Back to Journals » Clinical Optometry » Volume 15
Factors Affecting Unmet Need for Presbyopia Correction Among School Teachers in Debre Tabor Town, Northwest Ethiopia
Authors Yalew AB , Alemu HW , Alemayehu AM
Received 13 April 2023
Accepted for publication 12 June 2023
Published 16 June 2023 Volume 2023:15 Pages 129—138
DOI https://doi.org/10.2147/OPTO.S411708
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Mr Simon Berry
Amsalu Belete Yalew,1,* Haile Woretaw Alemu,2,* Abiy Maru Alemayehu2,*
1Department of Ophthalmology and Optometry, School of Medicine, College of Medicine and Health Sciences, Hawassa University, Hawassa, Ethiopia; 2Department of Optometry, School of Medicine, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
*These authors contributed equally to this work
Correspondence: Abiy Maru Alemayehu, Email [email protected]
Background: Uncorrected presbyopia is the leading cause of near visual impairment among working-age adults in the world. In Ethiopia, there was limited evidence on the magnitude of uncorrected presbyopia and its associated factors among school teachers. Therefore, this study aimed to determine the magnitude of untreated presbyopia and its associated factors among school teachers in Debre Tabor town, Northwest Ethiopia.
Methods: An institution-based cross-sectional study was conducted on 448 school teachers at Debre Tabor town using a simple random sampling technique. The data were collected using a face-to-face interview and a comprehensive ocular examination. A binary multivariable logistic regression model was conducted to identify associated factors of the uncorrected presbyopia.
Results: Generally, the prevalence of uncorrected presbyopia among school teachers was 63.62% (95% CI: 59.2– 67.9). Age (35– 45) (AOR: 4.56, 95% CI: 1.74, 11.91), female gender (AOR: 3.03, 95% CI: 1.75, 5.26), unaware of presbyopia (AOR: 2.35, 95% CI: 1.30, 4.25), unaware of refraction site (AOR: 4.21, 95% CI: 2.42, 7.33), no eye checkup history (AOR: 2.76, 95% CI: 1.52, 5.01), and no family history of spectacle use (AOR: 2.61, 95% 4.67) were significantly associated with uncorrected presbyopia.
Conclusion: In the current study, the magnitude of uncorrected presbyopia was high. Age below 45 years, female gender, lack of awareness of presbyopia and refraction site, lack of history of eye checkups, and family spectacle use were significantly associated with uncorrected presbyopia. The early correction of presbyopia, health education on presbyopia, and the provision of affordable spectacle corrections for school teachers were recommended.
Keywords: Debre Tabor, Ethiopia, magnitude, presbyopia
Introduction
Presbyopia is a common age-related ocular condition characterized by reduced near vision due to progressive loss of lens accommodation.1 There are many factors contributing to the development of presbyopia, but aging is the most consistent one.2–4 Approximately 1.8 billion people were living with presbyopia globally, and from those, around 215 million (12%) were living in Africa.2 In Ethiopia, the prevalence of presbyopia ranges from 69% to 95%.3,4 Uncorrected presbyopia is the leading cause of universal near visual impairment among the working-age population in the world.2
Globally, 1.8 billion people were living with presbyopia; however, 826 million (45%) had no correction or inadequate correction of presbyopia.2 A meta-analysis study on the assessment of global vision impairment from 1990 to 2020 showed that 510 (371–667) million people remain visually impaired at present due to a lack of presbyopia correction.5 The magnitude of uncorrected presbyopia among school teachers ranges from 29% to 96.3%, which was worse in sub-Saharan Africa.1,6–9 Studies done in Ethiopia showed that the magnitude of uncorrected presbyopia ranges from 52% in Hawassa to 69% in Bahir Dar.4,10,11
School teachers are one of the main building blocks of a progressive society, and their ability to see clearly is essential for their daily activities. Most of their activities require extensive periods of near and intermediate work to prepare teaching materials and read students’ scripts, which rely on the use of near corrections. Due to this, proper and adequate correction is required to maximize their performance and quality of life.1
Uncorrected presbyopia has a significant impact on near-vision-related tasks (2–8 folds), reduce vision-related quality of life,12–15 induce distress and low self-esteem,16 loss of productivity among working age population, and it causes more than 25.4 billion-dollar’s loss in working-age adults.17–19
