is related to patient-centered care (Y) through workplace safety (W) with a standard coefficient value of 0.202 (p=0.000). Workplace safety acts as a partial mediator, encouraging adherence to standard precautions that protect patients from HAIs. The infection prevention climate fosters workplace safety through the availability of IPC resources, supporting health workers, and enhancing the quality of health services.10,21
H5: Relationship between Infection Prevention Climate and Risk Mitigation
The results support H5, indicating a significant relationship between infection prevention climate (X) and risk mitigation (M) with a standard coefficient value of 0.636 (p=0.000). This is consistent with Cruz (2019), who emphasizes that an optimal infection prevention climate influences health workers’ adherence to IPC for risk mitigation.7,9,20 Similar findings are supported by Pogorzelska-Maziarz et al and Abalkhail and Aslamah (2020). In implementing infection prevention for patients, the values and culture established by the organization play an important role in developing health workers’ better understanding of IPC.16,18
H6: Relationship between Risk Mitigation and Patient-Centered Care
H6 is validated, demonstrating a significant relationship between risk mitigation (M) and patient-centered care (Y) with a standard coefficient value of 0.304 (p=0.000). Risk mitigation, as a strategy to minimize the risk of exposure and unwanted events, is associated with patient-centered care. Adhering to IPC procedures, a form of risk mitigation, ensures patient safety, quality, and satisfaction, contributing to patient-centered care.9,10,34
H7: Relationship between Infection Prevention Climate and Patient-Centered Care through Risk Mitigation
H7 is supported, indicating a significant relationship between infection prevention climate (X) and patient-centered care (Y) through risk mitigation (M) with a path coefficient of 0.193 (p=0.000). Risk mitigation serves as a partial mediator, as the infection prevention climate encourages workplace safety through the availability of reliable IPC resources. The relationship between infection prevention climate and patient-centered care is maintained, emphasizing the role of risk mitigation in fostering patient-centered care.35
The infection prevention climate, an intangible aspect, shapes health workers’ values about IPC, impacting patient-centered care through active risk mitigation. Optimal infection prevention climates encourage health workers to adhere to IPC, ensuring patient safety and delivering patient-centered care.10
The paper discusses the importance of patient-centered care through risk mitigation and workplace safety, emphasizing the need for organizational support to ensure healthcare workers can deliver quality services. Despite the awareness among healthcare workers regarding nosocomial infections, the implementation of patient-centered infection prevention and control (IPC) is challenging without adequate organizational support.36
The research highlights the potential for organizations to shape health workers’ values, fostering compliance with IPC as a work culture that enhances workplace safety and ultimately improves the quality of patient-centered care. It underscores that even with sufficient knowledge, barriers such as organizational support and individual values significantly influence compliance with patient-centered IPC. Factors contributing to health workers’ non-compliance include the absence of a comprehensive IPC program, insufficient control functions of the IPC committee, an unsupportive work culture, limited training, facilities, and personal protective equipment, work overload, and insufficient management support.37 Furthermore, the reluctance of some hospitals to prioritize IPC due to cost concerns exacerbates the problem.33
In addition to a robust IPC program and conducive working environment, values related to the infection prevention climate impact the delivery of quality services. Personal values and attitudes, such as viewing IPC as solely the responsibility of healthcare workers or perceiving it as time-consuming and uncomfortable, can act as barriers to implementation.36 The paper suggests that organizations can influence health workers’ values to establish a long-term work culture that promotes quality health services, allowing health workers to voluntarily implement IPC in their daily practices, driven by a desire to prioritize patient care.38
The research emphasizes the role of organizational support in shaping health workers’ values and beliefs, leading to a higher level of commitment. It cites Sun et al in supporting the notion that organizational support can positively impact health workers’ values and beliefs.38
While the study sheds light on how the infection prevention climate influences health workers’ compliance with patient-centered IPC, the paper acknowledges the need for longitudinal research to validate the observed changes in health workers’ performance resulting from the establishment of an adequate infection prevention climate.16 Furthermore, the paper calls for additional long-term research to investigate whether an infection-prevention climate can enhance patient satisfaction and reduce hospital-acquired infections (HAIs).
