Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 11
Factors associated with adherence to diabetes care recommendations among children and adolescents with type 1 diabetes: a facility-based study in two urban diabetes clinics in Uganda
Authors Kyokunzire C, Matovu N
Received 12 November 2017
Accepted for publication 19 February 2018
Published 29 March 2018 Volume 2018:11 Pages 93—104
DOI https://doi.org/10.2147/DMSO.S156858
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Ming-Hui Zou
Catherine Kyokunzire,1 Nicholas Matovu2,3
1Department of Community Health and Behavioural Sciences, School of Public Health, College of Health Sciences, Makerere University, Kampala, Uganda; 2Department of Community Health, Division of Noncommunicable Diseases, Ministry of Health – Uganda, Kampala, Uganda; 3Global Health Corps Fellowship Program 2017/2018, New York, NY, USA
Purpose: The purpose of this study was to determine the level of adherence and the factors associated with adherence to diabetes care recommendations among type 1 diabetic children and adolescents at two urban diabetes clinics in Kampala, Uganda.
Research design and methods: A facility-based cross-sectional study was carried out among 200 children and adolescents with type 1 diabetes at two major diabetes clinics in Kampala. Caretakers of the children and adolescents were interviewed using pretested questionnaires to provide information on sociodemographic characteristics, diabetes care, knowledge, attitudes, and adherence to diabetes care recommendations in type 1 diabetes. Prevalence rate ratios (PRRs) at the 95% confidence interval (CI) were used to establish the factors associated with adherence using modified Poisson regression, with robust standard errors. The data were analyzed by using STATA Version 13.0.
Results: The overall prevalence of adherence to diabetes care recommendations was at 37%. However, evaluating adherence to specific treatment parameters showed that 52%, 76.5%, and 29.5% of the children and adolescents adhered to insulin, blood glucose monitoring, and dietary recommendations, respectively. In the final adjusted model, active diet monitoring (adjusted PRR [APRR]: 1.95; 95% CI: 1.01, 3.78), being under care of a sibling (APRR: 1.66; 95% CI: 1.61, 1.71), being under care of a married caretaker (APRR: 1.10; 95% CI: 1.05, 1.14) and a separated or divorced caretaker (APRR: 1.60; 95% CI: 1.12, 2.27), taking three or less tests of blood glucose per day (APRR: 0.63; 95% CI: 0.42, 0.95), and having a caretaker with poor knowledge about diabetes (APRR: 0.49; 95% CI: 0.43, 0.57) and who is inactive in supervision of insulin injections (APRR: 0.58; 95% CI: 0.56, 0.60) were associated with adherence to type 1 diabetes care recommendations.
Conclusion: Adherence to type 1 diabetes care recommendations is still low among this population. The results suggest that reinforcing caretaker involvement could be vital in improving adherence to diabetes care recommendations in this population.
Keywords: adherence, type 1 diabetes, Kampala, children, adolescents, Uganda
Corrigendum for this paper has been published
Introduction
There were ~422 million people with diabetes globally in 2014,1 and type 1 diabetes was attributable to 5%–10% of these cases.2 Many of the children and adolescents with type 1 diabetes are from low- and middle-income countries.3 In Africa, type 1 diabetes among children and adolescents contributed to 166,400 cases in 2015, with 7,600 newly diagnosed children each year.4 In Uganda, there is very limited information about the prevalence of type 1 diabetes among children and adolescents although anecdotal data from Mulago National Referral Hospital and Masaka Regional Referral Hospital – which are centers of childhood diabetes management in the central region of Uganda – indicate a rise in type 1 diabetes, which silently accounts for a high morbidity and a high mortality among people aged <18 years.
One of the key dimensions of health care quality and improved disease management is adherence to recommended therapy given by health care workers. The World Health Organization defines adherence as “the extent to which a patient’s behavior – taking medication, following a prescribed diet, and/or executing lifestyle changes – corresponds with agreed recommendations from the health care provider.”5 Notably, children and adolescents with type 1 diabetes face numerous daily challenges associated with adherence to diabetes care recommendations due to the adolescent, child, and family factors – including challenges in adhering to intensive therapeutic insulin regimes (daily injections or pump adjustments), dietary restrictions, regular exercise, and frequent monitoring of biochemical markers.6 In addition, even with the availability of effective treatment, adolescents and children with type 1 diabetes have been reported to have challenges regarding adherence to treatment regimens compared with other age groups with diabetes.7 Certainly, the consequences due to nonadherence to recommendations in type 1 diabetes are concerning and can be potentially life threatening. However, given that some of the previous studies have consistently shown an association between poor adherence and worsening glycemic control,8 there is a critical need to improve adherence to therapy in children and adolescents with type 1 diabetes.
