Back to Journals » Risk Management and Healthcare Policy » Volume 17
Human Resources Allocation of the Centers for Disease Control and Prevention in China
Authors Zhou M
Received 29 November 2023
Accepted for publication 8 February 2024
Published 17 February 2024 Volume 2024:17 Pages 341—353
DOI https://doi.org/10.2147/RMHP.S452475
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Minghua Zhou
Department of Administration Office, Luzhou People’s Hospital, Luzhou, Sichuan, People’s Republic of China
Correspondence: Minghua Zhou, Email [email protected]
Objective: To analyze the equity of human resources allocation of the Centers for Disease Control and Prevention (CDCs) and to predict the development in the next five years in China, and to provide a scientific basis for promoting the development of human resources.
Methods: The data of the CDCs from 2017 to 2021 were obtained from the “China Health Statistical Yearbook”, and descriptive analysis, health resource density index (HRDI), Theil index, and health resource agglomeration degree (HRAD) were used to evaluate the equity, and the grey prediction model GM (1, 1) was used to predict the development from 2022 to 2026.
Results: Measured by the HRDI, the shortage of human resources in the western region was relatively obvious, with a shortage of more than 11,656 health technicians, more than 6418 licensed (assistant) physicians, and more than 693 registered nurses. The Theil index of human resources allocation by population was between 0.016 and 0.071, and the Theil index of human resources allocation by geography was between 0.312 and 0.359. The allocation of human resources by geography was more unequal than those allocated by population. In terms of HRAD, human resources are over-allocated equitably by geography in the eastern and central regions, while they are under-allocated equitably by geography in the western region. In terms of the difference between the HRAD and PAD, the eastern region has a shortage of human resources relative to the concentration population, and the western region has an excess of human resources relative to the concentration population.
Conclusion: The human resources allocation of the CDCs in China was uneven. The human resources of the CDCs were allocated more equitably by population than by geography. There was a situation where the equity of human resource allocation of the CDCs was contrary to the actual demand for medical care.
Keywords: human resources, equity, prediction, centers for disease control and prevention, China
Introduction
The Outline of the Healthy China 2030 Plan requires promoting the equalization of basic public health services,1 expanding the content of health services, improving the quality of health services, and enabling urban and rural residents to enjoy equal access to basic public health services.2 As an important part of the public health service system, the Centers for Disease Control and Prevention (CDCs) play an important role in preventing and controlling infectious diseases and chronic noncommunicable diseases,3 and responding to public health emergencies. Health human resources are the total of all persons trained in the health professions who are able to provide health services and contribute to the health sector. In the development of the CDCs, health human resources are the most dynamic resources and the foundation for building CDCs. It is a key element in the implementation of the CDCs task force and represents an important guarantee for the overall improvement of the service capacity of the CDCs. Through the allocation of health human resources, make the health human resources in the region should be made compatible with the health needs of the population and the demand for health services, so as to achieve the goal of obtaining the highest output with the lowest input. The equitable allocation of human resources of the CDCs is important for improving the equity of public health services, improving the quality of public health services and promoting national health.4
At present, the relevant research on human resources of the CDCs in China mainly includes three aspects. First, the quantity, quality, structure and technical level of health personnel in the CDCs, including changes in age, education, and titles of professional and technical personnel, tackling the brain drain in Chinese CDCs by using discrete choice experiment survey.5 Second, the capacity building situation of the CDCs, including the current status and capacity of pathogen laboratories in the CDCs during the COVID-19 pandemic and other requested content.6 Third, the inequity of health resources in the CDCs, including the inequity of public health resources by the health resource density index (HRDI),7 the inequity of the public health workforce at county-level CDCs,8 and the analysis of overall equity by using the Gini coefficient and the Theil index,9 and so on. In terms of research perspectives, relevant studies are less likely to carry out research on human resource allocation of the CDCs in China under the perspective of regional coordinated development; in terms of research methodology, relevant studies are less likely to carry out research on human resource allocation of the CDCs in China by using methods such as the health resource agglomeration degree (HRAD) and the grey prediction model GM (1, 1), and the equity and prediction of human resource allocation of the CDCs in China are still need to be further strengthened. In this study, from the perspective of regional coordinated development, the HRDI, Theil index, and HRAD were used to evaluate the equity of human resources allocation of the CDCs in China from 2017 to 2021, and the grey prediction model GM (1, 1) was used to predict the development of human resources from 2022 to 2026.
