Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 15
Factors Associated with HIV Positive Serostatus Disclosure to Sexual Partners Among Sexually Active Young People on Anti-Retroviral Therapy in Central Uganda
Authors Kavuma D , Kirwana VB , Taani M
Received 7 February 2023
Accepted for publication 28 May 2023
Published 8 June 2023 Volume 2023:15 Pages 293—311
DOI https://doi.org/10.2147/HIV.S407535
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Olubunmi Akindele Ogunrin
David Kavuma,1– 3 Venantius Bbaale Kirwana,4,5 Mary Taani6
1Mildmay Institute of Health Sciences, Kampala, Uganda; 2School of Graduate Studies, Uganda Martyrs University-Nkozi, Kampala, Uganda; 3Makerere University School of Public Health, Kampala, Uganda; 4Monitoring, Evaluation and Learning, Sexual Reproductive Health and Rights Alliance, Kampala, Uganda; 5Makerere University School of Statistics and Applied Economics, Kampala, Uganda; 6Community Systems Strengthening, Mubende Region, Mildmay Uganda, Kampala, Uganda
Correspondence: David Kavuma, Tel +256772839416, Email [email protected]; Venantius Bbaale Kirwana, Tel +256781630721, Email [email protected]
Introduction: HIV serostatus disclosure is a fundamental HIV prevention and care strategy yet with a paucity of literature. This study comprehended the factors associated with HIV serostatus disclosure to sexual partners among young people aged 15– 24 years on anti-retroviral therapy (ART).
Methods: This explanatory sequential study utilized quantitative data from 238 young people who had been on ART for over 12 months and were sexually active for at least 6 months in seven districts of Central Uganda. Pearson’s Chi-square and multinomial logistic regression analysis at α=0.05 was used to determine the factors associated with serostatus disclosure among study participants. Qualitative data from 18 young people were collected using an in-depth interview guide and analyzed thematically.
Results: Non-disclosure was at 26.9%, one-way disclosure was at 24.4%, and two-way disclosure was at 48.7%. Participants who contracted HIV from their partners were three times more likely (RRR=2.752; 95% CI: 1.100– 6.888) to have one-way disclosure than non-disclosure, compared to those who had a perinatal infection. Those who contracted HIV from their partners were twice more likely (RRR=2.357; 95% CI: 1.065– 5.214) to have two-way disclosure than non-disclosure, compared to those who had a perinatal infection. Participants who stayed with their partners were four times more likely (RRR=3.869; 95% CI: 1.146– 13.060) to have two-way disclosure than non-disclosure, compared to those who stayed with their parents. Young people disclosed because they were tired of secrecy and desired treatment adherence and did not disclose due to fear of stigma and losing their partners’ support.
Conclusion: Many sexually active young people on ART did not disclose their HIV-positive status to sexual partners mainly due to poverty, having multiple-sexual partners, and stigma. Interventions fighting stigma, multiple-sexual relationships, and poverty among sexually active young people on ART should be strengthened.
Keywords: self-disclosure, one-way disclosure, two-way disclosure, non-disclosure, stigma, ART, single-sexual partner, multiple-sexual partners
Background
HIV-positive self-serostatus disclosure is the process and autonomous decision by which an HIV-positive person voluntarily informs another person (be it a sexual partner, family member(s), or friend) of his or her HIV status.1–3 Available literature notes that a person can choose to disclose his or her HIV status to a family, a group of people, or media (full-disclosure) or to a friend or relative, or health worker (partial disclosure) chooses not to reveal his or her status to anyone (non-disclosure).4
HIV serostatus to the sexual partner is considered to be one the important public health interventions in HIV prevention and care.1,5 Despite the practical and psychological complexities involved (like stigma) in HIV serostatus disclosure to a sexual partner, several benefits of HIV self-disclosure include a reduction in HIV transmission, decreased feelings of isolation, increased access to social support, and improved outcomes from anti-retroviral therapy (ART).1,6–8 Similarly, HIV-positive serostatus disclosure has been identified as one of the effective measures that have the potential of reducing risky sexual behaviors, especially among those that are sexually active (whether concordant HIV positive or discordant).2,8,9 Melis Berhe et al noted that HIV-positive serostatus disclosure provides an opportunity to discuss condom use and other contraceptives that would reduce further HIV transmission and enables them to make informed reproductive health choices with all its benefits.3 It is against this background that even UNAIDS and WHO supports HIV serostatus disclosure to sexual partner as a key HIV prevention intervention so long as it is free from criminalization.10,11
Health workers are not only required to encourage HIV-positive serostatus disclosure to the sexual partner right from when the sexually active person tests HIV positive, but also, should encourage those being enrolled to disclose their HIV serostatus to their sexual partners.1 Even those who failed to disclose after receiving HIV testing services or before being on anti-retroviral therapy (ART), should be continuously supported by health workers for HIV-positive serostatus disclosure to their partners.1,10
Despite the documented evidence on the benefits of HIV-positive serostatus disclosure among sexually active partners,1 it is reported that the magnitude of HIV-positive serostatus disclosure in low-and middle-income countries, is generally lower (about 50%) compared to the developed world with about (79%).12,13 Relatedly, it is reported that Uganda has low rates of HIV-positive serostatus disclosure among sexually active people.9 This poses a threat to HIV prevention, care, and treatment efforts since it is not only likely to affect the ART treatment outcomes but could also increase HIV reinfections and HIV drug resistance (HIVDR) whose rate is increasing in Uganda and other Sub-Saharan African (SSA) countries with HIV burden.14,15 In the long run, limited HIV-positive serostatus disclosure among sexually active partners on ART can lead to poor adherence to ART (like poor and inconsistent condom use) and increased chances of mother-to-child transmission of HIV.16
Despite the existence of various interventions like engaging men in HIV prevention among adolescent girls and young women,17,18 the 2015 Uganda’s HIV Prevention and Control Act that promotes HIV disclosure in the context of HIV prevention and care,19 a lot is still desired especially to protect Uganda’s window of hope which is still vulnerable to HIV infection. The 2022 Uganda Population-based HIV Impact Assessment survey, noted that about 360 young people get infected with HIV each day.20 Similarly, UNAIDS also emphasizes the vulnerability of young people to HIV infection where one gets HIV infection every after three minutes globally.21 This is further explained by the high rates of unprotected sex among HIV-positive young people5,20 in most Sub-Saharan African countries that continue to be the epicenter of HIV with over 70% of the 37 million people living with HIV worldwide by the end of the year 2022, of which 67% (n=29m were accessing ART in 2021).12,21
Much as there is a handful of studies done in some Sub-Saharan African (SSA) countries about HIV-positive serostatus disclosure among people on ART, those done specifically on sexually active young people on ART are hardly available in Uganda. Probably, this would help to address the paucity of literature on HIV serostatus disclosure to sexual partners among young people on ART in Uganda and beyond.