The Uganda Diabetes Association – spearheaded by the Ugandan Ministry of Health in collaboration with its partners and stakeholders – has made efforts in the awareness and prevention of diabetes mellitus through providing information, advise, and support; conducting risk assessments; and early diagnosis of the disease; however, these efforts are highly intensified toward type 2 diabetes with little emphasis on type 1 diabetes. In addition, issues concerning adherence to treatment have not been given critical attention, especially among the youth with type 1 diabetes. In other efforts to improve treatment outcomes among children and adolescents with type 1 diabetes, a program named Changing Diabetes in Children was rolled in 2009 in developing countries including Uganda.9 This program aimed at building the capacity of the health workers and at improving health outcomes of children with diabetes; however, it only focuses on system issues such as provision of diabetes care materials, insulin, and diagnostic equipment and self-care counseling, but does not address any adherence to treatment-related issues, yet this is very important for proper disease management.
Type 1 diabetes patients need to adhere to several treatment parameters such as diet, insulin regimens, and blood glucose monitoring among others specifically because they all contribute to better disease outcomes. Although adherence to type 1 diabetes recommendations has been widely assessed in various studies, most of them assessed adherence incorporating one treatment parameter. For instance, some studies assessed adherence to blood glucose monitoring alone,10 while others assessed diet adherence discretely.11 Given that improved disease management among type 1 diabetes subjects requires combined adherence to several treatment components,12 it is equally important to understand the extent to which type 1 diabetes patients adhere to all treatment parameters. Moreover, adhering to good dietary practices, keeping insulin injection schedules, and regularly monitoring blood glucose have been found very beneficial in improving treatment outcomes in people with diabetes.13
Studies elsewhere that have assessed adherence to single treatment parameter found suboptimal adherence rates, with the proportions of adherence ranging from 39% to 44% for blood glucose monitoring10,14 and between 7.2% and 28% for diet adherence.8,15 A study that assessed adherence to recommendations on three treatment parameters such as insulin, blood glucose monitoring, and diet in Tanzanian type 1 diabetes children and adolescents also found somewhat unsatisfactory adherence levels – with only 68%, 48%, and 28% of them adhering to those recommendations, respectively.8 In Uganda, however, no study has been conducted to ascertain the level of adherence to diabetes care recommendations – especially incorporating these three treatment parameters (blood glucose monitoring, insulin regimen, and diet) among children and adolescents with type 1 diabetes, and therefore, this creates a critical knowledge gap. The aims of this study were therefore to establish the level of adherence to type 1 diabetes care recommendations among children and adolescents and to establish the factors associated with adherence to such recommendations in two urban diabetes clinics in Uganda. Knowing the determinants of adherence to diabetes care recommendations will tailor appropriate interventions to address this issue and to achieve better disease management among children and adolescents with type 1 diabetes.
Research design and methods
Study design and setting
It was a facility-based cross-sectional study among children and adolescents with type 1 diabetes from two urban diabetes clinics in Kampala, the capital of Uganda: Mulago Hospital and St Francis Hospital Nsambya pediatric diabetes clinics. The first one is a part of Mulago Hospital – which is a public and Uganda’s National Referral Hospital and runs its type 1 diabetes clinic on Tuesday every week. The latter is a part of St Francis Hospital Nsambya – which is a private not-for-profit hospital and runs its clinic every Friday on a weekly basis. These two clinics have specialized diabetes staff including diabetologists, medical doctors, diabetes nurses, clinicians, dieticians or nutritionists, and practicing interns who offer type 1 diabetes–related care and support to the children and adolescents. At these clinics, health care providers give specific diabetes care recommendations (for insulin, diet, and blood glucose monitoring) to type 1 diabetes children and adolescents, for which they are urged to routinely follow in order to elicit better treatment outcomes (Supplementary materials). These recommendations depict some of the very important care practices in type 1 diabetes that are widely known. This study therefore assessed adherence to diabetes care recommendations based on clinic-specified recommendations. Noteworthy, clinic-specified diabetes care recommendations were preferred because they are context specific, and all children and adolescents are regularly educated on these recommendations whenever they visit the clinics. These two clinics are attended by people from different regions of Uganda, ie, both urban and rural regions.
Study and target populations
The study population included all children (0–9 years) and adolescents (10–19 years) with type 1 diabetes, attending and obtaining treatment at pediatric diabetes clinics in Kampala. However, our study targeted only children and adolescents with type 1 diabetes attending and receiving treatment at Mulago Hospital and St Francis Hospital Nsambya diabetes clinics between April and July 2017. Only participants (0–17 years) whose caretakers assented and those aged 18 or 19 years who provided informed verbal consent to participate were included in the study. In addition, patients were also included if they had been diagnosed with type 1 diabetes in >12 months from the time of the study interviews. However, patients who were too ill were excluded.