The major risk factors for uncorrected presbyopia among school teachers were younger age (below 45 years), being female, lack of awareness of presbyopia and refraction sites, no history of eye check-ups, and self-rated good vision.10,11,20,21
The World Health Organization (WHO) sets different priorities for the provision of presbyopia correction services.22 Effective correction of vision in presbyopia can be achieved through spectacles correction, contact lenses, intraocular lenses, and refractive surgery.23–25 Uncorrected presbyopia is a major public health issue that needs to be addressed in both the developing and developed worlds.26 Therefore, this study was aimed at determining the magnitude of uncorrected presbyopia and its associated factors among school teachers in Debre Tabor town, Northwest Ethiopia. This study will provide valuable information for advocacy, planning, providing refraction and affordable spectacle services, and implementing a program of eye health services for schoolteachers.
Methods and Materials
Study Design, Area, and Period
An institution-based cross-sectional study was done among schoolteachers at Debre Tabor town, North Ethiopia. The town is in Amhara regional state, the capital city of the South Gondar zone, which is located 667 km from the capital city of Ethiopia (Addis Ababa). Debre Tabor town has an estimated population of 119,176 (51.3% males, 48.7% females).27 The town has a total of 6 kebeles (the smallest government administrative units in Ethiopia), with 11 public schools (7 primary and 4 secondary) and 9 private schools (8 primary and 1 secondary), with a total of 1156 teachers aged 35 years and above (Debre Tabor town educational office, unpublished report, 2022). The town has a comprehensive, specialized hospital, one private specialty eye clinic, and two private optical workshops, which provide general eye health services and spectacle services for the surrounding community. The study period was from May 24 to June 28, 2022.
Inclusion Criteria
All school teachers of age 35 years and above and presenting near visual acuity worse than N6, who worked in primary and secondary schools at Debre Tabor town during the study period, were included in the study.
Exclusion Criteria
School teachers with medial opacity that obscured the view of their retina and hindered refraction correction, such as significant cataracts, central corneal opacity, and retinal disease like macular degeneration were excluded from the study.
Sample Size Determination and Sampling Procedures
Power analysis software was used to determine a maximum sample size using the following assumptions: sex as a consistent factor,11 power 80%, unexposed to exposed ratio 1:1, confidence interval of 95%, uncorrected presbyopia among unexposed 42.0%, OR 1.78, and non-response rate 10%. The final sample size based on sex was 451.
To select the study participants from 20 schools, a simple random sampling technique was used. To assure representativeness, the number of teachers aged 35 years and older in each school was identified by asking their current age using their name list as a sampling frame. According to the number of teachers, the necessary sample from each school was allocated proportionally, and 451 participants who met the inclusion criteria were randomly chosen by lottery methods from all schools. When the selected individuals did not fulfil the eligibility criteria of the study, the next participant was selected by lottery.
Data Collection Tools
Resources from studies that have been conducted earlier were used to develop the tool.1,3,4,10,11 The structured questionnaires were initially prepared in English by the principal investigator, then translated into Amharic (local language) by language expertise and re-translated to English to check consistency in the meaning of words and concepts. The questionnaire consisted of demographic information and questions to identify the associated factors of uncorrected presbyopia. It was pre-tested and modified prior to the data collection. A pen-torch light was used for anterior segment examinations and direct ophthalmoscope for posterior segment examinations. Snellen acuity chart was used for distance and near visual acuity measurements with a pinhole to identify whether vision reduction was due to refractive error or not. Streak retinoscope, trial frame, trial lenses, and accessories were used for determining refractive errors of study subjects.