Materials and Methods
Data Sources
Data on human resources of the CDCs in China were obtained from the “China Health Statistical Yearbook” (2018–2022), and the population and geographical area were obtained from the “China Statistical Yearbook” (2018–2022). Due to the inconsistency of statistical caliber in Hong Kong, Macao, and Taiwan, the data of this study included the health human resources of CDCs in 31 provincial-level administrative areas (excluding Hong Kong, Macao and Taiwan) in mainland China from 2017 to 2021.
Regional Division
According to the new situation of coordinated regional development in China, the Chinese mainland (excluding Hong Kong, Macao and Taiwan) has been divided into the northeastern region (Heilongjiang, Jilin and Liaoning), the central region (Shanxi, Henan, Hunan, Hubei, Jiangxi and Anhui), the eastern region (Beijing, Tianjin, Hebei, Shandong, Jiangsu, Shanghai, Zhejiang, Fujian, Guangdong and Hainan) and the western region (Chongqing, Sichuan, Guangxi, Yunnan, Guizhou, Shaanxi, Gansu, Inner Mongolia, Qinghai, Ningxia, Xinjiang and Tibet).
Indicators
According to the principles of scientificity and accessibility, health technicians, licensed (assistant) physicians and registered nurses were selected as evaluation indicators. Health technicians include health professionals such as licensed physicians, licensed assistant physicians, registered nurses, pharmacists, laboratory technicians, imaging technicians, health supervisors, and trainee medical technicians (pharmacy, nursing, and technician), excluding health technicians engaged in management work. Licensed (assistant) physician refers to the “level” of “physician’s license” as “licensed (assistant) physician” and actually engaged in medical treatment, preventive health care work, excluding actually engaged in the management of the licensed (assistant) physician. Registered nurse is a person who has a registered nurse certificate and is actually practicing nursing, excluding nurses who are engaged in management.
Research Methods
The descriptive analysis, HRDI, Theil index, and HRAD were used to evaluate the equity of human resources allocation of the CDCs in China from 2017 to 2021, and the grey prediction model GM (1, 1) was used to predict the development of human resources from 2022 to 2026.
Descriptive Analysis
The descriptive analysis method uses the number of human resources per 1000 population and per square kilometer for descriptive analysis.
Health Resource Density Index(HRDI)
HRDI is the arithmetic square root of health human resources per thousand population and per square kilometer,10 which is used to comprehensively measure the balanced allocation of health human resources in a region in terms of resident population and geographical area.11 The higher the HRDI, the better the distribution of health resources.12 The formula is:
The HRDI of human resources of the CDCs in China was used as a reference, and the needs, shortages and shortage ratios of each of the four regions were calculated relative to the reference standard. The formulas are:
Theil Index
The Theil index is used to measure the overall balance of health human resources.13 It has a good decomposition, and can comprehensively reflect the differences within and between regions and the contribution of each part of the differences to the overall differences.14 A higher Theil index indicates worse equity, and a lower Theil index indicates better equity. The formula is:
Where n is the number of regions; Pi is the proportion of the population (or geography) of region i accounts to the total population (or geography); Yi is the proportion of health human resources in the region i accounts to the total health human resources.
Health Resource Agglomeration Degree(HRAD)
HRAD and population agglomeration degree (PAD) are commonly used to evaluate the equity of health human resource allocation.15 HRAD indicates the proportion of health resources concentrated in 1% of the total land area of a region. PAD indicates the proportion of the population concentrated in 1% of the total land area of a region. The formulas is:
HRi is the number of health resources in region i, Ai is the land area of region i, An is the land area of the whole region, and HRn is the total health resources of the whole region. PAD is calculated by replacing the number of health resources by the number of population in the area.
