Back to Journals » Hepatic Medicine: Evidence and Research » Volume 15
Epidemiology of Hepatitis B in Saudi Arabia from 2006 to 2021
Authors Alghamdi IG , Alghamdi RM, Alghamdi MS, Alghamdi AM, Alghamdi MI, Alghamdi ZI, Alghamdi KS
Received 20 September 2023
Accepted for publication 15 December 2023
Published 21 December 2023 Volume 2023:15 Pages 233—247
DOI https://doi.org/10.2147/HMER.S438099
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Gerry Lake-Bakaar
Ibrahim G Alghamdi,1 Rahaf M Alghamdi,2 Mohamed S Alghamdi,3 Atheer M Alghamdi,3 Murad I Alghamdi,4 Ziyad I Alghamdi,5 Khalil S Alghamdi6
1Public Health Department, College of Applied Medical Sciences, University of Al-Baha, Al-Baha city, Saudi Arabia; 2Laboratory Medicine Department, College of Applied Medical Sciences University of Al-Baha, Al-Baha city, Saudi Arabia; 3General Directorate of Health Affairs Al-Baha, Ministry of Health, Al-Baha city, Saudi Arabia; 4College of Medicine, University of Al-Baha, Al-Baha city, Saudi Arabia; 5College of Clinical Pharmacy, University of Al-Baha, Al-Baha city, Saudi Arabia; 6General Directorate of Health Affairs Jeddah, Ministry of Health, Jeddah City, Saudi Arabia
Correspondence: Ibrahim G Alghamdi, Public Health Department College of Applied Medical Sciences, University of Al-Baha, Prince Mohammad Bin Saud, Al-Baha, Al-Baha city, 65527, Saudi Arabia, Email [email protected]
Background: This study describes the epidemiological pattern of acute hepatitis B virus (HBV) infection in Saudi Arabia from 2006 to 2021. It explores case frequency and the crude incidence rate (CIR) by year of diagnosis, age group, region, gender, and nationality of patients.
Methods: Retrospective data on acute hepatitis B cases diagnosed across 20 regions of Saudi Arabia during January 2006 to December 2021 were obtained from the Saudi Ministry of Health’s Statistical Yearbook. Statistical analyses were conducted using SPSS version 20.0, employing both parametric and non-parametric tests.
Results: The highest CIR was reported in the regions of Qunfudah, Jeddah, Tabuk, and Taif (28.6, 25.2, 25.1, and 23.4 per 100,000 people). In contrast, the lowest CIR was documented in the regions of Hail, Qurayyat, Jouf, and Hafr AL-Baten (3.6, 3.5, 2.9, and 1.2 per 100,000 people). Incidence rates were notably elevated in those aged 45 years and above (30.6 per 100,000 individuals), followed by the 15– 44 age group (14.2 per 100,000 individuals), and were lowest in children aged 0– 14 years (0.8 per 100,000 individuals). Regarding gender differences, HBV infection rates were 1.4 times higher in Saudi males than females and 2.2 times higher in non-Saudi males compared to females. Overall, Saudi nationals had a 4.2 times higher HBV infection rate than non-Saudis during the study period.
Conclusion: This study highlights diverse acute Hepatitis B infection rates across Saudi regions, with higher rates in Qunfudah, Jeddah, Tabuk, and Taif, and lower rates in Hail, Qurayyat, Jouf, and Hafr AL-Baten. Predominance among ages 45+, followed by 15– 44, and lowest in 0– 14 age groups was observed. Gender variations showed notably higher rates in Saudi and non-Saudi males. The notably higher prevalence among Saudi nationals implies key considerations for public health strategies.
Keywords: Hepatitis B virus, Saudi Arabia, retrospective study, epidemiology, incidence
Introduction
Hepatitis B is an infectious liver virus that can be contracted through exposure to the blood or other bodily fluids of an infected individual.1 Despite the existence of effective vaccines and treatment strategies for hepatitis B, it continues to pose a significant global health challenge, potentially resulting in acute and chronic conditions, severe liver failure, and even malignancy. This complex health scenario contributes to elevated rates of morbidity and mortality.2 According to the World Health Organization (WHO), the worldwide impact of hepatitis B virus remains substantial. In 2015, an estimated 257 million individuals were afflicted with chronic hepatitis B virus (HBV) infection, constituting a global prevalence ranging from 3% to 5%. Alarmingly, this health burden translated into approximately 887,000 fatalities attributable to liver-related complications stemming from chronic HBV infection.3 Notably, the WHO’s data revealed that in 2019, there were around 296 million people living with HBV infection, with an additional 1.5 million new cases being diagnosed during that year.4 This persistence and the ongoing emergence of new cases underscore the urgent need for continued efforts in prevention, diagnosis, and treatment of hepatitis B on a global scale.
