Back to Journals » Vascular Health and Risk Management » Volume 18
Factors Influencing Self-Care Behaviors in Hypertension Patients With Complications
Authors Pahria T, Nugroho C, Yani DI
Received 17 March 2022
Accepted for publication 24 June 2022
Published 5 July 2022 Volume 2022:18 Pages 463—471
DOI https://doi.org/10.2147/VHRM.S366811
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Daniel Duprez
Tuti Pahria,1 Cahyo Nugroho,1,2 Desy Indra Yani1
1Faculty of Nursing, Universitas Padjadjaran, Jatinangor, 45363, Indonesia; 2Nursing Management Team, Majenang Hospital, Majenang, 53257, Indonesia
Correspondence: Desy Indra Yani, Faculty of Nursing, Universitas Padjadjaran, Jl. Raya Bandung-Sumedang KM 21, Jatinangor, 45363, Indonesia, Tel/Fax +62 22-7796647, Email [email protected]
Abstract:
Purpose: While hypertension with accompanying complications remains a life-threatening illness, a critical program in its management and prevention is implementing self-care behaviors (SCBs). This study examined the factors associated with SCB that are dominant in hypertension patients with complications.
Materials and Methods: This quantitative study was conducted using the regression analytic method and a cross-sectional approach. The non-probability sampling technique was used, and the response rate was 96.2%. Data were collected using a modified hypertension self-care profile (HBP-SCP) questionnaire, hypertension knowledge questionnaire, family support questionnaire, and the brief-illness perception questionnaire (B-IPQ).
Results: The mean total SCB score was high at 55.9% with a mean of 191.01, SD = 5.16; 77.5% of the respondents had no disease history, 80.4% had good knowledge, 58.8% had strong family support, and 50% had a good perception of the disease. Factors that were significantly related to SCB were family support (p = 0.00, r = 0.75) and illness perception (p = 0.00, r = 0.77), while disease history (r = 0.47) and knowledge were not significantly related (r = 0.13). Moreover, the analysis of multiple linear regression with the backward method showed that the most dominant factor influencing SCB was illness perception (p = 0.00, = 0.47, B = 0.495, R2 = 0.650). The effect of illness perception on SCB (65%) meant that each 0.50 perception score increased the SCB score by one.
Conclusion: It is recommended that health workers increase patient perception using innovative interventions to improve the SCB of hypertension patients with complications.
Keywords: disease history, disease perception, family support, hypertension complications, self-care behaviors
Introduction
Uncontrolled hypertension can cause various complications. Each increase in systolic blood pressure of 20 mmHg to > 115 mmHg or a rise in diastolic blood pressure of 10 mmHg to 75 mmHg will elevate the risk of cardiovascular disease and stroke.1 Constant uncontrolled increase in blood pressure can cause changes in the blood vessels and heart, leading to complications in cardiovascular disease, including myocardial infarction, left ventricular hypertrophy, congestive heart failure, aneurysms, and stroke. Further, prolonged hypertension potentially leads to chronic kidney disease, nephropathy, and retinopathy.2,3 Globally, hypertension with complications is estimated to cause the deaths of approximately 9.4 million people with 17 million cases worldwide each year.4 The prevalence of hypertension in Indonesia in the population aged 18 years and over increased from 25.8% in 2013 to 34.1% in 2018.5 According to the Heart Center for Data and Information in 2014, the complications of hypertension that most frequently result in death are heart disease and stroke, at rates of 45% and 51%, respectively.6 The death rate is predicted to reach 23.3 million by 2030.7 Aside from cardiovascular complications, hypertension also causes kidney dysfunction and visual problems.8
Hypertension patients with complications and poor self-care behaviors (SCBs) might experience several impacts, including decreased quality of life, reduced sleep quality, and stress. A study stated that hypertension patients who experience complications with chronic kidney, cardiovascular, and diabetes mellitus diseases had a lower quality of life than those without complications. Further, quality of life is determined by the number of complications that accompany the disease and is associated with the physical functioning of patients.9 Another study concluded that 66.70% of respondents with abnormal blood pressure had poor sleep quality.10 Patients’ ability to perform SCBs correlated with better clinical outcomes, controlled blood pressure, reduced frequency of medical consultations, and drug consumption.11,12 These behaviors can also improve the quality of life in patients with chronic conditions, prevent disability, and reduce care costs. SCB has also been shown to reduce primary care visits by 17% for outpatients and 50% for emergency presentations.13