Data Collection Procedures
The data were collected by three well-trained optometrists under the supervision of two supervisors. The optometrists conducted a face-to-face interview using an Amharic version structured questionnaire that had been pre-tested in advance that included socio-demographic data, eye care service-related data, and clinical variables following the receipt of participant’s informed consent. After completing the interview, all study participants received a comprehensive ocular examination. Both the anterior and posterior segments were examined using pen-light torch and a direct ophthalmoscope, respectively.
Using a standard Snellen chart, distance visual acuity (DVA) was measured at 20 feet under ambient light condition for all participants. Study participants with DVA worse than 6/6 were refracted, while teachers with DVA 6/6 and better directly underwent near refraction. Following this, near visual acuity (NVA) was measured binocularly after best-corrected distance vision with a near vision chart at 40cm. Participants with binocular NVA of N6 were refracted with plus spherical lenses on top of distance correction to obtain the best corrected NVA.
After the comprehensive ocular examination, each participant received an advice regarding their eye health, presbyopia treatment options, and visual status. Individuals who had no spectacle correction and who had other ocular conditions were referred to Debre Tabor Hospital for further examination and treatment.
Data Quality Assurance
To confirm the accuracy of the data, a pre-test was conducted among school teachers in Gasagn town on 5% of the sample using the Amharic version of the structured questionnaire. Training was given to the data collectors and supervisors by the principal investigators on data collection procedures and sampling techniques. The collected data was checked for completeness and consistency each day, and double entry of data was done to assure the quality of the data.
Data Processing and Analysis
Epi-Data version 4.6 was used to code and enter the data before it was exported and imported into the statistical package for social science version 26 for analysis. The data were described using summary statistics like proportion, frequency, mean, and interquartile range. A binary multivariable logistic regression model was built to identify the significant associated factors of uncorrected presbyopia. The variance, inflation factor, and tolerance were used to test a presence of multi-collinearity. The backward elimination method was used to enter variables into a multivariable binary logistic regression. The Hosmer and Lemeshow goodness of fit test (p = 0.74) was used to determine the model’s fitness. The strength of the association between the variables was expressed using the adjusted odds ratio (AOR) at the 95% confidence level. A variable with a P-value of less than 0.05 was considered statistically significant.
Results
Profiles of the Study Subjects
The study included 448 school teachers, with a 99.3% response rate. Their mean age of the study subjects was 46.79 (6.24) years (IQR: 35–65). From the total participants, 244 (54.5%) were female. Most of the participants (353, or 79%) were public school teachers, and 206, or 46.0%, were working on teaching from 16 to 30 years old. The median average monthly income of participants was 7300 ETB (IQR = 6000–8000) (Table 1).
 |
Table 1 Profiles of Study Subjects at Debre Tabor Town, Northwest Ethiopia, 2022 (n = 448) |
Awareness and Eye Care Service-Related Factors
Among the total participants, 205 (45.8%) had no awareness of presbyopia, and 242 (54.0%) were unaware of refraction sites. 76% of the instructors reported having no eye checkup history in the previous year. Among the total study participants, 190 (42.4%) rated their current vision as good (Table 2) and 77.4% had near spectacle correction among teachers rating their current vision as poor.
 |
Table 2 Awareness and Eye Care Service-Related Factors of School Teachers at Debre Tabor Town, Northwest Ethiopia, 2022 (n = 448) |
Clinical Data of the Study Subjects
Among 448 participants, 161 (35.9%) had refractive errors. However, only 37 (23%) had spectacle corrections. Most of the participants (302) (67.4%) had a mild degree of presbyopia, and 269 (60%) required from +1.00 to +1.75D of nearsightedness as a correction modality (Table 3).