When HRAD is greater than 1, it indicates that health resources are over-allocated equitably by geography, and when HRAD is less than 1, it indicates that there is a shortage.16 When the difference between HRAD and PAD is greater than 0, it indicates that health resources are over-allocated relative to agglomerated populations, and when the difference is less than 0, it indicates that they are under-allocated relative to agglomerated populations.17
Grey Prediction Model GM (1, 1)
The grey prediction model GM (1, 1) represents a grey model of differential equations of order 1 and 1 variable. The basic idea is to use the original data to generate the original data series, generate the cumulative series by accumulation, define the grey derivatives and grey differential equations according to the generated cumulative series, use the least squares method to obtain the development coefficient and the value of the grey role variables, establish the model and the time-response equation, and calculate the predicted value using the time-response equation. Finally, the accuracy of the prediction model is tested by applying the posterior error ratio (C-value) and the small error probability (P-value), when P is greater than 0.95 and C is less than 0.35, it means that the prediction model is reliable and can be used to make predictions.
Statistical Analysis
Excel 2010 was used to establish the database, Excel 2010 was used to calculate the equity of human resource allocation in the CDCs, and SPSS22.0 was used to predict the development of human resources in the CDCs.
Results
Basic Information of Human Resources
The health technicians, licensed (assistant) physicians, and registered nurses per 1000 population of the CDCs in China grew from 0.102, 0.051, and 0.011 in 2017 to 0.112, 0.053, and 0.013 in 2021, respectively. The health technicians, licensed (assistant) physicians, and registered nurses per square kilometer of the CDCs in China grew from 0.015, 0.007, and 0.002 in 2017 to 0.017, 0.008, and 0.002 in 2021, respectively (Table 1).
 |
Table 1 Basic Information of Human Resources in CDCs |
HRDI of Human Resources in CDCs
The HRDI of health technicians, licensed (assistant) physicians, and registered nurses of the CDCs in China increased from 0.039, 0.019, and 0.004 in 2017 to 0.043, 0.020, and 0.005 in 2021, respectively. Taking the human resources of the CDCs in China as a reference, the HRDI of health technicians, licensed (assistant) physicians and registered nurses in the eastern and central regions are above average, and the HRDI of health technicians, licensed (assistant) physicians and registered nurses in the western region are below average, and the HRDI of health technicians in the northeastern region are above average, and the HRDI of registered nurses in the northeastern region are below average (Table 2).
 |
Table 2 HRDI of Human Resources in CDCs |
Demand, Shortage and Shortage Ratio of Human Resources
Using the HRDI of the human resources of the CDCs in China as a reference, the human resources in the eastern and central regions are above average, with health technicians in the eastern and central regions are above average by more than 10,447, licensed (assistant) physicians are above average by more than 4357, and registered nurses are above average by more than 407. The western region has a more obvious shortage of human resources, with a shortage of health technicians of more than 11,656, licensed (assistant) physicians of more than 6418, and registered nurses of more than 693. Health technicians in the northeastern region are slightly above average, and registered nurses in the northeastern region are in a state of shortage, with a shortage ratio of more than 3.7% (Table 3).
 |
Table 3 Demand, Shortage and Shortage Ratio of Human Resources in CDCs |
Theil Index of Human Resources Allocation by Population
The Theil index of human resources allocation by population was between 0.016 and 0.071, the Theil index of health technicians and licensed (assistant) physicians was within 0.020, and the Theil index of registered nurses was above 0.060, indicating that registered nurses were relatively more unequal. The Theil index of health technicians was greater within regions than between regions, indicating that the inequity comes from within regions. The Theil index of licensed (assistant) physicians was smaller within regions than between regions from 2018, indicating that inequity comes mainly from between regions (Table 4).
 |
Table 4 Theil Index of Human Resources Allocation by Population in CDCs |
Theil Index of Human Resources Allocation by Geography
The Theil index of human resources allocation by geography was between 0.312 and 0.359, and the value was larger than the Theil index of human resources allocation by population, indicating that human resources allocation by geography is more unequal. The Theil index of health technicians, licensed (assistant) physicians, and registered nurses was smaller within regions than between regions, indicating that the inequity comes mainly from between regions (Table 5).
 |
Table 5 Theil Index of Human Resources Allocation by Geography in CDCs |
HRAD of Human Resources
The PAD of the eastern and central regions was more than 3.91 and 2.39 respectively, and the PAD of the northeastern and western regions was less than 1. The population of China was relatively concentrated in the eastern and central regions.
