Back to Journals » Patient Related Outcome Measures » Volume 15
Family Satisfaction with Care Provided in Intensive Care Unit; a Multi-Center, Cross-Sectional Study
Authors Liyew TM, Mersha AT , Admassie BM , Arefayne NR
Received 25 January 2024
Accepted for publication 11 April 2024
Published 22 April 2024 Volume 2024:15 Pages 105—119
DOI https://doi.org/10.2147/PROM.S453246
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Robert Howland
Temesgen Misganaw Liyew, Abraham Tarekegn Mersha, Belete Muluadam Admassie, Nurhusen Riskey Arefayne
Department of Anesthesia, College of Medicine and Health Sciences, University of Gondar, North Gondar, Ethiopia
Correspondence: Belete Muluadam Admassie, Email [email protected]
Background: Healthcare provided in medical facilities should prioritize the needs of families, as it enhances the quality of care for the patients. Family satisfaction gauges how effectively healthcare professionals address the perceived needs and expectations of family members. Numerous factors, including information dissemination, communication, family dynamics, patient characteristics, hospital facilities, and the caregiving process, serve as predictors of family satisfaction. Thus, this study seeks to evaluate the satisfaction of families with the care received by patients admitted to the intensive care unit.
Methods: A hospital-based cross-sectional study involving 400 participants was conducted across multiple centers from March to June 2023. Multicollinearity was assessed by examining variance inflation factors (VIF), while the goodness-of-fit was evaluated using the Hosmer and Lemeshow test. Both bivariable and multivariable logistic regression analyses were utilized to identify factors correlated with family satisfaction. Variables with a p-value below 0.2 in the bivariable logistic regression were included in the multivariable logistic regression analysis. Adjusted Odds Ratios (AORs) with 95% Confidence Intervals were computed to indicate the strength of association. In the multivariable analysis, variables with a p-value less than 0.05 were deemed statistically significant.
Results: The overall family satisfaction with the care provided in the intensive care unit was 58.6%, with a 95% confidence interval ranging from 55.882% to 61.241%. Families expressed higher satisfaction levels with patient care (64.8%) and professional care (67.4%). However, they reported lower satisfaction levels regarding care provided for families (52.2%), the ICU environment (56.8%), and involvement of families in decision-making (55.8%). Lack of formal education (AOR: 1.949, 95% CI: 1.005, 4.169), completion of primary education (AOR: 2.581, 95% CI: 1.327, 5.021), and completion of grades 9– 12 (AOR: 2.644, 95% CI: 1.411, 4.952) were found to be significantly associated with overall family satisfaction.
Conclusion and recommendation: The overall level of satisfaction is satisfactory. To enhance service quality and family satisfaction, healthcare providers should prioritize effective and regular communication with family members. Keeping them well informed about the patient’s condition and treatment plan is essential.
Keywords: critical care, family satisfaction, intensive care unit, quality care, satisfaction
Introduction
Intensive care units (ICUs) are advanced medical facilities where critically ill patients receive treatment and nursing care.1 Due to their condition, many patients in the ICU are unable to make consistent or reliable decisions for themselves, and often depend on their family members for support and guidance.2
In tertiary referral ICUs in the USA, mortality rates typically range from 15% to 20%.3 Among those who survive, many require ongoing medical attention, while others may not fully recover. In Ethiopia, mortality rates vary across different regions: Addis Ababa (39%), Gondar (38.7%), Jimma (37.7%), and Mekelle (27%).4
Many families find the time spent in the intensive care unit (ICU) to be difficult, filled with uncertainty about the patient’s condition, treatment plan, and prognosis.1
Patients in the intensive care unit, along with their families, express diverse needs, including the desire for information, effective communication, reassurance, proximity to their loved ones, comfort, and support.5 Critically ill patients often cannot engage in complex medical decision-making or effectively communicate their values, goals, and preferences to healthcare staff. Therefore, the treatment of admitted patients frequently involves direct collaboration with the patient’s family.6
Assessing the quality of intensive care units (ICUs) should encompass evaluating the satisfaction of the patient’s family regarding the care provided, the information communicated, and the decision-making process.7 Families in the intensive care unit (ICU) have been recognized as a distinct group with specific needs, irrespective of the medical outcome of the patient.8 Family members of patients in intensive care are more prone to experiencing feelings of anxiety, depression, fatigue, hopelessness, and fear.9,10 Families often undergo stress when visiting a patient in an intensive care unit (ICU).11 Responses regarding patient rooms, waiting areas, communication with doctors, and emotional support were reported with lower levels of satisfaction.12 Family satisfaction was significantly influenced by inadequate management of patients’ pain.13
Nursing care in ICUs should be prioritized, as it enhances family satisfaction when nursing interventions are tailored to the specific needs of ICU-admitted patients and their families.14 Understanding how to support families in managing mental stress is one of the most critical components of comprehensive care. Patients admitted to intensive care units may experience higher levels of satisfaction if their families’ needs are effectively addressed.15 Patients in the ICU confront life-threatening illnesses and undergo complex treatments involving various technologies and equipment. These circumstances may potentially lead to dissatisfaction among the families of the patients.16
Low family satisfaction with the critical care stay happens with the family experiences that develop during the ICU stay.17 Family members experience stress and low satisfaction due to poor communication.18 Areas such as emotional support for family members, consistency, comprehensiveness, and clarity of information provided, coordination of care, and assessment and treatment of agitation are all identified as having low levels of satisfaction.19 Unmet needs of family members impact negatively on family satisfaction with care, information, and decision-making.20
