Back to Journals » Journal of Multidisciplinary Healthcare » Volume 17
Factors Determining the Functional Efficiency of Patients After Ischemic Stroke After Neurological Rehabilitation
Authors Ścisło L , Staszkiewicz M , Walewska E, Paplaczyk-Serednicka M, Bodys-Cupak I, Zawieja P
Received 27 October 2023
Accepted for publication 12 February 2024
Published 4 March 2024 Volume 2024:17 Pages 959—969
DOI https://doi.org/10.2147/JMDH.S444049
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Lucyna Ścisło,1 Magdalena Staszkiewicz,1 Elżbieta Walewska,1 Małgorzata Paplaczyk-Serednicka,1 Iwona Bodys-Cupak,2 Paulina Zawieja3
1Department of Clinical Nursing, Institute of Nursing and Midwifery, Faculty of Health Sciences, Jagiellonian University, Medical College, Kraków, 31-501, Poland; 2Laboratory of Theory and Fundamentals of Nursing, Institute of Nursing and Midwifery, Faculty of Health Sciences, Jagiellonian University Medical College, Krakow, 31-126, Poland; 3Faculty of Health Sciences, Jagiellonian University, Medical College, Kraków, 31-501, Poland
Correspondence: Lucyna Ścisło, Department of Clinical Nursing, Institute of Nursing and Midwifery, Faculty of Health Sciences, Jagiellonian University, Medical College, 25 M. Kopernik street, Kraków, 31-501, Poland, Email [email protected] Magdalena Staszkiewicz, Department of Clinical Nursing, Institute of Nursing and Midwifery, Faculty of Health Sciences, Jagiellonian University, Medical College, 25 M. Kopernik street, Kraków, 31-501, Poland, Email [email protected]
Introduction: The factors determining the level of functional efficiency in patients after ischemic stroke are: age, sex, physical condition, mental activity before stroke, previous neurological deficits, comorbidities, nutritional status and the course of the stroke.
Aim: Assessment of the functional efficiency of patients before and after rehabilitation due to ischemic stroke and determination of the influence of selected factors on the effects of rehabilitation measured by functional efficiency.
Material and Methods: The study was conducted in neurological rehabilitation centers among 82 people diagnosed with ischemic stroke. The examination was performed twice: on admission to the ward and after a month of neurological rehabilitation. The diagnostic survey method, the Barthel scale, the NRS 2002 scale were used, and the BMI was calculated.
Results: The functional efficiency level of the patients was varied, higher after one month of rehabilitation (p < 0.05). Among the patients who achieved a lower level of functional efficiency, the following factors had a significant influence: underweight and overweight (p = 0.002), risk of malnutrition (p = 0.002), right-sided paresis (p = 0.016), limited physical activity before stroke (p = 0.01) and the later rehabilitation period (p = 0.01). There was no correlation between sociodemographic data and the level of efficiency of patients after a stroke after one month of rehabilitation.
Conclusion: The level of functional efficiency after rehabilitation improved in all patients, however, to a different extent depending on the nutritional status and physical activity. Therefore, it is important to to undertake rehabilitation in the shortest possible time.