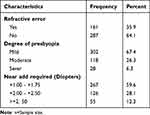 |
Table 3 Clinical Data of Study Subjects at Debre Tabor Town, North Ethiopia, 2022 (n = 448) |
Prevalence of Uncorrected Presbyopia
The prevalence of uncorrected presbyopia was 285 (63.62%) (95% CI: 59.2–67.9%) (Figure 1). Of these, 180 (63.2%) were under 45 years of age (Figure 2) and 175 (61.4%) were unaware of presbyopia.
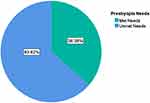 |
Figure 1 Prevalence of uncorrected presbyopia among school teachers in Debre Tabor town, Northwest Ethiopia, 2022. |
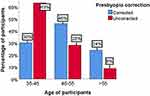 |
Figure 2 Prevalence of uncorrected presbyopia among school teachers based on their age groups in Debre Tabor town, Northwest Ethiopia, 2022. |
Factors Associated with Uncorrected Presbyopia
By using a bivariable analysis, age, gender, education level, income, school type, experiences, presbyopia awareness, refraction site awareness, spectacle use for distance, history of eye check-ups in the past year, family spectacle use, degree of presbyopia, and amount of near-add power required were associated with uncorrected presbyopia at the 0.05 level of significance. However, following the multivariate logistic regression analysis’s correction for possible confounders, age, gender, presbyopia awareness, awareness of refraction sites, eye checkup history, and family history of spectacle use were statistically significantly associated with uncorrected presbyopia with a p-value <0.05.
Participants aged 35–45 years had almost five times (AOR = 4.56, 95% CI: 1.74, 11.91) the likelihood of having uncorrected presbyopia than those aged greater than 55 years. With respect to gender, the likelihood of having uncorrected presbyopia was three times higher (AOR = 3.03, 95% CI: 1.75, 5.26) in female subjects relative to males. Lack of awareness of presbyopia increased the risk of unmet need by two times (AOR = 2.35, 95% CI: 1.30, 4.25) in contrast to those who were aware. Similarly, subjects who had no awareness of refraction sites were four times (AOR = 4.21, 95% CI: 2.42, 7.33) more probable to have uncorrected presbyopia in comparison to those who were aware. The odds of uncorrected presbyopia for study subjects who had no eye check-up in the previous year were almost three times (AOR = 2.76, 95% CI: 1.52, 5.01) greater than those subjects who had a history of eye check-ups. Subjects who had no family spectacle correction had almost three times (AOR = 2.61, 95% CI: 1.46, 4.67) the greater likelihood of having uncorrected presbyopia in comparison to those who had family spectacle correction (Table 4).
 |
Table 4 Bivariable and Multivariable Logistic Regression Analysis of Factors Associated with Uncorrected Presbyopia Among School Teachers in Debre Tabor Town, Northwest Ethiopia, 2022 (n = 448) |
However, marital status, level of education, level of income, level of school, type of school, working experiences, distance spectacle use, self-rated vision, refractive error, severity of presbyopia, and near-add power required were not associated with uncorrected presbyopia.
Discussion
In the current study, the prevalence of uncorrected presbyopia was 63.62% (95% CI: 59.2, 67.9%). The finding was in line with the studies conducted in Finote Selam (61.95%)4 and Ghana (64%).28 This could be a result of similarities in the mean age of study subjects, the definition of uncorrected presbyopia, and spectacle service provisions. The high prevalence of unmet needs in developing countries might be attributed to the poor accessibility of affordable and qualitative eye care and spectacle services.29
However, in the current study, the magnitude of uncorrected presbyopia was greater than in the previous studies done at Hawassa (51.26%),11 Nigeria (31.3%, 36.4%),1,8 Ghana (29.6%, 54.7%)6,7 and Jakarta (Indonesia) (41%).30 The difference might be due to the variation in the definition of uncorrected presbyopia, the age of participants, and eye care services. In the South Ethiopia study, unmet need was described as binocular near vision worse than N8 with or without existing correction. However, in the current study, uncorrected presbyopia was described as binocular near vision worse than N6 with or without existing correction, which led to a higher magnitude of unmet need. Moreover, there were available and affordable spectacle services, including public spectacle workshops in Hawassa and glasses for teachers without facing monetary hardship in Indonesia, while in this study area there was low accessibility of affordable spectacle services without a public-owned optical dispensing unit, and optical workshops are private-centered and possibly costly.31 This leads to a higher level of uncorrected presbyopia due to the low accessibility of spectacle services and their high cost. Furthermore, the studies conducted in Nigeria included younger teachers ≥30 years old who had fewer near-visual complaints, and in Ghana, >40-year-old subjects were involved with small samples to achieve at least N8 opto-types at 30cm. Conducting research in those age groups showed a lower prevalence of uncorrected presbyopia.