Globally, the prevalence of chronic hepatitis B virus (HBV) infection exhibits significant variation. The WHO’s Global Hepatitis Report of 2017 reveals distinct patterns across regions. The Western Pacific region (6.2%) and Africa (6.1%) exhibit the highest rates of chronic HBV infection. Meanwhile, prevalence rates are intermediate in the Eastern Mediterranean region (3.3%), lower in Southeast Asia (2%) and Europe (1.6%), and least in North and South America (0.7%).5 While the impact of vaccination has led to a reduction in HBV burdens in developed nations, the prevalence of HBV remains notably elevated in endemic regions. This phenomenon is primarily attributed to vertical transmission from mother to child and early-life exposures, perpetuating the prevalence of HBV.6
As previously mentioned, countries situated in the Middle East are categorized as having intermediate endemicity for hepatitis B virus (HBV) due to their prevalence rates falling between 2% and 8%. This can be attributed to factors such as political instability and inadequate healthcare infrastructure that have disrupted effective vaccination campaigns in some of these regions.7 Given the potential challenges in gathering precise epidemiological data, the assessment of HBV prevalence among blood donors has emerged as an attractive approach in these areas due to the considerable number of individuals involved.8 A comprehensive review study conducted in 2016 yielded valuable insights into the prevalence of HBV among blood donors across the Middle East. The study revealed an average HBV prevalence of 1.62% among blood donors in the region. Notably, the pooled prevalence rates of HBsAg, a marker of HBV infection, were as follows for specific countries: Iraq, 0.67%; Jordan, 1.72%; Saudi Arabia, 3.02%; Lebanon, 0.92%; Cyprus, 3.00%; Iran, 0.58%; Turkey, 1.68%; Yemen, 5.05%; and Kuwait, 1.92%.9
Saudi Arabia was previously described as a highly endemic area for HBV infection in the Middle East.10 A great number of studies have been undertaken in Saudi Arabia, and a systematic review that pooled data from 36 studies reported between 1965 and 2013 discovered a prevalence of 3.2% in the region. A more recent systematic review conducted by Aljumah et al in 2019 estimated the prevalence of HBV infection in Saudi Arabia to be approximately 1.3%.10,11 The decline in the prevalence of the infection is attributed to the launch of HBV vaccination programs in 1989 for all newborns and in 1990 for all school children. It has also been influenced by the development of healthcare facilities and the improvement of socioeconomic standing.10
Compared to adults, children affected with HBV are at greater risk of developing a chronic infection and have poor health outcomes over the long run. Vaccination and anti-HBV drugs, such as interferons and nucleoside analogs, are available for the prevention and management of infection, but their efficacy is limited, and they frequently produce severe side effects.1 In addition, there is still a substantial elderly population that was infected prior to the introduction of large-scale vaccination programs. This large, infected population nevertheless contributes significantly to the worldwide burden of disease due to the high risk of deterioration to cirrhosis, HCC, and mortality.12
As recognition of the hepatitis B virus infection continues to increase, especially in Saudi Arabia, identification of the virus’s epidemiological pattern has become crucial. Therefore, the present retrospective study aims to analyse the epidemiological pattern of the acute hepatitis B virus in the different regions of Saudi Arabia between the years 2006 and 2021.
Methods
Study Setting and Population
This retrospective, descriptive study spanned the entirety of reported cases of acute Hepatitis B Virus (HBV) infection in Saudi Arabia from January 2006 to December 2021.
Study Design and Study Duration
The study’s retrospective design encompassed a comprehensive analysis of epidemiological data pertinent to acute HBV infection trends across diverse cohorts in Saudi Arabia. It spanned a significant 16-year duration, from 2006 through 2021.
Data Collection
The primary data source utilized for this investigation was the Statistical Yearbook of the Saudi Ministry of Health (MoH). This esteemed resource provided an exhaustive array of health-related statistics and indicators within the Kingdom. The study involved a meticulous retrospective review of all acute HBV infection cases officially reported in Saudi Arabia during the stipulated period (January 2006 to December 2021 The data are publicly available and readily accessible through the Statistical Yearbook of Saudi MoH; therefore, no ethical approval was required for the study. The most recent available Saudi MoH Statistical Yearbook dates back to 2021.
Within the specified time frame, the study incorporated a total of 79,282 documented cases of Hepatitis B, averaging 4955 cases annually. This data compilation encompassed detailed and comprehensive information for 20 distinct regions within Saudi Arabia, delineating the number of diagnoses for acute Hepatitis B cases (prevalence) and the calculation of the crude incidence rate (CIR). The CIR was formulated as the count of new Hepatitis B cases occurring per 100,000 individuals within a specific population over a single year.
Study Measurements
The investigation meticulously collated data encompassing the number of diagnoses and the crude incidence rate (CIR) for acute Hepatitis B. The stratification of this information was based on several key variables, including the year of diagnosis, age group, Saudi Arabian region, gender, and patient nationality (Saudi or non-Saudi).