In terms of HRAD, health technicians, licensed (assistant) physicians, and registered nurses in the eastern and central regions are all greater than 1, indicating an over-allocation of equity by geography. Health technicians, licensed (assistant) physicians, and registered nurses in the western region are all less than 1, indicating insufficient equity by geography. Health technicians and licensed (assistant) physicians in the northeastern region are less than 1 from 2019, indicating a lack of equity by geography from 2019. Registered nurses in the northeastern region is less than 1, indicating a lack of equity in allocation by geography.
In terms of the difference between the HRAD and PAD, the difference between health technicians, licensed (assistant) physicians and registered nurses in the eastern region is less than 0, indicating a shortage of health human resources relative to the population concentration. The difference between health technicians, licensed (assistant) physicians and registered nurses in the western region is greater than 0, indicating an excess of health human resources relative to the agglomeration population. The difference between health technicians in the northeastern region is greater than 0, indicating that there is an excess of health technicians relative to the agglomeration population. The difference between registered nurses in the northeastern region is less than 0 except in 2021, indicating that there is a shortage of registered nurses relative to the agglomeration population. The difference between health technicians and licensed (assistant) physicians in the central region is less than 0, indicating that there is a shortage of health technicians and licensed (assistant) physicians relative to the agglomeration population (Table 6).
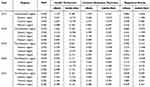 |
Table 6 HRAD of Human Resources in CDCs |
Prediction Model and Test Results of Human Resources in CDCs
The data on human resources of the CDCs in China from 2017 to 2021 were each used as the original data series respectively, and the prediction models of health technicians, licensed (assistant) physicians and registered nurses were established according to the calculation steps of the grey prediction model GM(1,1). Using the posterior error ratio (C-value) and small error probability (P-value) to test the accuracy of the prediction models, P is greater than 0.95 and C is less than 0.35 in the prediction models, and the accuracy level is 1, indicating that the prediction of each model fits well, and the model predictions are accurate and reliable, and can be used for prediction (Table 7).
 |
Table 7 Prediction Model and Test Results of Human Resources in CDCs |
Prediction Results of Human Resources in CDCs from 2017 to 2026
According to the prediction, the predicted value of human resources of the CDCs in China is consistent with the trend of change of the actual value, and the relative error is within 3.236%, indicating that the prediction has a good degree of reasonableness. According to the prediction, the human resources of the CDCs in China will continue to grow, and the number of health technicians, licensed (assistant) physicians, and registered nurses will reach 190,867.94, 81,259.68, and 23,746.89, respectively, in 2026 (Table 8).
 |
Table 8 Prediction Results of Human Resources in CDCs from 2017 to 2026 |
Discussion
The total number of human resources in the CDCs showed a decreasing trend from 2017 to 2019, and the total number of human resources increased rapidly from 2020 to 2021, in which the total number of human resources increased by 5390 in 2020, 13,246 in 2021, and the total number of human resources showed an increasing trend from 2022 to 2026 according to the prediction, indicating that human resources in the CDCs are being developed. Affected by COVID-19 since December 2020, the CDCs have recruited a large number of technicians to work on epidemic prevention and control, and nucleic acid testing, thus promoting the growth of human resources. Under the influence of COVID-19,18 the administration has paid more attention to the construction of the public health service system in terms of policy, actively promoted the enhancement of the capacity to prevent, control and respond to major epidemics and public health emergencies, and strengthened the construction of the CDC’s human resources.