On the contrary, the finding of the current study was lower magnitude than the studies done in Bahir Dar (69.2%),10 Eritrea (90.1%),32 Durban, South Africa (96.3%),9 Bangladesh (96.8%),33 Nepal (90%),34 and Nicaragua (89.58%).35 The discrepancy could be attributed to the variety of study subjects’ demographics, definitions, awareness, and study settings. This study was conducted with school teachers from an actively working-age population with high near-vision demands, which implies that they became aware of their blurry vision early on and sought visual correction, while the previous studies were community-based with a lower education level, and their near-vision demands might be less essential. Those may make people less likely to get near corrections, which resulted in a higher magnitude of uncorrected presbyopia in previous studies as compared to our study. Moreover, studies done in Bahir Dar defined unmet need as binocular near vision worse than N8, which led to a higher magnitude of uncorrected presbyopia than this study. Also, the study participants’ awareness and behavior regarding the use of eye care services, as well as the accessibility and availability of those services, could play a role in this discrepancy.
Regarding the associated factors, participants aged 35 to 45 years had a nearly five times greater likelihood of having uncorrected presbyopia than those aged above 55 years. This finding was in line with the studies done in Hawassa11 and Bahir Dar, Ethiopia.10 The reason for their association could be that as age increases, the co-existence of age-related progressive loss of ability to accommodate at near increases the severity of presbyopia and near visual impairment. Those could be the main reason to get a correction as compared to the younger age (35–45 years).9 Moreover, youthful age (35–45 years) had subconsciously adapted to a mild degree of presbyopia, and there may be a lack of felt need for correction as compared to older age.7
The odds of having uncorrected presbyopia among female participants were three times greater than those among male participants, which was validated by studies conducted in Bahir Dar,10 Hawassa, Ethiopia,11 and Japan.21 This might be because presbyopia affects women more frequently than men and manifests earlier in their life in women.1 Compared to females, males were most likely to afford for spectacles36 and aware of where to get the refraction services.
Individuals who had no awareness of presbyopia and refraction sites had 2 and 4 times higher untreated presbyopia in comparison to those who had awareness, respectively. Those findings were supported by similar studies done in Bahir Dar10 and Hawassa,11 Nigeria,1 and Ghana.7 This might be as a result of the possibility of receiving various eye health-related information among individuals who have awareness of presbyopia and refraction sites, which might increase eye health service-seeking behavior and motivate them to have spectacle corrections as compared to their counterparts.4,37
In accordance with a Bahir Dar study,10 subjects who had no eye check-up in the previous year had three times higher levels of uncorrected presbyopia than subjects with a history of eye checkups. This could be as a result of eye health education and medical advice given to individuals coming for eye examinations, which helped them acquire some basic knowledge about presbyopia, increase awareness, and increase their motivations for using corrections.4,18 Moreover, individuals receive medical advice, instructions, and education about eye health when they come to eye clinics, which helps them learn some fundamental information on presbyopia.