SCB is the ability to care for oneself and undertake the activities needed to achieve, maintain, or promote optimal health, including specific activities in response to chronic conditions.14 According to Orem, SCB comprises a series of complex actions intended to achieve specific goals and obtain predetermined results. The main goal is to maintain life, health, and wellbeing,15 as seen in the application of Orem’s self-care deficit nursing theory (SCDNT). According to Orem, a person’s initiative in performing SCBs is influenced by the ability or capacity to carry out self-care, as well as fundamental conditioning factors. Although the concept of primary conditions has been identified, there is no standard applied to conditions, place, and time.15 Individuals who experience hypertension for a long time need support to carry out daily activities with their families and communicate with health workers about their treatment and care. Essential conditioning in hypertension patients adapted from Orem’s SCDNT theory includes age, gender, marital status, family history, duration, knowledge support, and perception of hypertension.16 Therefore, patient communication with health workers has a strong influence, directly or indirectly, on SCBs through knowledge, family support, and perceptions about hypertension.
Several previous studies reported factors influencing SCBs, including age, gender, place of residence, ethnicity/race, education level, marital status, availability of blood pressure measuring devices at home, monthly income, history, and duration of hypertension.3,11,17–19 Other factors include having a comfortable place for activities, knowledge, social support, family support, and perceptions of the disease severity.16,19–22
There were limited studies on the population of hypertension patients with complications, despite these being prevalent in the majority of such patients. The management of the hypertensive in hospital is not optimal; only an assessment is conducted to ascertain blood pressure and accompanying symptoms. SCBs in hypertension patients to prevent the occurrence of more severe complications of hypertension have not received attention. Management is limited to following instructions from doctors who focus on administering drugs. The present paper addresses this gap by analyzing the factors associated with SCBs in hypertension patients with complications.
Materials and Methods
This quantitative study was conducted using a regression analytic method and a cross-sectional approach. It was carried out at the internal medicine clinic, the neural disease clinic, and the hemodialysis room in a hospital in Cilacap Regency, Central Java from November 10 to December 7, 2020.
The study population consisted of hypertension patients with complications receiving treatment/control at these hospital clinics. We used a non-probability sampling technique. Patients selected for the sample were members of the population who met the inclusion criteria, which included those who were declared to have hypertension by a doctor; those routinely taking hypertension drugs accompanied by at least one of the following: hypertension complications, stroke, heart disease, and kidney disease/failure triggered by hypertension; those with compos mentis consciousness, with no a cognitive impairment or severe motor disorders, such as paresis/-plegia of the upper extremities; and those who could read and write independently. Heart disease triggered by high blood pressure is known as hypertensive heart disease (HHD). The exclusion criteria were dangerous illnesses or acute or chronic conditions that limited a patient’s ability to participate in the study. The sample size was calculated using Thorndike’s rule of thumb formula with multiple analyses. Based on this formula, the required number of samples was 10×4 + 50 = 90 respondents, accounting for a 20% drop-out rate; hence, the total number of respondents was 108.
The dependent variable was SCBs in hypertension patients with complications, while the independent variables were family history, knowledge, family support, and perception of the disease. The measure of SCBs was the hypertension self-care profile (HBP-SCP), modified to measure hypertension patients with complications. This instrument is a comprehensive measuring tool including three domains to assess behaviors, motivation, and self-efficacy in patients with hypertension. It was based on a combination of two theories: Orem’s self-care model and motivational interviewing.23
The hypertension knowledge instrument was adapted from a previous study (Prasetyo 2012) and comprised a questionnaire consisting of ten questions, including understanding hypertension, risk factors, signs and symptoms, therapy, low-salt diet, and physical activity. The answer choices consisted of true and false (scored true = 1 and false = 0).