Keywords: ischemic stroke, functional efficiency, Barthel scale
Introduction
Acute ischemic stroke (AIS), characterized by a sudden onset of focal or generalized cerebral disturbances, leads to neurological deficits, such as hemiparesis, cognitive, emotional and intellectual disorders.1–3 Hemiparesis, or unilateral paresis, indicates one-sided brain damage. Right-sided paresis indicates the occurrence of a stroke in the left hemisphere of the brain and vice versa. According to the National Stroke Prevention and Treatment Program, in Poland 60,000 people are affected each year by a stroke, and the risk of its occurrence increases with age. The data from the report show that the incidence of stroke in young people is 1 in 30,000, in people between 75 and 85 years of age - 1 in 45, and in older people over 85 years of age - even 1 to 30.4,5 The most common consequence of AIS is motor disability, ie paresis (weakening of muscle strength), paresis of the muscles of the face and limbs, difficulties with maintaining balance, lack of motor coordination, speech disorders. Muscle tension as well as surface and deep sensation disorders are common.6,7
Factors influencing the functional efficiency in patients after AIS include age, sex, physical condition and mental activity before stroke, previous neurological deficits, comorbidities, nutritional status, and the course of stroke.8,9
The principles of modern rehabilitation of stroke patients assume that each patient is treated from the very beginning as if he were to fully recover the lost functions. Knowledge of stroke risk factors is essential in identifying patients at increased risk of stroke, as well as in the early introduction of prophylaxis. Proceedings in the post-stroke rehabilitation ward are undertaken by a closely cooperating specialized team.10–12 The overall goals of neurological rehabilitation in the early period of AIS are: to reduce mortality within 1 month of stroke by preventing life-threatening complications; minimizing the degree of disability of patients later after a stroke; improving the quality of life of patients; influence on the patient’s mental state and cooperation in the therapeutic process; reducing stroke expenses as well as patient and family education.13–15
In the case of UNM, the immobilization period lasts about 2–5 days. Early bedside rehabilitation is aimed at preventing complications arising from prolonged immobilization, ie contractures, bedsores, pneumonia, deep vein thrombosis, urinary disorders and limitations in verbal contact with the patient. At a further stage in the rehabilitation process of post-MI patients, attention is focused on restoring and re-forming motor functions. This process involves repeatedly repeating good patterns of given movements, which are then memorized by the CNS. Next comes the acquisition of the ability to sit up on the bed, and when this element is achieved, then it is necessary to move on to the gradual verticalization of the patient. In uprighting and learning to walk, movement control, proper positioning of the head, trunk and pelvis, as well as proper assessment of defense mechanisms are important elements.
The greatest neurological progress is noticed during the first 3 months after UM. However, rehabilitation exercises should be carried out all the time until the progression of the patient’s functional ability is visible. The great merit of rehabilitation for patients after UM is the recovery, in many cases, of total or partial independence that allows normal functioning and fulfillment of social roles.10,12
The greatest improvement in functional performance is seen in the first 3 months after a stroke. However, rehabilitation exercises should be carried out for as long as the patient’s functional efficiency is progressing. A great merit of rehabilitation for patients after a stroke is the recovery, in many cases, of complete or partial independence that enables normal functioning and fulfilling social roles.10,14,16–19
The aim of the study was to assess the functional efficiency of patients before and after rehabilitation due to cerebral ischemic stroke and to determine the influence of selected factors on the effects of rehabilitation.
Materials and Methods
The study was conducted in neurological rehabilitation centers in the Małopolskie Voivodeship in 2018–2019 among 82 people diagnosed with acute ischemic stroke (AIS). The examination was performed twice: on admission to the ward and after a month of neurological rehabilitation (physical rehabilitation, neuropsychological and speech therapy rehabilitation, supportive conversations, education). The study included people who met the criteria for inclusion in the study group: expressed consent to participate in the study, age ≥ 60 years, first-time ischemic stroke, the period of time up to 3 months from the occurrence of AIS, presence of hemiparesis, no information and cognitive function (f.e. memory, attention, thinking and perception) disorders that would make it impossible to establish verbal-logical contact. 100 people were included in the study, but 11 people resigned from rehabilitation, 2 people’s health condition deteriorated and 5 people did not express their informed consent to participate in the study.
The participants of the study were informed about the purpose of the study, voluntary participation in it and the possibility of withdrawing at each stage of its conduct. Each patient consented to participate in the study and signed the attached “Declaration of informed consent to participate in the study”. The study used targeted selection of participants. Initially, potential participants were selected in consultation with the organizational heads of the units.
The study was conducted in accordance with the principles of Good Scientific Practice, the principles of the Helsinki Declaration, Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC (General Data Protection Regulation) and the act of 10 May 2018 on the protection of personal data.20,21 Research based on the consent of the bioethics committee in Jagiellonian University number KBET/27/B/2014.
In order to conduct the study, the diagnostic survey method was used. The research technique was a survey. The research tool was the original questionnaire. The study also used the Barthel scale, the NRS 2002 scale, and the BMI was calculated. The survey questionnaire consisted of 12 questions on sociodemographic data, such as: age, sex, education, marital status, professional situation, type of professional work and questions related to the type of stroke (right-sided, left-sided), comorbidities, eg high blood pressure, ischemic heart disease, atrial fibrillation, a history of myocardial infarction, diabetes, additional physical activity undertaken, eg cycling, swimming, walking, Nordic walking, hiking, dancing, gymnastics. The respondents were asked about the time between the occurrence of a stroke and undertaking rehabilitation.