Taking the HRDI of the human resources of the CDCs in China as a reference, the human resource allocation in the eastern and central regions are above average, while the human resource allocation in the western regions are below average, which is consistent with the situation of “more in the east and less in the west” in China’s health resources allocation,19 indicating that the human resources of the CDCs in China are not balanced. Researcher believe there are two reasons for this. First, it is the difference in the level of economic development that leads to the different allocation of human resources in different regions. Theoretically speaking, the region with the better economic foundation will have more financial income to invest in public health, the eastern region has a higher level of economic development, and the western region has a relatively poorer financial foundation, so the human resources allocation in the western region is in a relatively weaker position.20 Second, the human resources of the CDCs are highly mobile, and it is difficult to ensure equity simply by relying on market regulation. The human resources of the CDCs are highly mobile resources, but human resources sometimes move blindly and profitably, thus flowing to areas with better incomes, smooth promotion channels and convenient transportation. Health human resources in the western region are more likely to flow to the eastern and central regions, leading to greater regional disparities in the allocation of human resources. The public health services of the CDCs in China depend on the overall planning and construction of the administration,21 which should implement the main responsibility for the construction, it should actively develop the level of the regional economy, and increase the investment to the CDCs, so as to compensate for the inadequacy of regional human resource allocation.
According to the calculation of HRDI, the shortage in the western region is obvious, the shortage of health technicians is more than 11,656, the shortage of licensed (assistant) physicians is more than 6418, and the shortage of registered nurses is more than 693, indicating that the shortage of human resources in the western region is large, and it is far from being able to meet the demand for public health services for the people in the western region. The western region is vast and sparsely populated, the radius distance of public health services is large, and the cost of public health services is high. Especially in the remote mountainous areas of the western region, which have a poor economic base and harsh environmental conditions, the welfare, education and training of existing health technicians cannot be achieved, which further contributes to the shortage of human resources.22 Therefore, it is necessary to further improve the investment mechanism for human resources development of the CDCs in the western region,23 and to gradually improve the human resources construction in the western region by providing appropriate policy support in terms of income and treatment, promotion of titles, and protection mechanisms. At the same time, it is necessary to further strengthen the education and training of existing health technicians and improve their professional and technical capabilities, in order to better provide public health services to the people.24
The Theil index of human resources by population is between 0.016 1 and 0.071 2, and the Theil index of human resources by geography is between 0.311 9 and 0.358 7. The Theil index of human resources by geography is larger than that by population, indicating that human resources by geography are more unequal than those by population.25 For a long time, the allocation standard of health resources has been based on the possession of health resources per thousand population as the main indicator, and has not taken the geography as a reference factor,26 resulting in the human resource allocation of the CDCs being oriented to meet the service needs of the population, and not fully taking into account the impact of geographical factors on the equity and accessibility of public health services.27 Therefore, it is necessary to improve the construction of the public health service system, strengthen the allocation of human resources in remote and backward areas, and shorten the distance between the people’s enjoyment of public health services, so as to reduce the impact of geographical factors on inequality.