Evaluations of family needs provide useful knowledge for improving families’ comprehension, satisfaction, and ability to make decisions.21 It may be possible to increase the satisfaction of families of patients in critical care with their involvement in decision-making and their perspective by using an evidence-based structured communication algorithm.22
A study done in the USA, Neuro ICU and MICU families’ satisfaction with the waiting area’s atmosphere was notably poor (47.3%), emphasizing a need for improvement. Less than 60% of the family participants in the study from the Neuro ICU reported being completely satisfied with the frequency of communication by Neuro ICU doctors (46.6%), inclusion in decision making (52.6%), support during decision-making (44%), and control as a patient’s family over the care of their loved one (54%).23
Staff may be able to communicate more effectively and increase satisfaction with concerned family members if they have a better understanding of how severe stress affects family members.12 Family satisfaction plays a critical role in the overall care provided to critically ill patients. Enhancing the relationship between healthcare providers and patients’ family members can have a profoundly positive impact on satisfaction levels.24
Family members’ satisfaction with nursing care, respect, courtesy, and compassion for the patient and the family was high. However, waiting room environment, doctor communication, and decision-making support received the least satisfaction.25,26 According to a Saudi Arabia study, information, proximity and comfort affect family satisfaction.27 Additionally, a study done in the United Kingdom revealed that family member age, ethnicity, relationship to patient, frequency of visits, patient acute severity of illness, and receipt of invasive mechanical ventilation were all associated with overall family satisfaction for ICU.28,29
A study done in Italy on 122 clinicians stated that clinicians’ moral distress is inversely related with family satisfaction regarding breathlessness and agitation management, provision of emotional support, understanding of information, and inclusion in the decision-making process.30
To aid in the improvement of healthcare services, it is advisable to assess the experiences of both patients and their families, as well as their levels of satisfaction following care received in the ICU.31
Significance of the Study
Satisfaction serves as a key quality indicator, aiding in the identification of areas requiring improvement. Family satisfaction with ICU care serves as an outcome measure, reflecting the quality of care provided to both patients and their families. A high level of family satisfaction can contribute to better adherence to treatment plans, enhance communication between healthcare providers and families, and alleviate stress and anxiety for both patients and families.
Family satisfaction with the care provided to the patient during their ICU stay is a crucial component for overall ICU quality enhancement. It helps ensure that the care delivered aligns with the needs of both the patient and their family members. Furthermore, analyzing family satisfaction allows for an investigation into how various demographic variables influence their satisfaction ratings. This information can be invaluable in refining and tailoring ICU services to better meet the needs of patients and their families.
The findings of this study can serve as foundational data for program developers seeking to improve the quality of ICU services. Additionally, the research results may stimulate further exploration into predictors of satisfaction and other crucial quality assessments within the ICU environment. Ultimately, these efforts could contribute significantly to ongoing initiatives aimed at enhancing the overall experiences of patients and families in intensive care units.
Understanding family satisfaction in the ICU provides crucial insights into the experiences and requirements of families during their time there. This information is essential for hospitals and healthcare providers, enabling them to identify areas requiring improvement and to implement necessary changes to enhance overall satisfaction for families in the ICU.
Methodology
Study Design and Study Period
A cross-sectional study, conducted from March to June 2023, was carried out in multiple hospitals within the Amhara region, specifically, the Comprehensive Specialized Hospitals located in North West Ethiopia.
Study Area
Amhara is one of Ethiopia’s 10 regional states, spanning an area of 154,909 square kilometers in the northern part of the country. Bahir Dar serves as the capital city of the Amhara regional state, situated approximately 570 kilometers from Addis Ababa. According to the 2007 Housing Census of Ethiopia, the total population of Amhara is estimated at 20.02 million.
The Amhara Regional State boasts a total of seven Comprehensive Specialized Hospitals, and this study was conducted in four of them: Tibebe Ghion Comprehensive Specialized Hospital (TGCSH), University of Gondar Comprehensive Specialized Hospital (UOGCSH), Debre Markos Comprehensive Specialized Referral Hospital (DMCSRH), and Felege Hiwot Comprehensive Specialized Hospital (FHCSH). These hospitals were chosen randomly, taking into account financial considerations and the ability to obtain an adequate sample size.
UOGCSH offers both adult and pediatric ICU services, with 15 beds allocated for adult ICU and 6 beds for pediatric ICU. TGCSH provides similar services with nine beds for adult ICU, six mechanical ventilators, and 2 beds for pediatric ICU. FHCSH also offers adult and pediatric ICU services, featuring 12 beds and 6 mechanical ventilators. DMCSH provides adult and pediatric ICU services with 4 beds available.
Source Population
All close family members of the ICU admitted patients with ages greater than 18 years within the selected hospitals during the study period.
Study Population
One close family of patients who was admitted to SICU, MICU, PICU, age >18-year-old and stayed in the ICU for more than 24 hours in the study hospitals at the study period.
Inclusion Criteria
The study included patients’ close family members who stayed with the patient for more than 24 hours and had responsibilities in caring for the patient. These family members were required to be 18 years of age or older and present at the time of data collection.
Exclusion Criteria
Families not willing to participate in the study
Sample Size Determination
Actual sample size for the study was computed using single population proportion formula. From the previous study done in Addis Ababa, the sample size was determined by taking 62% prevalence of family satisfaction in care of critically ill patients.32 By giving any particular outcome to be within 5% marginal error and 95% confidence interval of certainty (alpha = 0.05). Based on this assumption the sample size is calculated below.