The family support instrument was adapted from the theory of House and Kahn and encompassed four supports: instrumental, reward, informational, and emotional.24 It comprised 20 positive question items divided into four parts—instrumental, reward, informational, and emotional supports—each housing five questions. The answers were dictated by a Likert scale, with never (TP) = 1, sometimes (KD) = 2, often (SR) = 3, and always (SL) = 4.
The hypertension perception measurement used the brief-illness perception questionnaire (B-IPQ),25 the Indonesian version of which has been tested for reliability and validity. This study received permission to use this instrument.26
The univariate analysis sought to explain the characteristics of the respondents and provide a description of each variable. Features of respondents—age, gender, education level, marital status, and complications experienced—were described in frequency and percentage distributions. The dependent variable, SCBs, was described as the average score, categorized as high when greater than the mean total score and low when less than the mean total score. Meanwhile, disease history, knowledge, family support, and illness perception were described in frequency distribution categories and presentations.
The bivariate analysis was conducted to determine the relationship between the dependent and independent variables. Before this analysis, the data normality test was carried out on numerical data using the Kolmogorov Smirnov test with a sample greater than 50. A bivariate selection of each independent and dependent variable was conducted. Variables included in the multiple regression models are those with a p-value less than 0.25. The bivariate analysis obtained values for disease history (p = 0.012, p < 0.25), knowledge (p = 0.190, p < 0.25), family support (p = 0.000, p < 0.25), and illness perception (p = 0.000, < 0, 25), indicating that all independent variables could be included in the multiple analysis model. We used the multiple analyses, including linear regression analysis, together with the backward method.
Permission was obtained from the Research Ethics Commission of the Faculty of Medicine, the Universitas Padjadjaran, with Ethics No. 1019/UN6.KEP/EC/2020, in compliance with the Declaration of Helsinki. The nurses in the hospital introduced the researchers to the patients who would be potential subjects of the study. All respondents received verbal and written explanations and a consent form was given to interested respondents. Signed informed consent or verbalization of willingness to participate was obtained for all participants. The researcher assured the respondents that their participation was voluntary and that they could leave the study. All information was maintained confidentially, and the results were presented in aggregate form for academic purposes only. Additionally, there was no risk associated with the completion of the questionnaires.
Results
Approximately half of the respondents were aged between 56 and 65 years, and 37 (36.3%) had an average age of 56.37 years. The majority, 63 (61.8%), were male, and 83 (81.4%) had attained at least primary-level education. A higher proportion of respondents were married (93, or 91.2%), and the most prevalent complications experienced included stroke 49 (48%), kidney disorders (CKD) 39 (38.2%), and HHD 14 (13.7%) (Table 1).
 |
Table 1 Frequency Distribution of Demographic and Health Data (n=102) |
Complicated hypertension patients mostly had high levels of SCB, with a total of 57 (55.9%) exhibiting good SCBs, and a mean of 191.01 (SD = 5.16). The majority of respondents (77.7%) had no disease history; 80.4% had relatively good knowledge of their disease; 58.8% had strong family support, and 50% were observed to have a good perception of the disease. The variables derived from the questionnaires are shown in Table 2.
 |
Table 2 Frequency Distribution of Self-Care Behaviors Disease History, Knowledge, Family Support, and Perception of Illness (N= 102) |
The bivariate analysis results showed a significant relationship between medical history and SCBs (p = 0.01, r = 0.47), and family support and SCBs (p = 0.00, r = 0.75). Further, illness perception had a significant relationship with SCB (p = 0.00, r = 0.77), while the knowledge factor had no meaningful relationship (Table 3).
 |
Table 3 Relationships Between Disease History, Knowledge, Family Support, and Illness Perception with Self Care Behaviors (N= 102) |
Differences in family support and disease perception accounted for 65% of the variances in SCB levels. As shown in Table 3, the result of Durbin-Watson test indicated that there was no autocorrelation with a value of 2.25, as the normal range value for no autocorrelation is between 1.5 and 2.5. The magnitude of the influence caused by these two variables was obtained by an R2 value of 0.65, meaning that the independent variables, family support and disease perception, affect SCB by 65%. Other factors account for the remaining 35% (see Table 4).
