Back to Journals » Risk Management and Healthcare Policy » Volume 17
Impact of Structural Employee Empowerment on Hospital Ratings: Mediating Role of Social Climate and First-Line Managers’ Resilience
Authors Jankelová N, Joniaková Z , Skorková Z , Gažová Adamková H
Received 12 January 2024
Accepted for publication 24 March 2024
Published 11 April 2024 Volume 2024:17 Pages 883—901
DOI https://doi.org/10.2147/RMHP.S453351
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Nadežda Jankelová, Zuzana Joniaková, Zuzana Skorková, Hana Gažová Adamková
Department of Management, Faculty of Business Management, University of Economics in Bratislava, Bratislava, Slovakia
Correspondence: Zuzana Skorková, University of Economics in Bratislava, Department of Management, Faculty of Business Management, Dolnozemská cesta 1, Bratislava, 852 35, Slovakia, Tel + 421 2 67 29 56 08, Email [email protected]
Objective: The purpose of this article is to investigate the relationship between the structural empowerment of first-line health managers and health facility performance, examining the mediating roles of resilience and social climate in shaping the ratings of Slovak hospitals. Additionally, we aim to investigate the deeper mechanisms of this relationship, particularly the impact of resilience and the social climate, which can positively influence it.
Materials and Methods: The data collection was conducted through a questionnaire survey in February 2022. Respondents included 540 healthcare managers at the first level of management from 44 Slovak hospitals, all of which were part of the evaluation by the Institute for Economic and Social Reforms (INEKO). The analysis involved the use of the PLS-SEM method to examine the relationships between variables and assess direct and indirect effects, utilizing SmartPLS 3.3 software.
Results: The findings reveal a positive association between the structural empowerment of first-level managers and the ranking of health facilities. The hypotheses regarding the mediation of both variables - First-Level Managers’ (FLMs) resilience and social climate - are supported, whether considered separately or jointly. In the case of joint mediation, a significant portion of the indirect effect is conveyed through FLMs’ resilience, suggesting a potential avenue of support from hospital management to enhance health facility ratings.
Conclusion: Structural empowerment of first-line managers establishes the conditions for improving the ratings of health facilities. The total effect is significantly more pronounced in promoting their resilience and fostering a supportive social climate.
Keywords: health facility performance, healthcare management, social climate, resilience, hospital rating
Introduction
Healthcare, a vital and rapidly growing economic sector, faces resource constraints, heightened patient demands, and the imperative for high-quality services, aligning with public health objectives.1–3 Amid rapid economic, social, technological, and environmental shifts, the healthcare system grapples with substantial financial and existential pressures.4 The contemporary public health system has undergone swift transformation to adapt to modern challenges and opportunities.5 In this dynamic operating environment, healthcare facilities face significant demands for effective management.6
Governments acknowledge the importance of optimizing practices and care pathways, introducing innovative approaches like digital health, and ensuring transparent reporting through facility ratings.7
In healthcare organizations, safeguarding human life entails immense pressure to maintain high service quality.8 First-line managers (FLMs), particularly department heads and head nurses, play a pivotal role in ensuring sustained facility performance, serving as the crucial link bridging health facility executives and management.9 Their evolving roles shift from a dual focus on expertise and supervision to a more concentrated management role.10
The demanding role of FLMs, exacerbated post-COVID-19, underscores the pivotal role of their resilience.11 Support mechanisms, empowerment, and a positive social climate are crucial for FLMs to navigate intense pressure and conflicting expectations effectively.12 The resilience of FLMs becomes pivotal in adapting to the challenges faced post-COVID-19.13
Effective support for FLMs in problem-solving and on-the-job learning is crucial for their demanding roles.12 A positive social climate is closely linked to enhanced perceptions of the work environment’s quality and subsequent satisfaction among both staff and patients.14
A large portion of conducted studies is related to the relationship between hospital ratings and patient satisfaction.15–17 This fact is understandable, as assessors, rating agencies, and policymakers consider patient experiences crucial.18 Only a few studies focus on the impact of managerial factors on hospital ratings – most commonly on the influence of communication skills on patient satisfaction scores, examined.19,20 However, today we know that soft skills have a fundamental impact on organizational management.21 We consider this fact to be a research gap and an area deserving greater scientific attention in the context of hospital rating examination. These facts form the basis of constructing our research model, the purpose of which is to explore the relationships between the variables of Structural Empowerment (SE) and Hospital Rating (HR), and the mediating role of First-Line Managers’ Resilience (FLMR) and (social climate SC).
Literature Review and Hypotheses Development
Hospital Rating (HR)
Hospital ratings are pivotal indicators of healthcare quality, influencing patient choices and facilitating resource allocation.22 Assessing care quality involves multifaceted dimensions, encompassing clinical outcomes and patient experiences.23 Patients are recognized as healthcare consumers, emphasizing the importance of their experiences in evaluating system quality.24
Policymakers and hospital management consider patient experience crucial, reflected in hospital ratings as a key criterion for healthcare system effectiveness. Empirical evidence highlights correlations between economic outcomes, workplace quality of life, and care quality.25–28 Assessing hospital performance through workplace quality of life gains prominence29 with ratings aiding patients in selecting suitable facilities.30
Our study, within the Slovak healthcare context, utilizes INEKO ratings, assessing healthcare institutions based on indicators like patient satisfaction, healthcare quality measures, doctors’ practical experience, diagnostic complexity, management, and transparency over four years. INEKO gathers data from diverse sources, ensuring comprehensive evaluations.31
Hospital Rating (HR) and Structural Empowerment (SE)
Structural Empowerment significantly contributes to individual ratings, representing the extent to which employees have access to resources, information, and support for effective job performance.32 SE includes access to information, support, resources, and learning opportunities.33,34 Learning opportunities involve challenging tasks and acquiring new skills, influencing professional growth.35,36
Access to information encompasses knowledge of organizational aspects, policies, and goals, while support involves feedback from various stakeholders.37,38 SE significantly supports First-Line Managers (FLMs) and their role in creating empowering conditions for subordinates.34,39 FLMs’ access to empowering structures positively influences their performance, impacting subordinates.40
Promoting structural empowerment enhances job satisfaction for FLMs and fosters organizational citizenship behavior.40 Access to empowering structures correlates with positive outcomes, including reduced turnover, prevention of burnout,41 increased patient satisfaction,42 higher staff-rated quality of care,43 professional behaviors,44 and evidence-based practices.42
Studies affirm the substantial influence of structural empowerment, clinical leadership, and a creative team climate on hospital performance.45 Access to empowering structures not only positively affects FLMs’ performance but also benefits patients, contributing to overall facility ratings.43,46 An empowering environment can provide the best care and a healthy, engaged staff.