Where n = required sample size
Zα/2 = Z value at 95% CI [1.96]
p = Estimated prevalence rate in 62% [0.5]
d = Margin of error tolerated is 5% [0.05]
and non-response rate 10% is added and it is 398.2≈400
Sampling Technique and Procedures
In each hospital, a total of 572 patients were admitted in three-month period from November 2022 to January 2023 in each intensive care unit. Among these 188 cases were in UOGCSH, 143 cases were in TGCSH, 156 cases were admitted in FHCSH, and 85 cases were admitted to DMCSH intensive care unit. Estimated sample size in each hospital was calculated by using proportion allocation formula ni = n/N*Ni, n = total sample size to be selected, N = total population, Ni = total population of each hospital, ni = sample size from each hospital (Figure 1).
A total of 400 study participants were included. Data were collected with consecutive sampling technique by allocating participants to each hospital. Each participant was selected by following the admission date of patients from patient chart and participants for meeting criteria.
Variable of the Study
Dependent Variable
Family Satisfaction.
Independent Variables
Socio demographics: Age, Sex, Educational status, Income, Relationship with the patient, Occupational status, and Live with the patient.
Family and patient-related factor: Length of stay, patient’s health condition, number of visits, families’ ICU experience, Patient on mechanical ventilator.
Admission unit: Pediatric intensive care unit, Medical intensive care unit and Surgical ICU
Operational definition
Satisfied: Refers to participants who respond greater or equal to mean level of satisfaction.32–34
Not satisfied: Refers to participants who respond with less than mean level of satisfaction.32–34
Close family: Spouse, parent, child, siblings, or other relatives, such as cousin, aunt, grandparent.35
Family lives with the patient: Family member who lives closest to the patient or the same household as the patient admitted to the ICU.36
Competence: Having the knowledge, skill, and experience necessary to fulfil the requirements of the position of a medical professional.37
Data Collection Procedure
English and Amharic versions of the questionnaire were used in data collection. The Family Satisfaction in the ICU survey (FS-ICU) questionnaire was adopted from the Departments of Medicine and Nursing, Kingston General Hospital for assessing family satisfaction with care in the ICU.16 The data collectors were trained anesthetists and nurses from each site. Supervisors were also trained and assigned to each hospital to follow data collectors. The questionnaire assesses the socio-demographic character of families, ICU-related factors, and the level of family satisfaction. The questioner uses Likert scale from 1 to 5.1 - not at all satisfied, 2 - barely satisfied, 3 - quite satisfied, 4 - very satisfied, and 5 - completely satisfied and the higher score is 100% and the lower score is 0. Family satisfaction was categorized into two groups: those reporting satisfaction levels below the mean and those equal to or above the mean, classified as not satisfied and satisfied, respectively. Confidentiality was maintained, with no collection of individual identifiers. Data collection commenced following ethical clearance approval. The questionnaire was prepared in both Amharic and English versions to ensure easy understanding for all participants. The aim of the study was explained to the participants, and informed consent was obtained and the trained data collectors asked the participants the questions and recorded their responses. Participants were informed that their participation was voluntary, and they had the full right to decline participation or withdraw at any time. It was ensured that the study adhered to the principles of the Declaration of Helsinki.
Data Processing and Analysis Procedure
After completion of the data collection, the data was checked manually by the principal investigator for its completeness and consistency. Each completed questionnaire was assigned a unique code and entered to Epi Data version 3.1 Software. Then, data was exported to SPSS version 20 for analysis. Multi-collinearity was checked by examining the variance inflation factors (VIF), the values for each variable is less than or equal to 5 was taken as no similarity. The model goodness-of-fit was checked by Hosmer and Lemeshow test, and the results were found with p = 0.281. The data distribution normality was checked by histogram, and it was normally distributed. Descriptive statistics was applied to summarize in figures and tables to display the result. The association between independent factors and the outcome variable was determined at 95% confidence interval with bivariable logistic regression analyses and multivariate logistic regression analyses. Pearson correlation testing was used to identify the relationship between dependent and independent variables. Those variables with p-value of <0.2 in bivariate logistic regression was inserted into the final model. Factors associated with family satisfaction was identified using multivariable logistic regression analysis at a significance level of p-value <0.05 with 95% confidence interval. Adjusted Odds Ratio was used to see the strength of the association for multivariate logistic regression.
Data Quality control
To ensure data quality, several measures were implemented. A pre-test was conducted at the University of Gondar Comprehensive Specialized Hospital, involving 5% of the sample size. Participants in the pre-test were excluded from the main study. The collected data underwent thorough checks for completeness, accuracy, and clarity. Analysis revealed no need for modifications to the questionnaire.
Result
Sociodemographic Characteristics of the Study Participants
The study included a total of 400 parents whose family members had been admitted to the ICU, achieving a 100% response rate. The majority of participants (60.5%) were male. About 69.5% of the participants were aged between 18 and 40. Regarding educational level, 31.2% had completed high school, while those with no formal education accounted for the lowest proportion at 21.8%. Participants who were patient brothers or sisters constituted 28% of the sample. A significant portion of participants (30.2%) identified as farmers, and 68% of the participants resided with the patients (Table 1).
