Back to Journals » Clinical Ophthalmology » Volume 17
Functional Profile of a Customized Wound Parameter in Femtosecond Laser-Assisted Corneal Incision for Cataract Surgery
Authors Neves NT , Boianovsky C , Lake JC
Received 16 August 2022
Accepted for publication 9 December 2022
Published 11 January 2023 Volume 2023:17 Pages 175—181
DOI https://doi.org/10.2147/OPTH.S384660
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Nathália Teles das Neves,1 Celso Boianovsky,2 Jonathan Clive Lake2,3
1Federal District Eye Hospital – HODF, Brasilla, Brazil; 2Department of Ophthalmology, Hospital of Vision – OFTALMED, Brasilia, DF, Brazil; 3Department of Ophthalmology, Hospital Oftalmológico de Brasília – HOB, Brasilia, DF, Brazil
Correspondence: Nathália Teles das Neves, Federal District Eye Hospital – HODF, Brasilia, Brazil, Tel +5561992738688, Email [email protected]
Purpose: To evaluate the performance of optimized parameters of femtosecond laser for cataract surgery corneal incisions regarding opening, patency and surgically induced astigmatism (SIA).
Patients and Methods: Patients scheduled for femtosecond laser-assisted cataract surgery between May 2018 and December 2018 were enrolled. Inclusion criteria were a healthy preoperative cornea and uneventful FLACS. Exclusion criteria were preoperative corneal astigmatism over 1.0 D, previous corneal trauma or pathologies. Clinical data were obtained from the electronic medical records. Surgical planning was based on Scheimpflug tomography images for keratometric data. At postoperative day 60, new keratometric evaluation was performed, obtained using the same device.
Results: 101 eyes (61 patients) matched the criteria for SIA analysis. Overall mean SIA was 0.44 ± 0.33 D (0– 1.55 D). Axis and size did not have any statistically significant effects on SIA. The overall centroid of the SIA was 0.11. For the opening analysis, was included 156 eyes (79 patients). Successful opening in 87.7% of cases (137 eyes). Temporal incisions had the highest success rate (98.36%).
Conclusion: These femtosecond laser parameters showed high opening rates with low opening times. These optimized parameters led to a low incidence of SIA and high predictability regardless of incision site and size. The association between incision opening and SIA was not statistically significant. There was, however, an association between incision opening success and site.
Keywords: femtosecond laser, cataract surgery, clear corneal incisions, corneal induced astigmatism
Introduction
The development of premium intraocular lenses (IOLs) capable of neutralizing refractive errors has led to improvements in cataract surgery. Improved results of the procedure have led to greater patient expectations for spectacle independence.1 Preoperative measurements have become more precise with the advent of newer technologies. However, postoperative refractive outcomes are directly influenced by various factors and intraoperative results depend on effective lens positioning and incision characteristics, such as width, length, and position.
Self-sealing clear corneal incisions (CCIs) are preferred because they protect the conjunctiva, lead to faster healing, have a low incidence of postoperative astigmatism, and obviate the need for suturing.2 Although CCIs are associated with a risk for endophthalmitis,3 this risk can be reduced using multiplanar instead of uniplanar CCIs to prevent postoperative leakage and hypotony.2 The precise length, architecture, and geometry of a multiplanar incision is difficult to achieve manually using a keratome blade.1–3 The advent of femtosecond laser technology has increased the potential of incisions, capsulorhexis, and nucleus fractures in cataract surgery. It allows computer-guided, standardized, and systematic creation of different incisions, and makes the process more reproducible.
However, a limitation of this method is that it only works in transparent tissues. Incisions close to the limbus, which are generally safer and more effective, using this technology either do not open or take too long to open. Incisions placed anteriorly in the transparent cornea, while easy to open, increase surgical manipulation and the risks related to sealing and astigmatism.4 However, these incisions can be made with limitless planes and sizes. Therefore, it is possible to create a type of incision that leads to effective opening and low astigmatism, and is still placed at the best possible site.
