Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 15
Health System Responsiveness for Persons with HIV and Disability in South Western Uganda
Authors Kibet E, Namirimu F, Nakazibwe F, Kyagera AZ, Ayebazibwe D, Omech B
Received 13 April 2023
Accepted for publication 4 August 2023
Published 8 August 2023 Volume 2023:15 Pages 445—456
DOI https://doi.org/10.2147/HIV.S414288
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Olubunmi Akindele Ogunrin
Emmanuel Kibet,1 Florence Namirimu,1 Felista Nakazibwe,1 Arnold Zironda Kyagera,1 Disan Ayebazibwe,1 Bernard Omech2
1Faculty of Medicine, Mbarara University of Sciences and Technology, Mbarara City, Uganda; 2Department of Health Planning and Management, Lira University, Lira City, Uganda
Correspondence: Bernard Omech, Email [email protected]
Background: Inequitable access to Human Immunodeficiency Virus/Acquired Immune Syndrome (HIV/AIDS) Treatment and Care Services (HATCS) for People With Disabilities (PWD) is a hurdle to ending the pandemic by 2030. The aim of this study was to evaluate the Health System’s Responsiveness (HSR) and associated factors for PWD attending HATCS at health facilities in South Western Uganda.
Methods: Between February and April 2022, we enrolled a total of 106 people with disabilities for a quantitative study and 14 key informants from selected primary care HIV clinics. The World Health Organization Multi-country study’s disability assessment schedules 2.0 and Health system responsiveness (HSR) questionnaire were adopted to measure the level of disabilities and responsiveness, respectively. The level of HSR was evaluated using descriptive analysis. The association between socio-demographics, level of disabilities and HSR was evaluated through binary and multivariable logistic regression. The qualitative data were collected from 14 key informants using interview guide and analyzed according to thematic areas (deductive approaches).
Results: Overall, Health system responsiveness (HSR) was at 47.62% being acceptable to people living with HIV and Disabilities in south western Uganda. Across different domains, the best performance was reported in social consideration (68.57%) and autonomy (67.62%). The least performance was registered in dignity (2.83%), confidentiality (2.91%), prompt Attention (17.35%) and Choices (30.48%). Whereas performance in communications (53.92%) and quality of basic amenities (42.27%) were average. There were no socio-demographics or disability variables that were predictive of HATCS responsiveness. PWDs experienced lack of social support, poor communication, stigma and discrimination during the HATCs services. On the other hand, the health-care providers felt frustrated by their inability to communicate effectively with PWDs and meet their need for social support.
Conclusion: HSR was comparatively low, with dignity, confidentiality, prompt attention, and choice ranking worst. To address the universal and legitimate requirements of PWDs in accessing care, urgent initiatives are required to create awareness among all stakeholders.
Keywords: HIV/AIDS, disability, health system responsiveness, Uganda
Background
Over one billion individuals, or 15% of the world’s population, have some form of impairment. More than 80% of disabled persons reside in low- and middle-income nations.1 In Uganda, a National Household Survey in 2016 found a disability prevalence of 12.4% among people aged two and above, implying that about 4.5 million Ugandans report one form or another form of disability. Disability rates rise sharply with age and are higher amongst women and in rural populations.2
Disability is a complex multi-dimensional experience with varied definitions based on different disciplines. The United Nations Convention on the Rights of Persons with Disabilities (UNCRPD) defines disability as
Persons who have long-term physical, mental, intellectual, or sensory impairments that, when combined with other barriers, may prevent them from participating fully and effectively in society on an equal basis with others.3
Disability can shape HIV vulnerabilities in a variety of ways, and health systems must be able to adapt in order to address these vulnerabilities.4 The patient’s experience with HIV/AIDS, disability, and associated debility is unique to the individual, shaped by broader social and structural factors, and frequently includes health needs that go beyond medical interventions.5,6 While HIV and AIDS prevalence has reduced in Uganda, it remains high amongst key populations, including PWDs. People with disabilities are at higher risk of HIV exposure due to stigma, discrimination and limitations in Health care delivery system.7,8