Family and Patient Related Factors Characteristics
Out of all participants, 49% of families visited the patient more than three times. The majority of participants had no previous experience with the same service. Additionally, a significant proportion of patients (76.8%) were on mechanical ventilators (Table 2).
 |
Table 2 ICU-Related Factors Related with Family Satisfaction with the Care Provided for ICU Admitted Patients in Amhara Region Comprehensive Specialized Hospitals, North West Ethiopia 2023, n=400 |
Level of Family Satisfaction with the Care Provided in ICU Admitted Patients
Over all family satisfaction with care provided to patients admitted to the intensive care unit was 58.6% at 95% CI (55.882,61.241). Families of patients are more satisfied with the care given for the patient (64.8%) and professional care (67.4%) provided for the patient. However, they were not satisfied by the care given for family (52.2%), the ICU environment (56.8%) and the decision-making involved during their ICU stay (55.8%). Atmosphere of ICU waiting room was the least satisfaction reported by families during their stay in ICU. ICU set up and physician skill and competence were the most which makes the families satisfied (Table 3 and Figure 2).
 |
Table 3 Level of Family Satisfaction with the Care Provided for ICU Admitted Patients in Amhara Region Comprehensive Specialized Hospitals, North West Ethiopia 2023, n=400 |
 |
Figure 2 Level of family satisfaction with the care provided in ICU admitted patients in Amhara region comprehensive specialized hospitals, North West Ethiopia 2023. |
Factors Associated with Level of Family Satisfaction for the Care Provided for ICU Patient
In the bivariable logistic regression analysis, variables such as age, educational status, income, living arrangements with the patient, the patient’s health condition, and families’ ICU experience demonstrated a p-value of less than 0.2, suggesting they are factors associated with family satisfaction with the care provided for ICU-admitted patients (Table 4).
In the multivariable logistic regression analysis, variables including age, educational status, income, patient’s health condition, and families’ ICU experience with a p-value of less than 0.05 were considered significant predictors of family satisfaction with the care provided for ICU-admitted patients. The study found that lacking formal education (AOR: 1.949, 95% CI: 1.005–4.169), completing primary education (AOR: 2.581, 95% CI: 1.327–5.021), and finishing grades 9–12 (AOR: 2.644, 95% CI: 1.411–4.952) were significantly associated with overall family satisfaction. Families who lacked previous ICU experience were 1.858 times more likely to report satisfaction with the care provided in the ICU compared to those with previous ICU experience (AOR: 1.858, 95% CI: 1.093–3.157) (Table 4 and Figure 3).
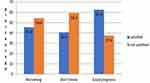 |
Figure 3 Satisfaction of families based on patient’s health condition admitted to ICU in Amhara region comprehensive specialized hospitals, North West Ethiopia 2023. |
Discussion
The study states that overall family satisfaction with the care provided for ICU-admitted patients is 58.6% at 95% CI:(55.882,61.241). The study conducted in the Republic of South Korea in 2018, reported a higher satisfaction level of 75.4% (SD, 17.7), while the study in Norway in 2021 found a satisfaction level of 70.4% (SD, 16.1), both surpassing the satisfaction level observed in the current study.1,34 Indeed, it is notable that a previous study conducted in Addis Ababa in 2017 reported a higher satisfaction level of 62%, which surpasses the satisfaction level observed in our current study. This variation might stem from differences in study populations, methodologies, or healthcare delivery systems between the two studies. Further exploration of these differences could provide valuable insights into improving satisfaction levels in ICU care.32 Compared to other studies, our results indicate a lower level of satisfaction. This discrepancy could be attributed to several factors, such as the cost of ICU care, communication barriers, understaffing, and inadequate equipment, all of which may have a negative impact on family satisfaction. Additionally, family members’ lack of information about medical procedures and technical aspects of intensive care might lead to heightened expectations, which could also contribute to lower satisfaction levels.1
In this study, family satisfaction with ICU care revealed that families reported being less satisfied with the atmosphere of the ICU waiting room. This finding is consistent with similar studies conducted in Norway, Australia, and Germany, which also found that families were less satisfied with the waiting environment of the ICU.1,38,39 Absolutely, the dissatisfaction with the ICU waiting room atmosphere could stem from various factors, such as inadequate comfort for families, insufficient seating, or lack of restroom facilities. These shortcomings in the waiting room environment can indeed contribute to a less satisfactory experience for families. Providing amenities and accommodations that prioritize the comfort and well-being of families could help address this issue and improve overall satisfaction with ICU care.
It appears that in this study, family satisfaction was notably low regarding the ease of obtaining information and the consistency of information during their involvement in decision-making processes. However, in contrast, the highest ratings for family satisfaction were related to the time provided for obtaining answers to their inquiries and the willingness of the intensive care staff to address these questions. Additionally, families reported receiving sufficient information to understand the patient’s condition, treatment plan, and progress. This discrepancy in satisfaction levels highlights the importance of effective communication and consistent provision of information in enhancing family experiences in ICU care.1 Indeed, the disparity in satisfaction levels regarding information provision may stem from families feeling that the information they receive is incomplete or insufficient. When families perceive that they lack essential information about their loved ones' condition, treatment options, and prognosis, it can lead to feelings of frustration and dissatisfaction. Therefore, ensuring that families receive comprehensive and clear information is crucial for improving satisfaction levels in ICU care.
In this study, dissatisfaction with physician communication with the family was reported as part of professional care. Interestingly, a similar study conducted in Norway found consistent results, with family members reporting low satisfaction with the frequency of conversations with physicians. This similarity suggests a common trend across different settings, highlighting the importance of improving physician-family communication to enhance family satisfaction in ICU care.40 Certainly, the dissatisfaction with physician communication may be attributed to families feeling they have limited opportunities to ask questions, express concerns, and seek clarification about their family members' condition. When families perceive a lack of open communication channels with physicians, it can contribute to feelings of frustration and dissatisfaction. Therefore, facilitating more opportunities for families to engage with physicians and address their concerns could help improve satisfaction levels in ICU care.