CCIs induce corneal astigmatism. However, the comparison of surgically induced astigmatism (SIA) caused by femtosecond laser and manual incisions has yielded conflicting results.4 Some optimized parameters are more effective, including opening, patency, and SIA.2,4 The present study investigated the optimal parameters and their effectiveness in restoring these requirements.
Materials and Methods
This was a retrospective, consecutive case series at a private ophthalmological referral service in Brasilia, Brazil. Prior approval was obtained from the local ethics committee and the institutional review board (Hospital Oftalmológico de Brasília – HOB) and informed consent was not obtained, as it is data from a review of medical records, and so the institutional review board of the referred hospital approved that consent was not required. Patients scheduled for femtosecond laser-assisted cataract surgery (FLACS) between May 2018 and December 2018 were enrolled. The Lensx (Alcon Surgical Inc., Fort Worth, TX, USA) platform was used for all cases. The study was performed in accordance with the Declaration of Helsinki.
The incisions were performed by a single experienced femtosecond laser surgeon (NN), and the phacoemulsifications were performed by two surgeons (JL and CB) experienced in both phacoemulsification and femtosecond laser-surgery techniques. All procedures were performed under topical anesthesia. Capsulotomy and phacofragmentation were performed using the femtosecond laser and an intraocular lens (IOL) was placed in the capsular bag in all cases. The corneal incisions were left unsutured but were hydrated afterwards to close the incisions. All patients received the same postoperative treatment, including antibiotics, steroids, and nonsteroidal anti-inflammatory agents.
Inclusion criteria were a healthy preoperative cornea and uneventful FLACS. Exclusion criteria were preoperative corneal astigmatism over 1.0 D, previous corneal surgery or trauma, and corneal pathologies. As we focused on corneal keratometric changes and did not evaluate visual outcomes, patients with retinal pathologies, glaucoma, or other ocular comorbidities were not excluded. Clinical data were obtained from the electronic medical records.
All patients received a standard preoperative evaluation (visual acuity, biomicroscopy, Goldmann’s applanation tonometry, and fundoscopy). Surgical planning was based on preoperative measurements obtained using optical biometry (Lenstar; Alcon Surgical Inc.) for IOL power and Scheimpflug tomography (Pentacam HR; OCULUS Optikgeräte GmbH, Wetzlar, Germany) for keratometric data. At postoperative day 60, a fresh keratometric evaluation was performed, including tomographic images obtained using the same device.
Primary incisions were made toward the limbus, just anterior to the conjunctival arcades, in three planes using the energy setting of 4.80 µJ, and spot and line separation of 3 µJ, guided by the real-time imaging system. Plane 3 started at a 130% depth with a side cut angle (SCA) of 70°, plane 2 started at a posterior plane depth (PPD) of 85% with a 15° SCA and a length of 1600 µm, and plane 1 started at an anterior plane depth (APD) of 60% with a 70° SCA. Secondary (side) ports were placed diametrically opposed to the primary incisions. All incisions were made using these parameters and measured 2.4 mm or 2.8 mm.
Patients were classified into four groups based on the position of the primary incision: temporal (group 1), superior (group 2), oblique (group 3), and nasal (group 4) groups. Temporal incisions were placed between 150° and 210° on the right eye and between 330° and 30° on the left eye; superior incisions were placed between 60° and 120° in both eyes; oblique incisions were placed between 120° and 150° on the right eye and between 30° and 60° on the left eye; and nasal incisions were placed between 30° and 120° on the right eye and between 120° and 150° on the left eye.
Incision opening and patency were evaluated using timecodes of the video footage of the surgeries. Incision opening rates were distributed on the basis of incision size and meridian. SIA and centroids were calculated on the basis of the vector analysis of the pre- and postoperative (Day 60) keratometric data. SIA distribution was based on the incision size and meridian.
