Back to Journals » Drug, Healthcare and Patient Safety » Volume 15
Evaluation of Rational Drug Use Based on WHO/INRUD Core Drug Use Indicators in a Secondary Care Hospital: A Cross-Sectional Study in Western Uganda
Authors Goruntla N , Ssesanga J , Bommireddy BR , Thammisetty DP , Kasturi Vishwanathasetty V , Ezeonwumelu JOC , Bukke SPN
Received 2 June 2023
Accepted for publication 8 September 2023
Published 14 September 2023 Volume 2023:15 Pages 125—135
DOI https://doi.org/10.2147/DHPS.S424050
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Hemalkumar B Mehta
Narayana Goruntla,1 Joackim Ssesanga,1 Bhavana Reddy Bommireddy,2 Durga Prasad Thammisetty,3 Veerabhadrappa Kasturi Vishwanathasetty,4 Joseph Obiezu Chukwujekwu Ezeonwumelu,1 Sarad Pawar Naik Bukke5
1Department of Clinical Pharmacy and Pharmacy Practice, School of Pharmacy, Kampala International University, Western Campus, Ishaka, Uganda; 2Research Scholar, Department of Pharmacy Practice, Raghavendra Institute of Pharmaceutical Education and Research (RIPER) – Autonomous, Anantapur, Andhra Pradesh, India; 3Department of Pharmacy Practice, Sri Padmavathi School of Pharmacy, Tirupati, Andhra Pradesh, India; 4Department of Pharmacognosy and Pharmaceutical Chemistry, School of Pharmacy, Kampala International University, Western Campus, Ishaka, Uganda; 5Department of Pharmaceutics and Pharmaceutical Technology, School of Pharmacy, Kampala International University, Western Campus, Ishaka, Uganda
Correspondence: Narayana Goruntla; Joackim Ssesanga, Department of Clinical Pharmacy and Pharmacy Practice, School of Pharmacy, Kampala International University, Western Campus, Ishaka, Uganda, Tel +256 760060453, Email [email protected]; [email protected]; [email protected]
Purpose: Rational drug use (RDU) promotes safe, efficient, and cost-effective utilization of medicines in hospital settings. The aim of this study was to assess rational drug use based on the World Health Organization (WHO) and the International Network for Rational Use of Drugs (INRUD) core drug use indicators.
Patients and Methods: This prospective, descriptive, hospital-based cross-sectional study was conducted among patients attending the Outpatient Department of a secondary care hospital located in the Sheema District of Western Uganda. A total of 450 prescriptions were prospectively collected from eligible patients and subjected to evaluation by using the WHO/INRUD core drug use indicators (prescribing, patient care, and health-facility indicators).
Results: The average number of drugs prescribed per encounter was found to be 3.2 (optimal value=1.6– 1.8). The percentages of drugs prescribed by their generic name (90.48%) and from the Essential Medicine List (96.23%) were close to the WHO reference (100%). The percentage of antibiotics (66.22%) and injections (25.22%) per encounter exceeded the WHO standards (antibiotics=20.0– 26.8; injections=13.4– 24.1). Among the patient-care indicators, the average consultation time (5.41 minutes), average dispensing time (131.03 seconds), percentage of medicines dispensed (76.11%), percentage of medicines adequately labeled (59.74%), and percentage of patients with dosage knowledge (49.50%) did not meet the WHO reference. Facility indicators such as the percentage of key medicines available in the stock (66.67%) did not conform to the WHO optimal value. The hospital made the EML hundred percent available to all practitioners.
Conclusion: The study concludes that the prescribing, patient care, and health facility indicators at Sheema District Secondary Care Hospital deviate from the optimal values recommended by the WHO. Therefore, this study indicates a need for improvement on these indicators and a requirement for the ongoing educational initiatives focused on rational drug prescribing, dispensing, and patient use in order to comply with the standards set by the WHO.