Conclusion
This research provides crucial insights into the complex dynamics of infection prevention, workplace safety, risk mitigation, and patient-centered care in the context of RSUDBK. The findings underscore the interconnectedness of these elements and emphasize the pivotal role of organizational support and values in influencing health workers’ compliance with infection prevention measures and the delivery of patient-centered care. The study highlights the significance of organizational backing in creating an infection prevention climate conducive to patient-centered care. Lack of support, as evidenced by the absence of a well-socialized IPC program, controlling function of the IPC committee, and unsupportive work culture, poses challenges to health workers’ compliance. Personal values and attitudes, including misconceptions about the limited scope of IPC to healthcare workers, time constraints, and discomfort, act as barriers to implementation. The research suggests that organizations play a vital role in reshaping these values to establish a daily work culture centered on patient care. The study acknowledges that IPC programs are sometimes perceived as a drain on hospital funding, leading to variations in resource allocation across hospitals. Despite financial challenges, the impact of healthcare-associated infections on patient outcomes necessitates prioritizing resources for IPC.
Establishing an infection prevention climate requires creating an enabling environment within the organization. This involves hospital accreditation for IPC performance, effective communication of IPC programs and goals, periodic evaluation, and feedback mechanisms. The multidisciplinary role of health workers is crucial for supporting compliance with IPC implementation. An integrated approach, involving various healthcare professionals, can enhance the effectiveness of risk mitigation strategies. Regular training programs, including patient-centered IPC training for health workers and IPC education for patients and families, contribute to a culture of safety and infection prevention. These initiatives aim to improve knowledge, skills, and overall compliance. Establishing non-blaming reporting systems encourages open communication and reporting of incidents related to infection prevention. This creates a transparent environment where healthcare workers can contribute to continuous improvement.
Limitations and Recommendations
The study’s focus on intensive care and inpatient units in a local government hospital limits the generalizability of findings. Future research should encompass a broader range of healthcare units, including private hospitals, to provide a more comprehensive understanding. While the research explores patient-centered care from the perspective of health workers, further investigations should incorporate the patient’s viewpoint. This multilevel approach can offer a holistic understanding of the patient experience in relation to infection prevention. The study advocates for longitudinal research to assess how the establishment of an adequate infection prevention climate influences health workers’ performance over time. Additionally, long-term research is needed to measure the impact of an infection-prevention climate on patient satisfaction and the reduction of HAIs.
Disclosure
The authors report no conflicts of interest, ensuring the transparency and integrity of the research process. Overall, this study contributes valuable knowledge to the ongoing efforts to enhance infection prevention, workplace safety, and patient-centered care in healthcare settings.
References
1. Tardivo S, Moretti F, Nobile M, et al. Definition of criteria and indicators for the prevention of Healthcare-Associated Infections (HAIs) in hospitals for the purposes of Italian institutional accreditation and performance monitoring. Ann Ig. 2017;29:529–547.
2. Benenson S, Cohen M, Schwartz C, et al. Is it financially beneficial for hospitals to prevent nosocomial infections? BMC Health Serv Res. 2020;20(1):653. doi:10.1186/s12913-020-05428-7
3. English K, Langley J, McGeer A, et al. Contact among healthcare workers in the hospital setting: developing the evidence base for innovative approaches to infection control. BMC Infect Dis. 2018;18(1):184. doi:10.1186/s12879-018-3093-x
4. Wyer M, Jackson D, Iedema R, et al. Involving patients in understanding hospital infection control using visual methods. J Clin Nurs. 2015;24(11–12):1718–1729. doi:10.1111/jocn.12779
5. Zizzo N, Bell E, Lafontaine AL, et al. Examining chronic care patient preferences for involvement in health‐care decision making: the case of Parkinson’s disease patients in a patient‐centred clinic. Health Expectations. 2017;20(4):655–664. doi:10.1111/hex.12497
6. Birgand G, Johansson A, Szilagyi E, et al. Overcoming the obstacles of implementing infection prevention and control guidelines. Clin Microbiol Infect. 2015;21(12):1067–1071. doi:10.1016/j.cmi.2015.09.005
7. Eygelaar JE. A programme to facilitate quality client-centred care in primary health care clinics of the rural west coast district. Univ West Cape. 2018;2018:1.