Based on the evaluation of hospitals’ performance through their ratings, we formulate the following hypothesis:
H1: We Hypothesize That the SE of Healthcare Executives Positively Affects the HR of Hospitals.
First-Line Managers’ Resilience (FLMR) and Structural Empowerment (SE)
The intricate relationship between Structural Empowerment (SE) and Hospital Rating (HR) is influenced by various factors, with the resilience of First-Line Managers (FLMs) emerging as a crucial variable, particularly in the context of the ongoing COVID-19 pandemic.11,12 Resilience, defined as the capacity to endure and adapt to adverse conditions, plays a significant role in navigating workplace adversity and showcasing personal strength.47–49
In the realm of FLMs, resilience is recognized as a valuable strategy for addressing challenging situations in healthcare.50–53 Resilience, considered a characteristic, process, and outcome, is stable as a personality trait but can evolve dynamically in response to various contexts and over time.54,55
Lower resilience levels among FLMs may pose challenges in empowering their subordinates, emphasizing the importance of creating conditions that enhance FLMs’ access to empowering structures.48,56 First-line managers resilience (FLMR) resilience in daily work is vital for organizational resilience and can be supported through a well-developed infrastructure, coordination between levels, and an extended model emphasizing coordination as a linking aspect between various resilience potentials.57 Research highlights a significant increase in FLMs’ resilience scores following an empowerment-focused educational intervention, leading to greater readiness to enhance quality outcomes, improve team performance, and ultimately elevate facility ratings.29,49
H2: We Hypothesize That the Relationship Between SE and HR is Mediated by FLMR.
Social Climate (SC)
The social climate (SC) is characterized by trust, cooperation, and shared codes that exist among individuals within the organization. The social climate of healthcare institutions is determined by many factors such as leadership, organizational structure, historical forces, level of accountability, behavior, and communication.58 Through these social mechanisms, the resilience of employees,59 institutional performance, and their external evaluation (HR) can be positively influenced.60 Social climate, shaped by norms and interactions, influences how employees perceive their workplace interactions, fostering trust, collaboration, and shared values.61–63 Positive social climates in healthcare, predominantly studied among doctors and nurses, contribute to high work engagement and well-being.64 However, limited attention has been given to First-Line Managers (FLMs) in this context.
FLM engagement across medical specialties is influenced by the workplace’s social climate, empowering them to lead effectively, act independently, and cope with demands, reducing burnout risk.65,66 A negative social climate may lead FLMs to feel undervalued, and studies suggest a moderate link between climate and FLM structural empowerment.67 Positive social climates yield favorable outcomes at both individual and organizational levels, mediated by FLM resilience.63
In healthcare settings, positive social climates enhance staff and patient satisfaction, interaction quality, and perception of wards as safe places.68 Conversely, negative social climates are linked to increased aggression.69,70 Social climate significantly influences patient satisfaction, impacting overall facility perception.71 Active management and monitoring of social climate are crucial for healthcare facilities, given its potential impact on ratings.14,72
Understanding the connections between social climate, job satisfaction, engagement, and burnout is essential for effective climate management.73,74 Recent research emphasizes the need for a positive organizational climate in the healthcare sector to maintain motivation, commitment, job satisfaction, and innovative behavior.74–76 Empirical analysis supports a positive human resource-oriented social climate enhancing work engagement.64 Consequently, we hypothesize that Social Climate (SC) mediates the relationship between Structural Empowerment (SE) and Hospital Rating (HR).
H3: We Hypothesize That the Relationship Between SE and HR is Mediated by SC.
Given that these factors do not operate in isolation but simultaneously, we investigate the model as a whole, assuming that the relationship between SE and HR is simultaneously mediated by First-Line Manager Resilience (FLMR) and Social Climate (SC).
H4: We Assume That the Relationship Between SE and HR is Mediated by FLMR and SC Simultaneously.
Figure 1 illustrates the theoretical model of the study.
 |
Figure 1 Theoretical model of the study. |
Materials and Methods
Sample and Procedures
In this study, we employed quantitative research methods, with data collection conducted via a questionnaire. Prior to its implementation, we conducted a pilot survey in the form of interviews with 10 managers from healthcare facilities. The aim was to validate the relevance of the questions and the entire model in the context of their practical experience. After comparing and making slight modifications to the statements while retaining their relevance, we distributed questionnaire links to first-line managers at 11 university hospitals and 33 general hospitals. These hospitals were part of the Institute for Economic and Social Reforms (INEKO) monitoring program, which provided a set of indicators for their evaluation. Details on the method of data collection for determining the hospital rating are provided in the measurement section. The questionnaire distribution and data collection took place during January and February 2022.
The respondents were first-level managers in the hospitals, including chief executives and head nurses from various clinical areas. We approached them to collaborate in our research, explaining the study’s purpose and offering the opportunity to access the research results if they were interested. At the end of the questionnaire, respondents provided their consent for data processing. A total of 1560 participation requests were sent, with a questionnaire return rate of 35%.
A total of 540 responses were collected from healthcare managers, with an average age of 47.5 years (min.=29, max.=64, SD=9.67) and an average of 14.72 years of experience in a management role (min.=1 year, max.=24 years, SD=10.41). Among these managers, 40% were female, and 60% were male, and all held a university degree. Additionally, 30% had completed specialization courses in management. The hospitals where these managers worked were both government-owned (51%) and privately-owned (49%), and all of them were facilities with a staff size exceeding 250.
All the measurement instruments used in the study were standardized. Since these instruments were not available in the Slovak language, we addressed intercultural complexities by following the recommendations of,77 which included the process of back-translation before administering the instruments. The first step involved translating the instruments from English into Slovak, followed by back-translation to verify accuracy. Bilingual experts carried out the translation, and any ambiguities were resolved by modifying statements while preserving their intended meaning.
The questionnaire comprised 32 indicator variables, in addition to the identification data. To mitigate common method bias, a common challenge in research, we used concise, straightforward sentences. Items were randomly distributed and intermixed to prevent response interference. We also conducted collinearity statistics, including the calculation of the VIF.