Data Management and Analysis
Data were analysed using the Statistical Package for the Social Sciences (SPSS), version 20.0 (IBM Corporation, Armonk, NY, USA). Descriptive analysis of the epidemiological data was performed by calculating the overall population diagnosed with acute hepatitis B and the CIR stratified by year of diagnosis, age group (less than 1 year, 1–4 years, 5–14 years, 15–44 years, and 45 years and over), region, sex, and nationality (Saudi or non-Saudi). In addition, the age specific incidence rate of acute hepatitis B was calculated for the year 2021.
The differences in CIR between Saudi Arabian regions as reported by the 2006 to 2021 Statistical Yearbooks were used to study geographic distribution patterns of acute hepatitis B in the country. An independent sample t-test was used to compare the CIR of acute hepatitis B among Saudi and non-Saudi nationals. The Shapiro–Wilk test was used to assess the normality of the CIR of acute hepatitis B among Saudi and non-Saudi nationals. It evaluates whether a given sample of data comes from a normally distributed population. This test is commonly employed in statistics to determine if data follows a normal distribution. If the p-value associated with the Shapiro–Wilk test is greater than the chosen significance level (commonly 0.05), the null hypothesis (that the data is normally distributed) is accepted, indicating that the data significantly does not deviate from a normal distribution. Lastly, the Kruskal–Wallis analysis was used to compare the CIR of acute hepatitis B among different years of diagnosis, age groups, and regions.
Results
Distribution of Hepatitis B Cases by Year of Diagnosis
From 2006 to 2021, a total of 79,282 acute hepatitis B cases (overall per year = 4955 cases) were registered in the Statistical Yearbooks of Saudi MoH. Over the considered 16-year time period, two peaks in the number of yearly acute hepatitis B cases were observed.
The number of reported cases increased from 4264 in 2006 to 5066 in 2008. This represents a consistent rise over this three-year period, indicating a potential increase in the incidence of acute hepatitis B infections during these years. Between 2008 and 2015, the number of new cases experienced a gradual decrease, dropping to 3486 diagnosed cases in 2015, the year with the lowest number of cases recorded. However, a noticeable increase that more than doubled between 2015 to 2018, peaking in 2018 with a total of 7432 cases diagnosed during that year. Subsequently, from 2019 to 2021, there was a decline in the number of hepatitis B cases, with the year 2020 recording 4314 cases and a slight increase to 4955 cases in 2021. Despite this increase, the numbers remained considerably lower compared to previous years, indicating a trend of declining incidence during this period (Figure 1).
 |
Figure 1 Total number of acute hepatitis B cases in Saudi Arabia from 2006 to 2021. |
Yearly CIRs of acute hepatitis B cases per 100,000 people, stratified by year of diagnosis from 2006 to 2021, reflect the above trends. There was a modest increase in CIR between 2006 and 2008 (18 to 20.4 per 100,000 people), followed by a steady decrease starting in 2009 (CIR=19.8 per 100,000), and reaching the lowest point recorded during the analysed period in 2015, at 11.1 per 100,000 people. The CIR for acute hepatitis B rose sharply between 2015 and 2018, with a new all-time peak in 2018 of 22.2 per 100,000 people. However, from 2019 to 2021, a notable decline in the CIR was observed, with figures reaching 15.7 per 100,000 people in 2020 and showing a slight increase to 18.0 per 100,000 people in 2021 (Figure 2).
 |
Figure 2 Yearly crude incidence rate (CIR) of acute hepatitis B cases in Saudi Arabia from 2006 to 2021. |
Distribution of Hepatitis B Cases by Age Group
The data from the MoH were employed to calculate the average number and percentage of acute hepatitis B cases diagnosed between 2006 and 2021 stratified by age group. Between 2006 and 2021, the highest total number of acute hepatitis B cases were recorded in the 15–44 age group (mean = 3144 cases/year). These values were almost twice that of the second-most affected age group, 45 years and over (mean = 1715 cases/year) (Table 1). The overall number of cases in each age group was different from the other three groups by Kruskal–Wallis analysis (χ2(4, N=79,282) =127,902.563, P-value < 0.001). In contrast, the children age groups (0–14 years) recorded the lowest overall number of acute hepatitis B cases (cumulative mean = 327 cases/year) (Table 1).
 |
Table 1 Total & Overall Number of Acute Hepatitis B Cases by Age Group in Saudi Arabia from 2006 to 2021 |
The Age-Specific Incidence Rate (ASIR) of acute hepatitis B cases for the year 2021 was calculated across distinct age groups to provide a comprehensive understanding of the distribution of cases. Among individuals aged 0 to 4 years, the CIR was 0.8 cases per 100,000 population, with 21 reported cases among a total population of 2,689,431. Similarly, in the age group of 5 to 14 years, the CIR was 0.3 cases per 100,000 population, with 19 cases among 5,686,771 individuals. These findings reflect relatively lower incidence rates in the younger age groups (Table 2).
