Back to Journals » Clinical Ophthalmology » Volume 18
Efficacy of Adding Sodium Hyaluronate Eye Drops to Tobramycin and Dexamethasone in the Treatment of Post-Cataract Surgery Dry Eye Disease: A Retrospective Analysis and Prospective Questionnaire Assessment
Authors Amer AA , Abu El Wafa Ali EG, Hamed MA , Gad Elkareem AM, Ahmed Sinjab AA, Awny I
Received 5 December 2023
Accepted for publication 21 February 2024
Published 28 February 2024 Volume 2024:18 Pages 613—621
DOI https://doi.org/10.2147/OPTH.S451442
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ahmed Ali Amer,1,* Essam Ghanem Abu El Wafa Ali,2,* Mohamed Atito Hamed,3,* Ashraf Mohammed Gad Elkareem,2,* Alaa Abdalsadek Ahmed Sinjab,4,* Islam Awny4
1Ophthalmology Department, Qena Faculty of Medicine, South Valley University, Qena, Egypt; 2Ophthalmology Department, Al Azhar University, Assuit, Egypt; 3Ophthalmology Department, Luxor University, Luxor, Egypt; 4Department of Ophthalmology, Sohag Faculty of Medicine, Sohag University, Sohag, Egypt
*These authors contributed equally to this work
Correspondence: Ahmed Ali Amer, Tel +20 101 182 7000, Email [email protected]
Purpose: This study aimed to compare the efficacy of using a combination of antibiotic and corticosteroid eye drops to using the same combination in addition to sodium hyaluronate eye drops.
Patients and Methods: This study included patients who underwent phacoemulsification for age-related cataract and presented to the ophthalmology department or outpatient clinic of the two hospitals in the study with DED during the period from January 2020 to January 2023. The study involved a two-pronged approach in which we retrospectively analyzed the prospectively maintained data of the patients and prospectively called the patients for an evaluation of the dry eye impact on vision-related function. The study patients were recruited from two hospitals. During the study period, patients who were treated with a combination of antibiotic and corticosteroid eye drops were enrolled in Group A, and those who were treated with the same combination with sodium hyaluronate eye drops were enrolled in Group B.
Results: The present study included 143 patients with post-phacoemulsification DED. Group A included 70 patients, and Group B included 73 patients. There was statistically significant improvement 4 weeks after treatment (p < 0.05) in the two groups. Comparing the two groups showed statistically significant improvements in group B compared to group A (p < 0.05). Assessment of the overall efficacy outcome revealed a statistically significant high percentage of cure (35.6% vs 1.4%) and high effectiveness (42.5% vs 13.6%) and a low percentage of effectiveness (21.9% vs 74.3%) and ineffectiveness (0.0% vs 5.7%) in Group B compared to Group A (p < 0.001).
Conclusion: Combining sodium hyaluronate eye drops with tobramycin and dexamethasone eye drops yielded obviously better efficacy outcomes compared to using tobramycin and dexamethasone eye drops alone.