The values found were less than or equal to 3.3, therefore we can conclude that our chosen model is not subject to common method bias.78
Measures
Hospital rating (HR) values were obtained from data from INEKO (Institute for Economic and Social Reforms), a non-governmental organization that annually awards the Hospital of the Year award and publishes a ranking of hospitals in Slovakia. This award does not comprehensively assess the quality of inpatient healthcare facilities but informs about their performance based on available selected indicators of patient satisfaction, indicators of the quality of healthcare provided, the operational experience of doctors, the complexity of diagnoses, management, and transparency over the past four-year period (HR1 to HR6). INEKO collects data from health insurance companies (VšZP, Dôvera, Union), health care institutions, the Ministry of Health of the Slovak Republic, the Ministry of Finance of the Slovak Republic, municipalities, the Health Care Supervision Authority of the Slovak Republic, the National Centre for Health Information, the Operational Centre of the Emergency Medical Service of the Slovak Republic, and Transparency International Slovakia. 11 university hospitals and 33 general hospitals in Slovakia passed the qualification criteria, which ensure the relevance of the assessment. The resulting hospital rating is calculated as a weighted average of the scores achieved for the above indicators.
The overall performance assessment of hospitals consists of 6 categories. Individual criteria contribute to the assessment with different weights. The criteria like quality + patient satisfaction, together comprise almost 60% of the overall assessment. However, other criteria also reflect performance, which is influenced by the management level at the FLM level. The quantity and complexity of services that a healthcare facility is capable of delivering in a year partly reflect the quality of its management. The same applies to economic results and the hospital’s openness to its environment. These criteria, which are related to the quality of FLM management, are indirectly accounted for in the overall performance assessment of the facility with lesser weight. Table 1 describes the criteria included in the INEKO assessment.
 |
Table 1 Criteria Included in the INEKO Assessment |
The criteria were evaluated over a period of 4 years, ensuring stability of quality, with the weights of the data decreasing towards the past (the data from the last evaluated year having the highest weight). Individual criteria are converted into point values ranging from 0 to 100 points.
In total, a facility can receive a maximum of 100 points, with a minimum of 0 points. The higher the score, the better the rating and ranking. The resilience of first-line managers (FLMR) was assessed using the Connor-Davidson Resilience Scale (CD-RISC) (Campbell-Sills & Stein, 2007). This validated 10-item Measure of Resilience is a shortened version of the original 25-item instrument for measuring resilience. Respondents rated these 10 resilience items using a 5-point Likert scale (1 = never, 2 = exceptionally, 3 = sometimes, 4 = often, 5 = almost always). This instrument has demonstrated satisfactory psychometric properties and has been used in other studies.79
Social climate (SC) was assessed using a 10-item instrument developed by.62 Respondents rated these items on a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree). This instrument has also shown satisfactory psychometric properties and has been utilized in other studies.63
Structural empowerment (SE) was assessed using the Conditions of Work Effectiveness Questionnaire-II (CWEQ-II),80 which consists of 12 items. This instrument is built upon Kanter’s model of work support and includes four dimensions: opportunities, information, support, and resources. The questionnaire’s aim is to determine the extent of first-line managers’ access to each dimension mentioned above. A five-point scale was used, ranging from 1 (no access) to 5 (full access). The published reliability coefficients for the scale items have been reported in the range of 0.78 to 0.89 in various studies.56,81,82 Table 2 provides an overview of latent variable categories and descriptors utilized in the study, offering a comprehensive classification of the analyzed variables.
 |
Table 2 Latent Variable Categories and Descriptors |
Age (in years), management experience (in years), gender (0 for male, 1 for female), and completion of specialization studies in management (0 for no, 1 for yes) were included as control variables. These control variables were chosen based on their theoretical relevance and the potential influence on the studied relationships. Notably, these same control variables have been employed in previous healthcare studies.83–85
Data Analysis
Data analysis was performed using SmartPLS 3.3 software,86 the primary software used in partial least squares structural equation modeling (PLS-SEM). We used this tool because of its ability to estimate complex models with many constructs, indicator variables, and structural paths (direct and indirect) without imposing distributional assumptions on the data. PLS-SEM allows for a better understanding of the relationships between the selected latent and observed variables. SmartPls as a software support allows to test multiple hypotheses simultaneously, examines direct and indirect effects in complex system, highlights and enables prediction in estimating statistical models.
Results
Our model comprises a set of variables, and it’s crucial to assess the measurement model’s reliability and validity to ensure it meets our predefined criteria. The reliability criterion is met as all standardized loadings exceed 0.70 (Chin, 2010). We retained variables SC1 and SC7 in the model, despite their lower factor loadings, and excluded variables SE1 and SE11 due to low factor loadings.
Furthermore, our intrinsic construct reliability, assessed using Cronbach’s alpha, composite reliabilities (CR), and rho, also meets the requirements. Cronbach’s alpha falls within the 0.7 to 0.95 range for all constructs. CR, the most liberal criterion, also satisfies these criteria. Rho_A falls between Cronbach’s alpha and CR, aligning with theoretical expectations.87
Convergent validity was confirmed by calculating the average variance extracted (AVE), which exceeds the 0.5 threshold for most constructs, with SC and SE values coming close to 0.5. This indicates that the construct explains at least 50% of its item’s variance. Discriminant validity was evaluated using three indicators. This adjustment maintains the original content while enhancing the text’s overall flow and readability.
We ensured discriminant validity using two well-established methods. First, we applied the Fornell-Larcker criterion, where the square root of AVE for each construct exceeded the inter-construct correlation. Additionally, we utilized the heterotrait-monotrait ratio of correlations, which yielded values below the acceptable threshold of 0.90,88 confirming the discriminant validity.
To further verify discriminant validity, we conducted cross-loading calculations to assess how factors loaded onto their respective constructs. While we successfully established discriminant validity, we refrain from providing specific values due to the extensive volume of data. Tables 3–5 offer a detailed analysis of model performance, including loadings, reliability, and validity measures, as well as criteria for discriminant validity.
 |
Table 3 Loadings, Reliability and Validity |
 |
Table 4 Discriminant Validity (Fornell-Lacker Criterion) |
 |
Table 5 Discriminant Validity (HTMT Criterion) |
Structural Model
We evaluated the model’s predictive significance and path significance using R2 and Q2 values, both of which meet the defined criteria. With an R2 value exceeding 0.1, we confirm the model’s predictive capability. Furthermore, Q2 values above 0 indicate the model’s predictive relevance. The SRMR value of 0.056 demonstrates an acceptable model fit. Tables 6–8 provide essential insights into model fit, R Square statistics, and construct cross validated redundancy, contributing to a comprehensive understanding of the model’s efficacy.
 |
Table 6 Model Fit |
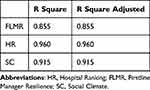 |
Table 7 R Square Statistics |
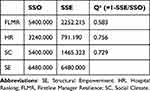 |
Table 8 Construct Cross Validated Redundancy |
Table 9 presents all observed results (path coefficients) and other related values (STDev, T statistics, p values).
 |
Table 9 Path Coefficients, Total Effects Results, Direct and Indirect Effects Results |
All direct effects are statistically significant, and the same holds for indirect effects. The results provide support for Hypothesis H1, indicating that SE significantly influences HR (β = 0.858, p < 0.05).