This study aimed to understand the factors associated with HIV-positive serostatus disclosure to sexual partners among young people on anti-retroviral therapy in selected public health facilities of Central Uganda. The study further explored the reasons for disclosure and non-disclosure of HIV serostatus by study participants to their sexual partners. This evidence findings of this study could inform the practices of healthcare providers, policy makers and research agendas, in the context of HIV prevention, care and treatment interventions among sexually active young people on ART. In addition, the results from this study would contribute to medical advances Uganda has made in the fight against HIV hence adding momentum to Uganda’s efforts to end the HIV by the year 2030 as stated in UN Sustainable Development Goal 3, target 3.3 that intends to end HIV epidemic.22
Study Setting and Population
This study took place in the Central region of Uganda which is one of the four regions (Central Western, Eastern, and Northern) which was purposefully selected for having the highest number of young people on ART.20 The Central region has 13 districts of which seven districts namely Kassanda, Kyotera, Luwero, Mityana, Mubende, Mukono, and Wakiso, were selected by simple random sampling method. Three public health facilities were selected from each district using a simple random sampling method.
Methodology
Study Design and Duration
This was a mixed methods study that utilized an Explanatory sequential design (Quantitative → Qualitative approach).23–25 Quantitative data were collected using a cross-sectional survey and later analyzed using descriptive and inferential statistics. Because there was a need to explain some quantitative data (reasons for participants’ disclosure and non-disclosure of HIV serostatus to sexual partners), there was a purposeful selection of participants to provide qualitative data through in-depth interviews. Later, there was coding and thematic analysis of textual data. Thereafter, there was the integration of quantitative and qualitative results through interpretation and explanation and provision of implications for future research. Figure 1 shows the flow chart of the Explanatory sequential design.
 |
Figure 1 Flow chart of explanatory sequential mixed methods design. |
Quantitative data were collected between May 2019 and July 2019 while qualitative data were collected between February 2020 and March 2020. Ethical approval was obtained from the Mildmay Uganda Research Ethics Committee (MUREC) an affiliate of Uganda’s National Council for Science and Technology.26
Sample Size Estimation for Quantitative Methods
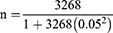
The seven districts, 21 health facilities, and 357 study participants were selected using multi-level sampling. The seven districts and 21 public health facilities were randomly selected while the study participants were conveniently selected. The selection criteria of the study participants were based on: sexually active young people aged 15–24 years old that had turned up for ART services on the day of data collection and were on ART for 12 months and above; in a sexual relationship for the past 6 months and above and provided informed consent, were enrolled for the study. The researcher used Israel’s (1992) formula to determine the sample size. According to the Baseline Assessment of Access to HIV Testing, Care, and Treatment among Adolescents in Uganda,17 the estimated number of young people receiving ART in Central Region 1 was 3268. After establishing the population size, the researchers established the Margin of Error or Confidence Interval which is 0.05. A sample size of 356 was calculated using the Israel formula.27
Where;
n=Sample Size.
Size of the Target Population (which is 3268).
e=Margin Error/Level of Precision (which is 0.05).
The initial study selected 357 participants, however, 238 (66.7%) participants who were sexually active, was considered for this study.
Sample Size Estimation for Qualitative Data
The researchers targeted six5 participants from each participating district to give a total of 42 young people on ART. The purposive sampling method was used to select the participants. The required 42 participants were selected among the 238 considered for this study, to explain their HIV serostatus disclosure to their sexual partners. However, by third district data collection, 18 (males=9; females=9) participants, there was already data saturation. The three districts included Luwero, Mityana, and Wakiso.
Quantitative Data Collection
Before collecting quantitative data, the researchers pre-tested the questionnaire to enhance its validity and reliability. The pre-test process took a sample of 20 participants, who were non-school-going young people receiving ART at the Mildmay Uganda Hospital. Lessons from the pre-test process aided the amendment of the questionnaire. Of the 357 study participants in the initial study, 350 consented, making a response rate of 98%. Those who did not consent to participate in the study said that they had no time to complete the questionnaire. Some were concerned that their participation would infringe on their privacy, while others wanted some sort of reward to participate in the study. The data collection tool had 75 questions, which took between 50 to 70 minutes. Some questionnaires were self-administered (for those participants who wanted to do it themselves) while others were interviewer-administered (for those who were uncomfortable with willing the questionnaire themselves). The data collection tool was both in English and Luganda—a local language (which is widely spoken in the Central region), to a better expression of the study participants. Data collection took four weeks, as one day was assigned to the ART clinic in most facilities. Data for the 238 participants were analyzed for this study.
Qualitative Data Collection
The young people that participated in the data collection were conveniently selected from those that had turned up for the routine clinic visits. The interviews were conducted at the most convenient time on the day the respondent visited the health facility. This was done to enable the study participants to speak freely about their HIV serostatus disclosure to their sexual partners. Written consent was obtained from the study participants before data collection.
For confidentiality, face-to-face in-depth interviews were conducted from a private room at the health facility. Data were collected by five selected health workers (one from each public health facility) where study participants were drawn. The health workers were graduates with a degree qualification in Counselling. Before data collection, the lead researcher empowered them with competencies in conducting in-depth interviews.
The in-depth interview face-to-face guide explored the respondent’s biodata (that included age, sex, occupation, education level, source of HIV infection and period on ART, and whether the respondent stays with the sexual partner or not) and the reason(s) for disclosure or non-disclosure of HIV serostatus to the sexual partner.
The in-depth interviews were conducted in the Luganda language, the one predominantly spoken by the people in the Central region of Uganda, which was the study setting. The interviews were audio-recorded on a smartphone after obtaining consent from the respondent. The interview took an average of ten minutes. The in-depth interview guide was first piloted and later enriched thereafter before the subsequent interviews. The data that was collected in the pilot phase of the in-depth interviews were also included in the data analysis.