Each person was assessed for functionality according to the Barthel scale on the day of commencement of rehabilitation and after the period of 1 month of rehabilitation. The BMI was calculated for each patient on the day of starting rehabilitation, and the risk of malnutrition was assessed based on the NRS 2002.
A healthy adult with a normal weight-to-height ratio has an index between 18.5 and 24.9. A BMI below 18.5 indicates that you are underweight. People with a BMI of 25.0–29.9 are overweight. A BMI above 30.0 is considered obese.
The Barthel scale is used to assess efficiency in terms of everyday activities. It allows the assessment of self-reliance and the degree of need for assistance. This scale consists of ten basic daily activities, such as eating, moving and sitting, moving on flat surfaces, climbing stairs, dressing and undressing, personal hygiene, using the toilet, bathing the whole body and controlling body functions. A score of 100 points is possible on the Barthel scale. There are three scoring ranges: scoring 0 to 20 means total dependence, 20 to 80 points means the patient needs the help of an outside person to some extent, while scoring between 80 and 100 points means the patient can function independently with a little help from an outside caregiver/nurse.22–24
The NRS 2002 scale assesses the risk related to the nutritional status and the severity of the disease. Assessment is made in two categories: nutritional deterioration and disease severity. The points from both categories are summed up and constitute the final result, which should be assessed according to the scoring (malnutrition: mild, moderate and severe).25
Statistical Analysis
The study applied the following statistical methods. The data collected as part of the surveys and the results of the clinimetric methods were subjected to statistical analysis using the following methods: Student’s t-test, chi-square statistics and the values of the non-parametric correlation coefficient.
Correlations between quantitative variables were analyzed using the Spearman’s rank correlation coefficient. The level of significance in the analysis was α = 0.05. The collected research material was prepared in the IBM SPSS program.26
Characteristics of the Study Group
The study group (SG) consisted of 53% women and of 47% men. People aged 60–70 were the most numerous group (73%). These people were under hospital care. The sociodemographic characteristics is presented in Table 1.
 |
Table 1 Study Participants in Terms of Sociodemographic Variables |
Health Situation of the Respondents
Before the stroke, patients were physically fit After, in the study group, 60% had left hemiparesis, and 40% had right hemiparesis. The most common comorbid disease was high blood pressure which occurred in 68% of the studied patients. Diabetes mellitus and ischemic heart disease were second, with 35% each. The rarest disease was cancer and it occurred among 4% of respondents. Among the studied group, 37% of patients were admitted to the neurological rehabilitation unit ≤ 14 days from the occurrence of a stroke incident, 51% of patients were hospitalized between 15–31 day, and 12% were admitted ≥ 31 days from the onset of AIS. Taking into account the assessment of risk related to the nutritional status assessed using the NRS 2002 scale, 70% of patients achieved a result of ≤ 2 points, which indicated the current normal nutritional status, 30% of patients obtained ≥ 3 points, which meant the risk of malnutrition and the need to start nutritional support – Table 2.
 |
Table 2 Study Participants in Terms of Clinical Variables |
Results
Using the Barthel scale on admission to the ward, the functional efficiency of the patients was assessed before rehabilitation and after a 1-month rehabilitation period – Table 3.
 |
Table 3 Division Depending on the Degree of Disability According to the Barthel Scale After Rehabilitation |
Before the start of rehabilitation, the most numerous group were people with severe disabilities (76%). There were no people with full efficiency in the study group. Mild disability concerned 9% of the respondents, and moderate disability – 16%. However, after 1 month of rehabilitation, people with severe disability accounted for 46%, and 15% of respondents were fully functional. People with mild and moderate disabilities accounted for 20% each.
A significant correlation between rehabilitation and the functional state of patients has been shown. The analysis shows that after 1 month of rehabilitation, the functional capacity of patients improved in relation to the functional status assessed on the Barthel scale before the start of rehabilitation – Table 4.
 |
Table 4 Statistical Data Showing the Differences Between the Groups Before and 1 Month After Rehabilitation (Barthel Scale) |
The analysis shows that the improvement results do not depend on gender, education, age, marital status or professional activity (p>0.05).
