Back to Journals » Open Access Surgery » Volume 15
Evaluation of Factors Affecting Colostomy Closure Outcome in Children: A One-Year Prospective Cohort Study
Authors Aseme S , Negussie T, Tadesse A, Dejene B , Temesgen F, Getachew H, Derbew M, Kiflu W
Received 28 January 2022
Accepted for publication 9 June 2022
Published 15 June 2022 Volume 2022:15 Pages 57—64
DOI https://doi.org/10.2147/OAS.S360157
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Luigi Bonavina
Seblewongel Aseme,1 Tihitena Negussie,2 Amezene Tadesse,2 Belachew Dejene,2 Fisseha Temesgen,2 Hana Getachew,2 Milliard Derbew,2 Woubedel Kiflu2
1Department of Surgery, Defense University College of Health Sciences, Addis Ababa, Ethiopia; 2Department of Surgery, Addis Ababa University School of Medicine, Addis Ababa, Ethiopia
Correspondence: Seblewongel Aseme, Tel +251931284157, Email [email protected]
Background: Colostomy Closure is a routine procedure in pediatric surgery services. It is usually done for indications such as anorectal malformation, Hirschsprung’s disease, and trauma. It is associated with significant complications.
Purpose: To assess the effect of perioperative factors on colostomy closure outcome in children.
Methods: This is a prospective observational study on all children who underwent colostomy closure at Tikur Anbessa Specialized Hospital and Menelik II Referral Hospital from January 2019-February 2020, and Demographic data, nutritional status of the child, duration of mechanical bowel preparation, prophylactic antibiotic, type of anastomosis, operative details, and other perioperative factors were recorded, and patients were followed postoperatively for any complications. Data were entered and analyzed using SPSS 23, and perioperative factors were analyzed using χ2 tests for association with outcome. A p value of < 0.05 was considered statistically significant.
Results: A total of 71 patients were included in the study, and forty-two (59%) were female, and the median age was 2.3 years. A total of 23 complications occurred in 13 (18.3%) patients, and surgical site infection (SSI) was the most common complication occurring in 8 (11.3%) patients. Four (5.6%) patients had anemia which required transfusion, and complete wound dehiscence and adhesive intestinal obstruction each occurred in 1 (1.4%) patient. Duration of surgery > 120 min was associated with an increased risk for postoperative need for transfusion; otherwise, there was no association between other perioperative factors and other complications.
Conclusion: In this study, except for the duration of surgery, none of the other perioperative factors are associated with the complications of colostomy closure, so a guideline for optimal and uniform perioperative care of children undergoing colostomy closure should be prepared.
Keywords: mechanical bowel preparation, surgical site infection, prophylactic antibiotic, colorectal surgery, duration of surgery, anemia, wound class
Introduction
Colostomy closure is a routine procedure in pediatric surgery practice, and it is done for indications, such as anorectal malformation, HSD, perianal injuries, complicated intussusceptions, complicated bowel atresia, and pelvic malignancies.1 It has significant morbidity, and the total morbidity rate of stoma closure in pediatrics ranges from 15 to 55%. These morbidities include surgical site infections, anastomotic leaks, bleeding, anastomotic strictures, and even death.2
It is a question if there is an association between perioperative factors and postoperative complications. SSI is a common and serious complication of colorectal surgeries, and its incidence varies from 0.4 to 45%.3 Mechanical bowel preparation has been the main component of perioperative care, and it is used to lower the rate of postoperative complications. Literature showed varying findings on the effect of mechanical bowel preparation on SSI.4
Although studies are done on the effect of MBP and prophylactic antibiotics on the outcome of colorectal surgeries in adults, in children there are only a few studies are available; besides, very limited data are available about the effect of other perioperative factors, such as child nutritional status, duration of surgery, type of anastomosis, and intraoperative wound class on the outcome of colostomy closure.
This study aimed to assess the effect of perioperative factors on colostomy closure outcome in children.