Keywords: drug use pattern, health facility, irrational, patient care, prescribing pattern, rational, Uganda, WHO drug use indicators
Introduction
Rational Drug Use (RDU) promotes safe, efficient, and cost-effective utilisation of medication.1 It comprises appropriate prescribing by physicians, dispensing by pharmacists, and utilisation of medicines by patients in order to achieve definite therapeutic outcomes. To accomplish Rational Drug Use (RDU), patients must receive appropriate medications tailored to their specific medical condition, administered in an adequate dose and duration, and at a cost that is both affordable for the individual and society as a whole.2 The primary goal of RDU is to enhance patient care, decrease drug therapy expenses, prevent potential adverse drug reactions (ADRs) and drug interactions (DIs), and also enhance medication adherence and clinical outcomes.3
Globally, irrational drug use is a serious public health concern that has a major impact on microbial resistance.4 Irrational drug use exists all over the world, but it is highly prevalent in developing and underdeveloped nations due to fragile or fragmented healthcare systems.4 The most common irrational drug use practices in hospital settings include polypharmacy, improper antibiotic use, excessive use of injections instead of appropriate oral formulations, non-compliance with clinical guidelines, inappropriate dosage recommendations, and non-generic prescribing.5
Irrational drug use practices may increase the burden of drug-induced morbidity, mortality, and healthcare costs.6 Evidence shows that polypharmacy is significantly associated with the development of DIs and ADRs among hospitalised patients.7 Inappropriate use of antibiotics may result in increased microbial resistance, which further drives the prescribing of an alternative antibiotic that is not in the patient’s affordable range and later results in a loss of patient confidence in the healthcare system.8 According to a mathematical modeling study, the annual global burden of Hepatitis B, Hepatitis C, and Human Immuno Deficiency Virus (HIV) infections was 1.67 million, 315,120, and 33,877, respectively.9 Overuse of injections may increase the risk of injection transmitted infections, especially in developing countries where the use of unsterile syringes and needles is very high (34%) according to WHO estimates.10 Prescribers’ non-adherence to clinical guidelines and the essential medicine list can result in poor clinical outcomes and an increase in healthcare costs to the individual and society at large.11 One of the most prevalent irrational drug use behaviors that lead to poor therapeutic outcomes is the recommendation of inappropriate dosage. Although the World Health Organization (WHO) has recommended that all prescribers should adhere to generic prescribing, the majority of prescribers continue to follow trade/brand name prescribing practices.12 Generic prescribing reduces the likelihood of errors in prescribing and dispensing of medications by utilising a single approved name for each drug, rather than multiple brand names. Irrational medicine prescribing in hospital settings is influenced by multiple factors, such as the work environments of healthcare professionals (HCPs), the drug supply system, the availability of hospital formulary, legal regulations, accessibility of evidence-based information, and profit motives associated with selling medications.13
Drug use is a complex phenomenon. An essential tool is necessary to analyze drug utilization patterns in hospital settings in order to evaluate the appropriateness of drug use at the levels of physicians, patients, and health facilities.5 The WHO core drug use indicators are first-line measures used to evaluate irrational drug use practices in healthcare settings. These indicators are quantitative, feasible, and time-consistent. They have been compared with the standards set by the World Health Organization (WHO) as well as other hospital drug use guidelines and patterns. The WHO core drug use indicators are categorised into prescribing, patient-care, and health-facility indicators.3 The available information indicates that medicines are not used appropriately. Inappropriate drug use significantly impacts the healthcare system’s success, both in terms of health outcomes and economic implications.3
Evidence shows that the majority of the studies on appropriate medication use in Uganda are carried out in public health facilities using the Supervision, Performance Assessment, and Recognition Strategy (SPARS) tool.14–16 This tool was prepared by the Ministry of Health, Uganda to address medicine management in public and non-profit health facilities.17 The scores generated by the SPARS tool can address medicine management issues in Ugandan health facilities, but these scores will not quantify the rational drug use practices. To fill this gap, the current study aimed at assessing the rational prescribing pattern in a secondary care hospital in Sheema District of Western Uganda, using the WHO and the International Network of Rational Use of Drugs (INRUD) indicators.
Materials and Methods
Study Design and Settings
A prospective, hospital-based cross-sectional study was conducted to assess WHO/INRUD indicators among patients attending the outpatient department of a secondary care hospital (Health Centre III) in Sheema District, Western Uganda. The study was conducted over a duration of five months, spanning from January 2023 to May 2023.
Study Population
All patients, irrespective of gender, aged 18 years or older, attending the outpatient department for the treatment of acute or chronic illness, and expressed willingness to participate in the study are considered for inclusion.
Ethical Considerations
The KIU Research and Ethics Committee (KIU-REC 2023–014) granted approval for the study protocol, data collection tools, and informed consent procedure. The present investigation was carried out in adherence to the guidelines outlined in the Declaration of Helsinki pertaining to the ethical conduct of research involving human participants.