Study subjects who had no family history of spectacle correction had nearly three times higher uncorrected presbyopia than those who had a family history of spectacle correction. The possible justification for the association could be that subjects who had a family history of spectacle correction might have good familiarity with the problem and refraction sites, increase eye health seeking behaviors, and improve their misconceptions about spectacle correction as compared to their counterparts.18,22
In previous studies, low levels of income, distance visual impairment, and self-rated good vision were significant determinants of untreated presbyopia. But in our study, there was no significant association.11,20,21
Limitation of Study
The study was an institution-based study; it might not represent the real burden of uncorrected presbyopia in a general population, which affects the generalizability of the findings. Moreover, certain questionnaires rely on the respondent’s ability to recall events from the previous year, which could lead to recall bias. Since the study was cross-sectional, a cause-and-effect relationship could not be demonstrated.
Conclusion
In the current study, the magnitude of uncorrected presbyopia among school teachers was high. According to WHO’s priority setting for presbyopia correction provision, the result indicates that the area requires a moderate priority for the provision of presbyopia correction services. Age 35–45 years, being female, lack of awareness about presbyopia and refraction sites, lack of eye check-up history, and having no family history of spectacle correction were found to be independent and strongly associated with untreated presbyopia in this study. The Ministry of Health and eye health-care professionals should increase and encourage the spread of information on eye health, presbyopia, and their correction options through mass media and increase initiatives for eye health in schools involving vision checkups and the provision of affordable eyeglass services for school teachers. School teachers should have regular eye checks.
Abbreviations
AOR, Adjusted Odds Ratio; CI, Confidence Interval; COR, Crude Odds Ratio; WHO, World Health Organization.
Ethics Approval and Informed Consent
This study was conducted in line with the Declaration of Helsinki. A formal authorization paper was also received from the Debre Tabor health office and each school’s directors, in addition to ethical approval from the University of Gondar’s College of Medicine and Health Sciences, School of Medicine, Ethical Review Committee. Following an explanation of the study’s objectives, written informed consent was obtained from each study participant, and each study subject was informed of their right to withdraw from the study at any moment throughout the interview and examination. The study subjects’ privacy was well maintained.
Acknowledgments
We would like to express our deepest gratitude to the data collectors who faced an exhaustive data collection process. We wish to thank the study participants for their willingness to participate in the study.
Disclosure
The authors declare that no conflicts of interest exist.
References
1. Idowu OO, Aribaba OT, Onakoya AO, Rotimi-Samuel A, Musa KO, Akinsola FB. Presbyopia and near spectacle correction coverage among public school teachers in Ifo Township, South-West Nigeria. Nigerian Postgraduate Med J. 2016;23(3):132. doi:10.4103/1117-1936.190342
2. Fricke TR, Tahhan N, Resnikoff S, et al. Global prevalence of presbyopia and vision impairment from uncorrected presbyopia: systematic review, meta-analysis, and modelling. Ophthalmology. 2018;125(10):1492–1499. doi:10.1016/j.ophtha.2018.04.013
3. Andualem HB, Assefa NL, Weldemichael DZ, Tefera TK. Prevalence and associated factors of presbyopia among school teachers in Gondar city, Northwest Ethiopia, 2016. Clin Optometry. 2017;9:85. doi:10.2147/OPTO.S129326
4. Fekadu S, Assem A, Mengistu Y. Near vision spectacle coverage and associated factors among adults living in finote Selam Town, Northwest Ethiopia: community-based cross-sectional study. Clin Ophthalmol. 2020;14:3121. doi:10.2147/OPTH.S278262
5. Bourne R, Steinmetz JD, Flaxman S, et al. Trends in prevalence of blindness and distance and near vision impairment over 30 years: an analysis for the Global Burden of Disease Study. Lancet Global Health. 2021;9(2):e130–e143. doi:10.1016/S2214-109X(20)30425-3
6. Kumah D, Lartey S, Amoah-Duah K. Presbyopia among public senior high school teachers in the Kumasi metropolis. Ghana Med J. 2011;45(1). doi:10.4314/gmj.v45i1.68919
7. Koduah C, Bunce C, Gilbert C. Presbyopia and Other Eye Conditions in Teachers in Ghana. Int J Environ Res Public Health. 2019;16(17):3209. doi:10.3390/ijerph16173209
8. Chinawa N, Pedro-Egbe C, Ejimadu C. Barriers to uptake of presbyopic correction among primary and secondary teachers in public schools in B/K-dere communities in Rivers State, Nigeria. Adv Ophthalmol Vis Syst. 2016;5(3):00161.