Methods
This prospective cohort study is conducted on children who undergo colostomy closure at Tikur Anbessa Specialized Hospital (TASH) and Menelik II hospital (MIIH). The two centers are university-affiliated hospitals, where most pediatric surgical cases from all over the country get operated on, and the only pediatric surgery specialty (residency) training center. There were 7 Pediatric surgeons, two pediatric surgery fellows, eight 5th-year pediatric surgery trainees (residents), eight 4th-year, and six 3rd-year residents in the unit.
After getting approval from the Department of Surgery Ethical Committee, we started collecting data. From January 2019 to February 2020, 71 children undergo colostomy closure in the two hospitals, and all parents were willing and gave informed consent to participate in the study, so all were included in the study.
The patients’ Preoperative recorded data included demographic data, stoma characteristics, MBP duration, prophylactic antibiotics, nutritional status, and Hgb level. Operative techniques were documented, including the type of anastomosis, suture material, duration of surgery, and wound class. We followed patients, and all postoperative complications were documented. Data were analyzed for any association between the perioperative factors and complications of colostomy closure. The following complications were noticed, including SSI, wound dehiscence, intestinal obstruction, hospital-acquired pneumonia, and incisional hernia.
Patients were grouped based on their weight to see their nutritional status.
Underweight = was defined based on WHO guideline as a weight for age below − 2SD.
Postoperative significant anemia was defined as a need for blood transfusion due to significant blood loss.
Anemia = Hg below 12mg/dl preoperatively and if postoperative Hg is <9mg/dl.
All children received MBP, and the duration of MBP was variable. The reasons for the variation were the decision of the operating surgical team, and patients who had fecaloma were put on a longer duration of MBP. The MBP protocol of the unit includes Cleansing enema with 10–20mL/kg of Normal Saline BID plus fluid diet.
The intraoperative wound was classified based on the operating surgeon’s judgment as follows
- Clean contaminated: if the bowel was clean with clear content or minimal spillage.
- Contaminated: if there is gross spillage.
- Dirty: if there is significant contamination with feces or if fecaloma is present.
Patients were followed postoperatively in the hospital, and also for one outpatient visit after discharge, which is usually within two weeks after surgery. Patients who did not show up for follow-up were contacted by phone.
Data were recorded prospectively in the structured questionnaire and entered, cleaned, and analyzed using Statistical Package for the Social Sciences (SPSS version 23). Outcomes were compared with χ2 analysis, and a P-value of <0.05 was considered significant.
Result
Perioperative Status
A total of 71 children undergo colostomy closure in the given study period, and all were included in the study, out of which forty-two patients (59%) were female. The median age of the patients in this study was 2.3 years (min 6 months and max 14 years). The most common indication for colostomy opening was Anorectal malformation 62 (87.3%). Forty-nine (69%) colostomies were performed at TASH, and the remaining were referred from other hospitals. The mean time gap between colostomy creation and closure was 26.3 months with a range of 3 months to 14 years. The most common location of stoma was sigmoid colon 65 (91.5%), and 59 (83.1%) of the colostomies were Loop colostomies. Three (4.2%) of the colostomies were end colostomies, and these children were operated in other hospitals with less experience of pediatric surgical conditions. Twelve patients (17%) had experienced stoma-related complications, out of which peristomal excoriation was the most common stoma-related problem. Colostomy was refashioned for six kids for stoma prolapse and parastomal evisceration (please insert Table 1 here).
 |
Table 1 Stoma Characteristics |
Twelve (16.9%) patients had anemia preoperatively, and their mean hemoglobin was 11.9mg/dl. Based on the WHO weight for age curve, 18 (25.4%) were underweight. All patients received mechanical bowel preparation using 20mL/kg cleansing enema BID and were put on a fluid diet. The majority, 40 (56.3%), were prepared for 3 days, and the range of MBP duration was from 2 to 7 days. The reason for the variation of MBP duration was mainly OR cancellation due to time constraints. Those who had fecaloma were put on MBP for a longer duration based on the decision of the operating surgeon.