Study Measurement
Table 1 shows the variables included in this study.
 |
Table 1 Study Variables |
Management of Quantitative Data
Hard-copy questionnaires were used to collect data. The researcher entered this data into an electronic database. The database was amended to accommodate the responses categories, as elaborated in Table 1. This data-cleaning process aided the proper summarization of data in frequencies and percentages. The association of HIV serostatus disclosure and non-disclosure to sexual partners was done using bivariate analysis. Thereafter, multinomial logistic regression was done to classify study respondents based on values of a set of predictor variables. Variation inflation factor (VIF) was used to check for multicollinearity of the variables included in the regression model as in Figure 2. The VIF of 1.12 indicated that the variables included in the regression model were not correlated, thus the model was appropriate.
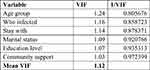 |
Figure 2 Multicollinearity check. |
Management of Qualitative Data
After data collection, research assistants (health workers) shared the audio-recorded interviews with the lead researcher who also shared them with the co-researchers. We listened to the audio interviews to check for consistency before sharing them with the translator. Thereafter, the interviews were shared with the independent translator for verbatim transcription and translation from Luganda to the English language. The translator shared the transcripts with the lead researcher who listened to and read the transcripts. The lead researcher shared the transcripts with the co-researcher to listen to and read the transcripts too. After listening to and reading the transcripts case by case, independently, the researchers confirmed that the transcripts are consistent with the data collected. The audio recordings and soft copies of the transcripts were saved on the researchers’ computers in file names only known to the researchers.
Analysis of Qualitative Data
The researchers utilized the five-step thematic content analysis approach to analyze the data.28,29 Firstly, the lead researcher familiarized himself with the data to make sense of the written and audio interview transcripts, case by case. Secondly, the lead researcher highlighted the phrases and sentences that described the study participants’ reasons for disclosure or non-disclosure of their HIV serostatus to sexual partners. Codes were assigned to those themes that looked similar. Thirdly, the researcher grouped and merged codes that had similar meanings or messages and they were respectively given themes. Fourthly, the researcher reviewed the codes to ensure they produce an accurate representation of the data. This was done by again listening to the case in the audio interview. Lastly, the succinct themes were generated to help understand the study participants’ reasons for disclosure or non-disclosure of their HIV serostatus to their sexual partners.
Thereafter, the lead researcher shared the data with the co-researcher who read the details of the analysis summary. Later, we came to a consensus on the easily understandable themes and codes to represent the data in the respective cases of study participants. The themes for the qualitative data on the reasons for disclosure included: prevent causing trauma to the partner, prevent to be dropped or abandoned, fear of being stigmatized, and desire to continue accessing basic needs (poverty); while the themes for non-disclosure included: got tired of pretending or being secretive and desire to adhere to ART.
Results
This section presents findings from the analysis of quantitative and qualitative data respectively. Quantitative data was collected and analyzed first and later the researchers collected qualitative data to help explain some quantitative data.
Results for Quantitative Data
Demographics of Study Participants
Of the 238 study participants, the majority (64.3%) were aged 20–24 years, while the rest were 15–19 years. The Majority (82.8%) of the study participants were female. Only 10.1%23 had no education while 39.1% (n=93) had primary education and 50.8% (n=121) had secondary education. Of the study participants who lived with their parents 32.4%, 29.0% of study participants stayed with their partners, 17.7% stayed with their relatives, and 21.0% stayed alone. More than half (56.3%) of the study participants were unemployed, and more than half of the study participants (55.0%) were unmarried. Most of the study participants (65.6%) had been on ART for 1–4 years, while the least number (16.8%) had been on ART for 5–9 years. The majority of the respondents (58.0%) reported having been infected by their partners, 29.8% of the study participants reported having been infected by their mothers at birth, while only 12.2% had been infected in other ways. Most (79.4%) study participants had only one partner, while the others had more than one partner. The majority of the study participants (96.6%) had high knowledge of disclosure, though 80.7% had positive attitudes toward disclosure and 79.8% had the right beliefs on disclosure. Other details on the socio-demographic characteristics of study participants are included in Table 2.
 |
Table 2 Socio-Demographic Characteristics of Study Participants |
Study participants that perceived service delivery to be good were 95.8%. Likewise, the majority of the study participants (92.9%) affirmed that the human resources at the health facilities were sufficient. About 70.6% of the study participants considered to have high levels of health education for the health facilities and 72.3% had a supportive community.
Almost half (48.7%) had two-way disclosure where each partner had disclosed their HIV serostatus to their sexual partner while 24.4% of the study participants had one-way disclosure where the study participants knew their partners’ status and their partners did not know. For the study participants who had not disclosed to one another were 26.9%.
Association Between Disclosure and Non-Disclosure with Various Factors
At the bivariate level (Table 3) age group, education level, staying with parents or relative or partner or alone, marital status, source of infection, and community support were significantly (p<0.05) associated with serostatus disclosure. These variables were noted with asterisks. While; sex, religion, employment status, residence, time on ART, number of sexual partners, knowledge of disclosure, attitudes on disclosure, belief on disclosure, the service delivery of SRHR services, human resources factors, and health education factors were not significant (p≥ 0.05) related to disclosure. Significant variables at bivariate levels were included in the multivariable model as shown in Table 3.
 |
Table 3 Association Between Disclosure and Non-Disclosure with Various Factors (Bivariate Analysis) |
Multinomial Logistic Regression for Factors Associated with Disclosure and Non-Disclosure of HIV Serostatus to Sexual Partners
Multinomial logistic regression analysis (as shown in Table 4) pointed out that the study participants who had contracted HIV from their partners were significantly (p=0.031) associated with one-way disclosure compared to no disclosure. Respondents who contracted HIV from their partners were almost three times more likely (RRR=2.752; 95% CI: 1.100–6.888) to have one-way disclosure than no disclosure, compared to those who had been infected by their mothers. Likewise, study participants who were perinatally infected were significantly (p=0.034) associated with two-way disclosure compared to no disclosure. The study participants who contracted HIV from their partners were twice more likely (RRR=2.357; 95% CI: 1.065–5.214) to have two-way disclosure than no disclosure, compared to those who had been infected by their mothers. Similar analysis indicated that study participants staying with their partners were significantly (p=0.029) associated with two-way disclosure compared to no disclosure. Study participants who stayed with their partners were almost four times more likely (RRR=3.869; 95% CI: 1.146–13.060) to have two-way disclosure than no disclosure, compared to those who stayed with their parents.