Sample size and sampling procedure
Sample size was calculated based on Daniel’s formula for a finite population.16 Using a standard normal value corresponding to a 95% confidence interval (CI), assuming a margin of error of 5% and a prevalence of the outcome of 28%8 (based on the least expected adherence levels), a sample size of 192 children and adolescents with type 1 diabetes was obtained from a finite population of 500 patients who regularly attended both clinics based on details from the clinic registers. With a 5% rate to account for nonresponse, the overall sample size required for the study was 202 respondents. Each hospital contributed half of the required sample size.
The two diabetes clinics were selected purposively based on patient load and pediatric diabetes specialty. These are the only specialized pediatric diabetes clinics solely focused on the treatment of type 1 diabetes among children and adolescents in Kampala district in Uganda. Sampling of the participants from these two diabetes clinics followed a consecutive approach, where every participant who met the inclusion criteria during the interview time was sampled as they arrived at the clinic until the required sample size was obtained.
Data collection
Interviewer-administered questionnaires were used to collect information from caretakers and adolescents (adolescents responded by themselves if they were not accompanied by their caretakers). Interviewers were two nurses and two nutritionists with a diploma and bachelor’s degree, respectively. The questionnaire had been pretranslated into the local language (Luganda) commonly used in the region, and the interviews lasted on an average of 30–45 minutes per respondent.
Study variables and their measurements
Dependent variable
The dependent variable of the study was “adherence to type 1 diabetes care recommendations”. Adherence to type 1 diabetes care recommendations was assessed under three parameters including insulin adherence, blood glucose monitoring adherence, and diet adherence. Adherence to each of these parameters was individually assessed in the first instance; however, overall adherence was assessed thereafter while integrating all these three. The validity of the questions used to assess adherence to each of the three parameters (insulin, blood glucose, and diet) was measured by the average congruency percentage method17 using a three-rater panel of diabetes experts from the two clinics.
Dietary adherence was assessed by using a set of five questions on the clinics’ recommended dietary practices to find out whether the participant adheres to the specified practice. For every appropriate answer given, which depicted a recommended dietary practice, a participant scored one point up to a maximum of five points. Adherence to recommended diet was found when a participant scored four or more points out of five, and nonadherence was found when they scored below four points out of five.
Insulin adherence: was also assessed by using five questions on recommended insulin practices given by the clinic. Four responses of never (1), sometimes (2), most of the times (3), and always (4) were given, and a participant who answered 1 and 2 scored zero point, while those who answered 3 and 4 scored one point. The maximum score was five, and the participants who scored four or more points were regarded as adherent, while those who scored below four points were regarded as nonadherent.
Blood glucose monitoring adherence: was similarly assessed by using five questions on the recommended blood glucose monitoring–related practices given by the clinics. Such criterion for insulin adherence was used for scoring the four responses and assigning cutoffs.
Computation of overall adherence to recommendations: the three parameters on which adherence to type 1 diabetes care recommendations was assessed altogether yielded 15 questions, with each recommended practice correctly executed by the participant yielding one point up to a maximum of 15 points. The 15 sets of questions yielded a satisfactory reliability to test overall adherence (Cronbach’s α =0.73). The participants who scored 80% (12 out of the 15 points) were regarded “adherent” to the recommendations. Those who scored <12 points were regarded “nonadherent” to the type 1 diabetes care recommendations. A cutoff of 80%–85% has been previously suggested as an appropriate measure.18
Independent variables
The independent variables of the study were the following: sociodemographic variables (age of caretaker and participant, sex of caretaker and participant, family size, caretaker level of education, marital status of caregiver, and age at diagnosis of type 1 diabetes), lifestyle variables (friends and family support), caretaker variables (level of knowledge about diabetes and caretaker involvement in diabetes management tasks), and child diabetes characteristics (glycated hemoglobin [HbA1c], the number of blood glucose tests per day, the number of insulin injections administered per day, alternative medication use, the frequency of insulin stock-out, receipt of diabetes education, and the frequency of missed visits), and they were assessed based on self-reports and by reviewing patients’ diabetes records as appropriate.
Diabetes knowledge: Diabetes knowledge of the caretakers and adolescents was assessed by using 15 questions adapted from the 23-item tool of the Michigan Diabetes Research and Training Center’s brief diabetes knowledge test – which had been previously validated.19 The participants were categorized as having good, medium, or poor knowledge in accordance to the correctly answered questions out of the 15 questions (Supplementary materials).