The decomposition of the sources of inequality by the Theil index shows that the inequality of human resources by geography mainly comes from between regions.28 The fact that the eastern region is densely populated and the western region is sparsely populated further contributes to the differences between regions in terms of human resources using population as a criterion for allocation, making the differences between the western region and the other regions the main source of inequity on the Theil index.29 The inequity of human resource allocation by population is complex. The inequity of health technicians comes mainly from within regions, and the inequity of licensed (assistant) physicians and registered nurses comes mainly from between regions. Within regions, different levels of economic development and emphasis on disease prevention and control have resulted in different human resources in different provinces, leading to greater overall differences in health technicians within regions. Between regions, there are already large differences in the allocation of licensed (assistant) physicians and registered nurses in different regions, combined with the characteristic of high mobility of human resources, resulting in significant inequities between regions.30 Therefore, it is necessary to take into account population and geographical factors in the allocation of human resources of the CDCs in China, especially in the western region, in order to meet the public health service needs of the local people. It is necessary to strengthen the training and education of human resources and to improve the skills of public health services in order to promote the full use of the existing human resources and to better serve the people.31
The HRAD calculation shows that the eastern region has an over-equity of health human resources allocation by geography, but an under-equity of health human resources relative to the agglomerated population. On the contrary, the western region has an under-equity of health human resources allocation by geography and an over-equity of health human resources relative to the agglomerated population. This indicates that the equity of human resources is contrary to the actual health care needs of the agglomerated population.32 In regions where the population is agglomerated, such as the eastern region, human resources are more equitably allocated by geography, but there is a shortage of human resources relative to the agglomerated population, which does not meet the health needs of the local agglomerated population. The eastern region has a developed socio-economy, a high population density, and a strong awareness of health care and a greater demand for public health services, resulting in an imbalance between the allocation of human resources and the actual health care needs of the population. In sparsely populated regions such as the western region, human resources are more equitably allocated by population, but there is greater inequity in the allocation of human resources by geography, making it impossible to meet the health needs of the local population. The western region is sparsely populated and characterized by large mixed settlements and small clusters, which makes the radius of public health services larger and the cost of public health services higher,33 and does not adequately take into account the impact of geographical area on the use of health services. Therefore, it is necessary to encourage regions to strengthen research and studies on population distribution and changes in the spectrum of diseases, and to comprehensively consider population and geographical factors in the allocation of human resources.34 At the same time, it is necessary to strengthen counterpart support from human resource-rich regions to weaker regions, so as to maximize the effectiveness of the human resources of the CDCs in China.
Limitations
Although researcher used the HRDI, Theil index and HRAD to analyze the equity of human resource of the CDCs in China, and to predict the development in the next five years, there are still some limitations. First, the evaluation indexes were selected based on previous related studies, which are the evaluation indexes usually used in similar studies. Second, the HRDI of human resources of the CDCs in China suggested that the inflow and outflow of human resources changed more significantly, and the flow of human resources was not analyzed in this study. Third, in addition to further improving the equity of human resources, there is a need to further improve the quality, structure, and technical level of human resources of the CDCs in China, which were not analyzed in this study.
Conclusion
The study used the HRDI, Theil index and HRAD to analyze the equity of human resources of the CDCs in China from 2017 to 2021, and the grey prediction model GM (1, 1) to predict the development of human resources from 2022 to 2026. The study found that using the HRDI of human resources of the CDCs in China as a reference, the HRDI of human resources in the eastern and central regions are above average, and the HRDI of human resources in the western region are below average. Measured by the HRDI, the shortage of human resources in the western region was relatively obvious, with a shortage of more than 11,656 health technicians, more than 6418 licensed (assistant) physicians, and more than 693 registered nurses. The Theil index of human resources allocation by population was between 0.016 and 0.071, and the Theil index of human resources allocation by geography was between 0.312 and 0.359. In terms of HRAD, human resources are over-allocated equitably by geography in the eastern and central regions, while they are under-allocated equitably by geography in the western region. In terms of the difference between the HRAD and PAD, the eastern region has a shortage of human resources relative to the concentration population, and the western region has an excess of human resources relative to the concentration population. According to the prediction, the number of health technicians, licensed (assistant) physicians and registered nurses of the CDCs in China will reach 190,867.94, 81,259.68 and 23,746.89 respectively by 2026. Researcher suggest that it is necessary to take into account the population and geography, focus on strengthening the human resources in the western region, further strengthen the education and training of existing health technicians, and give full play to the maximum effectiveness of human resources of the CDCs in China.
Data Sharing Statement
The datasets supporting the study are publicly available on the China Health Statistics Yearbook (http://www.nhc.gov.cn/) and China Statistical Yearbook (http://www.stats.gov.cn/). The specific situation has been explained in the text.
Ethics Approval and Consent to Participate
The data of the Statistical Yearbook are publicly available. Ethical approval is not needed because there is no secondary data for any personal information.
Funding
This work was supported by the project of 2023 science and technology programme of office of science & technology and talent work of Luzhou (2023ZRK207).
Disclosure
The author declares that they have no competing interests.