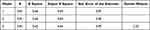 |
Table 4 Model Summary of Disease History, Knowledge, Family Support, Illness Perception to Predict Self Care Behaviors |
Disease history had the highest p-value (0.47); therefore, this variable was excluded from Model I. Similarly, the knowledge variable had a high p-value (0.20) and was hence excluded from Model II. The final modeling results showed that SCBs were influenced by family support and perception of the disease. The analysis results of multiple linear regression using the backward method obtained the equation SCB = 133.758 + 0.42** family support + 0.50** perception of the disease. This equation meant that each addition of 0.50 for family support added one score to the SCB value, as did every increment of 0.50 for illness perception. The constant, 133.758, means that when family support and perception of illness = 0, then SCB = 133.758. The most dominant factor that influenced SCB in the multiple linear regression analysis was illness perception, with a regression coefficient value of = 0.47 (see Table 5).
 |
Table 5 Modeling the Influence of Disease History, Knowledge, Family Support, and Perceptions of Self Care Behaviors (N= 102) |
Discussion
The Relationship Between Disease History and Self-Care Behaviors in Hypertension Patients with Complications
The statistical test results showed that the history of the disease had a positive relationship (r = 0.47) with SCB (p = 0.01). A history of comorbidities was significantly associated with the implementation of SCB among hypertension patients. In the previous study, the statistical test results obtained AOR = 0.50 and 95% (CI = 0.289, 0.88). Hypertension patients who performed adequate SCB could control their blood pressure by 44.7%. Meanwhile, low SCB levels in hypertension patients with comorbidities could worsen their conditions.27 This result is supported by a previous study, which found the history of comorbidities to be significantly associated with SCB when implementing lifestyle modification practices.28 Therefore, hypertension accompanied by comorbidities is complicated to control. Comorbidities can worsen the condition, making patients unable to implement optimal lifestyle changes. However, these results are not in line with a study conducted in Beijing, China, which found that hypertension patients with a history of diabetes mellitus (DM) and a family disease history were not significantly prone to SCB. Patients with DM history showed lower levels of SCB than those without a disease history (18% versus 31%, respectively; p = 0.09). Patients with a family history of hypertension exhibited higher levels of SCB than those without a disease history (29.4% versus 44.8%, respectively; p = 0.08). This is likely because patients with a disease history have learned about coping with their illnesses.29
The Relationship Between Knowledge and Self-Care Behaviors in Hypertension Patients with Complications
The statistical test results showed no significant relationship between knowledge and SCB (p = 019, r = 0.131), presumably because the respondents engaged in SCB already had a good understanding of their diseases. Therefore, this variable had no effect on SCBs in hypertension patients with complications. These results differ from those of another study, which found a significant relationship between the level of knowledge and SCB in weight management (AOR = 0.13, 95% CI = 0.03–0.57), and adherence to non-consumption of alcohol (AOR = 0.07, 95% CI = 0.03–0.16).30 Poor weight-management adherence is associated with inadequate levels of knowledge and education in the community. In addition, the socio-cultural influence of the Ethiopian community and the absence of a ban on drinking alcohol by local government result in high consumption.
The studies reported a significant relationship between SCB to lower the risks posed by hypertension and the knowledge of patients and their partners suffering from the disease.30,31 Another study conducted in Bushehr, Southern Iran, showed that good knowledge of hypertension was the factor most related to the ability to perform self-care in weight control (OR = 1.247) and medication regimens (OR = 1.376).32 Another study has reported that skilled patients have a higher frequency of self-care.33 One possible reason for these differences might be that the type of hypertension in the current study is hypertension with complications, while previous studies focused only on hypertension patients.