Correlation Between the Functional Efficiency and the Number of Coexisting Diseases
The results show a moderate, negative impact of the patient’s burden with comorbidities on the result of functional efficiency according to the Barthel scale. The greater the burden of comorbidities, the lower the functional efficiency after rehabilitation – Table 5.
 |
Table 5 The Correlation Between the Occurrence of Comorbidities and Functional Efficiency (According to the Barthel Scale) in Patients After Stroke |
Correlation Between Functional Performance Status and Body Mass Index (BMI)
The correlation between the patients’ body mass index and the results of functional efficiency according to the Barthel scale was also analyzed. The analysis shows that the results of rehabilitation depend on the body mass index in the studied group of patients, p = 0.002. It is noticeable that in the group of patients whose BMI exceeds the norm, the efficiency is lower. People who are underweight and overweight have the results of a lower level of functional efficiency after rehabilitation - Table 6.
 |
Table 6 Correlation Between the BMI Level and the Functional Efficiency Status in Patients After Stroke |
Correlation Between Functional Efficiency Status and Nutritional Risk Assessment (NRS-2002)
The correlation between nutritional risk assessment (NRS-2002) and functional efficiency scores was also analysed. It was shown that the improvement results depend on the nutritional risk assessment in the studied group of patients p = 0.002. Therefore, people at risk of malnutrition (NRS ≥ 3) have a lower level of functional efficiency after rehabilitation - Table 7.
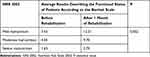 |
Table 7 Correlation Between the Nutritional Status of Post-Stroke Patients and Their Functional Efficiency |
Correlation Between Physical Activity Undertaken Before UNM and Functional Efficiency of Patients on the Basis of the Barthel Scale
Patients undertaking physical activity before the AIS achieved much better improvement results compared to patients who undertook only basic physical activity related to everyday functioning p = 0.01 - Table 8.
 |
Table 8 Correlation Between Physical Activity in Pre-Stroke Patients and Their Post-Stroke Physical Efficiency |
Correlation Between Functional Efficiency and the Side of Paresis After Stroke
The analysis showed that the final functional state after rehabilitation on the basis of the Barthel scale depends on the side of hemiparesis. People with left-sided paresis achieve an average of 4 points better results than people with right-sided paresis. This suggests that people with left-sided hemiparesis achieve better overall functional efficiency compared to people with right-sided hemiparesis (p <0.05) - Table 9.
 |
Table 9 Correlation Between the Occurring Type of Paresis and the State of Functional Efficiency in Patients After Stroke |
Correlation Between the Length of Time from the Onset of AIS to the Start of Rehabilitation and the Degree of Functional Attainment of the Subjects Based on the Barthel Scale
The study showed that the shorter the time from the onset of AIS to the start of rehabilitation, the better the patients’ functional status according to the Barthel scale p = 0.01. This correlation indicates that the sooner rehabilitation was undertaken after a stroke episode, the higher the functional performance scores were. Patients who received rehabilitation an average of 14 days after the stroke episode returned to full function, while patients who waited longer for rehabilitation were predisposed to develop lower functional capacity - Table 10.
 |
Table 10 Correlation Between the Time from the AIS Occurrence to Rehabilitation and the Functional Efficiency of Patients |
Discussion
Stroke remains the leading cause of adult disability, and the need for post-stroke rehabilitation services is increasing.27 The introduction of comprehensive rehabilitation in the early period after the occurrence of a stroke incident, adapted to the individual condition and needs of the patient, should take place immediately after stabilization of the clinical condition and should constitute an integral part of the treatment.28 The own research conducted was aimed at assessing the functioning of patients after AIS.
The assumption of the study was also to determine the relationship between various factors and the level of functional efficiency after a stroke with rehabilitation undertaken in the early period after a stroke.
Previous publications of studies that analyze the correlation between the given factors and the functional status of patients after stroke are only partially methodologically-highly assessed.29,30 An early and intensive rehabilitation program influences the functional outcomes of patients with acute stroke.31 The literature states that patients who developed AIS had comorbidities such as: arterial hypertension, atrial fibrillation, diabetes, ischemic heart disease and others. The most common comorbid disease in the study group is arterial hypertension (AH), which occurs in as many as 70% of patients. Significant is that every third patient is obese and has ischemic heart disease (IHD), almost every fifth patient has diabetes and hyperlipidemia, and every sixth patient has a history of atrial fibrillation.32
Numerous statistical studies show that the patient’s age, time elapsed since the stroke occurrence, number of comorbidities, and marital status of the patient were associated with low effectiveness of post-stroke rehabilitation.33 However, no studies by other authors were found to confirm this assumption.