Caretaker’s involvement in diabetes management–related tasks: was subdivided into two categories: 1) caretaker’s involvement in insulin injection supervision and 2) caretaker’s involvement in diet monitoring. Insulin injection supervision was assessed based on the number of injections supervised or administered by the caregiver out of the total required number in the past 3 days. Caretaker’s involvement in diet monitoring was determined by assessing the involvement of the caretaker in planning the child’s/adolescent’s meals (Supplementary materials).
Attitude toward diabetes: Attitude toward diabetes of adolescents and caregivers was assessed by using the revised version of the Diabetes Attitude Scale based on statements about attitude in only factors five and six of the scale.20,21 These two sections contributed a total of 10 statements that required responses of a 5-point Likert scale such as strongly agree, agree, neutral, disagree, and strongly disagree. The participants were classified as having good, medium, or poor attitude (Supplementary materials).
Data analysis
The data were analyzed by using STATA Version 13.0 (College Station, TX, USA). Background characteristics of the participants were presented as mean and standard deviation for continuous variables and as frequencies and percentages for categorical variables. Results for the background characteristics were also stratified by the sex of the participant. Categorical variables were compared by using Fisher’s exact test, while means of any two groups were compared by using Mann–Whitney U test.
Since we wanted to assess how several factors are associated with adherence to type 1 diabetes care recommendations given to the children and adolescent patients at the clinics, we combined all adherence parameters (such as dietary adherence, insulin adherence, and adherence to blood glucose monitoring) to form one final adherence variable which we used in the model analyses. It is notable that obtaining good treatment outcomes among type 1 diabetes patients requires adherence to all treatment parameters,12 and thus, it is on this basis that we combined all the three parameters to come up with one overall adherence variable.
Factors associated with adherence were established using unadjusted and adjusted prevalence rate ratios (PRRs) at 95% CI with robust standard errors via generalized linear models – using family (Poisson) and link (log),22 while adjusting for the cluster effect of health facility. PRRs were preferred over odds ratios because the latter tend to overestimate the strength of association in scenarios where the outcome of interest is somewhat prevalent.23,24 Covariates with p-value <0.1 at the bivariate analysis were considered for the multivariable model. The final model selection was based on Akaike information criteria (AIC), with smaller AIC values suggesting the better model. Covariates with a p-value <0.05 after multivariable analysis were considered independent predictors of adherence to diabetes care recommendations among type 1 diabetes children and adolescents.
Ethical considerations
Ethical approval from Makerere University School of Public Health Higher Degrees Research and Ethics Committee was sought and obtained. Consent and ethical approval from the hospital administrations and hospital ethics and research review boards were obtained before the research was conducted. Confidentiality of patients’ data was maintained.
Results
The study analyzed a total of 200 children and adolescents with type 1 diabetes who had complete data, of the 202 patients who were enrolled. The proportion of girls was slightly more than that of boys (52.0% vs 48.0%). Girls and boys did not differ in mean age (15.0 vs 15.7 years; p=0.058) and mean HbA1c levels (9.6% vs 9.7%; p=0.945). More than three quarters (161 of 200; 80.5%) of the children and adolescents with type 1 diabetes in this study had poorly controlled blood glucose levels with an HbA1c percentage of >7.5%. Furthermore, boys were diagnosed with diabetes at a significantly older age compared with girls (11.2 years vs 10.0 years; p=0.040). Table 1 summarizes the rest of the results.
Level of adherence to type 1 diabetes care recommendations
The majority of the participants adhered to recommendations of blood glucose monitoring (76.5%), followed by those who adhered to the insulin recommendations (52.0%). However, dietary recommendations had the least adherence from the participants in this study (29.5%). The overall prevalence of adherence was very low at 37.0% (95% CI: 30.3, 43.7; Figure 1).
  | Figure 1 Level of adherence to diabetes care recommendations among children and adolescents with type 1 diabetes. Abbreviations: BG, blood glucose; CI, confidence interval. |
Factors associated with adherence to type 1 diabetes care recommendations
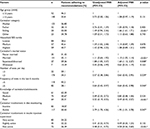
Factors associated with adherence to type 1 diabetes care recommendations are provided as child/adolescent factors in Table 2 and caretaker factors in Table 3.
  | Table 3 Caretaker factors associated with adherence to type 1 diabetes care recommendations Note: *Significant association. Abbreviations: CI, confidence interval; PRR, prevalence rate ratio. |
At bivariate analysis, the child/adolescent factors associated with adherence to the type 1 diabetes care recommendations included the following: coming from a household in the medium tertile of socioeconomic status (unadjusted PRR: 1.59; 95% CI: 1.02, 2.48), having visited the clinic for five times or less in the previous 6 months (unadjusted PRR: 0.64; 95% CI: 0.43, 0.97), and taking three or less blood glucose tests per day (unadjusted PRR: 0.57; 95% CI: 0.38, 0.86).