There is currently a growing interest in providing equitable access to HIV care around the world in order to eliminate HIV as a public health threat by 2030.1 However, there is a scarcity of data on the non-medical factors that contribute to vulnerability and how HIV programs can be made more accessible and inclusive for persons with disabilities, particularly in Uganda. National health systems strive for responsiveness, which is a health system goal and a universal indicator for access to care to its beneficiaries. It refers to how well the health system meets people’s genuine expectations for non-health promoting aspects of the health system.4,9 Social ideas of what defines health or ill-health, needs, proper care, and appropriate conduct during the care process impact these expectations.10 The World Health Organization (WHO) has proposed the most extensively used framework for understanding health system responsiveness.11,12 Many countries, including African settings, have validated the concepts of responsiveness, which include autonomy (involvement in medical decision-making), attention (timeliness of care and due attention), respect (dignity and treatment with regard), choice (of care provider and units), confidentiality (keeping medical secrets and maintaining privacy), communication (interactions with service providers), and amenities of care (convenience).13–15 Studies in Ethiopia and Iran revealed that, the more responsive the health system is, the more likely it is that treatments would be successful, that clients’ expectations will be met and that clients will be satisfied with the services.14,15
Uganda has made a series of commitment to the rights of persons with disabilities. The Persons with Disabilities Act (2020) provides for the respect and promotion of human rights for persons with disabilities.16 However, despite the noble intentions outlined in the legislation and policies, very little is known about the responsiveness of primary HIV/AIDS treatment and care services (HATCs) to persons with disabilities and HIV in Uganda. Therefore, the purpose of this study was to assess the responsiveness of the health system and related factors for PWDs utilizing HIV/AIDS treatment and care services at health facilities in South Western Uganda.
Methods and Materials
Study Design and Settings
A cross-sectional study was conducted at health facilities in Bushenyi district, South western Uganda that provide HIV/AIDS treatment and care services from February to April 2022, utilizing explanatory sequential mixed study designs (quantitative followed by qualitative approaches) in order to provide a comprehensive interpretation of the numeric findings in the study context in South Western Uganda. A key informant survey for selected service providers and PWDs was conducted to further understand the experiences and opinion of key stakeholder regarding access to HIV/AIDS services at primary care facilities. The study was conducted among HIV-positive patients attending routine primary care clinics in Bushenyi district. Bushenyi district is a predominantly rural district located 321.3 km southwest of the capital city-Kampala. According to census of 2012, it had about 251,400 people, with 8.5% (12,000) HIV/ADS prevalence and 10.9% (23,530) disability prevalence.17 It has 14 health centre IIs, 8 health centre IIIs, 2 health centre IVs and 3 hospitals. There are usually variable number of medical cadres deployed at each health facility depending on the level of care provided. Doctors are usually posted at Health IVs and Hospital Levels, Clinical officers and Midwives at health centre III, and Midwives and General nurses mostly run health centre IIs. HIV/AIDS treatment and care clinics are located at HCIII and higher levels. Patients are frequently referred after testing HIV positive in other departments or units, and they are registered and assessed on clinic days by a multi-disciplinary team of doctors, nurses, and social workers. There are no known schools for persons with disability in the region or ongoing rehabilitation service in the district.
Sample Size Calculation
For quantitative data, the sample size was estimated using Cohort Study formula.18 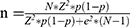 , where
, where  =sample size, N=Total population(=12,000),
=sample size, N=Total population(=12,000),  =proportion of people with disability(=10.9%), Z=the z-value corresponding to 95% CI=1.96, e=the level of precision=0.05. Accordingly, the sampled size was calculated at 136 patients.
=proportion of people with disability(=10.9%), Z=the z-value corresponding to 95% CI=1.96, e=the level of precision=0.05. Accordingly, the sampled size was calculated at 136 patients.
Population and Sampling Procedures
Inclusion Criteria
Patients aged 12 and above who were registered clients for HIV/AIDS treatment and care services in any of the health facilities in Bushenyi district were eligible.
Exclusion Criteria
Patients under the age of 12 years, those who were not resident in Bushenyi district or not enrolled clients of the HATCS in Bushenyi district. Refusal to consent by clients or caretaker. The sample was proportionally allocated to hospitals, health IVs and IIIs that were selected. Participants were consecutively screened from the HATCS clinics register, and those not in attendance were traced to their residence until the sample size was attained. Purposive sampling of informants with rich knowledge from a diverse variety of participants with various disabilities and roles was carried out until qualitative data saturation was attained.