In the authors’ own research, no correlation was found between patient’s education and rehabilitation outcomes. Different results were obtained by Kleinrok et al, ie low education predisposes to worse results of the rehabilitation process.34 In the remaining socio-demographic factors, ie marital status or the nature of the work performed, no dependencies were found, while Kleinrok et al indicate a negative significance for the results of rehabilitation of such factors as free marital status or the physical nature of professional work.33 Motor impairment after stroke is often permanent and causes disability, and women are less likely to recover fully and show worse functional outcomes.35 On the other hand, other researchers indicated that the best results of the rehabilitation process were obtained in the group of women under 60 years of age.32
During the analysis of many studies, a correlation was observed between the side of the paresis and functional performance after stroke. Damage to the left hemisphere of the brain, resulting in right-sided hemiparesis also leads to many other deficits in speech, verbal memory and writing skills. Damage to the left hemisphere of the brain also affects complex motor activities. Damage to the right hemisphere leads to minor disturbances, however, it may contribute to the occurrence of the hemispheric neglect syndrome.19 The conducted research shows that patients with left-sided paresis achieved better functional efficiency. Dziubek et al claim that the side of the paresis does not indicate prognosis and does not play a role in the analysis of the results of rehabilitation of patients.36
The obtained results of own research show that in the group of patients achieving BMI values exceeding the norm, the efficiency was lower. Patients with underweight and overweight achieved a lower level of functional status after rehabilitation. Rykała J. et al in their research show a correlation that is directly proportional between the BMI index and the functional efficiency of the studied group. Thus, the results show the correlation between excess body weight and a worse assessment of functional efficiency as a result of the performed rehabilitation without taking into account underweight.37 The analysis of own research also made it possible, on the basis of the NRS scale, to observe the correlation between the assessment of the risk of malnutrition and the results of rehabilitation. It turned out that people with a high risk of malnutrition obtained worse improvement results than people with a proper nutritional status. However, no studies by other authors confirming this assumption were found.
The issue of early neurological rehabilitation in patients in the early period after AIS is the subject of many scientific research and education of patients unaware of the importance of early rehabilitation for later functional efficiency in everyday life. After discharge from hospital, it is often necessary to continue rehabilitation after a stroke.38
Demonstration in the own study of the dependence of individual factors related to functional efficiency after a stroke with rehabilitation undertaken in the early period, indicates a strong need to undertake and continue therapeutic education and to motivate the society to undertake appropriate health behaviors to ensure the possibility of the best possible effects in the future if necessary undertaken rehabilitation activities.
The study of the functional performance of ischemic stroke patients after neurological rehabilitation is relevant from several perspectives, and is motivated by scientific, clinical and social aspects. A review of the literature indicates that there is limited data on specific factors affecting functional performance after such a stroke. Understanding the impact of nutritional status, side of hemiparesis, physical activity and sociodemographic data on rehabilitation outcomes can help tailor and optimize rehabilitation processes. Identifying key factors that influence functional improvement can lead to better therapeutic strategies.
The individual needs of patients can be better understood, allowing more effective rehabilitation plans to be constructed.
Summary
The results of the study may contribute to increasing public awareness of post-stroke rehabilitation and the role of various factors in the process of returning to daily functions. The social value of this study lies in promoting health behaviors against the occurrence of strokes, raising public awareness of neurological rehabilitation, and supporting stroke victims to return to active life.
The results of this study can provide a basis for further research into improving rehabilitation methods, developing new therapies and identifying potential areas for further scientific research.
Limitations of the Study
The time from discharge to rehabilitation was not examined, as some people were discharged home after treatment and waited longer for rehabilitation. This waiting time may have resulted in a worse rehabilitation outcome.
Conclusions
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Ratuszek–Sadowska D, Kowalski M, Woźniak K, Kochański B, Hagner W. Neurological rehabilitation of a patient after stroke – case report. J Educ Health Sport. 2016;6(8):28–40.
2. Siminska J, Pietkun K, Porzych P, et al. A review of selected methods for the rehabilitation of the upper extremity in patients after undergone brain ischemic stroke. J Educ Health Sport. 2016;6(4):240–248.