Logistic regression was used to evaluate the effects of axis and size on incision opening (dichotomous measure “yes” or “no”). As two different surgeons performed the surgeries, this measure was added as a control variable, together with eye laterality. Moreover, Pearson correlation coefficient was used to evaluate the possible linear association between axis and the time-to-opening. Finally, Fisher’s exact test was used to evaluate the association between site and opening success. The statistical significance level was set at 0.05. All of the analyses were performed using SPSS Statistics version 24 (IBM Corp., Armonk, NY, USA).
Linear regression was used to evaluate the effects of incision opening on SIA. We hypothesized that the association between SIA and incision opening would depend on the axis values (and their sites). An interaction model (also known as conditional model) was used to investigate the effects of axis on the association between SIA and incision opening. Both unconditional (ie, potential effects of incision opening on SIA) and conditional (ie, the interaction model) models were adjusted for the surgeons and laterality. In addition, the axis was considered a categorical variable called site (ie, nasal, temporal, superior, and oblique) in the conditional model. Lastly, we performed the Freeman-Halton extension of the Fisher exact probability test for a two-rows (ie, success or not) by four-column contingency table (ie, sites). The significance level was set at 0.05.
Results
We reviewed the clinical data of 101 eyes (61 patients) that matched the criteria for SIA analysis with recorded keratometric measurements. The mean age was 66.49 ± 8.11 years (range: 43–84 years). Overall, 34 patients were male (33.67%) and 67 were female (66.34%). Overall mean SIA was 0.44 ± 0.33 D (0–1.55 D) (Figure 1). SIA skewness was 1.33 (standard error [SE] = 0.24) and the kurtosis was 2.29 (SE = 0.48). The coefficient of variation was 6.81%. Axis and size did not have any statistically significant effects on SIA. The overall centroid of the SIA was 0.11 (p = 0.977 and 0.961, respectively). Overall centroids of SIA for 2.4 mm and 2.8 mm incisions were 0.12 and 0.1, respectively. Incisions were made in three planes using previously described parameters.
 |
Figure 1 Overall mean surgically induced astigmatism (SIA). |
For the opening analysis, we included 156 eyes (79 patients) with a mean age of 65 ± 9.65 years (range: 35–85 years). There were 57 male (36.94%) and 99 female (63.46%) patients. In all, 137 eyes had successful opening (87.7%). Among these, the time-to-opening obtained from the video footage timecode ranged from 2 to 40s. The mean time was 7.50 ± 6.83 s. Kurtosis and skewness were 10.16 (SE = 0.44) and 3.03 (SE = 0.224), respectively. Success rates significantly differed among sites (p = 0.012). Temporal incisions had the highest success rate (98.36%), followed by nasal incisions (90%), oblique incisions (81.5%), and superior incisions (75%).
Regarding size, 93.48% (43/46) of the 2.4 mm incisions and 85.45% (94/110) of the 2.8 mm incisions opened successfully (Table 1). Estimates of the logistic regression (odds ratio [OR]) showed that surgeon factors and laterality were not predictors of incision opening (p = 0.532 and 0.679, respectively; Table 2).
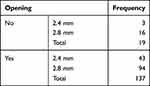 |
Table 1 Opening Success of Different Incision Sizes |
 |
Table 2 Estimates of Logistic Regression Adjusted for Surgeon and Laterality |
Table 3 shows the association between incision opening and site, which was statistically significant using the Fisher exact test (p < 0.001). This suggests an association between site and the opening outcome.
 |
Table 3 Association Between Site and Opening Success Using the Fisher Exact Test |
Table 4 shows the association between incision opening and site, found to be statistically significant using the Freeman-Halton extension of the Fisher exact test (p = 0.012). This also suggests an association between site and the opening outcome. The chi-square test was performed only if at least 80% of the cells had an expected frequency of 5 or greater, and no cell had an expected frequency lower than 1. The results of the chi-square test are, therefore, not reported.
 |
Table 4 Association Between Site and Opening Success Using the Freeman-Halton Test |
Discussion
Incisions for cataract surgery have been constantly evolving. The approach to incisions for phacoemulsification has changed from mounted razor blades to laser-sculpted microsurgical blades. The decrease in size and the shift from the sclera to the cornea has raised concerns regarding patency and sealing. This has led to the development of new materials and designs for incisions in manual surgery. The development of newer premium IOLs has also led to concerns about the impact of cataract incisions on optical quality of the eye.