The Relationship Between Family Support and Self-Care Behaviors
Family support had a positive relationship (r = 0.752) with SCB (p = 0.000). These results align with a study that tested levels of SCB and their influencing factors on respondents with controlled hypertension,34 finding that SCB was significantly related to family support (r = 0.21, p < 0.015). Another study in Nigeria revealed that good family functioning was significantly associated with SCB (OR = 2585, 95% CI = 1636, 4084).35 In addition, good family support was significantly related to SCB which controlled blood pressure (AOR = 1.9, 95% CI = 1.1–3.1).36 Medication adherence and regular blood pressure measurement, as aspects of self-care behavior, were positively related to family social support.21 The various domains of family support—motivational support (p = 0.000, RP = 2.65), reward support (p = 0.001, RP = 2.83), informational support (p = 0.000, RP = 4.27), and instrumental support (p = 0.000, RP = 12.7)—also showed significant correlation with the SCBs of hypertension patients.37
The Relationship Between Illness Perception and Self-Care Behaviors
Illness perception had a positive relationship (r = 0.771) with SCB (p = 0.000). This result is in line with a study that found disease severity perception to be a predictor for SCB performance in adherence to treatment regimens (OR = 1.301), low-salt diet (OR = 1.139), and abstinence from alcohol (OR = 1.562).32 Perception of poor health status can reduce SCB in hypertension patients. This result is corroborated by a study conducted in India, which reported that 62.9% of respondents had unfavorable SCB levels, which were influenced by negative perceptions of health status (OR = –2.8).13 Another study performed in China obtained a similar result, wherein perceptions of illness contributed to changing respondents’ SCB by 47%; the remaining 53% was influenced by other factors.38
The Most Dominant Factor Influencing Self-Care Behaviors
Illness perception was observed to be the most dominant factor influencing SCB. This result conforms to existing findings that people with hypertension require long treatment, perform daily activities with their families, and often communicate with health care providers.16 A positive perception of individual illness will inspire the right decisions regarding SCB activities. Illness perception affects individual behavior in responding to health risks and can encourage positive activities, such as complying with treatment regimens.39
It is recommended that nurses develop innovative interventions to improve awareness among patients with complications of hypertension. Interventions should be tailored to patients’ needs and may include a combination of strategies to improve patients’ conditions and treatment. In addition, nurses should involve families in patient interventions, which may allow families to actively support patients’ recovery, and thereby increase SCB. Nurses should conduct regular educational activities for patients and their families in outpatient clinics and hemodialysis rooms to deepen their understanding of the illness and raise their awareness.
This study cannot be generalized to all populations as it used a non-random sampling technique. Further, the study’s respondents exhibited a tendency toward good SCBs, as they were patients who actively engaged with their health facilities, attending the internal medicine clinic and the neurology clinic, and routinely performing hemodialysis. However, it is possible for patients who do not regularly seek treatment to have poor SCBs. Therefore, further investigation considering potential selection biases is essential.
Conclusion
The SCBs of hypertension patients with complications were encouraging. Disease history, family support, and illness perception were significantly correlated with SCBs. Conversely, hypertension knowledge did not have a substantial connection with SCB. As most respondents in the study already had good knowledge and experience of SCBs in this study, knowledge was less likely to affect the implementation of SCB. The most dominant factor influencing SCB was the perception of the disease.
Acknowledgments
We thank all respondents and the hospital for their cooperation.
Disclosure
The authors report no conflicts of interest in this study.
References
1. Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Clin Hypertens. 2014;16(1):14–26. doi:10.1111/jch.12237
2. Sawicka K, Szczyrek M, Jastrzębska I, Prasał M, Zwolak A, Daniluk J. Hypertension – the silent killer. J Pre-Clin Clin Res.2011;5(2):43–46.
3. Gebremichael GB, Berhe KK, Beyene BG, Gebrekidan KB. Self-care practices and associated factors among adult hypertensive patients in ayder comprehensive specialized hospital, Tigray, Ethiopia, 2018. BMC Res Notes. 2019;12(1). doi:10.1186/s13104-019-4502-y
4. World Health Organization. Global Brief on Hypertension. Silent Killer, Global Public Health Crisis. Geneva, Switz: World Health Organization; 2013.
5. Ministry of Health Republic of Indonesia. Report on the results of basic health research (riskesdas) Indonesia in 2018; 2018.
6. Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–e292. doi:10.1161/01.cir.0000441139.02102.80
7. Ministry of Health Republic of Indonesia. Infodatin: The Heart Health Situation. Jakarta: Data and Information Center of the Indonesian Ministry of Health; 2014.