Sample Size and Sampling Technique
Epi-Info Statistical Software (Centre for Disease Control, USA) was used to determine the sample size (n = 384), considering that 50% of prescriptions were in accordance with WHO/INRUD prescribing standards, a 95% confidence level, 80% power, and a 5% margin of error. Considering that 5% of prescriptions had missing information, the final sample size was 403 for prescribing and patient-care indicators.
Data Collection Tool
The data collection tool comprised two components: 1. Demographic and clinical characteristics; and 2. WHO/INRUD core drug use indicators:
Demographics and Clinical Characteristics
Demographics and clinical characteristics such as age, sex, diagnosis, and recommended treatment were included in this section.
WHO/INRUD Core Drug Use Indicators
The WHO/INRUD core drug use indicators were classified into three categories: prescribing indicators, patient-care indicators, and health-facility indicators. Prescribing indicators were used to assess medication prescribing patterns within healthcare settings. These included the average number of drugs prescribed per encounter, the percentage of drugs prescribed by generic name, the percentage of antibiotics prescribed, the percentage of injections prescribed, and the percentage of drugs prescribed from the Essential Drugs List (EDL).
Patient-care indicators were employed to evaluate the quality of care delivered to patients, specifically in relation to consultation, dispensing, drug labeling, and patient counseling. These included the average consultation time, the average dispensing time, the percentage of drugs dispensed, the percentage of drugs adequately labelled, and the percentage of patients having adequate knowledge about the drugs dispensed. The study tool included health facility indicators, such as the presence of the Essential Medicines List (EML) or hospital formulary copy, and the percentage of key drug availability. These indicators were used to evaluate the level of hospital support in promoting rational drug use.
Data Collection
A total of 450 prescriptions were prospectively collected from eligible patients at the Hospital’s outpatient pharmacy department. Prescription records were analysed using the WHO/INRUD methodology.13 Two pharmacy students were trained to capture and record the patient consultation time outside the consultation room and dispensing time outside the pharmacy. Patients were interviewed at the pharmacy outlet to assess their adequate knowledge about dispensed drugs (name of the drug, indication, and administration). Data on the availability of key drugs in the pharmacy were assessed by filling a checklist of 50 key drugs in the presence of a pharmacist and a medical officer.
Data Analysis
The collected data were entered into a spreadsheet and analyzed. The WHO/INRUD core drug use prescription, patient care, and health facility indicators are expressed in terms of frequency, proportion, and average. All estimated indicators were compared to the criteria set by the World Health Organization (WHO).
All WHO/INRUD core drug use indicators were converted into indices measures in order to provide a comprehensive assessment of drug utilisation within the healthcare system. The indices of non-polypharmacy, rational antibiotic use, and safe injection drug use were determined by dividing the WHO standard value by the observed value. The indices of drugs prescribed from the EDL, consultation time, dispensing time, drugs dispensed, drugs adequately labeled, patients’ knowledge of correct dosage, availability of a copy of the EML, and key drugs available in stock were calculated by dividing the observed value by the WHO standard value.13
Results
Prescribing Indicators
The study findings revealed that the average number of drugs prescribed per encounter was 3.2, which is higher than the WHO reference value (1.6–1.8). The percentage of drugs prescribed by the generic name (90.48%) and in the Essential Medicine List (96.23%) was close to the WHO reference value (100%). The percentages of antibiotics (66.22%) and injections (25.22%) per encounter were beyond the WHO standards (antibiotics = 20.0–26.8%; injections = 13.4–24.1%). Table 1 displays the distribution of WHO/INRUD prescribing indicators at Sheema Secondary Hospital.
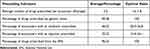 |
Table 1 WHO/INRUD Prescribing Indicators in Health Centre III of Western Uganda (n=450) |
Patient-Care and Health-Facility Indicators
The results obtained from the analysis of patient-care indicators indicate that the average consultation time was 5.41 minutes, the average dispensing time was 131.03 seconds, the percentage of medicines dispensed was 76.11%, the percentage of medicines adequately labeled was 59.74%, and the percentage of patients who possessed knowledge about the correct dosage was 49.50%. It is worth noting that these values did not meet the established reference standards set by the World Health Organization (WHO). Facility indicators such as the percentage of key medicines available in stock (66.67%) were short of the WHO optimal value. The hospital provided full access (100%) to the Essential Medicine List (EML) for practitioners to support rational prescribing practices. The distribution of the WHO/INRUD patient care and health facility indicators at Sheema Secondary Hospital is presented in Table 2.