In this study, the least satisfaction reported during care giving for families was related to spiritual support and emotional support. Interestingly, this finding aligns with a study conducted in India, which also reported similar results. This consistency suggests that spiritual and emotional support for families may be areas requiring improvement across different cultural contexts, highlighting the importance of addressing these aspects in ICU care to enhance family satisfaction.41
In this study, older respondents were reported to be more likely satisfied with the care provided to ICU-admitted patients. Remarkably, this finding mirrors a study conducted in Hong Kong in 2015, which also observed a similar trend. This consistency suggests that older age may be a factor associated with higher satisfaction levels among family members of ICU patients across different cultural contexts.42 Indeed, the observation that older respondents are more likely to be satisfied with ICU care could be attributed to several factors. Younger individuals may have higher expectations and awareness about the standard of ICU care, leading to increased scrutiny and potentially lower satisfaction levels. Additionally, younger family members may desire greater involvement in the decision-making process, and if their expectations are not met, this could impact satisfaction. On the other hand, older families may have stronger social support networks and greater resilience, enabling them to cope more effectively with the stress and uncertainty associated with ICU care, thus leading to higher satisfaction levels.
It is interesting to note the contrast in findings between this study and the one conducted in the UK. While this study suggests that older adults are more satisfied with ICU care, the UK study indicates that younger adults are more satisfied.36 This discrepancy could be due to various factors, including differences in cultural expectations, healthcare systems, and study methodologies.
It is notable that the youngest family members, aged 18–39 years, reported the highest satisfaction with the care provided.1 This finding suggests that younger adults may have different perspectives or expectations regarding ICU care compared to older adults. Factors such as communication styles, information needs, and coping mechanisms may vary among different age groups, influencing their satisfaction levels. Further exploration of these differences could provide valuable insights for improving satisfaction with ICU care across all age groups.
In this study, families with lower levels of educational attainments, such as those with no formal education or below 12th grade, reported higher satisfaction with the care provided for ICU-admitted patients. Interestingly, this finding aligns with similar studies conducted in Saudi Arabia in 2016, Lebanon in 2017, and Brazil in 2009. It suggests that educational background may influence perceptions of ICU care, with those with lower education levels expressing higher satisfaction. Further research could explore the reasons behind this association and how healthcare providers can better meet the needs of families with varying educational backgrounds.43–45 This could be due to families with higher education may have higher expectations of the healthcare system44,46 and communication barriers between healthcare providers and families may be more pronounced for families with higher education, who may expect more detailed information and explanations about their families' conditions and treatment plan.
This study states the family with the patient who has good prognosis have more likely report satisfied with the service than those whose condition was worsening. This finding was similar to a study conducted in Addis Ababa in 2017.32 This phenomenon might occur because families may experience a sense of relief and appreciation when their loved one’s condition improves. A positive prognosis can also enhance families’ confidence in healthcare providers and the quality of care delivered in the intensive care unit (ICU). On the other hand, according to the USA study - worsening patients’ condition decrease families’ satisfaction.47
Research conducted in the United States in 2007, the United Kingdom in 2019, and Norway in 2021 indicated that increased severity of illness was linked to heightened levels of family satisfaction.1,36,41 This variance might be attributed to the possibility that clinical staff allocate more time to the families of severely ill patients.41 Another study suggests that family satisfaction remained unaffected by the health condition status of the patient.39
The findings of this study indicate that families with no prior experience in the ICU expressed higher levels of satisfaction compared to those with previous ICU experience. This discovery aligns with similar results from a study conducted in Brazil in 2015.48 This trend could be attributed to inadequate communication with healthcare providers during previous experiences, leading to a lack of understanding regarding the patient’s condition and available treatment options. This supported by previous, frequency of visits with physicians and lack of receiving of accurate information even in the event of bad news decrease the level of family satisfaction of the ICU.49
In contrast to the findings of this study, research conducted in Canada in 2002 and Australia in 2020 suggests that families with prior ICU experience reported higher levels of satisfaction compared to families without such experience.50,51 Other studies indicate that prior experience had no significant impact on the satisfaction level with the care provided for ICU-admitted patients among families.43
In the present study, families who lived with the patient reported higher levels of satisfaction with the care provided for ICU-admitted patients. However, a study conducted in Australia in 2020 contradicts these findings, suggesting that families who lived with the patient reported lower satisfaction compared to those who did not live with the patient.38 The reason behind this could be that family members who live with the patient have increased opportunities to communicate with healthcare providers and receive updates on the patient’s condition.
In this study, individuals with higher economic status, indicated by their level of income, reported higher satisfaction with the care provided for ICU-admitted patients compared to those with lower economic status. This finding mirrors results from a similar study conducted in Addis Ababa.52 This discovery aligns with results from studies conducted in both the USA and Egypt, which suggest that lower income levels are correlated with decreased satisfaction with ICU care.47,53,54 This could be attributed to the fact that higher-income families may have the financial resources to manage the costs associated with ICU care. Consequently, they may experience less financial strain, enabling them to focus more on supporting their family members during their time in the ICU. This increased ability to provide support could lead to higher satisfaction with the care provided for the patient.