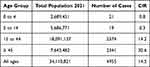 |
Table 2 The Crude Incidence Rate (CIR) of Acute Hepatitis B by Age Group in Saudi Arabia During the Year of 2021 |
On the other hand, the age group of 15 to 44 years exhibited a CIR of 14.2 cases per 100,000 population, with 2574 cases among 18,091,137 individuals. This age range demonstrated a substantial increase in acute hepatitis B cases compared to the younger groups. Notably, the age group of 45 years and older showed the highest CIR of 30.6 cases per 100,000 population, with 2341 cases among 7,643,482 individuals. This pattern shows a greater prevalence of acute hepatitis B cases among older individuals. However, considering all age groups collectively, the overall CIR for acute hepatitis B cases in 2021 was calculated as 14.5 cases per 100,000 population, with a total of 4955 cases among the entire population of 34,110,821.
Distribution of Hepatitis B Cases by Region
The average number of acute hepatitis B cases diagnosed between 2006 and 2021 stratified for the 20 Saudi Arabian regions was calculated from the Statistical Yearbooks of Saudi MoH (Table 3). The region of Jeddah recorded the highest total number of acute hepatitis B cases (a 16-year average of 1010 of hepatitis B cases), followed by Riyadh (840 overall cases), and the Eastern region (586 overall cases). In contrast, the regions of Qurayyat and Hafr AL-Baten (5 overall cases), Jouf (9 overall cases), and Hail (23 overall cases) recorded the lowest prevalence of acute hepatitis B cases in Saudi Arabia. However, the overall number of cases documented in the remaining regions ranged from 47 to 368 (Figure 3).
 |
Table 3 Total & Overall Number of Acute Hepatitis B Cases by Region in Saudi Arabia from 2006 to 2021 |
 |
Figure 3 Overall number of acute hepatitis B cases by region in Saudi Arabia from 2006 to 2021. |
The CIR of acute hepatitis B diagnoses varied substantially between the different regions, as shown in Table 4. The highest CIR was reported in the regions of Qunfudah 28.6 per 100,000 people, Tabuk 25.2 per 100,000 people, Jeddah 25.1 per 100,000 people, and Taif 23.4 per 100,000 people. These regions showed a highest CIR compared with the remaining ones by Kruskal–Wallis analysis (χ2(19, N=320) = 115.500, P-value < 0.001). In contrast, the lowest CIR was documented in the regions of Hafr AL-Baten 1.2 per 100,000 people, Jouf 2.9 per 100,000 people, Qurayyat 3.5 per 100,000 people, and Hail 3.6 per 100,000 people (Figure 4).
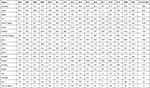 |
Table 4 Overall Crude Incidence Rate (CIR) Acute Hepatitis B Cases per 100,000 by Region |
 |
Figure 4 Overall crude incidence rate (CIR) of acute hepatitis B cases by region in Saudi Arabia from 2006 to 2021. |
Distribution of Hepatitis B Cases by Nationality
From 2006 to 2021, a total of 61,425 acute hepatitis B cases were recorded among Saudi nationals, a mean of 3839 cases/year. Of them, 35,985 (58.6%, mean of 2249 cases/year) were male and 25,440 (41.4%, mean of 1590 cases/year) were female. The CIRs among Saudi nationals, stratified by year of diagnosis and sex, indicate a slight increase from 2006 to 2009 (CIR=19.9 to 23.5 per 100,000 people). This was followed by a steady decrease, with a minimum CIR of 12.9 per 100,000 people in 2015, the lowest recorded in the study period. Between 2015 and 2019, the CIR among Saudi nationals almost doubled, peaking at 24.2 per 100,000 people in 2019. Furthermore, the subsequent years from 2020 to 2021 showed a reverse pattern, indicating a fluctuation in the incidence of acute hepatitis B among Saudi nationals (Table 5 and Figure 5).
 |
Table 5 Overall Crude Incidence Rate (CIR) of Acute Hepatitis B in Saudi Arabia per 100,000 by Nationality |
 |
Figure 5 The crude incidence rate (CIR) of acute hepatitis B in Saudi nationals from 2006 to 2021. |
With regard to non-Saudi nationals, a total of 14,752 acute hepatitis B cases, of which 10,129 were male (68.7%) and 4623 were female (31.3%), were recorded between 2006 and 2021. Average yearly cases were 633/year for males, 289/year for females, and 922/year for both sexes. The CIRs among non-Saudi nationals remained constant between 2006 and 2008 (CIR=12.5 per 100,000), followed by a rapid drop bottoming out at 5.4 per 100,000 people in 2013, the lowest CIR recorded among non-Saudi nationals. The CIR subsequently almost tripled between 2013 and 2018, peaking at 14.9 per 100,000 people in 2018. Similarly, the subsequent years from 2020 to 2021 showed a reverse pattern, indicating a fluctuation in the incidence of acute hepatitis B among non-Saudi nationals (Table 5 and Figure 6). An independent samples t-test was employed to assess the disparity in the CIR of acute hepatitis B between the Saudi and non-Saudi populations. Levene’s test was conducted to assess the equality of variances, yielding a non-significant result (F = 0.226, p = 0.638), indicating the assumption of equal variances was met. The t-test for equality of means demonstrated a significant difference in the CIR between the two groups t(16) = 9.327, P < 0.001).