Variables and Measurements
To define and quantify disability, the WHO Disability Assessment Schedule (WHODAS) 2.0 was utilized as the independent variables.19 A disability questionnaire, according to WHODAS 2.0, comprises six characteristics (cognition, mobility, self-care, getting along, life activities and participation) on a Likert scale of 1 to 5, with 1 indicating none and 5 indicating extreme or cannot do. A sequence of questions asked over a period of 30 days determined each domain (Table 1). The indications of 1(none) or 2 (mild) were considered absent and 3–5 were considered present during the evaluation for disability variable.
 |
Table 1 Definitions of Disability Domains |
Outcome Measures
Health system responsive (HSR) module was adapted from World Health Organization Multi-country study as the dependent variable.9,10,12 HSR module contains 34–37 standardized closed ended questions on patients' experiences over a 12 months period under eight domains. The domains include; dignity (four questions), autonomy (four questions), confidentiality (four questions), communication (six questions), prompt attention (six questions), social consideration (two questions), quality of basic amenities (three questions) and Choice and continuity of care (five questions). In the standardized questionnaire, each item was presented with a 5-point Likert scale (response code 1–5) where 1 refers to very bad and 5 represents very good.11 The scores of each of the eight domains were computed by dividing the total scores by the number of items. To calculate the variable health system responsiveness, the overall scores for the eight domains were averaged and translated to percentages (average scores/5 x100%).14,20 The HSR was then classified as unacceptable if the percentage score was less than 70% and acceptable if it was 70% or more.14
Data Collection Tools and Procedures
The quantitative data collection tool comprised Interviewer-administered questionnaire containing questions on socio-demographics (age, gender, level of education, level of income marital status), six disability domains, and adapted 34-item eight health system responsiveness domains.12,21 The questionnaire was previously validated in African population.20,22 The questionnaire was written in English and translated in Local Runyankole language and back to English for validity. Research assistants with medical background qualifications were trained on the questionnaire and pre-tested the tools on 10 patients from Mbarara Teaching hospital. Cronbach’s alpha reliability test checked the reliability of the tools. Accordingly, average Cronbach’s alpha for all domains was 0.82, all showed high internal consistency above the required cut-off 0.70. Semi-structured interviews were conducted with health facility staff and clients with disabilities who were purposely selected with knowledge and expertise in the care of people with disabilities. Interview schedules and questions on their experiences and challenges with care of people with disabilities in their health facility.
Data Processing and Analysis
The data were entered and cleaned using Epi-data info version 7 and analyzed using STATA version 17. The quantitative analysis included descriptive statistics about the health system’s responsiveness and inferential statistics about predictors of the health system’s overall responsiveness of PWD in the setting of HATCS. Descriptive statistics included computation of mean, frequency, and percentages, while inferential statistics involved logistic regression analysis at bivariate and multivariate levels to test for independent associations and determine predictors of HSR, respectively. A p-value of less 0.2 was used to select the variables for inclusion in the multivariate analysis and less 0.05 for determining predictors at multivariate analysis.
In the case of qualitative data, voice recordings and notes of the interview proceedings were done and transcribed shortly after the interviews, based on the interview guides and prompting questions using deductive approaches. Under the study themes, codes were developed, classified, and categorized according to the thematic areas. There was a general summary, interpretation, and explanation.
Ethics Approval and Consent to Participate
In line with the Declaration of Helsinki, we followed all the ethical guidelines and regulations needed to protect the participants from harm. Accordingly, ethical clearance was obtained from institutional review board (IRB) of Mbarara University of sciences and Technology (MUST-2021-294). Permission was obtained from the district health office of Bushenyi and the in-charges of health facilities selected in the district. Informed written consent including permission to publish anonymized responses were obtained from participants and parents or legal guardians of minors and assent from minors prior to enrollment.