Strength and Limitation
The study could serve as a foundation for future research, particularly considering the limited number of similar studies conducted in Ethiopia. However, the use of dichotomous Likert data might result in the loss of information, as the nuances between each choice cannot be fully captured. Additionally, the data collection method through structured interviews could introduce response bias and interviewer bias, potentially influencing the study’s outcomes. These limitations should be acknowledged and addressed in future studies to enhance the validity of the findings.
Conclusion
Overall, the level of satisfaction among families is positive. However, satisfaction levels were lower regarding the care for the family and their involvement in decision-making processes. Additionally, families reported the lowest satisfaction levels with the ICU waiting environment and the provision of spiritual support.
Certain demographic factors were associated with varying levels of satisfaction. Older age, lower educational attainment, and improvement in the patient’s condition were correlated with higher satisfaction levels. Conversely, families with patients on mechanical ventilators and those with previous ICU experience reported lower levels of satisfaction.
Recommendation
The overall satisfaction level in this study appears to be lower compared to other studies. To enhance family satisfaction, healthcare providers should focus on several key areas:
Effective Communication: Healthcare providers should communicate regularly and effectively with family members, ensuring they are informed about the patient’s condition and treatment plan.
Involvement in Decision-Making: Family members should be actively involved in the decision-making process regarding the patient’s care. This can help empower families and ensure their preferences are considered.
Education and Support: Providing education to family members about the patient’s condition, treatment plan, and post-discharge care can help alleviate anxiety and enhance their ability to support the patient.
Improving ICU Waiting Environment: Preparation of the waiting room and providing basic supplies for families in the ICU can contribute to a more comfortable and supportive environment for families.
Training for Healthcare Professionals: Healthcare professionals should undergo training on family-centered care and communication skills to better engage with and support family members during their loved ones' hospitalization.
Abbreviations
FS, Family satisfaction; ICU, Intensive care unit; MICU, Medical intensive care unit; MV, Mechanical ventilator; NICU, Neurological intensive care unit; PICU, Pediatric intensive care unit; SICU, Surgical intensive care unit.
Data Sharing Statement
All data generated or analyzed during this study were included in this published article and available on request.
Ethics Approval and Consent to Participate
Ethical clearance was obtained from the Institutional Ethics Review Committee from the university of Gondar School of Medicine's ethical review board with letter number 06/01/4097/2015. All information were kept confidential and no individual identifier was collected. The aim of the study was explained to the participants, and informed consent was obtained. Anyone not volunteering for participation is informed that they have the full right not to participate or stop at any time. We have confirmed that our study complies with the Declaration of Helsinki.
Ethical Consideration
Ethical clearance for this study was granted by the Ethical Review Committee of the School of Medicine and Health Sciences, College of Medicine, University of Gondar (UOG). Prior to participation, each study subject provided oral informed consent after receiving a thorough explanation of the study’s objectives, purpose, and their right to refuse participation. Confidentiality measures were implemented to ensure the privacy and anonymity of participants’ information.
Acknowledgment
We express our sincere gratitude to our colleagues for their invaluable contributions, whether direct or indirect, to the development of this study. Additionally, we extend our heartfelt thanks to the study participants for graciously agreeing to participate in our research. Their willingness to contribute has been instrumental in the advancement of our work.
Funding
University of Gondar.
Disclosure
The authors declared that they have no competing interests.
References
1. Haave RO, Bakke HH, Schröder A. Family satisfaction in the intensive care unit, a cross-sectional study from Norway. BMC Emergency Medicine. 2021;21(1):1–12. doi:10.1186/s12873-020-00394-z
2. Kodali S, Stametz RA, Bengier AC, Clarke DN, Layon AJ, Darer JD. Family experience with intensive care unit care: association of self-reported family conferences and family satisfaction. J Crit Care. 2014;29(4):641–644. doi:10.1016/j.jcrc.2014.03.012
3. Sundararajan K, Sullivan TR, Chapman M. Determinants of family satisfaction in the intensive care unit. Anaesthesia and Intensive Care. 2012;40(1):159–165. doi:10.1177/0310057X1204000120
4. Abate SM, Assen S, Yinges M, Basu B. Survival and predictors of mortality among patients admitted to the intensive care units in southern Ethiopia: a multi-center cohort study. Ann Med Surg. 2021;65:102318. doi:10.1016/j.amsu.2021.102318
5. Hinkle JL, Fitzpatrick E. Needs of American relatives of intensive care patients: perceptions of relatives, physicians and nurses. Intensive Crit Care Nurs. 2011;27(4):218–225. doi:10.1016/j.iccn.2011.04.003
6. Lai VKW, JC-H L, Lee A. Psychometric validation of the Chinese patient-and family satisfaction in the intensive care unit questionnaires. J Crit Care. 2019;54:58–64. doi:10.1016/j.jcrc.2019.07.009
7. Lange MP. Family stress in the intensive care unit. Crit Care Med. 2001;29(10):2025–2026. doi:10.1097/00003246-200110000-00031
8. Jones C, Bäckman C, Capuzzo M, Flaatten H, Rylander C, Griffiths R. Precipitants of post-traumatic stress disorder following intensive care: a hypothesis generating study of diversity in care. Intensive Care Med. 2007;33(6):978–985. doi:10.1007/s00134-007-0600-8
9. Delva D, Vanoost S, Bijttebier P, Lauwers P, Wilmer A. Needs and feelings of anxiety of relatives of patients hospitalized in intensive care units: implications for social work. Soc Work Health Care. 2002;35(4):21–40. doi:10.1300/J010v35n04_02
10. Lee LY, Lau YL. Immediate needs of adult family members of adult intensive care patients in Hong Kong. J Clin Nurs. 2003;12(4):490–500. doi:10.1046/j.1365-2702.2003.00743.x
11. Kentish-Barnes N, Lemiale V, Chaize M, Pochard F, É A. Assessing burden in families of critical care patients. Crit Care Med. 2009;37(10):S448–S456. doi:10.1097/CCM.0b013e3181b6e145
12. Carlson EB, Spain DA, Muhtadie L, McDade-Montez L, Macia KS. Care and caring in the intensive care unit: family members’ distress and perceptions about staff skills, communication, and emotional support. J Crit Care. 2015;30(3):557–561. doi:10.1016/j.jcrc.2015.01.012
13. Liang Y, Li J, Pan W. Family satisfaction in the intensive care unit: the influence of disease severity, care relationship, patient anxiety and patient pain. Inten Cri Care Nurs. 2021;63:102995. doi:10.1016/j.iccn.2020.102995
14. Yousefi H, Karami A, Moeini M, Ganji H. Effectiveness of nursing interventions based on family needs on family satisfaction in the neurosurgery intensive care unit. Iranian J Nurs Midwifery Res. 2012;17(4):296.