Hypothesis H2 is also supported. The relationship between SE and HR is mediated by FLMR, with a significant indirect effect (β = 0.602, p < 0.05). This mediation is incomplete, as the indirect effect size is less than 80%. FLMR explains 70% of the total effect as an indirect effect, while the direct effect contributes to the remaining 30% of the total effect. Hypothesis H3 is supported as well. It shows that the relationship between SE and HR is mediated by SC, with a significant indirect effect (β = 0.567, p < 0.05). Similar to H2, this mediation is incomplete, with the indirect effect size below 80% (66% indirect, 34% direct effect). The effect size is comparable to the mediation by FLMR.
Additionally, we find support for Hypothesis H4, which indicates a mediation effect involving two mediators, following a pattern of incomplete mediation. Of the total effect of SE on HR (0.858), the direct effect accounts for only 23% (0.194), while the remaining 77% of the total effect passes through both mediators simultaneously. Notably, FLMR contributes to a larger share of the indirect effect (61%), compared to the 39% attributed to SC.
We incorporated control variables into the model through multigroup analysis (MGA) and moderation. Once we established measurement invariance of composite models (MICOM), we proceeded with multigroup analysis. The outcomes indicated significant differences in certain pathways under examination. Specifically, we observed disparities in the SE and FLMR pathway and the SE and SC pathway in favor of women. Other coefficients related to the various pathways did not exhibit statistical significance.
Concurrently, we identified a statistically significant difference between managers with a specialization in management and those without in the SE and HR pathway (β=0.313 for those with a management specialization and β=−0.090 for those without) and the FLMR and HR pathway (β=0.524 for those with a management specialization and β=−0.030 for those without).
Furthermore, to assess the impact of managerial experience length and FLMs’ age on the SE and HR relationship, we conducted moderation analysis. Figure 2 illustrates the results of moderation analysis.
 |
Figure 2 Moderation effect of the variable age of FLMs on the relationship between SE and HR. |
The results indicate that the moderating effect of age is significant and negative (β = −0.102, p = 0.044), suggesting that the relationship between SE and HR is more pronounced for younger managers. Figure 3 illustrates the moderating effect of the management practice variable on the relationship between SE and HR.
 |
Figure 3 Moderating effect of the management practice variable on the relationship between SE and HR. |
The moderating effect of management experience length is indeed significant, albeit in a negative direction (β= −0.136, p=0.006). This suggests that the relationship between SE and HR is amplified among managers with less experience in their roles. Those with shorter tenure in management positions tend to derive more substantial benefits from structural empowerment.
Discussion
Hospital ratings serve as vital healthcare quality indicators, influencing patient decisions on hospital selection. In the Slovak context, INEKO assesses hospitals over four years, incorporating indicators like surgery volume, diagnostic complexity, patient satisfaction, management, and transparency. Despite varied methodologies, rating systems consistently demonstrate high predictive capacity, acting as a robust performance gauge.
Our study delves into the impact of structural empowerment (SE) on Hospital Rating (HR), examining the mediating roles of first-line managers’ resilience (FLMR) and social climate (SC). FLMs, crucial in healthcare, face complex demands impacting overall facility performance.89,90 SE significantly influences FLM performance (β = 0.896), aligning with previous studies (Al-Habib, 2020; Donahue et al, 2008; Hagerman et al, 2017). SE enhances employee performance, fostering resilience and reducing burnout.41,56
Positive associations exist between staff SE access and patient satisfaction, quality of care, and professional behaviors.42,44 Our study investigates the direct SE-FLMR-HR relationship, confirming FLMR and SC as significant mediators. FLMR and SC together mediate 77% of the total effect, with FLMR (β = 0.409) outweighing SC (β = 0.256).
Our findings resonate with studies highlighting FLMR’s positive impact on job performance.72 FLMR serves as a coping strategy, aiding effective navigation of challenges.51,53 FLMR, constituting 70% of the total effect, significantly contributes to HR. SC, vital in bolstering FLM performance, aligns with previous research emphasizing its role in motivation and innovative behavior.74,75
Age and management experience moderate SE- HR relationships, with younger and less experienced managers benefitting more. Significant gender and education differences exist, with women and managerially educated FLMs experiencing stronger effects. To address global healthcare challenges, our study advocates a proactive approach, structurally strengthening FLMs, fostering resilience, and cultivating a positive social climate. An integrated strategy, empowering FLMs, building resilience, and nurturing a collaborative social climate, holds promise for enhanced healthcare facility ratings.
Conclusion
The COVID-19 pandemic had a significantly detrimental impact on almost all the monitored indicators of healthcare quality, leading to a decline in various aspects. According to INEKO’s report in 2022, there was a notable reduction in the number of surgical procedures performed, delays in planned operations, and a decrease in the availability and quality of healthcare services. In the Slovak Republic, these issues have resulted in numerous challenges, including doctors going on strike and the resignation of around 2000 medical professionals due to inadequate wages and poor working conditions, as of October 31, 2022. The OECD has repeatedly warned Slovakia about its underfunded healthcare system and has urged the government to urgently implement necessary reforms. Health institutions’ management now faces the daunting task of maintaining the required healthcare performance and quality standards during these challenging conditions. In addition to awaiting systemic changes, they must also mobilize all available internal resources.
Our study offers valuable theoretical and practical insights for healthcare facility management. Theoretical implications encompass a deeper understanding of how the structural empowerment of first-line managers (FLMs) influences the quality of healthcare services. Moreover, our findings shed light on the underlying mechanisms governing this relationship. These implications are not only relevant within the context of the study but also have global applicability. Contemporary healthcare systems face similar challenges across developed countries, and although there may be local specificities, the effects of the variables examined can be considered universal.