3. Department of Health Statistics and Information Systems. WHO Methods and Data Sources for Global Burden of Disease Estimates 2000‒2011. Genewa: World Health Organization; 2013:1–2.
4. Grupa R. Chorób Naczyń Mózgowych składająca się z przedstawicieli Ministerstwa Zdrowia i Narodowego Funduszu Zdrowia. Ogólnopolski Program Profilaktyki Chorób Naczyń Mózgowych (ICD10: I60-I69); 2020. Polish.
5. Kuczma M, Wolniak J, Filarecka A, Kuczma W Przywracanie sprawności kończyny górnej po udarze mózgu. Choroby XXI wieku – wyzwanie w pracy fizjoterapeuty. Wydawnictwo Wyższej Szkoły Zarządzania, Gdańsk; 2017:140–160. Polish.
6. Raciborski F, Gujski M Raport Instytutu Ochrony Zdrowia. Udar mózgu – rosnący problem w starzejącym się społeczeństwie. Instytut Ochrony Zdrowia, Warszawa; 2016:47–49. Polish.
7. Kamel H, Healey JS. Cardioembolic Stroke. Circ Res. 2017;120(3):514–526. doi:10.1161/CIRCRESAHA.116.308407
8. Jędrych M, Kulik TB, Jędrych T, et al. An evaluation of the impact of rehabilitation on the quality of life in patients after cerebral stroke. J Educ Health Sport. 2018;8(12):245–254.
9. Spence JD. Nutrition and Risk of Stroke. Nutrients. 2019;11(3):647. doi:10.3390/nu11030647
10. Hoffman J, Zbonik M, Hoffman A, Sochanek M. Rola rehabilitacji w procesie leczenia pacjentów po przebytym udarze mózgu. Podgórska M Choroby XXI wieku – wyzwanie w pracy fizjoterapeuty. Wydawnictwo Wyższej Szkoły Zarządzania, Gdańsk; 2017:127–139. Polish.
11. Morreale M, Marchione P, Pili A, et al. Early versus delayed rehabilitation treatment in hemiplegic patients with ischemic stroke: proprioceptive or cognitive approach? Eur J Phys Rehabil Med. 2016;52(1):81–89.
12. Simić-Panić D, Bošković K, Milićević M, et al. The Impact of Comorbidity on Rehabilitation Outcome after Ischemic Stroke. Acta Clin Croat. 2018;57(1):5–15. doi:10.20471/acc.2018.57.01.01
13. Piskorz J, Wójcik G, Iłzecka J, Kozak-Putowska D. Wczesna rehabilitacja pacjentów po udarze niedokrwiennym mózgu. Medycyna Ogólna i Nauki o Zdrowiu. 2014;20(4):351–355. Polish. doi:10.5604/20834543.1132034
14. Kwolek A, eds.. Rehabilitacja medyczna.
15. López-Larraz E, Sarasola-Sanz A, Irastorza-Landa N, Birbaumer N, Ramos-Murguialday A. Brain-machine interfaces for rehabilitation in stroke: a review. Neuro Rehabilitation. 2018;43(1):77–97. doi:10.3233/NRE-172394
16. Sharififar S, Shuster JJ, Bishop MD. Adding electrical stimulation during standard rehabilitation after stroke to improve motor function. A systematic review and meta-analysis. Ann Phys Rehabil Med. 2018;61(5):339–344. doi:10.1016/j.rehab.2018.06.005
17. Dworzynski K, Ritchie G, Diane Playford E. Stroke rehabilitation: long-term rehabilitation after stroke. Clin Med. 2015;15(5):461–464. doi:10.7861/clinmedicine.15-5-461
18. Winters C, Kwakkel G, Meskers CGM. Moving stroke rehabilitation forward: the need to change research. NeuroRehabilitation. 2018;43(1):19–30. doi:10.3233/NRE-172393
19. Antecki J, Brelak E, Sobolewski P, Kozera G. Profilaktyka pierwotna i wtórna udaru niedokrwiennego mózgu w świetle obecnych zaleceń i rekomendacji. Forum Medycyny Rodzinnej. 2018;12(3):89–98. Polish.
20. The Act of 10th May 2018 on the protection of personal data. Dz.U; 2018. Available from: http://prawo.sejm.gov.pl/isap.nsf/DocDetails.xsp?id=WDU20180001000.