For all patients, prophylactic antibiotics were given intravenously just before the incision. Fifty-five (77.5%) patients received only ceftriaxone, while metronidazole was added for 16 (22.5%). The mentioned reason for not adding metronidazole for the 55 children was the lack of the drug in the Operation theatre pharmacy. Sixty-three (88.7%) patients had clean-contaminated wounds, while in 2 (2.8%) patient’s colon was loaded with feces with significant contamination. Fecaloma was evacuated from 6 (8.5%) patients’ bowels intraoperatively. Most of the surgeries were performed by 3rd-year and 4th-year pediatric surgery residents under the observation of the senior. A consultant or pediatric surgeon does the procedure in 10 of the patients (please insert Table 2 here).
 |
Table 2 Perioperative Factors: Prophylactic Antibiotics, Wound Class, and Level of Operating Person |
All colostomy closures were done with a vicryl suture. Fifty-two were single-layer anastomosis, and 19 were double-layered anastomosis. Most procedures were performed by pediatric surgery residents, under the observation of a consultant. The number of colostomy closures performed by the residents ranges from 1 to 9 closures, with a median of 3 closures. The mean duration of surgery is 126min ± 34min, and the duration of anesthesia was 144.6min ± 36.5min. The duration of the surgery ranged from 1hr 10min to 4hr and 55min, and the longest duration was taken for a patient who had end sigmoid colostomy done elsewhere, and it was hard to find the short distal stump, which was buried in the pelvis with significant adhesion. Spatulation of the distal bowel was done for 37 (52.3%) patients because of size discrepancies between the proximal and distal bowel. The mean of estimated blood loss by the operating surgeon in our study was 51mL ± 47.6mL.
There was a variation in the initiation of oral feeding and duration of intravenous antibiotics administration depending on the decision of the operating surgeon. Oral feeding was started on the 3rd postoperative day for forty-six (64.8%) patients, but feeding initiation was prolonged for four patients because of ileus. The mean hospital stay was 6.1 ± 2.8days. Postoperative intravenous antibiotics were administered for a different duration as described in the table (please insert Table 3 here).
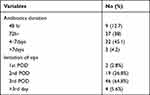 |
Table 3 Postoperative Factors: Antibiotics Duration and Oral Feeding Starting Day |
Outcome
The overall complication rate seen was 23 (32.4%), and these 23 complications occurred in 13 patients. The most common complication was surgical site infection, and it occurred in 8 (11.3%) patients. Eight patients developed anemia (Hgb <9g/dl), out of which 4 (5.6%) required transfusion. Three (4.2%) patients had an incisional hernia. Six (8.5%) patients had hospital-acquired pneumonia during their postoperative period, and they were treated with parenteral antibiotics. Postoperative ileus beyond the 3rd postoperative day occurred in 4 (5.6%) patients, but as it is regarded as a benign postoperative complication, it is not included in the overall morbidity rate. Mechanical adhesive intestinal obstruction occurred in 1 (1.4%) patient, and it responded with conservative treatment. There was no anastomotic leak, intra-abdominal abscess collection, or mortality in our patients (please insert Table 4).
 |
Table 4 Postoperative Complications |
Association Between Perioperative Factors and Complications of Colostomy Closure
There was no identified preoperative risk factor for surgical site infection in our study. None of the perioperative factors are associated with SSI, specifically, anemia, being underweight, wound class, duration of surgery >120 min, level of operating surgery trainee, age, sex, and MBP Duration < or >2days. Antibiotic administration beyond 3 days did not decrease the risk of SSI. None of the patients who took metronidazole + ceftriaxone as prophylactic antibiotics developed SSI, but this was not statistically significant (p value= 0.105).
Postoperative significant anemia was defined as anemia requiring transfusion in the postoperative or intraoperative period. Being underweight and having preoperative anemia was associated with an increased need for blood transfusion, and also operation time >120min increases the risk of postoperative anemia (p-value 0.001, 0.008, 0.001).