8. MacEwan SR, Beal EW, Gaughan AA, et al. Perspectives of hospital leaders and staff on patient education for the prevention of healthcare-associated infections. Infect Control Hosp Epidemiol. 2022;43(9):1129–1134. doi:10.1017/ice.2021.271
9. Wilkason C, Lee C, Sauer LM, et al. Assessing and reducing risk to healthcare workers in outbreaks. Health Secur. 2020;18(3):205–211. doi:10.1089/hs.2019.0131
10. Lyu X, Hu J, Xu X, et al. Factors influencing risk perception and nosocomial infection prevention practices of frontline nurse during the COVID-19 pandemic. BMC Nurs. 2021;20(1):78. doi:10.1186/s12912-021-00591-6
11. Caine LZ, Pinkham AM, Noble JT. Be seen and heard being clean: a novel patient-centered approach to hand hygiene. American. J Infect Control. 2016;44(7):e103–e106. doi:10.1016/j.ajic.2015.11.027
12. Uneke CJ, Ndukwe CD, Oyibo G, et al. Promotion of hand hygiene strengthening initiative in a Nigerian teaching hospital: implication for improved patient safety in low-income health facilities. Braz J Infect Dis. 2014;18(1):1. doi:10.1016/j.bjid.2013.04.006
13. Sundal JS, Aune AG, Storvig E, et al. The hand hygiene compliance of student nurses during clinical placements. J Clin Nurs. 2017;26(23–24):4646–4653. doi:10.1111/jocn.13811
14. Zingg W, Holmes A, Dettenkofer M. Hospital organisation, management, and structure for prevention of health-care-associated infection: a systematic review and expert consensus. Lancet Infect Dis. 2015;15(2):212–224. doi:10.1016/S1473-3099(14)70854-0
15. Colet PC, Cruz JP, Cacho G, et al. Perceived infection prevention climate and its predictors among nurses in Saudi Arabia. J Nurs Scholarsh. 2018;50(2):134–142. doi:10.1111/jnu.12360
16. Pogorzelska-Maziarz M, Nembhard IM, Schnall R, et al. Psychometric evaluation of an instrument for measuring organizational climate for quality: evidence from a national sample of infection preventionists. Am J Med Qual. 2016;31(5):441–447. doi:10.1177/1062860615587322
17. Adekanmbi FP, Ukpere WI, Kelvin-Iloafu LE. The relational effects of perceived organizational support, fear of COVID-19, and work-related stress on the safety performance of healthcare workers. Frontiers in Psychology. 2022;13. doi:10.3389/fpsyg.2022.963683
18. Abalkhail A, Alslamah T. Institutional factors associated with infection prevention and control practices globally during the infectious pandemics in resource-limited settings. Vaccines. 2022;10(11):1811. doi:10.3390/vaccines10111811
19. Hwang J. Development and testing of a patient-centred care competency scale for hospital nurse. Int J Nurs Pract. 2018;21(1):43–51. doi:10.1111/ijn.12220
20. Cruz JP. Infection prevention climate and its influence on nursing students’ compliance with standard precautions. J Adv Nurs. 2019;75(5):1042–1052. doi:10.1111/jan.13904
21. Ayele DG, Baye TZ, Demissie NG, et al. Compliance with standard precautions and associated factors among undergraduate nursing students at governmental universities of Amhara region, Northwest Ethiopia. BMC Nurs. 2022;21(1):1–10. doi:10.1186/s12912-022-01165-w
22. Shaw A, Flott K, Fontana G, et al. No patient safety without health worker safety. Lancet. 2020;396(10262):1541–1543. doi:10.1016/S0140-6736(20)31949-8
23. Jackson C, Lowton K, Griffiths P. Infection prevention as “a show”: a qualitative study of nurses’ infection prevention behaviours. Int J Nurs Stud. 2014;51(3):400–408. doi:10.1016/j.ijnurstu.2013.07.002
24. Haque M, Sartelli M, McKimm J, et al. Health care-associated infections – an overview. Infect Drug Resist. 2018;11:2321–2333. doi:10.2147/IDR.S177247