8. Devadason P. Risk factors for hypertension and its complications – a hospital based case control study risk factors for hypertension and its complications – a hospital based case control study. Int J Interdiscip Multidiscip Stud. 2016;1(August):1–5.
9. Soni RK, Porter AC, Lash JP, Unruh ML. Health-related quality of life in hypertension, chronic kidney disease, and coexistent chronic health conditions. Adv Chronic Kidney Dis. 2010;17(4):e17–e26. doi:10.1053/j.ackd.2010.04.002
10. Alfi WN, Yuliwar R. The relationship between sleep quality and blood pressure in patients with hypertension. J Berk Epidemiol. 2018;6(1):18. doi:10.20473/jbe.v6i12018.18-26
11. Salim H, Lee PY, Sazlina SG, et al. The self-care profiles and its determinants among adults with hypertension in primary health care clinics in Selangor, Malaysia. PLoS One. 2019;14(11):1–14. doi:10.1371/journal.pone.0224649
12. Labata BG, Ahmed MB, Mekonen GF, Daba FB. Prevalence and predictors of self care practices among hypertensive patients at Jimma University Specialized Hospital, Southwest Ethiopia: cross-sectional study. BMC Res Notes. 2019;12(1):86. doi:10.1186/s13104-019-4125-3
13. Dasgupta A, Sembiah S, Paul B, Ghosh A, Biswas B, Mallick N. Assessment of self-care practices among hypertensive patients: a clinic based study in rural area of Singur, West Bengal. Int J Community Med Public Heal. 2017;5(1):262. doi:10.18203/2394-6040.ijcmph20175794
14. Richard AA, Shea K. Delineation of self-care and associated concepts. J Nurs Scholarsh an off Publ Sigma Theta Tau Int Honor Soc Nurs. 2011;43(3):255–264. doi:10.1111/j.1547-5069.2011.01404.x
15. Orem DE. Nursing Concepts of Practice.
16. Saleema L, Panpakdee O, Arpanantikul M, Chai-Aroon T. The influence of basic conditioning factors and self-care agency on self-care behaviors in Thais with hypertension. Pacific Rim Int J Nurs Res. 2016;20(1):5–17.
17. Ademe S, Aga F, Gela D. Hypertension self-care practice and associated factors among patients in public health facilities of Dessie town, Ethiopia. BMC Health Serv Res. 2019;19(1):1–9. doi:10.1186/s12913-019-3880-0
18. Fazel S, Motlagh Z, Chaman R, Sadeghi E, Eslami AA. Self-care behaviors and related factors in hypertensive patients. Iran Red Crescent Med J. 2016;18(6). doi:10.5812/ircmj.35805.Research
19. Khresheh R, Mohammed N. Self-care behaviors among women with hypertension in Saudi Arabia. IOSR J Nurs Health Sci. 2016;5(3):52–56. doi:10.9790/1959-0503035256
20. Chang AKEJL. Factors affecting self-care in elderly patients with hypertension in Korea. Int J Nurs Pract. 2015;21:584–591. doi:10.1111/ijn.12271
21. Hu HH, Li G, Arao T. The association of family social support, depression, anxiety and self-efficacy with specific hypertension self-care behaviours in Chinese local community. J Human Hypertension. 2015;29(July 2014):198–203. doi:10.1038/jhh.2014.58
22. Ma C, Zhou W, Huang C, Huang S. A cross-sectional survey of self-rated health and its determinants in patients with hypertension ☆, ☆☆. Appl Nurs Res. 2015;28(4):347–351. doi:10.1016/j.apnr.2015.03.001
23. Han H-R, Lee H, Commodore-Mensah Y, Kim M. Development and validation of the hypertension self-care profile: a practical tool to measure hypertension self-care. J Cardiovasc Nurs. 2014;29(3):E11–E20. doi:10.1097/JCN.0b013e3182a3fd46
24. Bisnu MIKH, Kepel B, Mulyadi N. Relationship between family support and degree of hypertension in hypertensive patients at ranomuut health center manado city (hubungan dukungan keluarga dengan derajat hipertensi pada pasien hipertensi di puskesmas ranomuut kota manado). J Keperawatan. 2017;5(1):108–118.