15. Sole ML, Klein DG, Moseley MJ. Introduction to critical care nursing E-Book. Elsevier Health Sci. 2020;664.
16. Heyland DK, Tranmer JE, Kghirw G. Measuring family satisfaction with care in the intensive care unit: the development of a questionnaire and preliminary results. J Crit Care. 2001;16(4):142–149. doi:10.1053/jcrc.2001.30163
17. Hunziker S, McHugh W, Sarnoff-Lee B, et al. Predictors and correlates of dissatisfaction with intensive care. Crit Care Med. 2012;40(5):1554. doi:10.1097/CCM.0b013e3182451c70
18. Boyle DK, Miller PA, Forbes-Thompson SA. Communication and end-of-life care in the intensive care unit: patient, family, and clinician outcomes. Crit Care Nurs Quar. 2005;28(4):302–316. doi:10.1097/00002727-200510000-00002
19. Pagnamenta A, Bruno R, Gemperli A, et al. Impact of a communication strategy on family satisfaction in the intensive care unit. Acta Anaesthesio Scand. 2016;60(6):800–809. doi:10.1111/aas.12692
20. Salins N, Deodhar J, Muckaden MA. Intensive care unit death and factors influencing family satisfaction of intensive care unit care. Indian J Crit Care Med. 2016;20(2):97. doi:10.4103/0972-5229.175942
21. Molter NC. Needs of relatives of critically ill patients: a descriptive study. Heart Lung. 1979;8(2):332–339.
22. Huffines M, Johnson KL, Smitz Naranjo LL, et al. Improving family satisfaction and participation in decision making in an intensive care unit. Critical Care Nurse. 2013;33(5):56–69. doi:10.4037/ccn2013354
23. Hwang DY, Yagoda D, Perrey HM, et al. Assessment of satisfaction with care among family members of survivors in a neuroscience intensive care unit. J neuros nurs. 2014;46(2):106. doi:10.1097/JNN.0000000000000038
24. Baharoon S, Yafi WA, Qurashi AA, et al. Family satisfaction in critical care units. J Patient Safety. 2017;13(3):169–174. doi:10.1097/PTS.0000000000000140
25. Stricker KH, Kimberger O, Schmidlin K, Zwahlen M, Mohr U, Rothen HU. Family satisfaction in the intensive care unit: what makes the difference? Intensive Care Med. 2009;35(12):2051–2059. doi:10.1007/s00134-009-1611-4
26. Azoulay E, Chevret S, Leleu G, et al. Half the families of intensive care unit patients experience inadequate communication with physicians. Crit Care Med. 2000;28(8):3044–3049. doi:10.1097/00003246-200008000-00061
27. Alsharari AF. The needs of family members of patients admitted to the intensive care unit. Patient Preference Adherence. 2019;Volume 13:465–473. doi:10.2147/PPA.S197769
28. Abuqamar M, Arabiat DH, Holmes S. Parents’Perceived satisfaction of care, communication and environment of the pediatric intensive care units at a tertiary children’s hospital. J Pediatr Nurs. 2016;31(3):e177–84. doi:10.1016/j.pedn.2015.12.009
29. Wright S, Harvey S, Walmsley E, Ferrando-Vivas P, Harrison D, Rowan K. Family satisfaction with critical care in the United Kingdom. Inten Care Med Exp. 2015;3(1):1–S1. doi:10.1186/2197-425X-3-S1-A22
30. Lamiani G, Ciconali M, Argentero P, Vegni E. Clinicians’ moral distress and family satisfaction in the intensive care unit. J Health Psychol. 2020;25(12):1894–1904. doi:10.1177/1359105318781935
31. Idris AH, Becker LB, Ornato JP, et al. Utstein-style guidelines for uniform reporting of laboratory CPR research: a statement for healthcare professionals from a task force of the American heart association, the American college of emergency physicians, the American college of cardiology, the European resuscitation council, the heart and stroke foundation of Canada, the institute of critical care medicine, the safar center for resuscitation research, and the society for academic emergency medicine. Circulation. 1996;94(9):2324–2336. doi:10.1161/01.cir.94.9.2324
32. Teshome G, Roge N, Ayalew Y, Sibany A. Family satisfaction towards care provided to critically ill patients and associated factors in the ICU of governmental hospitals of Addis Ababa town, 2017. J Trauma Treat. 2018;7(429):2167–1222.1000429. doi:10.4172/2167-1222.1000429
33. Abebe S. Mother’s Satisfaction with neonatal intensive care services and associated factors at public hospitals of Bahir-Dar city North West Ethiopia; 2023.