On a practical level, our findings have important implications for the top management of healthcare facilities. Ongoing organisational changes, global shortages of healthcare staff, their enormous workload in the context of the ongoing pandemic, and problems with staff retention significantly threaten the quality of healthcare provided. They are therefore global challenges for managers not only in Slovakia (WHO, 2020). To address this situation in healthcare, a proactive approach to structurally strengthening FMLs is emphasized,34 which is considered one of the key factors for ensuring occupational health and organizational performance.29
First-line management plays a pivotal role, facing the dual challenge of achieving organizational objectives and fostering the commitment of their subordinates. To effectively fulfill these roles, their success hinges on the support of senior management and the establishment of enabling conditions, often in the form of structural empowerment. This requirement is especially pronounced for younger and less experienced first-line managers. Research by75 has demonstrated that when first-line managers, as well as other employees, perceive a lack of structural empowerment, it results in diminished engagement in hospital politics and a reduced awareness of organizational goals.
The positive effects of structural empowerment (SE) can be significantly enhanced by bolstering the resilience of first-line managers and cultivating a positive social climate grounded in trust. Healthcare facilities should take these considerations into account when shaping their human resource management processes, aligning with the recommendations of.91
Another noteworthy finding is that all the factors under examination work more effectively when interconnected, amplifying their impact. Therefore, a suitable strategy for healthcare facilities is to create an environment that empowers first-line managers, fosters their resilience in dealing with demanding tasks, and cultivates a social climate based on trust and collaborative synergy across organizational structures. In accordance with the insights of,29 it’s also crucial for first-line managers to have access to career and training opportunities beyond the healthcare team and to develop the skills required for this. These processes necessitate a transformation of management practices, extending from top-level management to the first line of management, with the aim of genuinely empowering staff sustainably.92,93 Such an approach holds the potential to significantly boost the ratings of healthcare facilities through the performance of their key personnel.
Limitations of Research
While our study brings new findings, it also has its limitations that need to be acknowledged. One of them is the use of cross-sectional data. A limitation of our research is also partially the use of the PLS-SEM method. Given that we are working with multilevel data, evaluating data from 44 clinics (units at the macro level) and from FLM (units at the micro level), the most appropriate method for this research would be multilevel analysis, as multilevel data are collected. We see this as a path for future follow-up research. As part of the future direction of the research, we would also like to focus on a deeper examination of the impact of SE on selected HR items such as quality of healthcare and patient satisfaction.
Abbreviations
FLMs, First-line Managers; FLMR, First-line Managers’ Resilience; SE, Structural Empowerment; SC, Social Climate; INEKO, Institute for Economic and Social Reforms.
Ethical Approval
Ethical clearance for the study was granted by the Ethics Committee of the University of Economics in Bratislava. All ethical considerations pertaining to the research were meticulously observed. The research objectives were clearly communicated to the participants, who were encouraged to contribute their data. Data collection was conducted with utmost regard for the confidentiality of the respondents. Participants signified their agreement to partake in the study. The voluntary consent to participate was upheld as a fundamental ethical tenet, with a simultaneous emphasis on ensuring participants were thoroughly informed about the study’s objectives, procedures, and potential risks. The study adhered to the guidelines outlined in the Declaration of Helsinki.
Acknowledgments
We would like to express our sincere gratitude to VEGA n. 1/0010/23, VEGA n. 1/0623/22 and VEGA n. 1/0188/24 for their generous support, which significantly contributed to the successful completion of this research.
Author Contributions
Each author contributed significantly to the conception and design, data acquisition, analysis, and interpretation of the study. They actively participated in drafting the article and critically revising it for important intellectual content. All authors endorsed the submission to the present journal, provided final approval for the version intended for publication, and committed to being accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Odone A, Buttigieg S, Ricciardi W, Azzopardi-Muscat N, Staines A. Public health digitalization in Europe. Euro J Pub Health. 2019;29(Supplement_3):28–35. doi:10.1093/eurpub/ckz161
2. Rosalia RA, Wahba K, Milevska-Kostova N. How digital transformation can help achieve value-based healthcare: Balkans as a case in point. Lancet Region Health. 2021;4:100100. doi:10.1016/j.lanepe.2021.100100
3. Wilson D, Sheikh A, Görgens M, Ward K; World Bank. Technology and universal health coverage: examining the role of digital health. J Glob Health. 2021;11:16006. doi:10.7189/jogh.11.16006
4. Kickbusch I, Agrawal A, Jack A, Lee N, Horton R. Governing health futures 2030: growing up in a digital world—a joint the lancet and financial times commission. Lancet. 2019;394(10206):1309. doi:10.1016/S0140-6736(19)32181-6