 |
Table 2 WHO/INRUD Patient-Care and Health-Facility Indicators in Health Centre III of Western Uganda (n=450) |
WHO/INRUD Performance Index
The findings of the performance index revealed that the Index of Rational Drug Prescribing (IRDP), the Index of Rational Patient-Care Drug Use (IRPCDU), and the Index of Rational Drug Supply (IRDS) had values of 3.71, 3.11, 1.67, and 8.49, respectively. The distributions of performance index indicators and their optimal values are presented in Table 3.
 |
Table 3 Drug Use Performance Indicators in Health Centre III of Western Uganda (n=450) |
Discussion
Irrational drug use practices exist worldwide and exert a significant impact on patient’s clinical and economic outcomes.18 This is the prime study conducted in Uganda, which aimed to address rational drug use practices. The study utilised WHO core drug use indicators in a secondary care hospital situated in Sheema District of Western Uganda. The findings of this study provide baseline information on drug use in hospital settings, which helps in resolving problems with drug therapy. The current findings were compared with the findings of ten studies that were conducted in developing and translational countries, displayed in Table 4.
 |
Table 4 Comparison of WHO/INRUD Indicators with Different Countries |
Prescribing Indicators
A prescription is a medical instruction written and authorised by a physician, which reflects their approach to the patient’s disease and the healthcare system in the country.28 The findings of the current study indicate that the average number of drugs per encounter was 3.2, which exceeds the WHO standard of 1.6–1.8. Evidence demonstrates that an increase in the number of drugs per prescription is closed linked to the risk of developing drug interactions, ADRs, and healthcare costs.29 It is vital to educate practitioners so that they may prescribe drugs in accordance with the guidelines, formularies or essential drug list (EDL). This will result in a reduction in the number of drugs prescribed, thereby further reducing the risk of drug-induced morbidity. Contrary to our findings, the average number of drugs per encounter was low in developing countries like Ethiopia (1.69) and Eritrea (1.78).19,22 However, the average number of drugs per encounter was reported to be high in developing and developed countries such as India (3.2), Sudan (2.5), Pakistan (3.4), Saudi Arabia (2.4), Egypt (2.5), Nigeria (2.76), Kenya (2.9), and UAE (4.9).13,20,21,23–27 The diversity in the average number of drugs per encounter in different countries may be attributed to changes in national drug policies and prescribing practices in each country. There are several common reasons for the higher number of drugs per prescription. These reasons may include unavailability or non-adherence to clinical practice guidelines, marketing promotional incentives to prescribers, a lack of continuous medical education in RDU, and a shortage of therapeutically correct drugs.
The World Health Organization strongly recommends that all practitioners should prescribe medicines using generic names (100%) in order to decrease dispensing errors and foster improved communication among healthcare professionals.13 The findings of the current study reveal that the majority of the drugs were prescribed using generic names (90.48%), which is closer to the optimal value of 100% recommended by the WHO. Though most practitioners adhere to standard prescribing practices, there are still a few who prescribe using brand names. To minimize this, continuous educational programmes should be organised. Studies have also reported that generic prescribing practices are low in developing countries such as India (74.6%), Sudan (44.1%), Pakistan (71.6%), Saudi Arabia (61.2%), Nigeria (78.02%), and Kenya (27.70%).13,20,21,24–26 Similar to our study findings, the percentage of generic prescriptions was closer to the WHO optimal value in countries such as Ethiopia (95.60%), Eritrea (94.86%), and Egypt (95.40%).19,22,23 The generic prescribing in UAE was found to be 100% which met the WHO reference value.27 The variation observed in generic prescribing among different studies may be due to the faith of prescribers in a specific branded drug, extensive marketing promotional activity that can influence the decision of prescribers, and non-adherence with national or international regulatory guidelines on rational prescribing practices.