Keywords: cataract surgery, dry eye disease, sodium hyaluronate
Introduction
Cataracts are commonly encountered in clinical practice, with subsequent increases in prevalence. The visual impairment caused by cataracts affects the patients’ quality of life as it can lead to difficulties in performing routine activities, including reading, driving, and recognizing faces. Additionally, cataracts can contribute to an increased risk of falls and injuries.1,2 The current surgical procedures for cataract surgery provide outstanding outcomes in terms of efficacy and safety.1,2 However, there are still potential surgery-related adverse events, which could be sight- or non-sight-threatening.3 One of the cataract-related complications is dry eye disease (DED),4 with a prevalence of up to 22% in patients undergoing non-complicated cataract surgeries during the first week postoperatively.5
Patients with DED present with eye dryness, photophobia, ocular fatigue, and foreign body sensations.6,7 Dry eye disease imposes a negative impact on the quality of vision (QOV) and quality of life (QOL).8 Therefore, it is essential to search for an ideal treatment that eliminates postoperative DED. The methods of DED treatment comprise using anti-inflammatory eye drops or artificial tears independently. Both of them showed limited symptoms’ improvement.9 Indeed, new modalities like intense pulsed light (IPL) have shown promise in managing postoperative DED. IPL therapy, with its anti-inflammatory and meibomian gland-targeting effects, presents an innovative approach to addressing dry eye symptoms. However, despite its potential benefits, one significant drawback is the associated expenses. The costs of IPL treatment can vary, and it may not be financially feasible for all individuals.10 Other more aggressive methods include lacrimal gland transplantation and embolization.11
While previous investigations have explored various treatment regimens for dry eye, including antibiotics and corticosteroid eye drops, there remains a paucity of evidence regarding the efficacy of combined eye drop regimens.12 Notably, sodium hyaluronate, as an artificial tear, is recognized for its conjunctival and corneal moisturizing properties13 and has shown reported improvements DED symptoms following cataract surgery.14 The inclusion of sodium hyaluronate in the combined regimens is a less-explored aspect in the existing literature. This study aimed to contribute to this gap in knowledge by comparing the efficacy of a combination of antibiotic and corticosteroid eye drops with and without the addition of sodium hyaluronate eye drops.
Materials and Methods
This study included patients who underwent phacoemulsification for age-related cataract and presented to the ophthalmology department/outpatient clinic of the two hospitals in the study with DED during the period from January 2020 to January 2023. The study involved a two-pronged approach in which we retrospectively analyzed the prospectively maintained data of the patients and prospectively called the patients for an evaluation of the dry eye impact on vision-related function. The study commenced after being approved by the Research Ethics Committee of faculty of medicine South Valley University with approval code of SVU\MED|OPHO26\7\22\3\363 and in adherence to the Helsinki Declaration with. From all patients, there were informed consent for participating in this research.
Patients who consecutively presented to the ophthalmology department with diagnostic criteria for postoperative DED15 were eligible for the study. The diagnosis was established based on a combination of symptoms, such as ocular dryness, photophobia, ocular fatigue, and foreign body sensations, as well as abnormal results from one or more diagnostic tests. These tests included Tear Break Up Time (TBUT), Schirmer I test, and fluorescein corneal staining (FS) level. A TBUT of less than 10 seconds, a Schirmer’s I test result of less than 10 mm in 5 minutes, and an FS score higher than 0 was considered abnormal.16–18
Patients with other postoperative complications, other eye disorders, previous eye surgery, autoimmune diseases, diabetes mellitus, or thyroid disease were excluded from the study. Patients who received drugs affecting eye dehydration (such as antihistaminics, diuretics, and glaucoma treatment) or other medications to treat DED and those with incomplete follow-up data or who did not respond to a call for evaluation of the impact of dry eye symptoms on quality of life using the ocular surface disease index (OSDI) questionnaire were also excluded.
Sample Size Calculation
For sample size calculation in this study, G*Power 1.3.9.7 software was used. The calculation was conducted using the formula for comparing two independent proportions. Specifically, we used the formula based on the Z-test for proportions, taking into account the reported efficacy scores from a similar published study,19 which found that adding sodium hyaluronate increased the efficacy scores from 88.9% to 99%. The minimum number of participants required in each group to achieve a statistically significant result with a confidence level of 95% (α level of 0.05) and a power of 80% was 68 patients in each group.
Study Groups
The study patients were recruited from two hospitals. During the study period, patients who were treated with a combination of antibiotic and corticosteroid eye drops were enrolled in Group A, and those who were treated with the same combination with sodium hyaluronate eye drops were enrolled in Group B.
Patients in group A received tobramycin (15 mg) and dexamethazone (5 mg) (Alcon Couvreur NV, Belgium) for 4 weeks (1–2 drops 4 times/day). Patients in group B received additional 0.24% sodium hyaluronate (Bausch + Lomb, Canada) as 1–2 drops 4 times per day. The used sodium hyaluronate drops are preservative-free and the ingredients of the used bottles were 2.4 mg/mL (0.24%) sodium hyaluronate, sodium chloride, potassium, chloride, disodium phosphate dodecahydrate, sodium dihydrogen phosphate-dihydrate, and water for injection.