34. Min J, Kim Y, Lee J-K, et al. Survey of family satisfaction with intensive care units: a prospective multicenter study. Medicine. 2018;97(32):e11809. doi:10.1097/MD.0000000000011809
35. Myhren H, Ekeberg Ø, Langen I, Stokland O. Emotional strain, communication, and satisfaction of family members in the intensive care unit compared with expectations of the medical staff: experiences from a Norwegian University Hospital. Intensive Care Med. 2004;30(9):1791–1798. doi:10.1007/s00134-004-2375-5
36. Ferrando P, Gould DW, Walmsley E, et al. Family satisfaction with critical care in the UK: a multicentre cohort study. BMJ open. 2019;9(8):e028956. doi:10.1136/bmjopen-2019-028956
37. Green P, Edwards EJ, Tower M. Core procedural skills competencies and the maintenance of procedural skills for medical students: a Delphi study. BMC Medical Education. 2022;22(1):259. doi:10.1186/s12909-022-03323-9
38. McLennan M, Aggar C. Family satisfaction with care in the intensive care unit: a regional Australian perspective. Aust Crit Care. 2020;33(6):518–525. doi:10.1016/j.aucc.2020.01.003
39. Schwarzkopf D, Behrend S, Skupin H, et al. Family satisfaction in the intensive care unit: a quantitative and qualitative analysis. Intensive Care Med. 2013;39(6):1071–1079. doi:10.1007/s00134-013-2862-7
40. Frivold G, Dale B, Slettebø Å. Family members’ experiences of being cared for by nurses and physicians in Norwegian intensive care units: a phenomenological hermeneutical study. Inten Cri Care Nurs. 2015;31(4):232–240. doi:10.1016/j.iccn.2015.01.006
41. Wall RJ, Curtis JR, Cooke CR, Engelberg RA. Family satisfaction in the ICU: differences between families of survivors and nonsurvivors. Chest. 2007;132(5):1425–1433. doi:10.1378/chest.07-0419
42. Lam S, So H, Fok S, et al. Intensive care unit family satisfaction survey. Hong Kong Med J. 2015;21(5):435–443. doi:10.12809/hkmj144385
43. Hajj M, Gulgulian T, Haydar L, Saab A, Dirany F, Badr LK. The satisfaction of families in the care of their loved ones in CCUs in Lebanon. Nursing in Critical Care. 2017;22(4):203–211. doi:10.1111/nicc.12195
44. Mahrous MS. Relating family satisfaction to the care provided in intensive care units: quality outcomes in Saudi accredited hospitals. Revista Brasileira de Terapia Intensiva. 2017;29(2):188–194. doi:10.5935/0103-507X.20170018
45. Neves FBCS, Dantas MP, Bitencourt AGV, et al. Analysis of family satisfaction in intensive care unit. Revista Brasileira de terapia intensiva. 2009;21(1):32–37.
46. Meneguin S, de Souza Matos TD, Miot HA, Pollo CF. Association between comfort and needs of ICU patients’ family members: a cross-sectional study. J Clin Nurs. 2019;28(3–4):538–544. doi:10.1111/jocn.14644
47. Baker R, Wu AW, Teno JM, et al. Family satisfaction with end-of-life care in seriously ill hospitalized adults. J Am Geriatr Soc. 2000;48(S1):S61–9. doi:10.1111/j.1532-5415.2000.tb03143.x
48. Fumis RRL, Ranzani OT, Faria PP, Schettino G. Anxiety, depression, and satisfaction in close relatives of patients in an open visiting policy intensive care unit in Brazil. J Crit Care. 2015;30(2):440. e1–e6. doi:10.1016/j.jcrc.2014.11.022
49. Azoulay E, Pochard F, Chevret S, et al. Impact of a family information leaflet on effectiveness of information provided to family members of intensive care unit patients: a multicenter, prospective, randomized, controlled trial. Am J Respir Crit Care Med. 2002;165(4):438–442. doi:10.1164/ajrccm.165.4.200108-006oc
50. Heyland DK, Rocker GM, Dodek PM, et al. Family satisfaction with care in the intensive care unit: results of a multiple center study. Crit Care Med. 2002;30(7):1413–1418. doi:10.1097/00003246-200207000-00002
51. Naef R, von Felten S, Petry H, Ernst J, Massarotto P. Impact of a nurse-led family support intervention on family members’ satisfaction with intensive care and psychological wellbeing: a mixed-methods evaluation. Aust Crit Care. 2021;34(6):594–603. doi:10.1016/j.aucc.2020.10.014
52. Damghi N, Khoudri I, Oualili L, et al. Measuring the satisfaction of intensive care unit patient families in Morocco: a regression tree analysis. Crit Care Med. 2008;36(7):2084–2091. doi:10.1097/CCM.0b013e31817c104e
53. Eltaybani S, Ahmed FR. Family satisfaction in Egyptian adult intensive care units: a mixed-method study. Inten Cri Care Nurs. 2021;66:103060. doi:10.1016/j.iccn.2021.103060
54. Becker G, Newsom E. Socioeconomic status and dissatisfaction with health care among chronically ill African Americans. Am J Public Health. 2003;93(5):742–748. doi:10.2105/AJPH.93.5.742
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.