 |
Table 4 Multinomial Logistic Regression for Factors Associated with Disclosure and Non-Disclosure of HIV Serostatus to Sexual Partners |
Results for Qualitative Data
Socio-Demographic Characteristics of Study Participants
A total of 18 (Males=9; Females=9) participants aged 15–24 years, participated in the in-depth interviews. The average age of study participants was 20 (range 15–24 years) whereas most participants (n=12) were aged 20–24 years. A total of 8 participants were staying with their sexual partners, 8 with their relatives/parents and 3 were staying alone. A total of 16 (7 Males; 9 Females) participants, were committed to one sexual partner at the time of the interview, where 10 (Males=5; Females=5) participants had disclosed their HIV serostatus to sexual partners and 06 (Males=2; Females=4) participants had not disclosed their HIV serostatus to sexual partners.
Two (both males) participants were in multiple concurrent sexual relationships, one with 4 and another with 5 sexual partners. The one with four had not disclosed to any, while the one with five had disclosed to only one, at the time of the interview. The number (n=9) of participants with multiple sexual partners was equal to those8 with one sexual partner. Of the participants who had one sexual partner, six of them (the majority) had disclosed their HIV serostatus to their sexual partners. While six of the participants who had multiple sexual partners had not disclosed their serostatus to their sexual partners. This indicated higher levels of disclosure among participants with one sexual partner.
Worth noting, of the nine8 female study participants, two were pregnant and had disclosed their serostatus to sexual partners. Eight (Males=4; Females=4) study participants were staying with their sexual partners and 8 (Males=3; Females=5) who were staying with their relatives/parents, had casual sexual partners. The two participants who were staying alone were in casual sexual relationships and it is these two engaged in multiple concurrent sexual relationships. More details socio-demographic factors of study participants that participated in in-depth interviews are included in Table 5.
 |
Table 5 Socio-Demographic Characteristics of Participants Interviewed |
Following the analysis of quantitative data on the factors associated with HIV serostatus disclosure and non-disclosure among sexually active young people on ART in Central Uganda, we considered it fit to go further to collect qualitative data to provide the reasons for disclosure and non-disclosure of their to their HIV status to sexual partners.
Reasons for Disclosure of HIV Serostatus to Sexual Partners Among Young People on ART
Table 5, indicates that, out of the 18 participants, 10 had disclosed their HIV status to sexual partners by the time of data collection. Several reasons were provided by study participants from which two broad qualitative themes, which we believe thoroughly explain the reason for HIV serostatus disclosure, were generated. The themes include: 1) getting tired of pretending and being secretive; and 2) the desire to adhere to ART. Table 6 shows how the themes for the reasons for disclosure, were generated.
 |
Table 6 Codes and Theme Allocation for Reasons for HIV Serostatus Disclosure |
Theme 1: I Got Tired of Pretending/Being Secretive
Regardless of their sex, several participants in this study noted that they decided to disclose their HIV serostatus to their sexual partners because they were tired of being secretive about taking their HIV medicines. Others had pretended for a long time. At first, they were successful in hiding their medicines in a way that their partners could not see them taking them. Consequently, because this practice of hiding medicines proved unsustainable, especially for those who were staying with their partners, they decided to disclose their status. One of the partners noted:
I realized that telling her a lie cannot help and I could not sustain a lie forever. I reflected upon this and I (later) told her that I am going to tell you (the truth), but will you continue loving me? She insisted that she wanted to know if I was (HIV) negative or positive… and I told her the truth that I am (HIV) positive. She said that it is what she wanted to know. (A male, 21 years).
Similarly, another participant disclosed that she was tired of being secretive about taking his HIV medicines. In addition, some never wanted their sexual partners to land on medicine before disclosure since this could result in unbearable consequences in the relationship. The quotations below support this finding.
I disclosed this because I was tired of being secretive whenever I visited my partner. The hours I had to take my medicine would always coincide with the time of the meeting. I reflected that if my partner came to find out by himself that I am on ART, it would lead to him dropping me and he would be annoyed with me forever. So, I got time and disclosed as being secretive cannot last forever. (A female, 24 years)
One time, I faced a challenge due to being secretive about my medicine. At times, I would miss taking my medicine especially when I happened to be with her and feared her seeing me taking the medicine. I felt guilty always. One day, I decided and disclosed to her the support you had provided to me before. One time, after dinner, I explained to her. The fact is that it was a hard experience but I disclosed it to her. I first tested her and asked her whether she would not drop me if I tell her this bad news and thereafter I disclosed to her that I have and I am on ART. The truth is, it was a hard experience. (A male, 21 years)
One of the study participants who disclosed the sexual noted that she did so because she loved her partner and believed that, individuals who are committed to one sexual partner should be open to one another at all times. Hiding a secret from the one you love is not fair. Good or bad times, serious lovers should stay together. Based on that belief, incidentally, they decided to disclose their serostatus to their sexual partners. One of the study participants stated:
One time, he came here for an HIV test and was found (HIV) negative. After he returned home, he told me his status and asked me to go for an HIV test. My results were positive. I was given ARVs and I showed them to him when I returned home and he said he has no problem. But, after three months, he went for a repeat (HIV) test and turned out (HIV) positive. He was given ARVs. He assured me that he will not drop me. (A female, 22 years)
I believe a serious partner should love you in good and bad times. That is the reason I decided to disclose to him. (A female, 21 years)
Similarly, another participant said:
…. after the hospital, he asked me how I got HIV. I told him, I was born with it. I explained to him but he told me that, for him, he still loves me. The time came when he wanted to marry me. He informed his parents. His mother had no problem but, the dad refused the marriage issue. Though my partner seriously loved me. (A female, 21 years)
Theme 2: Desire to Adhere to Anti-Retroviral Medicine
The need to adhere to the rules of anti-retroviral medicines influenced many study participants to disclose their HIV serostatus to sexual partners. Before the disclosure, they were aware that they were behaving contrary to what health workers used to tell them about adherence. Missing to take medicines at the right time was a common occurrence, especially when the time to take their medicines coincided with that of meeting their sexual partners. At such a point, it was equally hard for many to secretly take their medicines as scheduled. After some time, most study participants realized this was not good for their life and so, they decided to disclose their HIV serostatus to sexual partners. This is supported by the following quotations:
I was tired of taking my ARV secretly. In the first instance, after being initiated on ART, I used to take my medicine on time. Later, whenever my time to take medicine got him around, I could miss my dose since I did not want him to see me taking medicine. Later, health workers empowered me and guided me on how to disclose. (A female, 21 years)
I was tired of being secretive when it comes to taking my medicine. I was not adhering to medicine well. And at times he could invite me to visit him any time. At times I could go with the tabs and I could fail to swallow the medicine for fear of being seen. At times I would be restless since he would check my bag anytime. (A female, 20 years)
At times, I would miss taking my medicine especially when I happened to be with her. One day, I decided to disclose to her. (A male, 21 years)
I was not adhering to medicine well. At times, he would invite me to visit him anytime. At times, I would go with tablets (ARVs) and I would fail to take them for fear of being seen. At times. I would be restless since he would check my bag. So, I started taking medicine (ARVs) poorly. (A female, 22 years)
Other participants who disclosed interviewed stated that they disclosed because keeping or storing medicine the right way as advised by health workers, was increasingly becoming a challenge and it would result in many dangers.