5. Wong BLH, Maaß L, Vodden A, et al. The Dawn of digital public health in Europe: implications for public health policy and practice. Lancet Region Health. 2022;14:100316. doi:10.1016/j.lanepe.2022.100316
6. Lamb A, Martin‐Misener R, Bryant‐Lukosius D, Latimer M. Describing the leadership capabilities of advanced practice nurses using a qualitative descriptive study. Nurs Open. 2018;5(3):400–413. doi:10.1002/nop2.150
7. Shakeri Hossein Abad Z, Kline A, Sultana M, et al. Digital public health surveillance: a systematic scoping review. Npj Digit Med. 2021;4(1):41. doi:10.1038/s41746-021-00407-6
8. Hoşgör H, Yaman M. Investigation of the relationship between psychological resilience and job performance in Turkish nurses during the Covid‐19 pandemic in terms of descriptive characteristics. J Nurs Manage. 2022;30(1):44–52. doi:10.1111/jonm.13477
9. Galura S. On the Frontlines of Nursing Leadership. Nurse Leader. 2020;18(5):476–480. doi:10.1016/j.mnl.2020.05.012
10. Ericsson U, Augustinsson S. The role of first line managers in healthcare organisations – a qualitative study on the work life experience of ward managers. J Res Nurs. 2015;20(4):280–295. doi:10.1177/1744987114564258
11. Yuan CM, Chen X, Zeng X, Mao XR. The disaster resilience trajectory of the first batch front-line nurses at fighting the Novel Coronavirus Disease 2019 in Wuhan: a qualitative study. Int J Disaster Risk Reduct. 2022;77:103071. doi:10.1016/j.ijdrr.2022.103071
12. Hybinette K, Pukk Härenstam K, Ekstedt M. A First-line management team’s strategies for sustaining resilience in a specialised intensive care unit—a qualitative observational study. BMJ Open. 2021;11(3):e040358. doi:10.1136/bmjopen-2020-040358
13. Hedsköld M, Sachs MA, Rosander T, von Knorring M, Pukk Härenstam K. Acting between guidelines and reality- an interview study exploring the strategies of first line managers in patient safety work. BMC Health Serv Res. 2021;21(1):48. doi:10.1186/s12913-020-06042-3
14. Sawada U, Shimazu A, Kawakami N, Miyamoto Y, Speigel L, Leiter MP. The effects of the Civility, Respect, and Engagement in the Workplace (CREW) program on social climate and work engagement in a psychiatric ward in japan: a pilot study. Nurs Rep. 2021;11(2):320–330. doi:10.3390/nursrep11020031
15. Hong KJ, Cho SH. Associations between nurse staffing levels, patient experience, and hospital rating. Healthcare. 2021;9(4):387. doi:10.3390/healthcare9040387
16. Mistry JB, Gwam CU, Chughtai M, et al. Factors influencing patients’ hospital rating after total joint arthroplasty. Orthopedics. 2017;40(6):377–380. doi:10.3928/01477447-20171019-03
17. Mets EJ, Mercier MR, Hilibrand AS, Scott MC, Varthi AG, Grauer JN. Patient-related factors and perioperative outcomes are associated with self-reported hospital rating after spine surgery. Clin Orthop Relat Res. 2020;478(3):643–652. doi:10.1097/CORR.0000000000000892
18. Martsolf GR, Gibson TB, Benevent R, et al. An examination of hospital nurse staffing and patient experience with care: differences between cross-sectional and longitudinal estimates. Health Serv Res. 2016;51(6):2221–2241. doi:10.1111/1475-6773.12462
19. O’Leary KJ, Darling TA, Rauworth J, Williams MV. Impact of hospitalist communication‐skills training on patient‐satisfaction scores. J Hosp Med. 2013;8(6):315–320. doi:10.1002/jhm.2041
20. Belasen AT, Oppenlander J, Belasen AR, Hertelendy AJ. Provider–patient communication and hospital ratings: perceived gaps and forward thinking about the effects of COVID-19. Int J Qual Health Care. 2021;33(1):mzaa140. doi:10.1093/intqhc/mzaa140
21. Carvalho MM, Rabechini Junior R. Impact of risk management on project performance: the importance of soft skills. Int J P Res. 2015;53(2):321–340. doi:10.1080/00207543.2014.919423
22. Black N. Assessing the quality of hospitals. BMJ. 2010;340(apr19 2):c2066–c2066. doi:10.1136/bmj.c2066
23. Mohapatro A, Mahendran SK, Das TK. A framework for ranking hospitals based on customer perception using rough set and soft set techniques. Int J Healthc Inform Syst Inform. 2020;15(1):40–62. doi:10.4018/IJHISI.2020010103
24. Wagner D, Bear M. Patient satisfaction with nursing care: a concept analysis within a nursing framework. J Adv Nurs. 2009;65(3):692–701. doi:10.1111/j.1365-2648.2008.04866.x
25. Armstrong KJ, Laschinger H. Structural empowerment, magnet hospital characteristics, and patient safety culture: making the link. J Nurs Care Qual. 2006;21(2):124–132. doi:10.1097/00001786-200604000-00007
26. Donahue MO, Piazza IM, Griffin MQ, Dykes PC, Fitzpatrick JJ. The relationship between nurses’ perceptions of empowerment and patient satisfaction. Appl Nurs Res. 2008;21(1):2–7. doi:10.1016/j.apnr.2007.11.001
27. Schmutz J, Manser T. Do team processes really have an effect on clinical performance? A systematic literature review. Br J Anaesth. 2013;110(4):529–544. doi:10.1093/bja/aes513
28. Wong CA, Cummings GG. The relationship between nursing leadership and patient outcomes: a systematic review. J Nurs Manag. 2007;15(5):508–521. doi:10.1111/j.1365-2834.2007.00723.x
29. Cougot B, Gauvin J, Gillet N, et al. Impact at two years of an intervention on empowerment among medical care teams: study protocol of a randomised controlled trial in a large French university hospital. BMC Health Serv Res. 2019;19(1):927. doi:10.1186/s12913-019-4724-7
30. Anhang Price R, Elliott MN, Cleary PD, Zaslavsky AM, Hays RD. Should health care providers be accountable for patients’ care experiences? J GEN INTERN MED. 2015;30(2):253–256. doi:10.1007/s11606-014-3111-7
31. Elliott MN, Lehrman WG, Goldstein EH, et al. Hospital survey shows improvements in patient experience. Health Affairs. 2010;29(11):2061–2067. doi:10.1377/hlthaff.2009.0876