Data Collection and Efficacy Evaluation
The patients’ baseline demographic and clinical data were extracted. The pre-treatment and one-month after-treatment ocular examination indices were recorded and analyzed. These tests include Tear break up time (TBUT) that was done using fluorescein corneal staining,16 Schirmer I test that was performed without anesthesia,17 and fluorescein corneal staining (FS) level, which was graded as 0: no staining, 1: minimally depicted staining, 2: moderately detected staining, and 3: obviously visible staining. In our study, the ocular surface staining grading system comprised four categories: Grade 0 indicated no staining, denoting a healthy ocular surface; Grade 1 represented minimally detected staining, reflecting a subtle or faint presence of fluorescence, suggestive of minor, localized disruption to the tear film; Grade 2 indicated moderately detected staining with affection of half or less of the corneal surface, signifying a more noticeable and widespread fluorescence pattern, indicative of a moderate level of ocular surface disruption; and Grade 3 denoted obviously visible staining, revealing a pronounced and readily apparent presence of fluorescence, with affection of more than half of the corneal surface indicating a significant disruption of the tear film. These grades were assigned based on careful observation using a slit lamp with cobalt blue light after fluorescein corneal staining and was devised by Ogawa et al.18
The ocular surface disease index (OSDI) questionnaire was used to assess the impact of ocular dryness on vision-related function.20 It entailed an 12-item assessment, with 0 to 4 points assigned for each item. The net resultant score is the sum of all items’ scores multiplied by 25 and divided by the number of evaluated items. A higher score indicates a more severe condition.
The overall efficacy outcome was classified as:
- Cure: if the symptoms totally disappeared and the ocular examination indices were within a normal range: a TBUT of 10 seconds or more, A Schirmer’s I test result of 10 mm or more in 5 minutes, and an FS score of 0.
- High effectiveness: if the symptoms were considerably relieved and the results of one test were borderline: a TBUT of 5–10 seconds, A Schirmer’s 1 test result of 5–10 mm in 5 minutes, or an FS score of 1.
- Effectiveness: if the symptoms were partially relieved and the results of one test were abnormal (a TBUT of < 5 seconds, A Schirmer’s 1 test result of 5 mm in 5 minutes, or an FS score of 2), or if the results of more than one test were borderline,
- Ineffectiveness: if persistent or worsened symptoms and the results of more than one test were abnormal.
Study Outcomes
The primary outcome of the present work was the potential difference in the ocular dryness indices and the overall efficacy category between the two study groups. The secondary outcome was the difference in OSDI scores between the two groups.
Statistical Analysis
The obtained data and the eye measurements in the study groups were statistically analyzed using SPSS statistical software, version 28 (IBM Corp., Armonk, NY, USA). Numerical values were presented as mean ± standard deviation (SD) or median (interquartile range, IQR) and compared using an independent t-test, paired t-test, Mann–Whitney test, or Wilcoxon signed rank test, as appropriate. Categorical values were expressed as frequencies and percentages and compared using the Chi-square test or the Z test for proportions accordingly. A p-value less than 0.05 was considered statistically significant.