Health workers used to emphasize to us to keep medicines very well. Keeping medicine was a challenge. I used to keep it in the kitchen. At times in the garden. Later, I saw this causing me many difficulties. One time I shared my experience with the Counsellor and I got helped to disclose it.
Reasons for Non-Disclosure of HIV Serostatus to Sexual Partners Among Young People on ART
Out of the 18 participants, 8 had not disclosed their HIV ser-status to sexual partners at the time of the study. Three themes emerged from the analysis of qualitative data for participants’ non-disclosure partners, which include: 1) Fear of being stigmatized; 2) Desire to continue accessing basic needs (poverty); and 3) Preventing causing trauma to sexual partners. Table 7 shows how the themes of the reasons for the non-disclosure of HIV serostatus were derived.
 |
Table 7 Codes and Theme Allocation for Reasons for Non-Disclosure of HIV Serostatus |
Theme 1: Fear of Stigma and Discrimination
This was one of the major barriers to non-disclosure of HIV serostatus among most study participants who were not disclosed at the time of data collection. All the participants were aware of the benefits of disclosure but they chose not to disclose due to several reasons. Irrespective of the sex of participants, many had not disclosed it because they feared being dropped by their sexual partners. Some had been in sexual relationships before and were dropped off after their partners got to know they were HIV positive. So, after entering into another relationship, they had to conceal their HIV serostatus for fear of facing the same old consequences.
I have even more than one (sexual partner). About five. Long ago, I disclosed to one but later parted ways. One of the five is not on ART. For her, she knows I have HIV. Others, I have never disclosed this to them. One of them said she could not love a person who is HIV positive. I felt bad. Later, I asked myself; for we who are HIV positive, cannot have (love) those who are HIV negative? I later observed that, when a lover gets to know you are HIV positive, they abandon you. That girl whom I disclosed when abandoned me, I felt much pain. I was hurt. (A male, 23 years)
Me, I know about disclosure but I have never disclosed my HIV status to my partner. Because for me, I was born with HIV and I know about the issue of taking ARVs as per health workers’ instructions. But, the current coincidence is that my girlfriend loves me and she is HIV negative, yet I am HIV positive, but we love each other. (A male, 19 years)
When I talked about HIV issues with my lover, there is a way he responded that was scary. I can end up looking like Satan in his face. One time, he told me he would abandon me in case he gets to know that I have HIV. (A female, 22 years)
… since we live in the same village, I tend to imagine that if I disclose, she could tell her parents she lives with her in the village. (A male, 20 years)
On top of fearing being dropped by the sexual partner after knowing their HIV-positive status, some believed that the one who has dropped them could spread information in the community, which would spoil their image further. So, some dared not to disclose for fear of the possible consequences. Other participants noted:
… since we live in the same village (with the partner), I tend to imagine that if I disclose, she could tell her parents. I do not want them to start blaming me. (A male, 20 years)
Because she is still a girlfriend, any time, you might part ways. So if you already disclosed, that partner can disclose the information to other girls some can be your friends and this can result in stigma (A male, 19 years).
Qualitative results indicate that most participants who were in casual sexual relationships were less likely to disclose their HIV serostatus because of the limited commitment characterized by most casual sexual relationships. Some participants noted a sexual partner could drop you yet you disclosed your status and this disclosure may work against you in the future. Some of the quotations supporting this thinking are as follows:
He is not my future husband. I would disclose to my lifetime partner, not these boyfriends. Boyfriends can spread information about your HIV status to their peers and this can lead to stigma. This is the reason I have not disclosed this to my (current) partner. I want to disclose this to my lifetime partner instead. This will also enable me to take my medicine well since I will be free, which is not the case with these boyfriends who can spread the information about my status to anyone. (A female, 19 years)
Because she is still a girlfriend, any time, you might part ways. So if you already disclosed, that partner can disclose the information to other girls some can be your friends and this can result in stigma. (A male, 19 years)
Theme 2: Desire to Continue Accessing Basic Needs (Poverty)
The desire for some study participants to continue receiving assistance from their sexual partners influenced some study participants, especially the females, to disclose their HIV serostatus to sexual partners. They believed that, if the sexual partner got to know that one is HIV positive, he could easily support them, especially financially. One of the participants said:
The first thing, he is the person taking care of me. So, what if I tell him that, I am HIV positive and he drops me? Who will take care of me? What will I do? He is my provider. (A female, 22 years)
Theme 3: Prevent Causing Trauma to a Sexual Partner
Some participants decided not to disclose because they never wanted to traumatize their sexual partners with the scary news of being HIV positive. So, this too hindered some from disclosing their HIV status.