32. Kanter RM Men and Women of the Corporation; 1977.
33. Al‐Hammouri MM, Rababah JA, Ta’an WF. Structural empowerment, formal and informal power, and job performance quality: a moderated mediation analysis. J Nurs Manag. 2021;29(6):1596–1602. doi:10.1111/jonm.13311
34. Lundin K, Silén M, Strömberg A, Engström M, Skytt B. Staff structural empowerment—Observations of first‐line managers and interviews with managers and staff. J Nurs Manage. 2022;30(2):403–412. doi:10.1111/jonm.13513
35. Monje Amor A, Xanthopoulou D, Calvo N, Abeal Vázquez JP. Structural empowerment, psychological empowerment, and work engagement: a cross-country study. Eur Manage J. 2021;39(6):779–789. doi:10.1016/j.emj.2021.01.005
36. Almost J, Spence Laschinger HK. Workplace empowerment, collaborative work relationships, and job strain in nurse practitioners. J Amer Acad Nurse Practiti. 2002;14(9):408–420. doi:10.1111/j.1745-7599.2002.tb00142.x
37. McCorkle R, Engelking C, Knobf FAAN, et al. Transition to a new cancer care delivery system: opportunity for empowerment of the role of the advanced practice provider. JADPRO. 2012;3(1). doi:10.6004/jadpro.2012.3.1.4
38. Jankelová N, Joniaková Z, Blštáková J, Skorková Z, Procházková K. Leading employees through the crises: key competences of crises management in healthcare facilities in coronavirus pandemic. RMHP. 2021;14:561–573. doi:10.2147/RMHP.S288171
39. Hagerman H, Högberg H, Skytt B, Wadensten B, Engström M. Empowerment and performance of managers and subordinates in elderly care: a longitudinal and multilevel study. J Nurs Manag. 2017;25(8):647–656. doi:10.1111/jonm.12504
40. Narzary G, Palo S. Structural empowerment and organisational citizenship behaviour: the mediating–moderating effect of job satisfaction. Person Rev.2020;49(7):1435–1449. doi:10.1108/PR-11-2019-0632
41. Meng L, Liu Y, Liu H, Hu Y, Yang J, Liu J. Relationships among structural empowerment, psychological empowerment, intent to stay and burnout in nursing field in mainland China-based on a cross-sectional questionnaire research: relations among empowerment, intent to stay and burnout. Int J Nurs Pract. 2015;21(3):303–312. doi:10.1111/ijn.12279
42. Engström M, Skytt B, Nilsson A. Working life and stress symptoms among caregivers in elderly care with formal and no formal competence: working life for caregivers with formal and no formal competence. J Nurs Manage. 2011;19(6):732–741. doi:10.1111/j.1365-2834.2011.01270.x
43. Engström M, Högberg H, Strömberg A, Hagerman H, Skytt B. Staff working life and older persons’ satisfaction with care: a multilevel, correlational design. J Nurs Care Qual. 2021;36(1):E7–E13. doi:10.1097/NCQ.0000000000000463
44. Manojlovich M. Predictors of professional nursing practice behaviors in hospital settings. J Nurs Admin. 2010;40(10):S45–S51. doi:10.1097/NNA.0b013e3181f37e7d
45. Kuşcu Karatepe H, Türkmen E. Nurse performance: a path model of clinical leadership, creative team climate and structural empowerment. J Clin Nurs. 2023;32(3–4):584–596. doi:10.1111/jocn.16419
46. Van Bogaert P, Peremans L, de Wit M, et al. Nurse managers’ perceptions and experiences regarding staff nurse empowerment: a qualitative study. Front Psychol. 2015:6. doi:10.3389/fpsyg.2015.01585
47. Luthar SS, Cicchetti D, Becker B. The construct of resilience: a critical evaluation and guidelines for future work. Child Development. 2000;71(3):543–562. doi:10.1111/1467-8624.00164
48. Tau B, Du Plessis E, Koen D, Ellis S. The relationship between resilience and empowering leader behaviour of nurse managers in the mining healthcare sector. Curationis. 2018;41(1). doi:10.4102/curationis.v41i1.1775
49. Spiva L, Davis S, Case-Wirth J, et al. The effectiveness of charge nurse training on leadership style and resiliency. J Nurs Admin. 2020;50(2):95–103. doi:10.1097/NNA.0000000000000848
50. Ablett JR, Jones RSP. Resilience and well-being in palliative care staff: a qualitative study of hospice nurses’ experience of work. Psycho-Oncology. 2007;16(8):733–740. doi:10.1002/pon.1130
51. Cameron F, Brownie S. Enhancing resilience in registered aged care nurses: enhancing resilience in aged care nurses. Australas J Ageing. 2010;29(2):66–71. doi:10.1111/j.1741-6612.2009.00416.x
52. Gillespie BM, Chaboyer W, Wallis M, Grimbeek P. Resilience in the operating room: developing and testing of a resilience model. J Adv Nurs. 2007;59(4):427–438. doi:10.1111/j.1365-2648.2007.04340.x
53. Hodges HF, Keeley AC, Troyan PJ. Professional resilience in baccalaureate-prepared acute care nurses: FIRST STEPS. Nurs Educ Perspect. 2008;29(2):80–89. doi:10.1097/00024776-200803000-00008
54. Fletcher D, Sarkar M. Psychological resilience: a review and critique of definitions, concepts, and theory. Eur Psychol. 2013;18(1):12–23. doi:10.1027/1016-9040/a000124
55. Atkinson PA, Martin CR, Rankin J. Resilience revisited. J Psychiatr Ment Health Nurs. 2009;16(2):137–145. doi:10.1111/j.1365-2850.2008.01341.x
56. Wong CA, Laschinger HKS. Authentic leadership, performance, and job satisfaction: the mediating role of empowerment. J Adv Nurs. 2013;69(4):947–959. doi:10.1111/j.1365-2648.2012.06089.x
57. Karltun A, Karltun J, Coelho DA, Havemose K, Kjellström S. The work of first line managers – a key to resilience in manufacturing. Appl. Ergon. 2023;110:103993. doi:10.1016/j.apergo.2023.103993
58. Al-Surimi K, Alhayek Z, Edvardsson D, Al-Khateeb B, Shaheen N. Person-centered-care climate in a tertiary hospital: staff perspective. Risk Manage Healthc Policy. 2021;14:4269–4279. doi:10.2147/RMHP.S317947
59. Guest D, Conway N. The impact of HR practices, HR effectiveness and a ‘strong HR system’ on organisational outcomes: a stakeholder perspective. Int J Human Resour Manage. 2011;22(8):1686–1702. doi:10.1080/09585192.2011.565657
60. Khuluqo IE, Cholik C. Principal’s visionary leadership and work climate toward elementary school teachers’ performance. AIJP. 2022;14(3):3545–3556. doi:10.35445/alishlah.v14i3.2018
61. Collins CJ, Smith KG. Knowledge exchange and combination: the role of human resource practices in the performance of high-technology firms. Acad Manage J. 2006;49(3):544–560. doi:10.5465/AMJ.2006.21794671
62. Prieto IM, Pilar Pérez Santana M. Building ambidexterity: the role of human resource practices in the performance of firms from Spain. Hum Resour Manage. 2012;51(2):189–211. doi:10.1002/hrm.21463
63. Cooper B, Wang J, Bartram T, Cooke FL. Well‐being‐oriented human resource management practices and employee performance in the Chinese banking sector: the role of social climate and resilience. Human Resour Manage. 2019;58(1):85–97. doi:10.1002/hrm.21934