 |
Figure 6 The crude incidence rate (CIR) of acute hepatitis B in non-Saudi nationals from 2006 to 2021. |
With regard to the male-to-female CIR ratio, acute hepatitis B was found to be 1.4:1 higher among Saudi males than females, and 2.2:1 higher among non-Saudi males than females. Lastly, the overall CIR ratio for acute hepatitis B was 4.3:1 higher in Saudi compared to non-Saudi nationals in the study period.
Discussion
Hepatitis B continues to pose a significant health challenge in Saudi Arabia, demanding a comprehensive approach to enhance patient care and outcomes. Initiating progress towards a more effective strategy for managing Hepatitis B involves conducting a comprehensive epidemiological investigation. In this context, the aforementioned study represents a pioneering effort in offering a comprehensive epidemiological analysis of Hepatitis B incidence in Saudi Arabia. By shedding light on the spatial and temporal patterns of this disease within the Kingdom, this study provides valuable insights to guide future interventions and improve the management of Hepatitis B cases.
In examining the yearly incidence rates of acute hepatitis B cases per 100,000 people from 2006 to 2021, the trends provide a comprehensive insight into the changing dynamics of the disease’s prevalence. The fluctuating trends of acute Hepatitis B incidence rates (CIR) across the study period warrant thorough analysis. The CIR showed a varying pattern, with notable rises and falls over the years. From 2006 to 2008, there was a slight increase of the CIR of acute hepatitis B from 18 to 20.4 cases per 100,000 people. Subsequently, a downward trend was observed, with CIR values steadily decreasing from 19.8 in 2009 to 11.1 in 2015. This decline may reflect successful public health interventions and awareness aimed at reducing Hepatitis B transmission.
In the Kingdom of Saudi Arabia, a significant step was taken in combatting Hepatitis B through the launch of a vaccination program in October 1989. This initiative was aimed at protecting the health of all infants, administering doses at intervals of zero, three, and five months after birth.13 After this, the Saudi government implemented additional HBV vaccination campaigns in 1990 and 1996, strategically targeting unvaccinated children upon school enrolment. Remarkably, these efforts produced an impressive 99% protection rate, which persisted for an extensive eight-year period.11 Furthermore, vaccination is also extended to high-risk groups, such as healthcare workers and individuals with chronic conditions. While vaccination programs have significantly reduced the burden of HBV, fluctuations in its prevalence over the years cannot be entirely attributed to vaccination trends alone. It is essential to acknowledge the potential limitations of relying solely on HBsAg testing in capturing the complete landscape of HBV infections. This testing method may overlook cases of occult hepatitis, characterized by undetectable levels of HBsAg, which could lead to reactivation and contribute to fluctuations in HBV burden.
Several studies conducted globally have consistently demonstrated the effectiveness of vaccination in preventing hepatitis B infection. Notably, vaccination among healthcare workers has emerged as a crucial measure in reducing the transmission of the disease, thereby contributing significantly to the enhancement of public health and overall well-being.14 In a study led by Alshammari et al, it was found that a noteworthy percentage of healthcare workers in Saudi Arabia (83.5%) have received vaccination against Hepatitis B Virus.15 Nonetheless, this figure falls short of the CDC’s 2020 objective in the USA, which aimed for a vaccine coverage surpassing 90%.16
Health education and awareness provided by Saudi MoH may significantly reduce the Hepatitis B Virus (HBV) infection rate in Saudi Arabia from 2009 to 2015. Targeted campaigns provided knowledge on transmission, risk factors, and prevention methods for HBV, empowering individuals to make informed choices. Emphasizing HBV vaccination’s effectiveness, these efforts encouraged immunization for all. Health education also promoted proactive screening, early detection, and timely medical interventions to lower transmission risks.