CCIs made using femtosecond laser devices are comparable to those made using keratomes.1–5 Some studies have even suggested that the former are better than manual incisions.6 Well-made and well-placed incisions should allow for effective and comfortable phacoemulsification, should be self-sealing, and should induce minimal astigmatism.
Various authors have investigated the geometric characteristics and functionality of these incisions, including the architecture, biomechanical properties, endothelial misalignment, endothelial detachment rates, epithelial misalignment, and wound leaks.3,5,7–11 Although there appears to be no advantage in terms of corneal astigmatism and higher-order aberrations,10 CCIs in FLACS, particularly the multiplanar configuration, are better designed and more reproducible than manual techniques.4,12 In the present study, we found that CCIs preserved the anatomy of triplanar incisions, exactly as planned intraoperatively, even 3 months after the procedure (Figure 2).
This design is not manually reproducible. Even meticulously crafted manual incisions do not offer the same precision in terms of size and design. Although three-plane manual incisions may achieve a certain standard, variation in size, length, and design is common.
Femtosecond laser parameters do not rely solely on energy, spot separation, or line separation. The plane configuration of the femtosecond laser device involves size, inner diameter, and most importantly, depth. Although it is possible to configure biplanar or single-plane incisions, a three-plane incision allows for best stability and predictability of results, both during and after phacoemulsification. While there may be certain overriding parameters, a well-designed third plane allows for better self-sealing. It also allows for the use of corneal tissue for support, thus avoiding common problems, such as poor self-sealing and fish-mouth internal incisions. The second plane provides a path toward the anterior chamber. These incisions should not be too long, which would affect surgical manipulation, or too short, which would affect the sealing. In this study, we opted for a 4.5 mm long incision. In our opinion, the first plane is the most important. The use of femtosecond leads to what may be described as a “Velcro-zipper effect.” This requires the use of blunt instruments to open the incisions. The insertion of a blunt instrument, such as a spatula or a Sinskey hook, into the first deep plane creates enough space to allow opening of the tissues. The depth of our first plane was 60%.
The challenge is to place the incision as close as possible to the limbus. The problem with a standard 90-degree first plane is that if the perilimbal area is not optimally transparent, the entire first plane is created within a semi-opaque area, which does not allow for effective incision opening. We overcame this problem using a 70° inclination. This allowed for the laser to be applied within transparent tissue. Only a small portion was affected by tissue opacity, thus making the incision opening easier and more effective.
Previous studies have reported the optical parameters of femtosecond lasers for successful CCIs. Donnenfeld et al and Benard-Seguin et al suggested that a reverse SCA, with the incision directed toward the limbus from the center of the cornea, and then back toward the center of the eye, leads to better wound sealability.2,12 However, we adopted a 70° forward cutting angle with 60% APD in all cases, and there were no cases of hypotony, endophthalmitis, or leakage. Furthermore, reverse side-cut incisions are more prone to deformities and stretching during phacoemulsification and IOL implantation.
Femtosecond laser incisions with the parameters of the present study showed high opening rates with low opening times. After establishing the parameters, we retrospectively reviewed video footage of 150 cases to determine opening, time-to-opening, and induced astigmatism on the basis of placement. Temporal incisions offered the highest opening rate of 98%, while superior incisions had the lowest opening rate.