According to the findings of the study, the percentage of antibiotics prescribed per encounter was found to be 66.22%, which was higher than the optimal range of value of 20.0 to 26.8% recommended by the WHO. The majority of the studies conducted in developing and developed countries reported a higher percentage of antibiotics prescribed per encounter than the WHO optimal value.13,19–27 Irrational antibiotic use is a global problem that leads to microbial resistance, adverse drug effects, and hospitalisations.30 In developing countries, the overuse and misuse of antibiotics are major health concerns. This is primarily due to the lack of adequate laboratory facilities for screening culture sensitivity and resistance testing, which hinders the selection of appropriate antibiotic therapy.31 This situation inclines practitioners to prescribing broad-spectrum antibiotics to cover suspected bacterial infections. The overprescription of antibiotics can be attributed to several factors, including the absence of a comprehensive national antibiotic policy, the absence of antibiotic treatment guidelines within hospital settings, and prevailing cultural beliefs within the community.31
The study findings revealed that the percentage of prescriptions comprising injections was 25.22%, which is almost equal to the upper limit of the WHO optimal value range of 13.4–24.1. Similar to our study findings, the majority of the developing countries such as Ethiopia (15.90%), Kenya (24.90%), Sudan (12.0%), and India (11.4%) also showed that a percentage of prescriptions comprising injections within the WHO optimal value.19,20,25,26 A study conducted in UAE reported 16.9% of prescription comprising injections.27 However, some countries such as Pakistan (27.1%) and Ghana (80.0%) reported a high percentage of prescriptions with injections.13,32 Use of injections in place of oral formulations may increase the risk of blood-borne infections and ADRs.33 Also, injections are expensive than oral formulations. Evidence shows that patients sometimes compel physicians to prescribe and administer injections instead of oral formulations because they believe that injections can completely cure the disease and provide quick relief.13
The findings of this study showed that the percentage of drugs prescribed from the EML was 96.23%, which was close to the WHO optimal value of 100%. A study conducted in UAE reported that 100% of the drugs were prescribed from EML.27 The majority of studies conducted in developing countries reported that prescriptions from the EML constitute more than 90%.13,19,20,22–26 However, a few practitioners were non-adherent to the EML guidelines in prescribing medicines. Prescribing medicines from the EML will promote safe, effective, and economic drug use.34 However, if essential medicines are unavailable, practitioners may opt for non-EML prescribing practices and that option may increases prices of some drugs.
Patient-Care Indicators
The findings of the current study demonstrate that the average consultation time was 5.41 minutes, which was below the optimal time of equal or greater than 10 minutes. The study reported that the primary factor contributing to the short consultation duration was the high patient-to-physician ratio. A short consultation time was also observed in various studies conducted in developing countries, such as India (3.9), Sudan (2.9), Pakistan (2.2), and Kenya (4.1).13,20,25,26 According to the WHO, it is recommended that a consultation time of 10 minutes be allocated to ensure thorough history-taking, physical examinations, accurate diagnosis, and prescribing, as well as effective patient education. Indeed, optimal consultation time encourages good physician-patient interactions that can enable accurate diagnosis and rational drug therapy. Evidence shows that the short consultation time is a consequence of the heavy workload of physicians.13 Increasing the number of physicians per patient load is the only resolution to achieve optimal consultation time in hospital settings.
The current study reported an average dispensing time of 131.03 seconds, which is lower than the WHO optimal value of equal or more than ≥180 seconds. These findings were closer to the findings of studies conducted in Kenya (131.5 seconds), Saudi Arabia (100 seconds), and Sudan (99.5 seconds).20,24,25 However, dispensing time was shorter in Ethiopia (22.8 seconds), Eritrea (36.5 seconds), Egypt (47.4), Pakistan (38.0 seconds), and India (49.3 seconds).13,19,22,23,26 A study conducted UAE reported highest dispensing time of 576 seconds.27 Adequate dispensing time is required for the pharmacist to provide information about the medication regimen, precautions for drug use, untoward effects of drugs, possible drug interactions, and appropriate labeling of dispensed drugs.13 In the current study, short dispensing time is a consequence of heavy patient load observed in hospital settings.
The study findings revealed that 76.11% of drugs were dispensed, which was lower than the WHO optimal value of 100%. Similar findings were also observed in studies conducted in developing countries, such as Kenya (76.3%), Nigeria (76.97%), and Sudan (72.5%).20,21,25 In contrast to our study findings, a higher percentage of drugs were dispensed in a few developing countries, including Ethiopia (81.2%), Eritrea (87.32%), Egypt (95.9%), Saudi Arabia (99.6%), Pakistan (90.9%), and India (98.5%).13,19,22–24,26 The lower percentage of dispensed drugs observed in the current study and in other studies could be due to the unavailability of drugs in stock.