On the other hand, bivariate-level caretaker factors associated with adherence to the type 1 diabetes care recommendations included the following: having a divorced/separated caretaker (unadjusted PRR: 1.88; 95% CI: 1.05, 3.37), having a caretaker who actively monitors diet (unadjusted PRR: 2.79; 95% CI: 1.70, 4.56), having medium or poor knowledge about diabetes (unadjusted PRR: 0.49; 95% CI: 0.33, 0.72; or unadjusted PRR: 0.32; 95% CI: 0.19, 0.55, respectively), and having a caretaker who is slightly active or not active at all in supervision of insulin injections (unadjusted PRR: 0.41; 95% CI: 0.22, 0.73; or unadjusted PRR: 0.48; 95% CI: 0.31, 0.75, respectively).
Factors independently associated with adherence to type 1 diabetes care recommendations
In the multivariable model (Table 4), the results revealed that children and adolescents with five or lesser visits to the health facility in the previous 6 months were less adherent to type 1 diabetes care recommendations as compared to those who visited the clinic >5 days in the same period (adjusted PRR [APRR]: 0.64; 95% CI: 0.42, 0.98). The participants who were taken care of by siblings were similarly more adherent to diabetes care recommendations compared with those who were under care of their mothers (APRR: 1.66; 95% CI: 1.61, 1.71). In addition, caretakers who were married (APRR: 1.10; 95% CI: 1.05, 1.14) and those who were divorced/separated (APRR: 1.60; 95% CI: 1.12, 2.27) had children and adolescents who were 10% and 60% more adherent to diabetes care recommendations, respectively, compared with those who were never married. Children or adolescents who took three or less tests of blood glucose per day were found less adherent to diabetes care recommendations compared with their counterparts who tested for blood glucose more often (APRR: 0.63; 95% CI: 0.42, 0.95). Furthermore, the prevalence of adherence was 51% and 42% lower among participants whose caretakers had poor knowledge about diabetes and those whose caretakers were not actively involved in the supervision of insulin injections (APRR: 0.49; 95% CI: 0.43, 0.57; and APRR: 0.58; 95% CI: 0.56, 0.60, respectively). Finally, active motoring of children and adolescent diets by the caretakers was associated with higher adherence to diabetes care recommendations (APRR: 1.95; 95% CI: 1.01, 3.78). Age of child and household socioeconomic status were not associated with adherence to type 1 diabetes care recommendations in the final adjusted model.
Discussion
The aim of this study was to determine the level of adherence to type 1 diabetes care recommendations among children and adolescent patients in two urban diabetes clinics of Uganda. In addition, we also sought to establish the factors associated with adherence to these recommendations. Few studies have assessed adherence to type 1 diabetes care recommendations, especially incorporating the three treatment parameters.8 However, even studies that assessed adherence to individual treatment parameters used differing diabetes care recommendations compared with those used in this study; thus, literature comparisons across studies were daunting. In addition, adherence has been difficult to compare across studies because different studies used differing adherence assessment methods.
This study reports a higher adherence to blood glucose monitoring recommendations at 76.5% compared with that reported by Moström et al at 43.9% although the latter study was carried out among older patients with type 1 diabetes.10 In addition, Hansen et al also reported a lower prevalence (39%) of adherence to blood glucose monitoring recommendations among type 1 diabetes patients.14 The latter study, however, considered patients who tested more than three times a day as the only measure of adherence to blood glucose monitoring, while the prevalence reported by the present study encompasses five blood glucose monitoring–related recommendations on which adherence was measured, and compliance to any four was regarded as adherence to blood glucose monitoring. Evaluating only patients who had more than three tests per day as the abovementioned study did, patients in this study are certainly doing badly with only 22 of 200 (11%) meeting this specific recommendation. Several other studies25,26 elsewhere also report a higher proportion of patients testing more than three times per day ranging from 34% to 93%, compared with that reported in this study. The low testing rates among this population could probably be attributed to the lack of testing strips or fear of self-injection among the children and adolescents. It is also important to note that majority of our participants (42%) are from the lowest tertile of socioeconomic status, and thus, testing strips could be difficult to access by most of participants due to cost.