The increase in the CIR of Hepatitis B in Saudi Arabia from 2015 to 2018 could be attributed to several factors. Firstly, improvements in reporting systems and enhanced surveillance efforts during this period might have contributed to the observed increase. As healthcare systems became more proficient in identifying and reporting cases, the recorded incidence rates may have risen accordingly. Furthermore, Improved healthcare accessibility might have also played a role in the observed increase. Enhanced access to healthcare services could have resulted in more individuals being tested and diagnosed, leading to a higher detection rate and subsequently an increase in reported cases. Changes in risky behaviours among specific population groups, such as unsafe sexual practices or sharing needles, might have contributed to the increased transmission during this period as well. Data from the MoH does not distinguish what proportion of diagnoses hail from mandatory screening programs (pre-marital and pre-employment screenings, obligatory testing for healthcare workers, medical students, blood donors and dialysis patients), referral by other specialties (obstetrics and gynaecology, endoscopy, surgery), or referral by general practitioners/internal medicine following symptoms or abnormal liver function test results. Changes in reporting methods or in the efficiency of local testing practices may be responsible for the observed yearly fluctuations. Lastly, increased community education about HBV and improved awareness of the initial symptoms of the disease may contribute to more referrals by general practitioners.
In terms of affected age groups, the incidence of acute hepatitis B in Saudi Arabia is significantly higher in the adult population, with the highest CIR recorded for the over 45 years group, followed by the 15–44 years group. The higher prevalence of hepatitis B virus (HBV) among the adult population in Saudi Arabia might stem from several contributing factors. This trend could relate to the transmission dynamics prevalent among adults, such as exposure in healthcare settings, unsafe injection practices, or cultural practices increasing the risk of infection. Additionally, inadequate vaccination coverage or lower awareness among adults about preventive measures might play a role. Social and behavioral factors, including limited healthcare access or delayed health-seeking behavior among adults, could also contribute to the higher incidence observed in this demographic. Further exploration into these aspects is essential to understand the nuanced reasons behind the increased burden of acute hepatitis B in Saudi Arabia’s adult population. Conversely, the low CIR recorded for the child population (1.1 per 100,000 people for those under 15 years) provides evidence for the effectiveness of the vaccination program for newborns and the catch-up program for children entering school between 1990 and 1996. Our data reflects figures from the 2017 cross-sectional study in the Aseer Region, where prevalence among individuals <15 years was 0.8%, 1.3% among those 15–25 years, and 6.3% among those >25 years.17 While a lag in the trend of diagnosed cases in the population over 30 is to be expected, efforts to optimally implement mandatory vaccination of healthcare workers and voluntary vaccination of high-risk groups may favour such progress.
The study of geographical trends of acute hepatitis B cases provides precious insights into the territorial variability in terms of local testing and reporting practices, vaccine delivery, health education, and socio-economic progress. Regarding the total number of acute hepatitis B cases, the most affected regions were Jeddah, Riyadh, and the Eastern region. However, in terms of CIR, Qunfudah, Tabuk, Jeddah, and Taif reported the highest incidence of HBV infection (CIR = 23.4 to 28.6 per 100,000 people), numbers that are significantly higher compared with lower-incidence regions. The higher CIR would rather point to health education and socio-economic differences among different regions. Regions with a high CIR should therefore be the focus of community-based educational interventions, such as campaigns for HBV awareness and catch-up vaccinations. Conversely, encouraging data were observed for the regions of Hafr AL-Baten, Jouf, Qurayyat, and Hail, all reporting a CIR of acute hepatitis B below 4 per 100,000 people. However, variability in data collection methods, accuracy, and completeness can also influence reported CIR figures, leading to fluctuations from region to region. The decrease in acute hepatitis B CIR in these areas may be attributed to weaknesses in monitoring systems, accuracy, and under-detection of cases. The healthcare system in these regions could potentially be less robust, affecting the ability to effectively identify and monitor cases. Other potential factors include challenges in accessing healthcare services, lack of awareness about the importance of early detection and treatment, and limited healthcare resources available in those areas. It is important to improve awareness, provide support, and allocate healthcare resources in these regions to ensure better rates of combating hepatitis B transmission.
Our results indicate that CIRs of HBV infection have risen again since 2015 and 2013 in Saudis and non-Saudis nationals. The most likely explanations for the re-rising again of CIR of hepatitis B in Saudi Arabia since 2013 and 2015 till the present, are either improvements in reporting systems and enhanced surveillance efforts during this period or illegal immigration to Saudi Arabia especially from Yemen and other countries during Hajj and Umrah. Figures 3 and 4 show that the CIR of acute hepatitis B among Saudis re-rising again from 2015, while in non-Saudis, it increased in 2013, which means that the pattern of the disease in non-Saudis led to a change in the epidemiological trend of acute hepatitis B in Saudi Arabia from a downward trend to an upward trend. Epidemiological studies show that the endemicity of HBV infection is considered very high in Yemen, where the prevalence of positive HBsAG ranges from 8% to 20%, and up to 50% of the populations generally have serological evidence of previous HBV infection.18 In Saudi Arabia, there are approximately 2 million of Yemenis, and this will effect on the epidemiological pattern of hepatitis B in the entire population. In addition, for those people who come for Hajj and Umrah from the areas affected by hepatitis B and do not return to their home countries, may impact to the increase of the CIR of acute hepatitis B in Saudi Arabia. The CIRs stratified by nationality highlighted that Saudis are 4.3 times more affected by acute hepatitis B than non-Saudi nationals. This may reflect differences in immunization programs between the native countries of non-Saudi nationals and Saudi Arabia.