The WHO suggests that drugs that are prescribed should be adequately labelled (optimal value 100%) regarding the drug’s name, dosage, and administration guidelines. The current study revealed that only 59.74% of the drugs were adequately labelled, which was lower than the WHO optimal value. In contrast to our findings, studies conducted in Nigeria and Pakistan reported that 100% of drugs were adequately labeled.13,21 However, studies conducted in developing countries, such as Ethiopia (32.7%), Kenya (22.6%), and Sudan (22.5%), reported a lower percentage of drugs adequately labelled than our study.19,20,25 In our study, heavy patient loads and short dispensing time were the major reasons for the lower percentage of adequately labeled drugs.
Patient knowledge of the correct dosage is important for improving medication, adherence, and outcomes. The WHO recommends that 100% of patients should have correct knowledge of drug dosage.24 In our study, only 49.5% of patients had knowledge about the correct dosage, which was in contrast with the studies conducted in developing countries such as Egypt (94.0%), India (76.7%), Pakistan (62.1%), Saudi Arabia (79.3%), Eritrea (78.8%), and Nigeria (60.0%).13,21–24,26 A study conducted in Sudan reported 22.5%, which was lower than our study.25 In our study, the lower percentage of patients with knowledge of the correct dosage is a consequence of a lack of adequate labeling, short dispensing and consultation times, and a heavy patient load.
Health-Facility Indicators
According to the WHO, all healthcare facilities should provide an EML/formulary to practitioners to promote rational prescribing practices. In our study, we observed that a copy of the EML was available (100%) for practitioners to promote rational prescribing practices. However, the percentage of key drugs available (66.67%) in stock was lower than the WHO optimal value (100%). Similar to our study findings, various studies conducted in developing countries reported 100% availability of the EML/formulary.13,19,22–24,26 A study conducted in a developed country (UAE) reported having electronic formulary system (100%).27 However, countries such as Kenya (20.0%), Sudan (66.7%), and Nigeria (0.0%) reported a very low percentage or non-availability of the copy of EML/formulary.20,21,25 In contrast to our study, the majority of the studies conducted in developing countries showed a higher percentage of key drugs available in stock ranging between 73.4% and 100%.13,19–23,25,26 The procurement/purchase committee in every hospital must follow the EML/formulary and key drugs available in stock to order the purchase of medicines.
Strengths and Limitations
Although the study was cross-sectional, the collection of prescriptions, interviews with patients, and examinations of health facilities were conducted prospectively. Thus, the findings of this study represent real-time drug use practices in the hospital setting. The study was conducted at a secondary care hospital, which is located in the rural settings of Western Uganda. Therefore, the findings of this study may not be extrapolated to other healthcare centers.
Conclusion
The study concludes that the WHO/INRUD prescribing, patient-care, and health-facility indicators deviated from the optimal values in a secondary care hospital located in Western Uganda. However, the availability of a copy of the EML to healthcare practitioners, the percentage of prescriptions from the EML, and generic prescribing were found to be more than 90%. There is a need to organize continuous educational programs on rational prescribing practices for physicians to reduce the overprescribing of antibiotics and injections. The physician-to-patient ratio should be increased to prolong the consultation time for appropriate history taking, physical examination, accurate diagnosis, and rational prescribing. In addition, the availability of key drugs in stock should be improved to promote effective management of disease conditions.
Ethical Considerations
The study protocol, data collection tools, and informed consent procedure were approved by the KIU-Research and Ethics Committee (KIU-REC 2023-014). This study was conducted in accordance with the provisions of the Declaration of Helsinki for research on human subjects. All subjects were informed of the study and its objectives, and informed consent was obtained from each participant.