The mean time-to-opening for temporal incisions was 5 seconds. To the best of our knowledge, this was the first study to use time for incision opening as a surgical indicator. Incision opening time may be a useful indicator for the quality of surgery in both manual and femtosecond laser corneal incisions.
Conclusion
These optimized parameters led to a low incidence of SIA and high predictability regardless of incision site and size. The association between incision opening and SIA was not statistically significant. Moreover, this hypothesized association was not conditioned to the axis levels. There was, however, an association between incision opening success and site.
Disclosure
All authors have received research funding from Alcon Labs, Irvine, CA. Jonathan Clive Lake and Celso Boianovsky are consultants for Alcon Labs, Glaukos, and Johnson and Johnson. The authors report no other conflicts of interest in this work.
References
1. Diakonis VF, Yesilirmak N, Cabot F, et al. Comparison of surgically induced astigmatism between femtosecond laser and manual clear corneal incisions for cataract surgery. J Cataract Refract Surg. 2015;41(10):2075–2080. doi:10.1016/j.jcrs.2015.11.004
2. Donnenfeld E, Rosenberg E, Boozan H, Davis Z, Nattis A. Randomized prospective evaluation of the wound integrity of primary clear corneal incisions made with a femtosecond laser versus a manual keratome. J Cataract Refract Surg. 2018;44:329–335. doi:10.1016/j.jcrs.2017.12.026
3. Grewal DS, Basti S. Comparison of morphologic features of clear corneal incisions created with a femtosecond laser or a keratome. J Cataract Refract Surg. 2014;40(4):521–530. doi:10.1016/j.jcrs.2013.11.028
4. Zhu S, Qu N, Wang W, et al. Morphologic features and surgically induced astigmatism of femtosecond laser versus manual clear corneal incisions. J Cataract Refract Surg. 2017;43:1430–1435. doi:10.1016/j.jcrs.2017.08.011
5. Mastropasqua L, Toto L, Mastropasqua A, et al. Femtosecond laser versus manual clear corneal incisions in cataract surgery. J Refract Surg. 2014;30:27–33. doi:10.3928/1081597X-20131217-03
6. Chandra B, Chan T, Meades K. Factors affecting corneal incision position during femtosecond laser–assisted cataract surgery. J Cataract Refract Surg. 2017;43(12):1541–1548. doi:10.1016/j.jcrs.2017.09.024
7. Valbon BF, Ambrósio R, Gualdi L, Luz A, Alves MR. Changes of corneal biomechanical after femtosecond laser-assisted for cataract surgery. Rev Bras Oftalmol. 2015;74:297–302. doi:10.5935/0034-7280.20150061
8. Alió JL, Abdou AA, Soria F, et al. Femtosecond laser cataract incision morphology and corneal higher-order aberration analysis. J Refract Surg. 2013;29(9):590–595. doi:10.3928/1081597X-20130819-01
9. Hill JE, Binder PS, Huang LC. Leak-free clear corneal incisions in human cadaver tissue: femtosecond laser-created multiplanar incisions. Eye Contact Lens. 2017;43(4):257–261. doi:10.1097/ICL.0000000000000262
10. Masket S, Sarayba M, Ignacio T, Fram N. Femtosecond laser-assisted cataract incisions: architectural stability and reproducibility. J Cataract Refract Surg. 2010;36(6):1048–1049. doi:10.1016/j.jcrs.2010.03.027
11. Serrao S, Giannini DM, Schiano-Lomoriello D, Lombardo G, Lombardo M. New technique for femtosecond laser creation of clear corneal incisions for cataract surgery. J Cataract Refract Surg. 2017;43(1):80–86. doi:10.1016/j.jcrs.2016.08.038
12. Benard-Seguin É, Bostan C, Fadous R, et al. Optimization of femtosecond laser-constructed clear corneal wound sealability for cataract surgery. J Cataract Refract Surg. 2020;46(12):1611–1617. doi:10.1097/j.jcrs.0000000000000336
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