Postoperative hospital stay was longer in those patients who had SSI, anemia, and hospital-acquired pneumonia (please insert Table 5).
 |
Table 5 Association Between Perioperative Factors and Complications of Colostomy Closure |
Discussion
Colostomy closure is associated with significant morbidity. Earlier studies in the 1970s showed a complication rate as high as 45–55%.5 Out of the 71 patients, 21 (29.6%) had 1 or more morbidity, and the overall morbidity in our study was 23 (32.4%). This was lower when compared with other studies done by Chandramouli and Hassan which noted an overall morbidity of 39.3% and 46.3%, respectively.5,6 Pena reported a much lower rate of morbidity, 1.5%, in a retrospective study of 628 patients over 28 years.1 The complications noted in the literature and also in our study were SSI, incisional hernia, adhesive intestinal obstruction, and anemia. Our study had included hospital-acquired pneumonia as a postoperative complication, but it had not been mentioned in other studies.
Wound infection is the most common complication of stoma closure. In the literature, SSI rate of colorectal surgeries is more than 25%.3 In this study, SSI occurred in 8 (11.3%) of the patients, out of which one patient developed complete wound dehiscence and required wound closure. The wound infection rate of colostomy closure from recent studies was 10–16%. Chandramouli’s study from India revealed 9.9% SSI rate, and a study from Nigeria on 55 patients had a 10.9% SSI rate.5,7 A prospective study by Hassan on 106 patients showed a higher wound infection rate of 28.3%.6
MBP and antibiotics were introduced as prophylactic measures for wound infection in 1970.5,8 There is controversy about the benefit of MBP in colorectal surgeries. In a retrospective comparative study of 272 children who underwent colostomy closure, the group with bowel preparation had a higher rate of SSI and prolonged hospital stay than the non-preparation group (14.4%Vs 5.8%).9 A study from the USA using MBP for colostomy closure showed a wound infection rate of 14%, while another study was done comparing SSI in bowel preparation and no preparation group and the SSI rate was (15% VS 5%).10,11 Although only a few comparative studies were done in children, the studies showed avoiding MBP in colorectal surgeries had no deleterious complications. But still, most pediatric surgeons continued to use MBP.4 In a 2017 review of 32,359 adult patients by Sarah Koller at the American college of surgeons revealed that MBP+ oral antibiotics decreased SSI. In this study, the use of MBP + oral antibiotics was associated with a lower risk of SSI, anastomotic leak, and postoperative ileus.12
All children received MBP because it is the department guideline. So we could not omit MBP. We compared its effect based on its duration. Polyethylene glycol (PEG) is recommended for MBP, but PEG was not available here. So we used normal saline (NS) for bowel preparation. A study by Emanuel on 55 children showed that a one-day bowel preparation with saline was as effective as the 3-day preparation with no increased risk of SSI.7 The duration of MBP in our patients ranged from 2 to 7days. There was no difference in the intraoperative wound cleanness and SSI rate based on the duration of MBP. Thus, extending MBP duration above 2 days did not reduce the risk of SSI rate in our study.
A systemic review of the literature revealed that administering prophylactic antibiotics parenterally decreased SSI in colorectal surgeries. The surgical care improvement project (SCIP) recommends administering 2nd-generation cephalosporin as single-agent prophylaxis. The WHO recommends cephalosporin with metronidazole in colorectal surgeries. Studies revealed multi-agent prophylactic antibiotics to be superior in SSI prevention.3 In this study, all of them were given parenteral antibiotics before incision. Out of which, 16 (22.5%) got ceftriaxone + metronidazole, whereas the others received only ceftriaxone. Although it was not statistically significant, none of the 1st groups developed SSI. The administration of antibiotics for more than three days did not reduce the risk of SSI, and this finding was similar to other studies.13
The mean operation duration was 126min ± 34 min, and the mean in other studies ranges from 120 to 162 min. There are mixed results regarding the association between surgery duration and SSI. In the study by Daniel Gonzalez, operation duration >105min was an independent risk factor for SSI,19 while in another study, longer duration did not increase SSI rate.2 In our series, there was no association between SSI and surgery duration, and also, age, gender, being underweight and preoperative anemia did not affect the rate of SSI in our study which is similar to the report by Hira.14 However, operation duration >120min was associated with an increased risk of postoperative anemia.