Acknowledgment
We acknowledge the Hospital Administrator of the Secondary Care Hospital, Sheema District, Western Uganda for providing permission to enroll patients and conduct this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no conflict of interest and no affiliations with or involvement in any organisation or entity with any financial interest (such as honoraria, educational grants, participation in speakers’ bureaus, membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements) or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
References
1. Sisay M, Mengistu G, Molla B, Amare F, Gabriel T. Evaluation of rational drug use based on World Health Organization core drug use indicators in selected public hospitals of eastern Ethiopia: a cross sectional study. BMC Health Serv Res. 2017;17(1):161. doi:10.1186/s12913-017-2097-3
2. Huo H, Li X, Li H, et al. Analysis of rational drug use effect under hospital drug control system. Comput Math Methods Med. 2022;2022:1–6. doi:10.1155/2022/2927606
3. Sisay M, Mengistu G, Molla B, Amare F, Gabriel T, Devi Sagili K. Evaluation of rational drug use based on World Health Organization core drug use indicators in selected public hospitals of eastern Ethiopia: a cross sectional study. BMC Health Serv Res. 2017;17:1–9. doi:10.1186/s12913-017-2097-3
4. Sweileh WM. Global research publications on irrational use of antimicrobials: call for more research to contain antimicrobial resistance. Global Health. 2021;17(1):94. doi:10.1186/s12992-021-00754-9
5. Inform M, Mak D, Wendie TF, Ahmed A, Mohammed SA, Ghaffari F. Drug use pattern using WHO core drug use indicators in public health centers of Dessie. BMC Med Inform Decis Mak. 2021;21:1–10. doi:10.1186/s12911-021-01530-w
6. Kshirsagar NA. Rational use of medicines: cost consideration & way forward. Indian J Med Res. 2016;144(4):502–505. doi:10.4103/0971-5916.200901
7. Ahmed B, Nanji K, Mujeeb R, Patel MJ. Effects of polypharmacy on adverse drug reactions among geriatric outpatients at a tertiary care hospital in Karachi: a prospective cohort study. PLoS One. 2014;9(11):e112133. doi:10.1371/journal.pone.0112133
8. Atif M, Asghar S, Mushtaq I, et al. What drives inappropriate use of antibiotics? A mixed methods study from Bahawalpur, Pakistan. Infect Drug Resist. 2019;12:687–699. doi:10.2147/IDR.S189114
9. Pépin J, Abou Chakra CN, Pépin E, Nault V, Valiquette L. Evolution of the global burden of viral infections from unsafe medical injections, 2000–2010. PLoS One. 2014;9(6):e99677. doi:10.1371/journal.pone.0099677
10. Kanagasabai U, Singh A, Shiraishi RW, et al. Improving injection safety practices of Cambodian healthcare workers through training. PLoS One. 2020;15(10):e0241176. doi:10.1371/journal.pone.0241176
11. Wiedenmayer K, Ombaka E, Kabudi B, et al. Adherence to standard treatment guidelines among prescribers in primary healthcare facilities in the Dodoma region of Tanzania. BMC Health Serv Res. 2021;21(1):272. doi:10.1186/s12913-021-06257-y
12. Melku L, Wubetu M, Dessie B. Irrational drug use and its associated factors at Debre Markos referral Hospital’s outpatient pharmacy in East Gojjam, Northwest Ethiopia. SAGE Open Med. 2021;9:20503121211025144. doi:10.1177/20503121211025146
13. Atif M, Sarwar MR, Azeem M, Naz M, Amir S, Nazir K. Assessment of core drug use indicators using WHO/INRUD methodology at primary healthcare centers in Bahawalpur, Pakistan. BMC Health Serv Res. 2016;16(1):684. doi:10.1186/s12913-016-1932-2
14. Kwesiga B, Wagner AK, Seru M, Ross-Degnan D, Trap B. Costs and effectiveness of the supervision, performance assessment and recognition (SPARS) strategy for medicines management in Uganda. J Pharm Policy Pract. 2019;12(1):36. doi:10.1186/s40545-019-0196-8
15. Trap B, Ladwar DO, Oteba MO, Embrey M, Khalid M, Wagner AK. Article 1: Supervision, Performance Assessment, and Recognition Strategy (SPARS) - A multipronged intervention strategy for strengthening medicines management in Uganda: method presentation and facility performance at baseline. J Pharm Policy Pract. 2016;9(1):21. doi:10.1186/s40545-016-0070-x
16. Ladwar DO, Sembatya MN, Amony NM, et al. Article 4: impact assessment of supervision performance assessment and recognition strategy (SPARS) to improve supply chain management in health facilities in Uganda: a national pre and post study. J Pharm Policy Pract. 2021;14(1):14. doi:10.1186/s40545-020-00290-8
17. Management Sciences for Health. Supervision, performance assessment, and recognition strategy: how SPARS is improving health services across Uganda. Available from: https://msh.org/resources/supervision-performance-assessment-and-recognition-strategy-how-spars-is-improving-health/.