Results
Socio-Demographic Characteristics of Participants
A total of 106 were enrolled in the study from 6 health facilities offering HATCS in Bushenyi. More than half (56%) were females, more than 60% were older than 40 years of age and 99% are Christians. Most participants (52.83%) were unable to read and write, 24.53% attained primary level, 10.38% secondary levels and 4.72% had diploma and above. One-third of the participants were married (38.54%), 36.46% were singles and 25% divorced. Majority of the participants were unemployed (55.24%), 4.78% engaged in farming, 8.57% self-employed and the 6.67% formerly employed (Table 2).
 |
Table 2 Socio-Demographic Characteristics of Study Participants (106) |
Accessibility of the Study Participants to HATCS
A majority were from government health facility 58.1% (61/105) and 41.9% from Private Not For Profit Facilities (PNFP), with 40.57% (43/105) coming from the hospitals, 42.92% (42/105) from the Health center IIIs and 19.81% (21/105) from the Health center IVs. Most participants were not engaged in income generating activities (81.57%) and 56.6% lived more than 5km from health facilities. Most participants (80.77%) do not visit the traditional healers (Table 3).
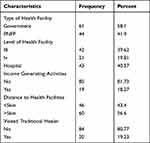 |
Table 3 The Accessibility of Respondents to Health Facilities (n=106) |
Manifestations/Domains of Disability of the Respondents
Based on WHODAS 2.0 scale of disability likert scales 1 and 2 were considered as not having difficulties and ≥3 were considered as having the difficulties. Of the 106 respondents, 68.57% were identified as having cognitive impairment (difficulty in understanding and communication ability), 92.38% had difficulty in mobility, 80% had difficulties with self-care-attending to one’s hygiene, dressing, eating and staying alone, 57.14% had difficulties getting along – interacting with other people, 27.71% had difficulties in Life activities – domestic responsibilities, leisure, work and school, and 44.74% reported difficulties in participation – joining in community activities, participating in society in the past 30 days (Table 4).
 |
Table 4 The Frequency of Various Manifestations of Disability Among Study Respondents. (N=106) |
Health System Responsiveness to People with Disability
Overall Health system responsiveness (HSR) was at 47.62% being acceptable. Across different domains, the best performance was reported in social consideration (68.57%) and autonomy (67.62%). The least performance was registered in dignity (2.83%), confidentiality (2.91%), prompt Attention (17.35%) and Choices (30.48%). Whereas performance in communications (53.92%) and quality of basic amenities (42.27%) were average (Figure 1).
 |
Figure 1 The health system performance among people with disabilities attending HIV/AIDS treatment and care services in Bushenyi. |
Factor Associated with HATCS Responsiveness to PWDs at Bushenyi Health Facilities
In bivariate logistic analysis; age, marital status and income generating activities were significantly associated with HS responsiveness. Age group 31–40 and 41–50 were less likely to be responsive to HSR compared to being less than 30 years. Being single was 3.4 times more likely to be responsive to HS. Those with income generating activities were 20% less likely to be responsive to HS.
In the final analysis, there were no socio-demographic or disability variables that were predictive of HATCS responsiveness (Table 5).
 |
Table 5 Bivariate and Multi-Variate Logistic Regression Analysis for Factors Associated with Responsiveness to HATCS in Bushenyi |
Experience of Persons with Disabilities Attending HIV/AIDs Treatment and Care Service in South Western Uganda
Provider’s Perspectives on Responsiveness
After key informant interviews with five (5) health workers in the HATCs facilities on the topic of “experiences of caring for persons with disabilities”, we identified two main themes: social support and communication skills.
Theme 1 -Social Support
Majority of the health workers interviewed reported a lack of social support for persons with disabilities when they came to their HATCS. There was nothing being offered by the government or any other organization to help PWDs move around the place, like using a wheelchair. Usually, relatives or well-wishers do provide some form of support. The majority of PWDs lacked transport to enable them to come to health facilities on appointment date, others did not have pocket money for refreshments or meals and yet they may spend a long day during clinic visits. These experiences were captured verbatim during the interviews as noted below:
There are people with disabilities who come and sit here, expecting us (health workers) to feed or provide drink for them. Sometimes the hospital digs into its pockets and buys meals or transportation for these people. HIV/AIDS peer counselor from Ishaka Hospital.