The mean of estimated intraoperative blood loss by the operating surgeon was 51mL ± 47.6mL. Eight (11.3%) patients developed anemia postoperatively out of which 4 required transfusions. Other factors associated with postoperative anemia in our study included being underweight and the presence of significant intraoperative adhesion. Patients who developed postoperative anemia had longer postoperative hospital stay than the non-anemic group, which was 8.63days.
There are different anastomosis techniques to do intestinal surgeries, but studies revealed that using different techniques or different suturing materials for bowel anastomosis has no impact on the outcome of the surgery. A comparative study was done in Mexico on 88 patients by comparing two groups with double layer and single layer intestinal anastomosis, and the outcome was similar in both groups. Another study by Brain showed that single layer extra mucosal anastomosis is safe in pediatrics.15,16 In our study, no association was found between the type of anastomosis and complications. Single layer anastomosis had a lower mean of operation duration than double-layer anastomosis (121min vs 131min).
Incisional hernia occurred in 3[4.2%] patients which is similar to other studies like those done by Hassan 3.8% and Chandramouli 1.8%.5,6 Stoma closure is the most common cause of incisional hernia in infants. Some studies mentioned technical factors as a cause of the incisional hernia, and Mullassery found age below six months and wound infection to be risk factors for incisional hernia, but in our study, no association was found.1,17
There was no anastomotic leak or deep space collection in this study, but the anastomotic leak rate in other studies varies from 1% to 5.7%. Only a few series reported had no anastomotic leak or fistula.6,18 Anastomosis leak is a predictor of mortality, and there was no mortality in our study. There were reoperations for two patients, the first one was for complete wound dehiscence with evisceration, and the other was for simple wound closure.
The mean of postoperative hospital stay was 6.1days ± 2.8days, and those who developed hospital-acquired pneumonia and ileus had longer postoperative stay than the others. Post-operative hospital stay from other studies ranges from 5 to 7days.2,19
Conclusion
Different pediatric surgeons have varying practices regarding MBP, prophylactic antibiotic duration, and initiation of Sips for colorectal surgeries. In our study, except for the duration of surgery, none of the other perioperative factors had an association with the complications of colostomy closure, so a guideline for optimal and uniform perioperative care of children undergoing colostomy closure should be prepared and practiced.
Abbreviations
ARM, anorectal malformation; HSD, Hirschsprung’s disease; MBP, mechanical bowel preparation; NS, normal saline; SSI, surgical site infection.
Ethical Approval
We obtained ethical approval from Addis Ababa University, the College of Health Sciences, Department of Surgery’s Research Publication Committee. Verbal consent was obtained from each patient’s parent. This study was conducted in accordance with the Declaration of Helsinki.
Acknowledgment
We would like to express our sincere thanks to the pediatric surgery unit of the department of surgery at Addis Ababa University, College of Health Sciences for encouraging the research.