Concerning male-to-female ratios, men were more affected by acute hepatitis B than women among both Saudi (ratio = 1.4) and non-Saudi (ratio = 2.2) nationals. Male dominance in acute hepatitis B infection is well-documented: men are more likely to become chronic carriers of HBV and develop HCC than women, and female HBV carriers generally have lower serum levels of HBsAg and viral DNA titres.19,20
This study investigates the Crude Incidence Rate (CIR) of acute Hepatitis B in Saudi Arabia is essential in shedding light on the disease’s prevalence and trends. However, several noteworthy limitations must be taken into account when interpreting the findings. Firstly, the data used in this study is derived from retrospective sources, which inherently carries the risk of data incompleteness, inaccuracies, and potential biases. These limitations stem from the reliance on historical medical records and reports, which might not consistently capture all instances of acute Hepatitis B cases. Additionally, variations in the quality of medical reporting and diagnostic accuracy over the study period might impact the reliability of the collected data. As a result, the observed trends in the CIR might be influenced by changes in diagnostic practices, public awareness, or healthcare-seeking behaviour rather than representing genuine shifts in disease incidence. Furthermore, a significant constraint of this study lies in its reliance on officially reported cases as the primary source of data. While these reported cases are crucial for disease surveillance and monitoring, they are subject to underreporting due to a variety of factors, such as individuals not seeking medical attention, misdiagnoses, or incomplete reporting procedures. This underreporting can potentially lead to an underestimation of the true disease burden and skew the calculated CIR. Moreover, the study’s focus on reported cases might not fully capture asymptomatic or mild cases that do not come to medical attention. Consequently, the calculated CIR might not accurately represent the actual incidence of acute Hepatitis B in the Saudi Arabian population. To address this limitation, future studies could consider incorporating additional data sources, such as seroprevalence surveys or hospital-based studies, to provide a more comprehensive view of the disease’s prevalence and its impact on public health.
Conclusions
This study offers a deeper understanding of the Crude Incidence Rate (CIR) of acute Hepatitis B in Saudi Arabia from 2006 to 2021. The study’s regional analysis highlights variations in acute Hepatitis B infection rates across different Saudi Arabian regions. The observed differences, with the highest rates recorded in Qunfudah, Jeddah, Tabuk, and Taif, and the lowest rates in Hail, Qurayyat, Jouf, and Hafr Al-Baten. The higher infection rates among individuals aged 45 and over, followed by those aged 15–44 years, and the lowest rates among individuals aged 0–14 years, emphasize the importance of modifying prevention and awareness efforts to these specific age ranges. The significant differences in male-to-female ratios, particularly the higher rates among Saudi males compared to females and even more pronounced among non-Saudi males, indicate the need for gender-sensitive strategies to mitigate these differences and ensure equitable healthcare access and awareness.
Data Sharing Statement
The data regarding hepatitis B in Saudi Arabia are publicly available and easily accessible through The Department of Statistical Health Records; therefore, no ethical approval was required for this observational descriptive epidemiological study.
All reports can be directly downloaded from the The Department of Statistical Health Records website, available from: https://www.moh.gov.sa/Ministry/Statistics/book/Pages/default.aspx.
Ethical Approval Statement
The authors declare that the paper does not raise any ethical concern.
The Statistical Yearbook of the Saudi Ministry of Health (MoH) serves as a comprehensive and authoritative resource that provides a detailed overview of various health-related statistics and indicators in the Kingdom of Saudi Arabia. This annual publication is a valuable tool for researchers, policymakers, healthcare professionals, and the public, offering insights into the healthcare landscape and trends within the country. The Yearbook covers a wide range of health-related topics, including demographic data, disease prevalence, healthcare infrastructure, medical services utilization, and public health indicators. It compiles and presents data from different sources, including hospitals, health centers, and other healthcare facilities across various regions of Saudi Arabia. The Statistical Yearbook of the Saudi Ministry of Health (MoH).
The Department of Statistical Health Records has made annual reports on infectious diseases in the Kingdom of Saudi Arabia accessible to the academic community. These reports encompass comprehensive data pertaining to various infectious diseases within the country. The information contained within these reports is openly accessible on the Statistical Health Records Administration website, facilitating the utilization of this data by researchers interested in scientific exploration in the field of infectious diseases. Importantly, there are no prerequisites, restrictions, or formal consents required for researchers to access these reports.
The Department of Statistical Health Records is committed to fostering a collaborative environment for research and scientific advancement. To this end, it has explicitly stated that all reports related to infectious diseases in the Kingdom of Saudi Arabia are readily available for researchers affiliated with universities and scientific research centers. The department actively encourages researchers to delve into these reports, engage in analyses, and contribute to the realm of scientific publishing without encountering any limitations.