So far the ones we have here, not all are doing well and most of them are really struggling with life. At times you find a patient with disability telling you that she borrowed money for transport to come for the drugs…. There is one I interacted with last week, she was like she reached a point of ending her life- I see myself hopeless and useless in life. HIV/AIDs counselor at Bushenyi HCIV
Theme 2 – Communications Skills
All the health workers interviewed expressed their frustration with lack of communication skills in attending to patients who could not talk or hear. Majority of the HATCs facilities have no braille or sign language specialist to help communicate with clinicians. This challenge was captured verbatim as below:
There is a lot of barrier to communication, at times a patient may be explaining something, as a clinician I may not know or be sure if I am getting it right or wrong…. But we usually use their caregivers to help us since they stay with them daily and know what is disturbing them. Health care Provider from Health III.
What makes it difficult in this sense is that I, as a health worker, am not trained in that language speech, language communication like the way they usually communicate to them using that body language, so you find what I can do if someone has the ability to see and read -I communicate through writing…. A doctor from Ishaka Hospital
People with Disability Experiences
We interviewed nine (9) persons with disabilities on the topic “experiences of living with disabilities and HIV at HATCs”, we identified four major themes – social support, confidentiality and privacy, dignity, stigma and discrimination and poor communication.
Theme 1- Social Support
Most persons with disabilities reported lack of social support like transportation to the clinics and lack of pocket money for refreshment and meals during the clinic’s visits. The following quotes illustrate their experience verbatim:
When I don’t have money I can’t come, even when I don’t have money to take me back, usually I don’t leave home. That’s the challenge I have for now. 40 year old female client with difficulty in walking from Bushenyi HCIV.
… previously for us HIV patients, they used to give us somethings like cooking oil, but now in this place, they don’t offer such, I don’t know if they are offered in other places. 36- year female with congenital limp malformation at RHYEISHE Health III.
Theme 2 -Confidentiality and Privacy
Some of the PWDs felt their privacy and confidentiality were not being protected at the HATCs centers. This was epitomized by one client in the quote below;
What I value when I come to the facility is treating me in a timely manner, giving me a private area so that if I have a personal problem that requires me to undress so the doctor can see it, I cannot undress from the clinic where there is one bringing a book, another asking for a file, another filling a viral load form, with these you cannot undress to show the doctor that this is where the problem is, so you give yourself respect as a patient, a 31 year female peer educator at Rheishe Health CentreIII.
Theme 3 - Stigmatization and Discrimination
Majority feel health-care providers do not care about persons with disabilities. Although a few had a positive experience of being prioritized when attending to clients during clinic visits. During the interviews, some of the sentiments were captured below:
…may be the problem is that they don’t mind about us the lame, they just leave us there with other people and they quickly call other people who even can easily help themselves, okay like the lame don’t easily get treatment. 23-year male, client with difficulty in mobility from Bushenyi HCIV.
No. that has never happened to me because the health workers handle you the way you have come, they treat you and you go back home. But when there are many people, you hear some one complain that “they have delayed”, but even after the delay, they always give her what she wants. A 29 year male client with difficulty in mobility from Kweizooba HCIII
Theme 4- Inability to communicate effectively to the Healthcare Providers
Concerning communication difficulties, many clients complained of being ignored because they could not hear their names being called. The following quotes illustrate the challenges being faced by those with hearing impairment:
The handicap that I have, you find that the doctor who understands me is not available, and it hurts me because you find that the health worker I’m going to converse with, we’re not getting along, and when he asks me, you find that what he has asked, I have not quickly understood him well, and he writes the way he has seen because he has seen that I am going to tire him, one of the peer educators with hearing impairment for PWD says.
…some times when the health workers are having a conversation, I feel like they are talking about me, and that makes me feel very bad at such moments… 33 year old female who is deaf at Kyabugimbi HCIV.