64. Ancarani A, Mauro CD, Giammanco MD. Linking organizational climate to work engagement: a study in the healthcare sector. Int J Public Administration. 2019;42(7):547–557. doi:10.1080/01900692.2018.1491595
65. Lautizi M, Laschinger HKS, Ravazzolo S. Workplace empowerment, job satisfaction and job stress among Italian mental health nurses: an exploratory study. J Nurs Manage. 2009;17(4):446–452. doi:10.1111/j.1365-2834.2009.00984.x
66. Viinikainen S, Rostila I, Green P, Asikainen P, Helminen M, Suominen T. The organizational social context in public healthcare as viewed by first-line nursing managers: a cross-sectional study. Nordic J Nurs Res. 2020;40(2):89–96. doi:10.1177/2057158519878342
67. Trus M, Galdikiene N, Balciunas S, Green P, Helminen M, Suominen T. Connection between organizational culture and climate and empowerment: the perspective of nurse managers. Nursing & Health Sciences. 2019;21(1):54–62. doi:10.1111/nhs.12549
68. Bressington D, Stewart B, Beer D, MacInnes D. Levels of service user satisfaction in secure settings – a survey of the association between perceived social climate, perceived therapeutic relationship and satisfaction with forensic services. Int J Nurs Stud. 2011;48(11):1349–1356. doi:10.1016/j.ijnurstu.2011.05.011
69. Ros N, Van der Helm P, Wissink I, Stams GJ, Schaftenaar P. Institutional climate and aggression in a secure psychiatric setting. J Foren Psychiatr Psychol. 2013;24(6):713–727. doi:10.1080/14789949.2013.848460
70. van der Helm P, Stams GJ, van Genabeek M, van der Laan P. Group climate, personality, and self-reported aggression in incarcerated male youth. J Foren Psychiatr Psychol. 2012;23(1):23–39. doi:10.1080/14789949.2011.633615
71. Tuvesson H, Wann-Hansson C, Eklund M. The ward atmosphere important for the psychosocial work environment of nursing staff in psychiatric in-patient care. BMC Nurs. 2011;10(1):12. doi:10.1186/1472-6955-10-12
72. Zhao J, Wu X, Chen Y, et al. What makes a hospital excellent? A qualitative study on the organization and management of five leading public hospitals in China. RMHP. 2023;16:1915–1927. doi:10.2147/RMHP.S424711
73. Hitka M, Štarchoň P, Caha Z, Lorincová S, Sedliačiková M. The global health pandemic and its impact on the motivation of employees in micro and small enterprises: a case study in the Slovak Republic. Econom Res. 2022;35(1):458–479. doi:10.1080/1331677X.2021.1902365
74. Mishra B, Tikoria J. Impact of ethical leadership on organizational climate and its subsequent influence on job commitment: a study in hospital context. JMD. 2021;40(5):438–452. doi:10.1108/JMD-08-2020-0245
75. Carlucci D, Schiuma G. Organizational climate as performance driver: health care workers’ perception in a large hospital. J Health Manage. 2014;16(4):583–594. doi:10.1177/0972063414548561
76. Purohit B, Wadhwa A. Organisational climate from view point of motivation in district hospital, India. Health. 2012;04(07):400–406. doi:10.4236/health.2012.47063
77. Schaffer BS, Riordan CM. A review of cross-cultural methodologies for organizational research: a best- practices approach. Organization Res Methods. 2003;6(2):169–215. doi:10.1177/1094428103251542
78. Kock N. Common Method Bias in PLS-SEM: a Full Collinearity Assessment Approach. Int J e-Collaboration. 2015;11(4):1–10. doi:10.4018/ijec.2015100101
79. Kašpárková L, Vaculík M, Procházka J, Schaufeli WB. Why resilient workers perform better: the roles of job satisfaction and work engagement. J Workplace Behav Health. 2018;33(1):43–62. doi:10.1080/15555240.2018.1441719
80. Laschinger HKS, Finegan J. Using empowerment to build trust and respect in the workplace: a strategy for addressing the nursing shortage. Nurs Econom. 2005;23:6–13.
81. Greco P, Spence Laschinger H, Wong C. Leader empowering behaviours, staff nurse empowerment and work engagement/burnout. cjnl. 2006;19(4):41–56. doi:10.12927/cjnl.2006.18599
82. Patrick A, Laschinger HKS, Wong C, Finegan J. Developing and testing a new measure of staff nurse clinical leadership: the clinical leadership survey: leadership and management in mental health nursing. J Nurs Manage. 2011;19(4):449–460. doi:10.1111/j.1365-2834.2011.01238.x
83. Kalisch BJ, Lee H, Rochman M. Nursing staff teamwork and job satisfaction: nursing staff teamwork and job satisfaction. J Nurs Manage. 2010;18(8):938–947. doi:10.1111/j.1365-2834.2010.01153.x
84. Stefanidis A, Strogilos V. Perceived organizational support and work engagement of employees with children with disabilities. PR. 2021;50(1):186–206. doi:10.1108/PR-02-2019-0057
85. Vesterinen S, Suhonen M, Isola A, Paasivaara L, Laukkala H. Nurse managers’ perceptions related to their leadership styles, knowledge, and skills in these areas—a viewpoint: case of health centre wards in Finland. ISRN Nurs. 2013;2013:1–8. doi:10.1155/2013/951456
86. Hair JF, Hult GTM, Ringle CM, Sarstedt M, Danks NP, Ray S. Partial Least Squares Structural Equation Modeling (PLS-SEM) Using R: A Workbook. Springer International Publishing; 2021. doi:10.1007/978-3-030-80519-7
87. Ringle CM, Sarstedt M, Mitchell R, Gudergan SP. Partial least squares structural equation modeling in HRM research. Int J Human Resour Manage. 2020;31(12):1617–1643. doi:10.1080/09585192.2017.1416655
88. Henseler J, Ringle CM, Sarstedt M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J Acad Mark Sci. 2015;43(1):115–135. doi:10.1007/s11747-014-0403-8
89. Van Der Borg WE, Verdonk P, Dauwerse L, Abma TA. Work-related change in residential elderly care: trust, space and connectedness. Hum Relat. 2017;70(7):805–835. doi:10.1177/0018726716684199
90. Woznyj HM, Heggestad ED, Kennerly S, Yap TL. Climate and organizational performance in long‐term care facilities: the role of affective commitment. J Occupat & Organ Psyc. 2019;92(1):122–143. doi:10.1111/joop.12235
91. Moore SJ, Durst PT, Ritter C, Nobrega D, Barkema HW. Effects of employer management on employee recruitment, satisfaction, engagement, and retention on large US dairy farms. Journal of Dairy Science. 2020;103(9):8482–8493. doi:10.3168/jds.2019-18025
92. Carney MB, Getz I. Freedom, Inc. How corporate liberation unleashes employee potential and business performance; 2016.
93. Lucas V, Spence Laschinger HK, Wong CA. The impact of emotional intelligent leadership on staff nurse empowerment: the moderating effect of span of control. J Nurs Manage. 2008;16(8):964–973. doi:10.1111/j.1365-2834.2008.00856.x
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