18. Prasad PS, Rudra J, Vasanthi P, Sushitha U, Sadiq MJ, Narayana G. Assessment of drug use pattern using World Health Organization core drug use indicators at secondary care referral hospital of South India. CHRISMED J Health Res. 2015;2(3):223. doi:10.4103/2348-3334.158683
19. Tassew SG, Abraha HN, Gidey K, Gebre AK. Assessment of drug use pattern using WHO core drug use indicators in selected general hospitals: a cross-sectional study in Tigray region, Ethiopia. BMJ Open. 2021;11(10):e045805. doi:10.1136/bmjopen-2020-045805
20. Nyabuti AO, Okalebo FA, Guantai EM. Examination of WHO/INRUD core drug use indicators at Public Primary Healthcare Centers in Kisii County, Kenya. Adv Pharmacol Pharm Sci. 2020;2020:1–7. doi:10.1155/2020/3173847
21. Ogbonna BO, Enyi-Okafor AS, Okoye MI, et al. Assessment of drug use in a tertiary hospital in Southeast Nigeria based on who core drug use indicators. Austin J Nurs Health Care. 2022;9(2):1072–1075. doi:10.26420/austinjnurshealthcare.2022.1072
22. Siele SM, Abdu N, Ghebrehiwet M, Hamed MR, Tesfamariam EH. Drug prescribing and dispensing practices in regional and national referral hospitals of Eritrea: evaluation with WHO/INRUD core drug use indicators. PLoS One. 2022;17(8):e0272936. doi:10.1371/journal.pone.0272936
23. Akl OA, El Mahalli AA, Elkahky AA, Salem AM. WHO/INRUD drug use indicators at primary healthcare centers in Alexandria, Egypt. J Taibah Univ Medical Sci. 2014;9(1):54–64. doi:10.1016/j.jtumed.2013.06.002
24. El Mahalli AA. WHO/INRUD drug prescribing indicators at primary health care centres in Eastern province, Saudi Arabia. East Mediterr Health J. 2012;18(11):1091–1096. doi:10.26719/2012.18.11.1091
25. Ahmed SA, Hamedelniel EI, Yousif AK. Assessing drug use indicators in health insurance facilities, Gezira State, Sudan, 2017–2018. PP. 2021;12(10):237–246. doi:10.4236/pp.2021.1210020
26. Meena DK, Mathaiyan J, Thulasingam M, Ramasamy K. Assessment of medicine use based on WHO drug‐use indicators in public health facilities of the South Indian Union Territory. Brit J Clin Pharm. 2022;88(5):2315–2326. doi:10.1111/bcp.15165
27. El-Dahiyat F, Salah D, Alomari M, Elrefae A, Jairoun AA. Antibiotic Prescribing Patterns for Outpatient Pediatrics at a Private Hospital in Abu Dhabi: a Clinical Audit Study. Antibiotics. 2022;11(12):1676. doi:10.3390/antibiotics11121676
28. Administration (TGA). Prescription medicines overview. Therapeutic Goods Administration (TGA); 2022. Available from: https://www.tga.gov.au/resources/resource/guidance/prescription-medicines-overview.
29. Guthrie B, Makubate B, Hernandez-Santiago V, Dreischulte T. The rising tide of polypharmacy and drug-drug interactions: population database analysis 1995–2010. BMC Med. 2015;13(1):74. doi:10.1186/s12916-015-0322-7
30. Dhingra S, Rahman NAA, Peile E, et al. Microbial resistance movements: an overview of global public health threats posed by antimicrobial resistance, and how best to counter. Front Public Health. 2020;8:535668. doi:10.3389/fpubh.2020.535668
31. Ayukekbong JA, Ntemgwa M, Atabe AN. The threat of antimicrobial resistance in developing countries: causes and control strategies. Antimicrob Resist Infect Control. 2017;6(1):47. doi:10.1186/s13756-017-0208-x
32. Bosu WK, Ofori-Adjei D. An audit of prescribing practices in health care facilities of the Wassa West district of Ghana. West Afr J Med. 2000;19(4):298–303.
33. Hauri AM, Armstrong GL, Hutin YJF. The global burden of disease attributable to contaminated injections given in health care settings. Int J STD AIDS. 2004;15(1):7–16. doi:10.1258/095646204322637182
34. World Health Organization. Promoting rational use of medicines: core components. World Health Organization; 2002.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