Discussion
This study was aimed at evaluating health system responsiveness to people with disabilities in HIV/AIDS Treatment and care service facilities in South Western Uganda. Our findings suggest a substantially lower HSR (47.62%) than previous studies on HIV-positive persons visiting HATCS using a comparable WHO questionnaire, whose responses ranged from 55% to 89.6%.14,20,22 In Kenya, results of WHO responsiveness elements in the context of Voluntary counseling and testing (VCT) were much higher in 2009.13 Similarly, a nationally representative survey of both private and public health facilities in South Africa using a similar WHO questionnaire found that the overall HSR for general outpatients was higher, at 67%.5 Despite the fact that the WHO questionnaire has been validated in a variety of settings, including chronic diseases, prenatal care, and mental illness,23–25 no published study has been focused on people with disabilities. Our low health system performance findings could be partly explained by the effect of both HIV and disability vulnerabilities.1 This is in line with disability-based studies of HSR conducted in China, Ghana, India, Mexico, Russia, and South Africa, which, with the exception of Ghana, found considerable disparities among PWDs in the outpatient setting.26 However, cultural and contextual factors may have had a significant impact on how people perceive and anticipate the responsiveness of the health system, which may account for the observed disparities.14
Furthermore, the performance of some components of HSR in Bushenyi District was exceedingly poor in terms of dignity (2.83%), confidentiality (2.91%), and prompt attention (17.35%) to patients with disabilities when compared to similar studies in Ethiopia.14,20,22 Primary care users in South Africa and Brazil gave substantially higher ratings to promptness (58% and 65%) and autonomy (70%, 66%), respectively.5,27 Our results on autonomy (67%) and social consideration (68%) were comparable to a report in the Wolaita region of Ethiopia.14 Our quantitative study’s findings have been corroborated by qualitative data, which showed that during key informant interviews, both PWDs and health providers at HATCs identified social support and communication skills as two crucial components of the health system that are required to satisfy the expectations of PWDs in the region.
The study’s findings revealed that socio-demographic variables were not significantly associated with HSR. This could mean that clients from different socio-demographic groups scored the HATCs equally, or that any discrepancies were attributable to errors, a small sample size, chance, confounding, or happened at random. This was in line with previous studies in Ethiopia and Tanzania that showed no significant correlation between socio-demographic factors and responsiveness.14,28 However, in another health system comparing the insured and uninsured users of primary care service in Ethiopia, there was a statistically significant negative relationship between age and responsiveness.29 In addition, our results showed no significant association between the different domains of disabilities with HSR. This was in contrast to a previous multi-country study that showed older persons with disabilities or severe disabilities had considerably lower HSR scores than older adults with either no disabilities or mild disabilities.26
Our finding is important in the context of UNAIDS strategy 2021–2026 of ending inequalities among key populations including people with disabilities.30 The overall health system performance appears to be consistent with those of Mulumba et al who reported in 2014 that persons with disabilities in Uganda face a long history of societal neglect, including political marginalization, discrimination, and unequal access to health care.31 Furthermore, according to the 2016 Uganda demographic health survey (UDHS), disabled women were less likely than non-disabled women to obtain pre-test HIV counseling (59.6% vs 52.4%), an HIV test result (68.2%vs 61.4%), post-test HIV counselling (55.5% vs 51.6%), and all HIV testing and counseling services (49.2% vs 43.5%).7 Despite the fact that Uganda has passed anti-discrimination laws and other measures that specifically address HIV/AIDS discrimination against vulnerable populations, such as individuals with disabilities, more needs to be done to improve service providers’ attitudes and behavior.16 While policy makers and advocacy groups have recognized these disparities in accessing care for PWDs,32 there are still gaps in understanding the key drivers of this inequitable access to HATCS in different regions and health-care settings in Uganda.
Limitations and Strength
HSR is a more recent idea. The subsequent analysis of the results is therefore constrained by the dearth of comparable data. Since this was a cross-sectional study, temporality of the associations between the factors associated with HSR could not be established. We acknowledge that the relatively small sample size could have limited the level of significant predictable variables. Despite the fact that our research assistants were certified medical practitioners who had been trained in questionnaire interviewing, their lack of abilities in using braille or sign language may have hindered their capacity to gather data from those who could not hear or see at all. Nonetheless, by using a mixed-method approach, we were able to gain a better understanding of the difficult concept of health system responsiveness in the context of disability and HIV/AIDS care settings.
Conclusion and Recommendations
This study adds to our knowledge of how health systems respond to people with disabilities in HIV/AIDS care settings. In comparison to prior studies in the region, HSR was significantly lower in Bushenyi district and the region. The health care system was found to be least responsive to people with disabilities in the domains of dignity, confidentiality, prompt attention and choice. Given the limited use of the WHO response in the health system in low-resource settings, public health experts should expand the practical application of this instrument as a means of bridging inequitable access to various services by vulnerable groups. All stakeholders must be made aware of their need to meet the universal and legitimate requirements of people with disabilities at their health-care facilities.