While the current study registered a low prevalence of adherence to diet recommendations (29.5%), it was higher than that reported among Pakistani adolescents at 7.2%.15 Certainly, the level of adherence to dietary recommendations in this study was comparable to that among Tanzanian type 1 diabetes children and adolescents, which was reported at 28%.8 This could be explained by the similarity in setting (for instance, comparable food patterns and dietary trends) between these two sub-Saharan countries. In addition, the difference in diet adherence levels between the studies from the two sub-Saharan countries and that among Pakistani adolescents could be due to cultural and dietary patterns difference among these populations. Although different assessments and recommendations were used as a basis to establish dietary adherence to type 1 diabetes care recommendations between this study and those done elsewhere,27 type 1 diabetes children are still reported to have a poor adherence to dietary recommendations as their diets are characterized by high proportions of saturated fat and low fruit, vegetable, and fiber content.11,27 The low financial status of families could be one of the limiting factors to the provision of adequate diets to these type 1 diabetes patients. Adherence to diabetes care recommendations among type 1 diabetes patients is generally low, and measures to address this are inevitably essential.
Involvement of caregivers in diet monitoring was one of the factors found to positively influence adherence to diabetes care recommendations in this study. Although caretaker and parental involvement are widely related to better treatment outcomes,12,28 no study, to the best of our knowledge, has yet considered diet monitoring in particular as key in improving adherence to diabetes care recommendations. We understand that children and adolescents’ diets in developing countries including Uganda are characterized with junk foods and consumption of unhealthy street foods,29 and therefore, diet monitoring among this type 1 diabetes population is very crucial to bring about better adherence and subsequent improvement in treatment outcomes in type 1 diabetes.
Sibling caretakers, as opposed to mother caretakers, had a higher prevalence of adherent type 1 diabetes patients in this study. First, adherence among type 1 diabetes individuals is a complex process that takes place within the social settings and usually involves alterations of social dynamics.30 Patients who have family and friend support have higher degree of optimism and self-esteem to manage their disease as they will be less depressed about their condition.31,32 Explaining why support or care from siblings led to higher adherence outcomes is not clear to the authors, although there could be a belief that siblings offer more time and are more available to fellow siblings than parents who sometimes leave them for work or go for other engagements. Previous evidence has suggested that there are higher levels of adolescent–parent conflicts in scenarios when most of the treatment responsibility belongs to adolescents, which may result in nonadherence to treatment.33 Such adolescent–parent conflicts may not be common in cases where siblings are the caretakers. Nonetheless, further research is required to explore this association.
Children and adolescents whose caretakers are married and those whose caretakers are divorced/separated were more adherent to type 1 diabetes recommendations in our study. It is believed that children and adolescents who are under the care of a married caretaker gain more support from both parents in terms of motivation for self-care.34 In addition, in such situations, there is usually a shared responsibility of diabetes management and self-care activities between both parents and the child/adolescent, which may lead to improved adherence outcomes.34 However, the authors also believe that divorced caretakers may have more time to engage in diabetes management tasks such as insulin administration and monitoring of injections as they may not have a lot of family tasks to engage in compared with when they were still married. Nonetheless, the authors cannot fully explain these relationships and thus encourage further research. Individuals who tested less often for blood glucose were found to be less adherent to type 1 diabetes care recommendations in the present study. A study by Hendrychova et al is in agreement with this result.35 Telo et al in their study also demonstrated that the frequency of blood glucose monitoring through testing was seen to correlate strongly with adherence,36 which further agrees to the results reported by the present study. Moreover, frequent blood glucose monitoring has been associated with lesser risk of hyperglycemia and hypoglycemia plus subsequent microvascular and macrovascular complications in patients with type 1 diabetes.10
Caretakers or adolescents with poor knowledge about diabetes had children who were less adherent (or were themselves less adherent) to diabetes recommendations in this study. Low diabetes knowledge was found to be positively associated with nonadherence in a study done by Riaz et al.15 Only 30.5% (61 of 200) of the adolescents (or children caretakers) had good knowledge about diabetes in this study, which may explain why this study similarly found poor adherence to recommendations in this population. This finding therefore makes it necessary for health care professionals to stage appropriate interventions in a view to increase knowledge about diabetes to caretakers.
Caretakers who were inactive in insulin injection supervision were found to have less adherent children or adolescents, and this has been documented elsewhere.37 Ellis et al37 also reported higher levels of adherence among adolescents whose parents were knowledgeable about their diabetes care completions/tasks and were frequently present during such completions. This finding is crucial when interventions addressing high-risk youth with type 1 diabetes are to be rolled out because it encourages their parents to continuously supervise them. It, therefore, appears that parents or caregivers who will provide more time to supervise their children while carrying out diabetes management tasks such as insulin injections and blood glucose tests will have their children in a better position to control their blood glucose.
Strengths and limitations
One of the strengths of this study is that it provides current knowledge on the factors associated with adherence to type 1 diabetes care recommendations among Ugandan children and adolescents with type 1 diabetes, which, to our knowledge, have not previously been documented. In addition, this study was founded on “clinic-specified diabetes care recommendations,” and therefore, the assessments of adherence are more context specific, rather than basing on any global or regional diabetes care recommendations, of which our setting may not be currently putting into practice.