References
1. Tao W, Zeng Z, Dang H, et al. Towards universal health coverage: lessons from 10 years of healthcare reform in China. BMJ Global Health. 2020;5(3):e002086. doi:10.1136/bmjgh-2019-002086
2. Ding L, Zhang N, Mao Y. Addressing the maldistribution of health resources in Sichuan Province, China: a county-level analysis. PLoS One. 2021;16(4):e0250526. doi:10.1371/journal.pone.0250526
3. Wang L, Wang Z, Qinglian M, et al. The development and reform of public health in China from 1949 to 2019. Globalization Health. 2019;15(1):45. doi:10.1186/s12992-019-0486-6
4. Dong E, Jie X, Sun X, et al. Differences in regional distribution and inequality in health-resource allocation on institutions, beds, and workforce: a longitudinal study in China. Arch Public Health. 2021;79(1):78. doi:10.1186/s13690-021-00597-1
5. Liu S, Yuanyuan G, Yang Y, et al. Tackling brain drain at Chinese CDCs: understanding job preferences of public health doctoral students using a discrete choice experiment survey. Human Res Health. 2022;20(1):46. doi:10.1186/s12960-022-00743-y
6. Wang J, Niu P, Zhang R, et al. Current status and capacity of pathogen laboratories in centers for disease control and prevention in China during the COVID-19 pandemic: a nationwide cross-sectional survey. Front Public Health. 2022;10:927318. doi:10.3389/fpubh.2022.927318
7. Zhao J, Yang Y, Ogasawara K. Measuring the inequalities in the distribution of public healthcare resources by the HRDI (Health Resources Density Index): data analysis from 2010 to 2019. Healthcare. 2022;10(8):1401. doi:10.3390/healthcare10081401
8. Cai W, Li C, Sun M, et al. Measuring inequalities in the public health workforce at county-level Centers for Disease Control and Prevention in China. Internat J Equ Health. 2019;18(1):179. doi:10.1186/s12939-019-1073-4
9. Li YQ, Hao CH, Guo HY. Examining inequality in the public health workforce distribution in the centers for disease control and prevention (CDCs) System in China, 2008–2017. Biomed Environ Sci. 2020;33(5):374–383. doi:10.3967/bes2020.051
10. Qi J, Qi T, Sun M, et al. Regional disparities of rehabilitation resources for persons with disabilities in China: data from 2014 to 2019. Int J Environ Res Public Health. 2020;17(19):7319. doi:10.3390/ijerph17197319
11. Qiuping L, Xing L, Zhang Q, et al. A cross-sectional nationwide study on accessibility and availability of neonatal care resources in hospitals of china: current situation, mortality and regional differences: neonatal care resources and newborn mortality in China. Lancet Reg Health. 2021;14:100212. doi:10.1016/j.lanwpc.2021.100212
12. Wang Z, Dong L, Xing X, et al. Disparity in hospital beds’ allocation at the county level in China: an analysis based on a Health Resource Density Index (HRDI) model. BMC Health Serv Res. 2023;23(1):1293. doi:10.1186/s12913-023-10266-4
13. Huimin Y, Shuangyan Y, Da H, et al. Equity analysis of Chinese physician allocation based on Gini coefficient and Theil index. BMC Health Serv Res. 2021;21(1):455. doi:10.1186/s12913-021-06348-w
14. Fan X, Zhang W, Guo Y, et al. Equity assessment of the distribution of mental health beds in China: based on longitudinal data from 2011 to 2020. BMC Health Serv Res. 2022;22(1):1453. doi:10.1186/s12913-022-08658-z
15. Wang Y, Yuyang L, Qin S, et al. The disequilibrium in the distribution of the primary health workforce among eight economic regions and between rural and urban areas in China. Internat J Equ Health. 2020;19(1):28. doi:10.1186/s12939-020-1139-3
16. Qianqian Y, Yin W, Huang D, et al. Trend and equity of general practitioners’ allocation in China based on the data from 2012–2017. Human Res Health. 2021;19(1):20. doi:10.1186/s12960-021-00561-8