25. Hair JF, Black WC, Babin BJ. Multivariate data analysis. Pearson. 2014;7:1.
26. Uzir MU, Bukari Z, Jerin I, et al. Impact of COVID-19 on psychological distress among SME owners in Ghana: partial least square–structural equation modeling (PLS-SEM) approach. J Community Psychol. 2022;50(3):1282–1314. doi:10.1002/jcop.22716
27. Omar AA, Abdo NM, Salama MF, Al-Mousa HH. Occupational injuries prone to infectious risks amongst healthcare personnel in Kuwait: a Retrospective Study. Med Princ Pract. 2014;24(2):123–128. doi:10.1159/000369462
28. Hair JF, Risher JJ, Sarstedt M, et al. When to use and how to report the results of PLS-SEM. Eur Bus Rev. 2019;31(1):2–24. doi:10.1108/EBR-11-2018-0203
29. Hair J, Alamer A. Partial Least Squares Structural Equation Modeling (PLS-SEM) in second language and education research: guidelines using an applied example. Res Method Appl Linguist. 2022;1(3):100027. doi:10.1016/j.rmal.2022.100027
30. Ayutthaya JSN, Tuntivivat S, Prasertsin U, et al. The effect of positive psychological capital and organizational climate on service quality: the mediation role of work engagement of hotel service employees in Ratchaburi province. J Adm Bus Stud. 2016;2(4):167–176.
31. Larson E, Sharma J, Bohren MA, et al. When the patient is the expert: measuring patient experience and satisfaction with care. Bull World Health Organ. 2019;97(8):563–569. doi:10.2471/BLT.18.225201
32. Mull C. Implementation of a Patient-Centered Communication Model in the Emergency Department. Grand Valley State University; 2017.
33. Stewart S, Robertson C, Kennedy S, et al. Personalized infection prevention and control: identifying patients at risk of healthcare-associated infection. J Hosp Infect. 2021;114:32–42. doi:10.1016/j.jhin.2021.03.032
34. Furin J, Loveday M, Hlangu S, et al. “A very humiliating illness”: a qualitative study of patient-centered care for rifampicin-resistant tuberculosis in South Africa. BMC Public Health. 2020;20(1):76. doi:10.1186/s12889-019-8035-z
35. Zampone G, Nicolò G, Sannino G, et al. Gender diversity and SDG disclosure: the mediating role of the sustainability committee. J Appl Account Res. 2022;2022:1.
36. Odagami K, Nagata T, Mafune K, et al. Association between perceived organizational support for infection prevention and work engagement during the COVID-19 pandemic among Japanese workers: a prospective cohort study. Int J Environ Res Public Health. 2022;19(23):16142. doi:10.3390/ijerph192316142
37. Houghton C, Meskell P, Delaney H, et al. Barriers and facilitators to healthcare workers’ adherence with infection prevention and control (IPC) guidelines for respiratory infectious diseases: a rapid qualitative evidence synthesis. Cochrane Database Syst Rev. 2020;4(4). doi:10.1002/14651858.CD013582
38. Sun M, Alam F, Ma C. How nurses’ person-organization fit influences organizational loyalty. Risk Manag Healthc Policy. 2023;2019–2036. doi:10.2147/RMHP.S425025
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