However, the major limitation of this study is that findings cannot be translated into causal relationships due to the cross-sectional nature of the research. The study findings may also not be generalizable to children or adolescents attending diabetes clinics of minor health facilities, as they may not be receiving routine education on specific diabetes care recommendations. In addition, it has been most frequently observed that adolescents who are nonadherent are less likely to take part in research.38 Therefore, we are uncertain that those who consented to participate were those with better adherence or vice versa. Nonetheless, this study showed a good response rate, and the findings demonstrate important programming and diabetes care implications particularly in the Ugandan context.
Conclusion
This study reports an overall poor adherence to diabetes care recommendations among type 1 diabetes children and adolescents in this population – although adherence to specific parameters such as blood glucose monitoring was promising. This study, therefore, suggests that children, adolescents, and their caretakers should be equally responsible for ensuring optimal adherence to the clinics’ prescribed diabetes care recommendations and should aim at keeping good caretaker–patient relationships. Further, caretakers who will not take initiative to learn about the basics of type 1 diabetes, supervise their children’s injections, and monitor their diets may continue having them nonadherent to recommendations as they will not know the basic management principles for the disease to provide the necessary support. Further research is nonetheless encouraged to understand how family and sociocultural dynamics influence adherence to diabetes care recommendations in this setting.
Acknowledgments
We thank the staff at Mulago Hospital and St Francis Nsambya Hospital diabetes clinics for the support during the study. The participants who took part in the study are also appreciated.
Author contributions
CK helped to conceptualize the design of the project, supervised the data collection, and helped to prepare and revise the final manuscript. NM assisted in conceptualizing the design of the study, carried out the data analysis, interpreted the data, prepared the first draft of the manuscript, and revised the final document. Both authors are responsible for the accuracy and integrity of the presented findings in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
World Health Organisation. Media centre: diabetes; 2017. Available from: http://www.who.int/mediacentre/factsheets/fs312/en/. Accessed November 11, 2017. | ||
Melmed S, Polonsky K, Larsen PR, Kronenberg PR. Williams Textbook of Endocrinology. Philadelphia, PA: Saunders; 2011. | ||
Della Manna T, Setian N, Savoldelli RD, et al. Diabetes mellitus in childhood: an emerging condition in the 21st century. Rev Assoc Med Bras (1992). 2016;62(6):594–601. | ||
Lu MC, Chang SC, Huang KY, Koo M, Lai NS. Higher risk of thyroid disorders in young patients with type 1 diabetes: a 12-year nationwide, population-based, retrospective cohort study. PLoS One. 2016;11(3):e0152168. | ||
WHO. Adherence to long term therapies: evidence for action; 2003. Available from: http://whqlibdoc.who.int/publications/2003/9241545992.pdf. Accessed February 16, 2018. | ||
AlBuhairan F, Nasim M, Al Otaibi A, Shaheen NA, Al Jaser S, Al Alwan I. Health related quality of life and family impact of type 1 diabetes among adolescents in Saudi Arabia. Diabetes Res Clin Pract. 2016;114:173–179. | ||
Borus JS, Laffel L. Adherence challenges in the management of type 1 diabetes in adolescents: prevention and intervention. Curr Opin Pediatr. 2010;22(4):405–411. | ||
Noorani M, Ramaiya K, Manji K. Glycaemic control in type 1 diabetes mellitus among children and adolescents in a resource limited setting in Dar es Salaam – Tanzania. BMC Endocr Disord. 2016;16(1):29. | ||
Novo Nordisk. An account of the Changing Diabetes® in Children Programme; 2014. Available from: http://bit.ly/2o8hAoD. Accessed September 24, 2017. | ||
Moström P, Ahlén E, Imberg H, Hansson PO, Lind M. Adherence of self-monitoring of blood glucose in persons with type 1 diabetes in Sweden. BMJ Open Diabetes Res Care. 2017;5(1):e000342. | ||
Patton SR. Adherence to diet in youth with type 1 diabetes. J Am Diet Assoc. 2011;111(4):550–555. | ||
Gandhi K, Vu BK, Eshtehardi SS, Wasserman RM, Hilliard ME. Adherence in adolescents with type 1 diabetes: strategies and considerations for assessment in research and practice. Diabetes Manag (Lond). 2015;5(6):485–498. | ||