Administrators of health-care facilities should work with stakeholders to provide proper training to service providers on how to treat people with disabilities with dignity, confidentiality, timely care, and freedom of choice of service providers. To improve fair access to care, the government and health facility management must pay attention to communication facilities and social support for PWDs.
Data Sharing Statement
The data that support the findings of this study are available from corresponding author Bernard Omech at [email protected] upon reasonable request but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available.
Ethics Approval and Consent to Participate
In line with the Declaration of Helsinki, we followed all the ethical guidelines and regulations needed to protect the participants from harm. Accordingly, ethical clearance was obtained from institutional review board (IRB) of Mbarara University of sciences and Technology (MUST-2021-294). Permission was obtained from the district health office of Bushenyi and the in-charges of health facilities selected in the district. Informed written consent and assent including publication of anonymized responses were obtained from the study participants prior to enrollment.
Acknowledgments
We are deeply indebted to our study participants for their time and voices during the study. We are very grateful to the project Administrator Dr Edith Wakida, and the Principal investigator Prof. Celestino Obua for their efforts in providing leadership for the entire Health-Professional Education Partnership Initiative – Transforming Ugandan Institutions Training Against HIV/AIDS (HEPI-TUITAH) project. Special regards to the research assistants Ms Sheila and Ronaldo. We wish to thank Biostatistician Mr Opio Bosco for his role in data processing and analysis.
Author Contributions
All authors contributed substantially to the work reported, whether in the conception, study design, execution, data acquisition, analysis, and interpretation, or in all of these areas; participated in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; agreed on the journal to which the article was submitted; and agree to be accountable for all aspects of the work.
Funding
Research reported in this publication was supported by the Fogarty International Center (US Department of State’s Office of the US Global AIDS Coordinator and Health Diplomacy (S/GAC) and the President’s Emergency Plan for AIDS Relief (PEPFAR)) of the National Institutes of Health under Award no. R25TW011210.
Disclosure
The authors declare that there are no conflicts of interest regarding the publication of this paper.
References
1. Unaids. The GAP report on people with disabilities; 2014:11.
2. Ubos, UBOS. Uganda National Household Survey 2016/17. Kampala, Uganda: UBOS; 2018.
3. Dean L. Shaping health systems to include people with disabilities. K4D Emerging Issues Report; 2018:1–35.
4. Mirzoev T, Kane S. What is health systems responsiveness? Review of existing knowledge and proposed conceptual framework. BMJ Global Health. 2017;2(4):e000486. doi:10.1136/bmjgh-2017-000486
5. Peltzer K. Patient experiences and health system responsiveness in South Africa. BMC Health Serv Res. 2009;9:1–12. doi:10.1186/1472-6963-9-117
6. Bajaria S, Exavery A, Toroka N, et al. Poor linkage to care for HIV-positive OVC with disabled caregivers: a longitudinal study in Tanzania. BMC Public Health. 2021:1–9. doi:10.1186/s12889-020-10013-y
7. Zandam H, Akobirshoev I, Nandakumar A, et al. Utilization of HIV testing and counselling services by women with disabilities during antenatal care in Uganda: analysis of 2016 demographic and health survey. BMC Public Health. 2021;21(1):1–7. doi:10.1186/s12889-021-12045-4
8. Ward E, Hanass-Hancock J, Amon JJ. Left behind: persons with disabilities in HIV prevalence research and national strategic plans in east and Southern Africa. Disabil Rehabil. 2022;44(1):114–123. doi:10.1080/09638288.2020.1762124
9. De Silva A. A Framework for Measuring Responsiveness. World Health Organisation; 2000:1–42.
10. Valentine NB, de Silva A, Kawabata K, et al. Health system responsiveness: concepts, domains and measurement. In: Health Systems Performance Assessment: Debates, Methods and Empiricism. Geneva: World Health Organization; 2003:96.
11. Darby C. Strategy on measuring responsiveness. GPE discussion paper series; 2013:1–23.
12. Üstün B. WHO multicountry household survey study on health and responsiveness 2000–2001. Global Programme on Evidence for Health Policy Discussion Papers; 2001.