“She is still studying. I cannot tell her because I am not sure of how she is likely to react to the (bad) news.” A male respondent does not even know the HIV status of his sexual partner. (A male, 19 years)
For me, I make sure that I take my medicine well. Secondly, when we get into love issues, I make sure that I use a condom. I do that to keep her safe. The reason why I have not disclosed this to her is that she can get trauma. (A male, 19 years)
Discussion
This study intended to understand the factors associated with HIV serostatus disclosure to sexual partners among sexually active young people on ART and the reasons for disclosure and non-disclosure of the HIV serostatus. Our discussion is based on the major outcomes that were significant in the findings of this study. The findings revealed that the proportion of participants who had disclosed their status was 73.1%, of which two-way disclosure was 48.7% and one-way disclosure was 24.4%. Relatedly, results from qualitative data indicate that 55.5% of study participants disclosed their HIV serostatus to sexual partners. Our findings are slightly consistent with the study done in Ethiopia where disclosure of HIV serostatus to a sexual partner was 92.6% (95%, CI = 90–95%),30 and another one in Zimbabwe where 93% of the study participants disclosed their status,31 and one in Uganda where 73.3% had disclosed32 to sexual partners. However, most studies, unlike ours, disclosure was one-way33 while other studies mainly focused on people living with HIV not necessarily on ART30,34 except the study in Haiti where 75.2% of the study participants were on ART.35 Some studies had smaller sample sizes like the Ugandan study by Ngonzi et al36 which had 103 participants, the Malawian study by Hino et al33 which had 40 participants and another Ugandan study by Atwijukiire et al,34 with 12 participants compared to our study. Worth noting, the average age of study participants in the Malawian study33 was 28 years while in the study in Haiti,35 the participants’ average age was 35 years. We regarded it very important to focus on the young population since it is mainly the world’s window of hope thus the study findings would greatly influence the HIV care services for this population.
Worth noting, the studies done in Malawi,33 Uganda,36 and Haiti37 were either qualitative or quantitative yet ours combined both quantitative and qualitative approaches. Our study did not only want to provide the frequency of disclosure and non-disclosure but also wanted to provide an in-depth explanation of disclosure and non-disclosure in a variety of contexts hence maximizing the strengths of data type (quantitative and qualitative) which facilitates a more comprehensive understanding of disclosure in HIV prevention and care.38
The study outcomes of quantitative data indicate that study participants that were staying with their sexual partners were almost four times (CI:95%[1.146–13.060]) more likely to disclose their serostatus to their sexual partners compared to those who were staying with their relatives or parents (CI:95%: 1.017[0.391–2.643]) and those who were staying alone (CI:95%: 1.246[0.464–3.346]). Similarly, qualitative findings revealed that all participants who were staying with sexual partners had disclosed their serostatus to their sexual partners. Our findings are generally in tandem with the Malawian study by Shifraew et al;30 the Ethiopian study by Shifraew et al,30,39 a Nigerian study by Yaya et al,40 and Ugandan studies by Atwijukire et al,34 and Naigino et al,32 where a big number of study participants who were staying with their partners had disclosed their HIV serostatus to their partners. The findings from the in-depth interviews indicate that several factors influenced HIV serostatus disclosure to sexual partners among study participants. The desire to express commitment in the sexual relationship, the desire to encourage their partner to get tested for HIV, the desire to prevent HIV transmission to the unborn baby following the sensitization from health workers to pregnant females, the desire for peace in a relationship influenced most participants to disclose to their sexual partners. Health workers at all levels should continue promoting adherence among young people on ART and sensitization of sexually active young people on ART about the benefits of sticking to one sexual partner and the risks involved in multiple sexual relationships especially where the partners do not know each other’s HIV serostatus.
On the other hand, the analysis of quantitative data further revealed that there were participants 26.9% who were in a sexual relationship but never disclosed their HIV serostatus to sexual partners, just like the qualitative data showed 44% had not disclosed to their sexual partners. Our findings are generally in agreement with the study. These findings conform with studies in Ethiopia,30,41 and Zimbabwe31 though the percentage of those that had not disclosed to their sexual partners was around 10% among the study participants. However, in Tanzania,11,12 Ethiopia,42 and Ugandan studies,32,36 the percentage of study participants that had not disclosed to their sexual partners was over 20%, just like the case with our study. Possibly this could be explained by the fact that the study contexts (Uganda and Tanzania) are almost the same. The reasons provided for non-disclosure were fear of adverse events like stigma and discrimination and violence. Slightly similar reasons were provided by participants in our study.
Other explanations provided by our study participants for non-disclosure to sexual partners were: fear to traumatize the sexual partner with shocking or bad news; the desire to continue receiving monetary support from the partner (especially by female partners), fear to break the sexual relationship and being in a relationship with a casual sex partner. Even though the biology of fear and anxiety are common in human beings and indeed normal (that would eventually prevent some from disclosing their HIV serostatus,43,44 psychosocial support services are critical here for such people since the costs of fear far outweigh the benefits. Similarly, the desire to continue receiving support to access basic needs is a barrier to disclosure whose underlying cause is poverty, this implies that economic empowerment should be promoted and strengthened since greatly contributes to the prevention of HIV transmission, especially among vulnerable populations like the young people45–47 and so appropriate sexual and reproductive health strategies should be employed to address this risky practice.
The study findings show that partners who got HIV from sexual partners are two times (CI:95%:2.357[1.065–5.214]) more likely to disclose their HIV status to sexual partners compared to those who were perinatally infected. Unfortunately, studies about the disclosure of HIV serostatus to sexual partners among perinatally infected young people are hardly available. Disclosure of HIV status to a sexual partner can lead to both positive and negative results though, in the context of HIV management, the benefits outweigh the costs. There is a need to strengthen interventions promoting HIV serostatus disclosure among sexual partners like assisted partner notification, peer support groups, and continuous education of the public about the benefits of disclosure to reduce the barriers to disclosure.
Study Limitations
During the collection of quantitative and qualitative data, this study relied on self-reporting by study participants. The researchers could not ascertain the truth in the response of whether participants were two-way honest in their responses to disclosure or non-disclosure of their HIV status to sexual partners. Despite the limitations, the study findings provide evidence for HIV prevention, care, and treatment interventions among sexually active young people on ART.