Aschner P, Horton E, Leiter LA, Munro N, Skyler JS; Global Partnership for Effective Diabetes Management. Practical steps to improving the management of type 1 diabetes: recommendations from the Global Partnership for Effective Diabetes Management. Int J Clin Pract. 2010;64(3):305–315. | ||
Hansen MV, Pedersen-Bjergaard U, Heller SR, et al. Frequency and motives of blood glucose self-monitoring in type 1 diabetes. Diabetes Res Clin Pract. 2009;85(2):183–188. | ||
Riaz M, Basit A, Fawwad A, Yakoob Ahmedani M, Ali Rizvi Z. Factors associated with non-adherence to insulin in patients with type 1 diabetes. Pak J Med Sci. 2014;30(2):233–239. | ||
Daniel. Biostatistics: A Foundation for Analysis in the Health Sciences. 7th ed. New York, NY: John Wiley & Sons; 1999. | ||
Popham WJ. Criterion Referenced Measurement. Prentice Hall: Englewood Cliffs; 1978. | ||
Karve S, Cleves MA, Helm M, Hudson TJ, West DS, Martin BC. Good and poor adherence: optimal cut-point for adherence measures using administrative claims data. Curr Med Res Opin. 2009;25(9):2303–2310. | ||
Fitzgerald JT, Funnell MM, Anderson RM, Nwankwo R, Stansfield RB, Piatt GA. Validation of the Revised Brief Diabetes Knowledge Test (DKT2). Diabetes Educ. 2016;42(2):178–187. | ||
Anderson RM, Donnelly MB, Dedrick RF. Measuring the attitudes of patients towards diabetes and its treatment. Patient Educ Couns. 1990;16(3):231–245. | ||
Redman KB. Measurement Tools in Patient Education. 2nd ed. New York, NY: Springer; 2002. | ||
Zu G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. | ||
Lee J, Tan CS, Chia KS. A practical guide for multivariate analysis of dichotomous outcomes. Ann Acad Med Singapore. 2009;38(8):714–719. | ||
Thompson ML, Myers JE, Kriebel D. Prevalence odds ratio or prevalence ratio in the analysis of cross sectional data: what is to be done? Occup Environ Med. 1998;55(4):272–277. | ||
Miller KM, Beck RW, Bergenstal RM, et al. Evidence of a strong association between frequency of self-monitoring of blood glucose and hemoglobin A1c levels in T1D exchange clinic registry participants. Diabetes Care. 2013;36(7):2009–2014. | ||
Karter AJ, Ackerson LM, Darbinian JA, et al. Self-monitoring of blood glucose levels and glycemic control: the Northern California Kaiser Permanente Diabetes registry. Am J Med. 2001;111(1):1–9. | ||
Rovner AJ, Nansel TR. Are children with type 1 diabetes consuming a healthful diet?: a review of the current evidence and strategies for dietary change. Diabetes Educ. 2009;35(1):97–107. | ||
Wysocki T, Gavin L. Paternal involvement in the management of pediatric chronic diseases: associations with adherence, quality of life, and health status. J Pediatr Psychol. 2006;31(5):501–511. | ||
Ochola S, Masibo PK. Dietary intake of schoolchildren and adolescents in developing countries. Ann Nutr Metab. 2014;64(Suppl 2):24–40. | ||
Rosland AM, Kieffer E, Israel B, et al. When is social support important? The association of family support and professional support with specific diabetes self-management behaviors. J Gen Intern Med. 2008;23(12):1992–1999. | ||
DiMatteo MR, Haskard-Zolnierek KB, Martin LR. Improving patient adherence: a three-factor model to guide practice. Health Psychol Rev. 2012;6(1):74–91. | ||
DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol. 2004;23(2):207–218. | ||
Miller TA, DiMatteo MR. Importance of family/social support and impact on adherence to diabetic therapy. Diabetes Metab Syndr Obes. 2013;6:421–426. | ||
Almeida AC, Pereira MG, Leandro E. Chapter 17. The influence of family support, parental coping and school support on adherence to type 1 diabetes’ self-care in adolescents. In: Escher AP, Li A, editors. Type 1 Diabetes. Rijeka: InTech; 2013:447–451. | ||
Hendrychova T, Vytrisalova M, Smahelova A, Vlcek J, Kubena AA. Adherence in adults with type 1 diabetes mellitus correlates with treatment satisfaction but not with adverse events. Patient Prefer Adherence. 2013;7:867–876. | ||
Telo GH, de Souza MS, Andrade TS, Schaan BD. Comparison between adherence assessments and blood glucose monitoring measures to predict glycemic control in adults with type 1 diabetes: a cross-sectional study. Diabetol Metab Syndr. 2016;8(1):54. | ||
Ellis DA, Podolski CL, Frey M, Naar-King S, Wang B, Moltz K. The role of parental monitoring in adolescent health outcomes: impact on regimen adherence in youth with type 1 diabetes. J Pediatr Psychol. 2007;32(8):907–917. | ||
Evangelista LS. Compliance: a concept analysis. Nurs Forum. 1999;34(1):5–11. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.