Funding
The research was partially funded by the school of Addis Ababa University College of Health Sciences, and the fund covered the cost of collecting data and stationaries.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bischoff A, Levitt MA, Lawal TA, Peña A. Colostomy closure: how to avoid complications. Pediatr Surg Int. 2010;26(11):1087–1092. doi:10.1007/s00383-010-2690-6
2. Hakan Y. Ostomy closures in children: variations in perioperative care do not change the outcome. Indian J Surg. 2015;77. doi:10.1007/s12262-015-1212-0
3. Rangel SJ, Islam S, St SD, et al. Prevention of infectious complications after elective colorectal surgery in children: an American Pediatric Surgical Association outcomes and clinical trials committee comprehensive review. J Pediatr Surg. 2015;50(1):192–200. doi:10.1016/j.jpedsurg.2014.11.028
4. Feng C, Sidhwa F, Anandalwar S, et al. Contemporary practice among pediatric surgeons in the use of bowel preparation for elective colorectal surgery: a survey of the American Pediatric Surgical Association. J Pediatr Surg. 2015:1–5. doi:10.1016/j.jpedsurg.2015.04.005
5. Chandramouli B, Srinivasan K, Jagdish S, Ananthakrishnan N. Morbidity and mortality of colostomy and its closure in children. J Pediatr Surg. 2004;39(4):596–599. doi:10.1016/j.jpedsurg.2003.12.016
6. Hassan KQ. Colostomy closure in Pediatric Age Group: analysis of out come in single-center experience. J Fac Med Baghdad. 2018;60:1. doi:10.32007/jfacmedbagdad.60133
7. Ameh EA, Lukong CS, Mshelbwala PM, Anumah MA, Gomna A. One-day bowel preparation in children with colostomy using normal saline. Afr J Paediatr Surg. 2011;8(3):291–294. doi:10.4103/0189-6725.91670
8. Rickwood AM, Hemalatha V, Brooman P. Closure of colostomy in infants and children. Br J Surg. 1979;66:273–274. doi:10.1002/bjs.1800660417
9. Serrurier K, Liu J, Breckler F, et al. A multicenter evaluation of the role of mechanical bowel preparation in pediatric colostomy takedown. J Pediatr Surg. 2012;47(1):190–193. doi:10.1016/j.jpedsurg.2011.10.044
10. Breckler FD, Rescorla FJ, Billmire DF. Wound infection after colostomy closure for imperforate anus in children: utility of preoperative oral antibiotics. J Pediatr Surg. 2010;45(7):1509–1513. doi:10.1016/j.jpedsurg.2009.10.054
11. Leys CM, Austin MT, Pietsch JB, Lovvorn HN, Pietsch JB. Elective intestinal operations in infants and children without mechanical bowel preparation: a pilot study. J Pediatr Surg. 2005;40:978–982. doi:10.1016/j.jpedsurg.2005.03.013
12. Koller SE, Bauer ÃKW, Egleston BL, et al. Comparative effectiveness and risks of bowel preparation before elective colorectal surgery. Ann Surg. 2017:1–9. doi:10.1097/SLA.0000000000002159
13. Akgiir FM, Tanyel FC, Biiyiikpamukqu N, Hiqsrnmez A. Pediatric Prophylactic antibiotics for colostomy closure in children. Pediatr Surg Int. 1992;279–281. doi:10.1007/BF00183980
14. Ahmad H, Nordin AB, Halleran DR, et al. Decreasing surgical site infections in pediatric stoma closures ☆. J Pediatr Surg. 2020;55(1):90–95. doi:10.1016/j.jpedsurg.2019.09.058
15. Bracho-Blanchet E, Nieto-zermetio J, Reyes-Retana R, Tovilla-Mercado JM, Leon-Villanueva V. Intestinal anastomosis in children: a comparative study between two different techniques. J Pediatr Surg. 1998;33(12):1757–1759. doi:10.1016/S0022-3468(98)90279-2
16. Ross AR, Hall NJ, Ahmed SA, Kiely EM. The extra mucosal interrupted end-to-end intestinal anastomosis in infants and children; a single surgeon with 21 years of experience ☆. J Pediatr Surg. 2015;51(7):1131–1134. doi:10.1016/j.jpedsurg.2015.11.018
17. Mullassery D, Pedersen A, Robb A, Smith N. Incisional hernia in pediatric surgery – experience at a single UK tertiary center. J Pediatr Surg. 2016;10–13. doi:10.1016/j.jpedsurg.2016.06.013
18. Kiely EM, Sparnon AL. Stoma closure in infants and children. Pediatr Surg Int. 1987;2:9–11. doi:10.1007/BF00174181
19. Gonzalez DO, Ambeba E, Minneci PC, Deans KJ, Nwomeh BC. ScienceDirect Surgical site infection after stoma closure in children: outcomes and predictors. J Surg Res. 2016;209:234–241. doi:10.1016/j.jss.2016.10.029
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