9. Naidoo KS, Jaggernath J, Martin C, et al. Prevalence of presbyopia and spectacle coverage in an African population in Durban, South Africa. Optometry Vision Sci. 2013;90(12):1424–1429. doi:10.1097/OPX.0000000000000096
10. Girum M, Gudeta AD, Alemu DS. Determinants of high unmet need for presbyopia correction: a community-based study in Northwest Ethiopia. Clin Optometry. 2017;9:25. doi:10.2147/OPTO.S123847
11. Munaw MB, Kebede BN, Adimassu NF. Unmet need for presbyopia correction and its associated factors among school teachers in Hawassa city, South Ethiopia. BMC Ophthalmol. 2020;20(1):1–8. doi:10.1186/s12886-020-01454-5
12. Berdahl J, Bala C, Dhariwal M, Lemp-Hull J, Thakker D, Jawla S. Patient and economic burden of presbyopia: a systematic literature review. Clin Ophthalmol. 2020;14:3439. doi:10.2147/OPTH.S269597
13. Williams S, Brian G, Toit R. Measuring vision-specific quality of life among adults in Fiji. Ophthalmic Epidemiol. 2012;19(6):388–395. doi:10.3109/09286586.2012.716896
14. Sivardeen A, McAlinden C, Wolffsohn JS. Presbyopic correction use and its impact on quality of vision symptoms. J Optom. 2020;13(1):29–34. doi:10.1016/j.optom.2018.12.004
15. Muhammad N, Alhassan MB, Umar MM. Visual function and vision-related quality of life in presbyopic adult population of Northwestern Nigeria. Nigerian Med J. 2015;56(5):317. doi:10.4103/0300-1652.170379
16. Lu Q, Congdon N, He X, Murthy GV, Yang A, He W. Quality of life and near vision impairment due to functional presbyopia among rural Chinese adults. Invest Ophthalmol Vis Sci. 2011;52(7):4118–4123. doi:10.1167/iovs.10-6353
17. Frick KD. What the comprehensive economics of blindness and visual impairment can help us understand. Indian J Ophthalmol. 2012;60(5):406. doi:10.4103/0301-4738.100535
18. Chan VF, MacKenzie GE, Kassalow J, Gudwin E, Congdon N. Impact of presbyopia and its correction in low-and middle-income countries. Asia-Pacific J Ophthalmol. 2018;7(6):370–374. doi:10.22608/APO.2018449
19. Frick KD, Joy SM, Wilson DA, Naidoo KS, Holden BA. The global burden of potential productivity loss from uncorrected presbyopia. Ophthalmology. 2015;122(8):1706–1710. doi:10.1016/j.ophtha.2015.04.014
20. Man REK, Fenwick EK, Sabanayagam C, et al. Prevalence, correlates, and impact of uncorrected presbyopia in a multiethnic Asian population. Am J Ophthalmol. 2016;168:191–200. doi:10.1016/j.ajo.2016.05.019
21. Sadamatsu Y, Ono K, Hiratsuka Y, et al. Prevalence and factors associated with uncorrected presbyopia in a rural population of Japan: the Locomotive Syndrome and Health Outcome in Aizu Cohort Study. Jpn J Ophthalmol. 2021;65(5):724–730. doi:10.1007/s10384-021-00863-3
22. Laviers HR, Omar F, Jecha H, Kassim G, Gilbert C. Presbyopic spectacle coverage, willingness to pay for near correction, and the impact of correcting uncorrected presbyopia in adults in Zanzibar, East Africa. Invest Ophthalmol Vis Sci. 2010;51(2):1234–1241. doi:10.1167/iovs.08-3154
23. Zebardast N, Friedman DS, Vitale S. The prevalence and demographic associations of presenting near-vision impairment among adults living in the United States. Am J Ophthalmol. 2017;174:134–144. doi:10.1016/j.ajo.2016.11.004