25. Moss-Morris R, Weinman J, Petrie K, Horne R, Cameron L, Buick D. The revised illness perception questionnaire (IPQ-R). Psychol Heal. 2002;17(1):1–16. doi:10.1080/08870440290001494
26. Robiyanto R. Test the validity of the Indonesian version of the B-Ipq Instrument in hypertensive patients at Sultan Syarif Mohamad Alkadrie Hospital Pontianak (Uji Validitas Instrumen B-Ipq Versi Indonesia pada pasien hipertensi Di Rsud Sultan Syarif Mohamad alkadrie. Soc Clin Pharm Indones J. 2016;1(1):41–49.
27. Abdulwahed A, Seid A. Level of self-care practice and associated factors among hypertensive patients in Jimma university specialized hospital, south west Ethiopia. Rehabil Sci. 2020;5(2):12. doi:10.11648/j.rs.20200502.11
28. Buda ES, Hanfore LK, Fite RO, Buda AS. Lifestyle modification practice and associated factors among diagnosed hypertensive patients in selected hospitals, South Ethiopia. Clin Hypertens. 2017;23(1):1–9. doi:10.1186/s40885-017-0081-1
29. Hu H, Li G, Arao T. Prevalence rates of self-care behaviors and related factors in a rural hypertension population: a questionnaire survey. Int J Hypertens. 2013;2013:1–8. doi:10.1155/2013/526949
30. Niriayo YL, Ibrahim S, Kassa TD, et al. Practice and predictors of self-care behaviors among ambulatory patients with hypertension in Ethiopia. PLoS One. 2019;14(6):e0218947. doi:10.1371/journal.pone.0218947
31. Asmah EE, Orkoh E. Self-care knowledge of hypertension prevention and control among women in Contemporary Ghana. Am J Heal Educ. 2017;48(6):374–381. doi:10.1080/19325037.2017.1358120
32. Larki A, Tahmasebi R, Reisi M. Factors predicting self-care behaviors among low health literacy hypertensive patients based on health belief model in Bushehr District, South of Iran. Int J Hypertens. 2018;2018:9752736. doi:10.1155/2018/9752736
33. Worku Kassahun C, Asasahegn A, Hagos D, et al. Knowledge on hypertension and self-care practice among adult hypertensive patients at university of Gondar Comprehensive Specialized Hospital, Ethiopia, 2019. Int J Hypertens. 2020;2020:5649165. doi:10.1155/2020/5649165
34. Lee E, Park E. Self-care behavior and related factors in older patients with uncontrolled hypertension. Contemp Nurse. 2017;53(6):607–621. doi:10.1080/10376178.2017.1368401
35. Ayodapo A, Monsudi K, Omosanya O, Elegbede O. Family functioning and adherence to medication: a study of hypertensive in a tertiary hospital, South Western Nigeria. CHRISMED J Heal Res. 2018;5(3):197–202. doi:10.4103/cjhr.cjhr_28_18
36. Chacko S, Jeemon P. Role of family support and self-care practices in blood pressure control in individuals with hypertension: results from a cross-sectional study in Kollam District, Kerala. Wellcome Open Res. 2020;5:180. doi:10.12688/wellcomeopenres.16146.1
37. Mariyani M, Azriful A, Bujawati E. Family support through self care behavior for hypertension patients. Divers Dis Prev Res Integr. 2021;2(1):1–8. doi:10.24252/diversity.v2i1.23180
38. Ma C. An investigation of factors influencing self-care behaviors in young and middle-aged adults with hypertension based on a health belief model. Hear Lung. 2018;47(2):136–141. doi:10.1016/j.hrtlng.2017.12.001
39. Alison Phillips L, Leventhal H, Leventhal EA. Assessing theoretical predictors of long-term medication adherence: patients’ treatment-related beliefs, experiential feedback and habit development. Psychol Health. 2013;28(10):1135–1151. doi:10.1080/08870446.2013.793798
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