Conclusions
The study findings emphasize the role of HIV serostatus disclosure to a sexual partner in the attainment of the goals of antiretroviral therapy that intends to reduce HIV transmission, reduction of morbidity, and mortality, particularly among the sexually active population. Prevention of HIV transmission between sexual partners in a situation where one is HIV negative or prevention of HIV reinfection where both are HIV positive is possible in case disclosure is practiced. HIV self-disclosure to sexual partners can as well greatly contribute to the virtual elimination of mother-to-child transmission of HIV in case HIV-positive pregnant women are appropriately empowered by health workers on how they can do it in their sexual relationships. Similarly, disclosure of HIV status to a sexual partner can potentially contribute to the attainment of the 3-Zeros (zero new HIV infection, zero stigma and discrimination, and zero-HIV related deaths) that are a center of focus in ending HIV by 2030.
Abbreviations
HIV, Human Immunodeficiency Virus; ART, Antiretroviral Therapy; ARV, Antiretrovirals; CI, Confidence Interval; RRR, Relative Risk Ratio; SRHR, Sexual Reproductive Health and Rights.
Data Sharing Statement
The corresponding author will share the data set in this study upon reasonable request.
Ethics Approval and Consent to Participate
The study was conducted following the internationally accepted standards as enshrined in the 1964 Declaration of Helsinki.48 Mildmay Uganda Research Ethics Committee (REF 0303-2019), an accredited Ethics research body by the Uganda National Council of Science and Technology (UNCST), approved the study protocol. After obtaining ethical clearance, the lead researcher presented it to the District Health Officers, Hospital administrators, and managers, where study participants were drawn. Thereafter, written informed consent was obtained from all study participants. Participants who were aged 15–17 years, were considered to be mature minors and provided informed consent independent of parents. The UNCST recognizes that human participants within the age range of 14–17 years old are mature minors if they have a sexually transmitted infection (STI) and they are allowed to provide independent consent if there is justification for not involving parents.49 The study participants had HIV, which is an STI, and it was justified not to involve their parents to preserve their confidentiality concerning their HIV-positive serostatus disclosure to sexual partners.
Acknowledgments
We extend our sincere gratitude to study participants, research assistants, Mildmay Uganda Research Ethics Committee, District Health Officers, Hospital administrators and managers, and health workers from those districts and hospitals where the study was conducted.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest.
References
1. Gabbidon K, Chenneville T, Peless T, Sheared-Evans S. Self-disclosure of HIV status among youth living with HIV: a global systematic review. AIDS Behav. 2020;24(1):114–141. doi:10.1007/s10461-019-02478-9
2. Evangeli M, Foster C. Who, then what? The need for interventions to help young people with perinatally acquired HIV disclose their HIV status to others. AIDS. 2014;28(SUPPL. 3):1–11. doi:10.1097/QAD.0000000000000334
3. Melis Berhe T, Lemma L, Alemayehu A, Ajema D, Glagn M, Dessu S. HIV-positive status disclosure and associated factors among HIV-positive adult patients attending art clinics at public health facilities of Butajira Town, Southern Ethiopia. AIDS Res Treat. 2020;2020. doi:10.1155/2020/7165423
4. International C, Agency D. Counselling guidelines on disclosure of HIV status; 2004:1–23.
5. Ministry of Health. Consolidated guidelines for prevention and treatment of HIV and AIDS in Uganda; 2020. Available from: http://library.health.go.ug/publications/hivaids/consolidated-guidelines-prevention-and-treatment-hiv-uganda.
6. Steinert JI, Cluver L, Melendez-Torres GJ, et al; Nations U, Programme, D, United Nations Development Programme. Cash transfers and HIV prevention. Glob Public Health. 2017;21:55–65.
7. UNAIDS. Turning point for Africa — an historic opportunity to end AIDS as a public health threat by 2030 and launch a new era of sustainability; 2018:16.
8. Health MOF. The Republic of Uganda Ministry of Health Health Sector; 2019.
9. Ndyanabangi B, Kipp W, Diesfeld H. Reproductive health behaviour among in-school and out-of-school youth in Kabarole District, Uganda. Afr J Reprod Health. 2004;8(3):55. doi:10.2307/3583393
10. UNAIDS. 2008 UNAIDS Annual Report: Towards Universal Access. UNAIDS; 2009.
11. Sanga E, Nampewo Z, PrayGod G, Wringe A. HIV positive status disclosure to sexual partners: a qualitative study to explore experiences and challenges among clients attending HIV care services in North-Western Tanzania. AIDS Care. 2021;1:1–8. doi:10.1080/09540121.2021.2012555
12. Damian DJ, Ngahatilwa D, Fadhili H, et al. Factors associated with HIV status disclosure to partners and its outcomes among HIV-positive women attending care and treatment clinics at Kilimanjaro region, Tanzania. PLoS One. 2019;14(3):1–13. doi:10.1371/journal.pone.0211921
13. Walcott MM, Hatcher AM, Kwena Z, Turan JM. Facilitating HIV status disclosure for pregnant women and partners in rural Kenya: a qualitative study. BMC Public Health. 2013;13(1). doi:10.1186/1471-2458-13-1115
14. Asio J, Watera C, Namuwenge N, et al. Population-based monitoring of HIV drug resistance early warning indicators in Uganda: a nationally representative survey following revised WHO recommendations. PLoS One. 2020;15(4):1–15. doi:10.1371/journal.pone.0230451
15. Kavuma D, Ndibazza J, Kirwana VB, Katongole SP, Baluku JB. Factors associated with condom use among out-of-school young people on anti-retroviral therapy in central Uganda. HIV/AIDS. 2022;14:217–230. doi:10.2147/HIV.S357535
16. Kiula ES, Damian DJ, Msuya SE. Predictors of HIV serostatus disclosure to partners among HIV-positive pregnant women in Morogoro, Tanzania. BMC Public Health. 2013;13(1). doi:10.1186/1471-2458-13-433
17. GAC. National HIV and AIDS strategic plan; 2016:1–8.
18. National HIV and AIDS Priority Action Plan 2020/2021- 2022/2023: Ending the HIV and AIDS epidemic: Communities at the forefront: Kampala: Uganda AIDS Commission; 2020.
19. The_Hiv_and_Aids_Prevention_and_Control_Act_2014_Signed_By_the_President.Pdf. Available from: https://www.ilo.org/dyn/natlex/natlex4.detail?p_isn=110805&p_lang=en.
20. Uganda Ministry of Health. Uganda population-based HIV impact assessment (UPHIA) 2016–2017. United States Dep Heal Hum Serv; 2019:252. Available from: https://phia.icap.columbia.edu/wp-content/uploads/2019/07/UPHIA_Final_Report_Revise_07.11.2019_Final_for-web.pdf.