24. Hutchins B, Huntjens B. Patients’ attitudes and beliefs to presbyopia and its correction. J Optom. 2021;14(2):127–132. doi:10.1016/j.optom.2020.02.001
25. Marmamula S, Keeffe JE, Rao GN. Uncorrected refractive errors, presbyopia and spectacle coverage: results from a rapid assessment of refractive error survey. Ophthalmic Epidemiol. 2009;16(5):269–274. doi:10.1080/09286580903144720
26. Wolffsohn JS, Davies LN. Presbyopia: effectiveness of correction strategies. Prog Retin Eye Res. 2019;68:124–143. doi:10.1016/j.preteyeres.2018.09.004
27. Service ES. Population size of towns by sex, region, zone and weredas as of July 2021. Available from: https://www.statsethiopia.gov.et/wp-content/uploads/2020/08/Population-of-Towns-as-of-July-2021.pdf.
28. Ntodie M, Abu SL, Kyei S, Abokyi S, Abu EK. Near vision spectacle coverage and barriers to near vision correction among adults in the Cape Coast Metropolis of Ghana. Afr Health Sci. 2017;17(2):549–555. doi:10.4314/ahs.v17i2.31
29. Muhammad RC, Jamda MA. Presbyopic correction coverage and barriers to the use of near vision spectacles in rural Abuja, Nigeria. Sub-Saharan Afr J Med. 2016;3(1):20. doi:10.4103/2384-5147.176301
30. Ehrlich JR, Laoh A, Kourgialis N, et al. Uncorrected refractive error and presbyopia among junior high school teachers in Jakarta, Indonesia. Ophthalmic Epidemiol. 2013;20(6):369–374. doi:10.3109/09286586.2013.848456
31. Alemu HW. Willingness to pay for spectacle among presbyopic population in South Gondar, Ethiopia: a cross-sectional study. bioRxiv. 2018;482943. doi:10.1080/09286586.2020.1786589
32. Chan VF, Mebrahtu G, Ramson P, Wepo M, Naidoo KS. Prevalence of refractive error and spectacle coverage in Zoba Ma’ekel Eritrea: a rapid assessment of refractive error. Ophthalmic Epidemiol. 2013;20(3):131–137. doi:10.3109/09286586.2013.783082
33. Muhit M, Minto H, Parvin A, et al. Prevalence of refractive error, presbyopia, and unmet need of spectacle coverage in a northern district of Bangladesh: rapid Assessment of Refractive Error study. Ophthalmic Epidemiol. 2018;25(2):126–132. doi:10.1080/09286586.2017.1370119
34. Sapkota Y, Dulal S, Pokharel G, Pant B, Ellwein L. Prevalence and correction of near vision impairment at Kaski, Nepal. Nepalese J Ophthalmol. 2012;4(1):17. doi:10.3126/nepjoph.v4i1.5845
35. Hookway LA, Frazier M, Rivera N, Ramson P, Carballo L, Naidoo K. Population‐based study of presbyopia in Nicaragua. Clin Exper Optometry. 2016;99(6):559–563. doi:10.1111/cxo.12402
36. Patel I, Munoz B, Mkocha H, Schwarzwalder AW, Mchiwa W, West SK. Change in function and spectacle-use 2 months after providing presbyopic spectacles in rural Tanzania. Br J Ophthalmol. 2010;94(6):685–689. doi:10.1136/bjo.2008.145607
37. Tsuneyoshi Y, Masui S, Arai H, et al. Determination of the standard visual criterion for diagnosing and treating presbyopia according to subjective patient symptoms. J Clin Med. 2021;10(17):3942. doi:10.3390/jcm10173942
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