17. Rixiang X, Tingyu M, Liu Y, et al. Trends in the disparities and equity of the distribution of traditional Chinese medicine health resources in China from 2010 to 2020. PLoS One. 2022;17(10):e0275712. doi:10.1371/journal.pone.0275712
18. Zhang P, Gao J. Evaluation of China’s public health system response to COVID-19. J Global Health. 2021;11:05004. doi:10.7189/jogh.11.05004
19. Chen J, Lin Z, Li-An L, et al. Ten years of China’s new healthcare reform: a longitudinal study on changes in health resources. BMC Public Health. 2021;21(1):2272. doi:10.1186/s12889-021-12248-9
20. Yang T, Rui B, Zhang C. Assessing health human resource structure at Urumqi’s center for disease control and prevention. Medicine. 2023;102(48):e36209. doi:10.1097/MD.0000000000036209
21. Gong H, Wang X, Zhang T, et al. How Can China’s new health care reform promote the balance of interest game?-Based on game evolution and simulation analysis. Risk Manag Health Policy. 2023;16:1435–1454. doi:10.2147/RMHP.S422296
22. Witter S, Hamza MM, Alazemi N, et al. Human resources for health interventions in high- and middle-income countries: findings of an evidence review. Human Res Health. 2020;18(1):43. doi:10.1186/s12960-020-00484-w
23. Wang Z, Lin T, Xing X, et al. Dynamic distribution, regional differences and convergence of health workforce allocation in township health centers in China. Heliyon. 2023;10(1):e23857. doi:10.1016/j.heliyon.2023.e23857
24. Li N, Wang Y, De-E Y, et al. Job satisfaction of staff in agencies for disease prevention and control in Hainan Province, China. J Pak Med Assoc. 2020;70(3):523–525. doi:10.5455/JPMA.5011
25. Wang Z, Haoyu H, Liu X, et al. Health resource allocation in Western China from 2014 to 2018. Arch Public Health. 2023;81(1):30. doi:10.1186/s13690-023-01046-x
26. Huang M, Luo D, Wang Z, et al. Equity and efficiency of maternal and child health resources allocation in Hunan Province, China. BMC Health Serv Res. 2020;20(1):300. doi:10.1186/s12913-020-05185-7
27. Zhengjun L, Yang L, Tang S, et al. Equity and efficiency of health resource allocation of Chinese medicine in Mainland China: 2013–2017. Front Public Health. 2020;8:579269. doi:10.3389/fpubh.2020.579269
28. Yao H, Zhan C, Sha X. Current situation and distribution equality of public health resource in China. Arch Public Health. 2020;78:86. doi:10.1186/s13690-020-00474-3
29. Wang R, Wang Q, Yao S. Evaluation and difference analysis of regional energy efficiency in China under the carbon neutrality targets: insights from DEA and Theil models. J Environ Manage. 2021;293:112958. doi:10.1016/j.jenvman.2021.112958
30. Yingjie F, Wang J, Sun J, et al. Equity in the allocation of general practitioner resources in mainland China from 2012 to 2019. Healthcare. 2023;11(3):398. doi:10.3390/healthcare11030398
31. Dong E, Liu S, Chen M, et al. Differences in regional distribution and inequality in health-resource allocation at hospital and primary health centre levels: a longitudinal study in Shanghai, China. BMJ Open. 2020;10(7):e035635. doi:10.1136/bmjopen-2019-035635
32. Cao F, Yan X, Zheng C, et al. How efficient are basic public health services between Urban and Rural in Shandong Province, China? A data envelopment analysis and panel tobit regression approach. Risk Manag Health Policy. 2022;15:727–738. doi:10.2147/RMHP.S354758
33. Zheng D, Gong J, Zhang C. Efficiency of medical service systems in the rural areas of Mainland China: a comparative study from 2013 to 2017. Public Health. 2019;171:139–147. doi:10.1016/j.puhe.2019.04.003
34. Wanmin S, Du L, Fan Y, et al. Equity and efficiency of public hospitals’ health resource allocation in Guangdong Province, China. Internat J Equ Health. 2022;21(1):138. doi:10.1186/s12939-022-01741-1
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.