21. Joint United Nations Programme on HIV/AIDS (UNAIDS). In UNAIDS Global AIDS Update 2022 Danger. Joint United Nations Programme on HIV/AIDS; 2022.
22. UNAIDS. Political declaration on HIV and AIDS: ending inequalities and getting on track to end AIDS by 2030. United Nations General Assembly. UNAIDS; 2021:1–28. Available from: https://www.unaids.org/sites/default/files/media_asset/2021_political-declaration-on-hiv-and-aids_en.pdf.
23. Ivankova NV, Creswell JW, Stick SL. Using mixed-methods sequential explanatory design: from theory to practice. Field Methods. 2006;18(1):3–20. doi:10.1177/1525822X05282260
24. Subedi D. Explanatory sequential mixed method design as the third research community of knowledge claim. Am J Educ Res. 2016;4:570–577.
25. Cameron R. A sequential mixed model research design: design, analytical and display issues. Int J Mult Res Approaches. 2009;3(2):140–152. doi:10.5172/mra.3.2.140
26. Masafumi A. No covariance structural analysis of health-related indices in the elderly at home with a focus on subjective feelings of healthTitle. Carbohydr Polym. 2019;6(1):5–10.
27. Polonia G. Analysis of sample size in consumer surveys analysis of sample size in consumer surveys, GfK Polonia 2; 2013:7–10.
28. Braun V, Clarke V. Thematic analysis; 2012:2.
29. Clarke V, Braun V. Thematic analysis. J Posit Psychol. 2017;12(3):297–298. doi:10.1080/17439760.2016.1262613
30. Shifraew MB, Shiferaew MT, Mitiku HZ, Ayalew AF. HIV-positive status disclosure to sexual partner and associated factors among adult HIV-positive patients in debre markos town, 2019. HIV/AIDS Res Palliat Care. 2021;13:571–579. doi:10.2147/HIV.S293017
31. Shamu S, Zarowsky C, Shefer T, Temmerman M, Abrahams N. Intimate partner violence after disclosure of HIV test results among pregnant women in Harare, Zimbabwe. PLoS One. 2014;9(10). doi:10.1371/journal.pone.0109447
32. Naigino R, Makumbi F, Mukose A, et al. HIV status disclosure and associated outcomes among pregnant women enrolled in antiretroviral therapy in Uganda: a mixed methods study. Reprod Health. 2017;14(1):1–11.
33. Hino S, Grodensky C, Rutstein SE, et al. HIV status disclosure during acute HIV infection in Malawi. PLoS One. 2018;13(7):1–10. doi:10.1371/journal.pone.0201265
34. Atwijukiire H, Nakidde G, Otwine AT, Kabami J. Experiences of HIV positive serostatus disclosure to sexual partner among individuals in discordant couples in Mbarara City, Southwestern Uganda. HIV/AIDS Res Palliat Care. 2022;14(May):231–242. doi:10.2147/HIV.S361898
35. Shantanam S. Myocardium extract from suckling rat HHS public access. Physiol Behav. 2018;176(1):139–148.
36. Ngonzi J, Mugyenyi G, Kivunike M, et al. Frequency of HIV status disclosure, associated factors and outcomes among HIV positive pregnant women at Mbarara Regional Referral Hospital, Southwestern Uganda. Pan Afr Med J. 2019;32:1–10. doi:10.11604/pamj.2019.32.200.12541
37. Shantanam S. Suckling rat heart muscle extract HHS public access. Physiol Behav. 2018;176(1):139–148.
38. Alasmari N. Mixed methods research: an overview. Int J Soc Sci Hum Res. 2020;03(09). doi:10.47191/ijsshr/v3-i9-04
39. Geremew TD, Nuri RA, Esmael JK. Sero status disclosure to sexual partner and associated factors among adult HIV positive patients in Bale Zone Hospitals, Oromia Region, Ethiopia: institution based cross-sectional study. Open J Epidemiol. 2018;08(02):43–53. doi:10.4236/ojepi.2018.82004
40. Yaya I, Saka B, Landoh DE, et al. HIV-positive status disclosure to sexual partner and associated factors among adult HIV-positive patients in debre markos town, 2019. HIV/AIDS Res Palliat Care. 2019;13(1):1–10.
41. Yaya I, Landoh DE, Saka B, et al. Predictors of adherence to antiretroviral therapy among people living with HIV and AIDS at the regional hospital of Sokodé, Togo. BMC Public Health. 2014;14(1):1–6. doi:10.1186/1471-2458-14-1
42. Genet M, Sebsibie G, Gultie T. Disclosure of HIV seropositive status to sexual partners and its associated factors among patients attending antiretroviral treatment clinic follow up at Mekelle Hospital, Ethiopia: a cross sectional study. BMC Res Notes. 2015;8(1):4–9. doi:10.1186/s13104-015-1056-5
43. Steimer T. The biology of fear- and anxiety-related behaviors. Dialogues Clin Neurosci. 2002;4(3):231–249. doi:10.31887/DCNS.2002.4.3/tsteimer
44. Adolphs R. The biology of fear - review de adolphs 2013.pdf. Curr Biol. 2013;23(2):79–93. doi:10.1016/j.cub.2012.11.055
45. Dvalishvili D, Ssewamala FM, Nabunya P, et al. Multidimensional poverty for adolescents living with HIV (ALWHIV) in Uganda. Public Health. 2022;19. doi:10.3390/ijerph192114326
46. Boyer CB, Greenberg L, Korelitz J, et al. Sexual partner characteristics, relationship type, and HIV risk among a community venue–based sample of urban adolescent and young adult men who have sex with men. Youth Soc. 2019;51(2):219–246. doi:10.1177/0044118X16669259
47. He J. Intimate relationship characteristics as determinants of HIV risk among men who have sex with regular male sex partners: a cross-sectional study in Guangzhou, China. BMC Infect Dis. 2018;18(1):1–12.
48. Declaration T, Code I, Ethics M. Declaration of Helsinki (1964) introduction I. Basic Principles; 1964:1–3.
49. Uganda National Council for Science & Technology. National guidelines for research involving humans as research participants. Uganda National Council for Scince and Technology Kampala-Uganda; 2014.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.