21. Regulation of the European Parliament and of the Council (EU) 2016/679 of 27th April 2016. On the protection of individuals with regard to the processing of personal data and on the free movement of such data and the repeal of Directive 95/46 / EC (General Data Protection Regulation). Available from: https://eur-lex.europa.eu/legal-content/PL/TXT/?uri=CELEX%3A32016R0679.
22. Borowicz AM. Tests for Evaluating the Functional Capacity of Older People. Wieczorowska-Tobis K, Kostka T, Borowicz AM, Eds. Warszawa, Poland: Wydawnictwo Lekarskie PZWL; 2011:45–60.
23. Mahoney FI, Barthel D. Functional testing: Barthel Index. Md Med J. 1965;14:56–61.
24. Kędziora-Kornatowska K, Mitura K. Analysis of the fitness of patients up according to the Barthel scale on the example seniors of nursing home residents. Pielegniarstwo w Opiece Dlugoterminowej. 2018;2:28–39.
25. Jak ocenić stan pacjentów w szpitalu? Polish. Available from: https://polspen.pl/jak-ocenic-stan/.
26. statistical calculations. Polish. Available from: https://www.ibm.com/pl-pl/products/spss-statistics.
27. Stinear CM, Lang CE, Zeiler S, Byblow WB. Advances and challenges in stroke rehabilitation. Lancet Neurol. 2020;19(4):348–360. doi:10.1016/S1474-4422(19)30415-6
28. Kałużny K, Kałużna A, Kochański B, et al. The influence of neurological rehabilitation on the functioning of patients after ischemic stroke – a retrospective analysis. J Educ Health Sport. 2016;6(12):38–52.
29. Veerbeek JM, Kwakkel G, van Wegen EE, Ket JC, Heyman MW. Early prediction of outcome of activities of daily living after stroke: a systematic review. Stroke. 2011;42(1482):1488. doi:10.1161/STROKEAHA.110.604090
30. Hakkennes SJ, Brock K, Hill KD. Selection for inpatient rehabilitation after acute stroke: a systematic review of the literature. Arch Phys Med Rehabil. 2011;92(12):2057–2070. doi:10.1016/j.apmr.2011.07.189
31. Imura T, Nagasawa Y, Fukuyama H, Imada N, Oki S, Araki O. Effect of early and intensive rehabilitation in acute stroke patients: retrospective pre-/post-comparison in Japanese hospital. Disabil Rehabil. 2018;40(12):1452–1455. doi:10.1080/09638288.2017.1300337
32. Kałużny K, Kałużna A, Kochański B, et al. Wpływ rehabilitacji neurologicznej na funkcjonowanie pacjentów po przebytym udarze niedokrwiennym mózgu – analiza retrospektywna. J Educ Health Sport. 2016;6(12):
33. Kobylańska M, Kowalska J, Neustein J, et al. The role of biopsychosocial factors in the rehabilitation process of individuals with a stroke. Work. 2018;61(4):523–535. doi:10.3233/WOR-162823
34. Kleinrok A, Płaczkiewicz D, Stefańczyk P, Kudrelek K. Wpływ wybranych czynników socjodemograficznych i klinicznych na stopień niepełnosprawności pacjentów hospitalizowanych z powodu udaru mózgu. Przeglad Medyczny Uniwersytetu Rzeszowskiego. 2013;2:151–163. Polish.
35. Grabowska-Fudala B, Jaracz K, Górna K. Zapadalność, śmiertelność i umieralność z powodu udarów mózgu – aktualne tendencje i prognozy na przyszłość. Przeglad Epidemiologiczny. 2010;64(3):
36. Dziubek W, Kowalska J, Nowak W. Ocena pacjentów starszych po udarze mózgu według Skandynawskiej Skali Udarów. Psychogeriatria Polska. 2011;8(2):63–72. Polish.
37. Rykała J, Kwolek A. Wpływ wybranych czynników na jakoś życia oraz stan funkcjonalny pacjentów po udarze mózgu. Przeglad Medyczny Uniwersytetu Rzeszowskiego. 2009;4:384–391. Polish.
38. Thompson S, Ranta A, Porter K, Bondi N. How much rehabilitation are our patients with stroke receiving? N Z Med J. 2019;132(1499):49–55.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