13. Njeru MK, Blystad A, Nyamongo IK, et al. A critical assessment of the WHO responsiveness tool: lessons from voluntary HIV testing and counselling services in Kenya. BMC Health Serv Res. 2009;9(1):1–11. doi:10.1186/1472-6963-9-243
14. Yakob B, Ncama BP. Measuring health system responsiveness at facility level in Ethiopia: performance, correlates and implications. BMC Health Serv Res. 2017;17(1):1–12. doi:10.1186/s12913-017-2224-1
15. Baharvand P. Responsiveness of the health system towards patients admitted to west of Iran hospitals. Electron J Gen Med. 2019;16(2):em121. doi:10.29333/ejgm/93481
16. Uganda. Person with Disabilities Act, 2020, P.O. Uganda, Editor. Uganda Gazette no. 10 on 14 February 2020 Kampala; 2020.
17. Ubos. National population and housing census 2014: main report. Kampala; 2016:84.
18. Camargo LMA, Silva RPM, de Oliveira Meneguetti DU. Research methodology topics: cohort studies or prospective and retrospective cohort studies. J Hum Growth Dev. 2019;29(3):433–436. doi:10.7322/jhgd.v29.9543
19. Üstün TB. Measuring Health and Disability Manual for WHO Disability Assessment Schedule. World Health Organization; 2010.
20. Asefa G, Atnafu A, Dellie E, et al. Health System Responsiveness for HIV / AIDS Treatment and Care Services in Shewarobit. Dovepress; 2021:581–588.
21. Da Silva RB, Contandriopoulos A-P, Pineault R, et al. A global approach to evaluation of health services utilization: concepts and measures. Healthcare Policy. 2011;6(4):e106–e117. doi:10.12927/hcpol.2011.22351
22. Negash WD, Tsehay CT, Yazachew L, et al. Health system responsiveness and associated factors among outpatients in primary health care facilities in Ethiopia. BMC Health Serv Res. 2022:1–11. doi:10.1186/s12913-021-07414-z
23. Röttger J, Blümel M, Fuchs S, et al. Assessing the responsiveness of chronic disease care - is the World Health Organization’s concept of health system responsiveness applicable? Soc Sci Med. 2014;113:87–94. doi:10.1016/j.socscimed.2014.05.009
24. van der Kooy J, Valentine NB, Birnie E, et al. Validity of a questionnaire measuring the world health organization concept of health system responsiveness with respect to perinatal services in the Dutch obstetric care system. BMC Health Serv Res. 2014;14(1):622. doi:10.1186/s12913-014-0622-1
25. Forouzan AS, Rafiey H, Padyab M, et al. Reliability and validity of a mental health system responsiveness questionnaire in Iran. Glob Health Action. 2014;7(1):24748. doi:10.3402/gha.v7.24748
26. Rahman MHU, Singh A, Madhavan H. Disability-based disparity in outpatient health system responsiveness among the older adults in low- to upper-middle-income countries. Health Policy Plan. 2019;34(2):141–150. doi:10.1093/heapol/czz013
27. Melo DDS, Martins RD, Jesus RP, et al. Assessment of the responsiveness of a public health service from the perspective of older adults. Rev Saude Publica. 2017:51. doi:10.1590/S1518-8787.2017051006614
28. Kapologwe NA, Kibusi SM, Borghi J, et al. Assessing health system responsiveness in primary health care facilities in Tanzania. BMC Health Serv Res. 2020;20(1):104. doi:10.1186/s12913-020-4961-9
29. Negash WD, Atnafu A, Asmamaw DB, et al. Does health system responsiveness differ between insured and uninsured outpatients in primary health care facilities in Asagirt District, Ethiopia? A Cross-Sectional Study. Adv Public Health. 2022;2022:3857873. doi:10.1155/2022/3857873
30. Unaids. Global update on aids; 2021.
31. Mulumba M, Nantaba J, Brolan CE, et al. Perceptions and experiences of access to public healthcare by people with disabilities and older people in Uganda. Int J Equity Health. 2014;13(1):1–9. doi:10.1186/s12939-014-0076-4
32. Hanass-Hancock J. Disability and HIV/AIDS - A systematic review of literature on Africa. J Int AIDS Soc. 2009;12(1):1–11. doi:10.1186/1758-2652-12-34
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