Disclosure
The authors declare no conflict of interest in this work.
References
1. Alshabi A, Fatima N, Marwan A, et al. Epidemiology screening and genotyping analysis for hepatitis B virus in Southwestern region of Saudi Arabia. J Infect Public Health. 2021;14(2):187–192. doi:10.1016/j.jiph.2020.11.016
2. Guvenir M, Arikan A. Hepatitis b virus: from diagnosis to treatment. Pol J Microbiol. 2020;69(4):391–399. doi:10.33073/PJM-2020-044
3. Stinco M, Rubino C, Trapani S, Indolfi G. Treatment of hepatitis B virus infection in children and adolescents. World J Gastroenterol. 2021;27(36):6053–6063. doi:10.3748/wjg.v27.i36.6053
4. Sani F, Alkhatry M, Alzanbagi A, Kumar S. Hepatitis B virus infection in Saudi Arabia and the UAE: public health challenges and their remedial measures. J Infect Public Health. 2023;16(9):1410–1417. doi:10.1016/j.jiph.2023.07.008
5. Yuen MF, Chen DS, Dusheiko GM, et al. Hepatitis B virus infection. Nat Rev Dis Prim. 2018;4(1):1–20. doi:10.1038/nrdp.2018.35
6. Odenwald MA, Paul S. Viral hepatitis: past, present, and future. World J Gastroenterol. 2022;28(14):1405–1429. doi:10.3748/wjg.v28.i14.1405
7. Gençdal G, Yurdaydin C. Epidemiology of hepatitis B virus in the Middle East. In: Carr BI, editor. Liver Cancer in the Middle East. Cham: Springer; 2021. doi:10.1007/978-3-030-78737-0_5
8. Akyıldız M, Ahıskalı E, Zeybel M, Yurdaydın C. Regional epidemiology, burden, and management of hepatitis B virus in the Middle East. Clin Liver Dis. 2019;14(6):212–214. doi:10.1002/cld.887
9. Babanejad M, Izadi N, Najafi F, Alavian SM. The HBsAg prevalence among blood donors from eastern Mediterranean and Middle Eastern countries: a systematic review and meta-analysis. Hepat Mon. 2016;16(3):3. doi:10.5812/hepatmon.35664
10. Alghamdi M, Alghamdi AS, Aljedai A, et al. Revealing hepatitis B virus as a silent killer: a Call-to-Action for Saudi Arabia. Cureus. 2021. doi:10.7759/cureus.14811
11. Aljumah A, Babatin M, Hashim A, et al. Hepatitis B care pathway in Saudi Arabia: current situation, gaps and actions. Saudi J Gastroenterol. 2019;25(2):73–80. doi:10.4103/sjg.SJG_421_18
12. Sanai FM, Alghamdi M, Dugan E, et al. A tool to measure the economic impact of hepatitis B elimination: a case study in Saudi Arabia. J Infect Public Health. 2020;13(11):1715–1723. doi:10.1016/j.jiph.2020.09.004
13. Alfaleh F, Alshehri S, Alansari S, Aljeffri M, Almazrou Y, Shaffi A. Abdo AA: long-term protection of hepatitis B vaccine 18 years after vaccination. J Infect. 2008;57(5):404–409. doi:10.1016/j.jinf.2008.08.008
14. Gerlich WH. Medical virology of hepatitis B: how it began and where we are now. Virol J. 2013;10(1):239. doi:10.1186/1743-422X-10-239
15. Alshammari TM, Aljofan M, Subaie G, Hussain T. Knowledge, awareness, attitude, and practice of health-care professionals toward hepatitis B disease and vaccination in Saudi Arabia. Hum Vaccines Immunother. 2019;15(12):2816–2823. doi:10.1080/21645515.2019.1629255
16. Morbidity and mortality report. CDC n.d. Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/rr6210a1.htm.
17. Al Humayed SM, El-Mekki AA, Mahfouz AA. Hepatitis B virus infection in Aseer Region, south-western Saudi Arabia: a call for an immediate action against a preventable disease. Public Health. 2017;146:24–28. doi:10.1016/j.puhe.2017.01.004
18. Gacche RN, Kaid AMS. Epidemiology of viral hepatitis B and C infection in Ibb City, Yemen. Hepatitis Mon. 2012;12(7):460. doi:10.5812/hepatmon.6140
19. Zhu ZZ, Wang D, Cong W-M, et al. Sex-related differences in DNA copy number alterations in hepatitis B virus-associated hepatocellular carcinoma. Asian Pacific J Cancer Prev. 2012;13(1):225–229. doi:10.7314/APJCP.2012.13.1.225
20. El-Serag HB. Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology. 2012;142(6):1264–1273. doi:10.1053/j.gastro.2011.12.061
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