Results
The present study included 143 patients with post-phacoemulsification DED. Group A included 70 patients with a mean age of 60.97 ± 6.75 years and a male percentage of 60% (n = 42). Group B included 73 patients with a mean age of 60.27 ± 6.33 years and a male percentage of 60.3% (n = 44). Smoking prevalence was 11.4% (n = 8) and 15.1% (n = 11) in the two groups, respectively. As shown in Table 1, both groups were comparable in the mean age (p = 0.262), sex distribution (p = 0.973), and smoking prevalence (p = 0.521).
 |
Table 1 Pretreatment and Post Treatment Data of the Examined Patients |
The mean/median pre-treatment and 4-week post-treatment TBUT, Schirmer I, and FS values in the two groups are presented in Table 1 and Figures 1–3. Both groups showed no statistically significant difference in the baseline measures (p > 0.05). There was statistically significant improvement 4 weeks after treatment (p < 0.05) in the two groups. Comparing the two groups showed statistically significant improvements in group B compared to group A (p < 0.05).
 |
Figure 1 Pretreatment and Post treatment TBUT values in the study groups. |
 |
Figure 2 Pretreatment and Post treatment Schirmer I values in the study groups. |
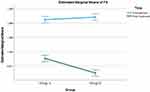 |
Figure 3 Pretreatment and Post treatment FS scores in the study groups. |
Assessment of the overall efficacy outcome revealed a statistically significant high percentage of cure (35.6% vs 1.4%) and high effectiveness (42.5% vs 13.6%) and a low percentage of effectiveness (21.9% vs 74.3%) and ineffectiveness (0.0% vs 5.7%) in Group B compared to Group A (p < 0.001).
The mean duration between treatment and OSDI assessment was 18.3 ± 7.31 months in group A and 17.2 ± 6.89 months in group B, with a statistically insignificant difference (p = 0.178). The post-treatment mean OSDI score value in Group A was 15.78 ± 5.85 and in Group B was 11.27 ± 3.59 (Figure 4). The post-treatment mean OSDI score value in Group B was significantly lower than its counterpart in Group A (p < 0.001).
 |
Figure 4 Post treatment OSDI values in the study groups. |
Discussion
While advancements in research, clinical practices, and technology often prioritize preventing sight-threatening complications, it is crucial not to overlook the importance of addressing and reducing less severe adverse events of cataract surgery. These events, although not sight-threatening, can greatly affect the patient’s quality of life. An instance of this is dry eye disease, where the negative impacts of cataract surgery on the eye’s surface can lead to the development or worsening of DED, both directly and by exacerbating any pre-existing conditions.4,21
Patients with dry eye after cataract surgery have continuous discomfort that impairs their quality of life and hinders recovery from surgery. Tobramycin and dexamethasone eye drops, being a combination of antibiotic and corticosteroid, have an anti-inflammatory effect that accelerates healing of the surgical incision and relieves the dryness symptoms.12 The composition of sodium hyaluronate shares key components with tears, facilitated the lubrication of the ocular surface and accelerating the adhesion of corneal epithelial cells, which helps restore the tear film’s stability and alleviate the symptoms of dry eye.22 Nevertheless, there are scarce research studies assessing the clinical efficacy of combining sodium hyaluronate with conventional anti-inflammatory eye drops in the treatment of DED after surgery for cataract.
The present work showed that treatment in both groups resulted in significant improvement of the patients’ condition, which ensured the anti-inflammatory effect of tobramycin and dexamethasone eye drops. However, when sodium hyaluronate was added, a significantly better outcome was evident, with a complete cure in more than a quarter of patients after 4 weeks of treatment. A statistically significant difference was noted in the TBUT values, reflecting an obvious effect on the stability of the tear film. Similar results were shown for Schirmer I test results, denoting that sodium hyaluronate may be involved in tear secretion. A significantly lower FS score was shown in the sodium hyaluronate-added group. This indicates significantly fewer areas of damage or dryness in the corneas. Moreover, the OSDI scores, which were assessed after a mean period of more than one year after treatment, were significantly better in the sodium hyaluronate-added group. This indicates that sodium hyaluronate effectively alleviated dry eye symptoms, improved ocular surface health and comfort, and enhanced the overall well-being of the patients in that group.
Similar findings were reported in the few earlier studies that assessed the benefit of adding sodium hyaluronate to the treatment regimen of DED after cataract surgery.14,16,23 Chen et al14 observed that sodium hyaluronate was able to restore the structure of the tear film and improve the regularity of the corneal surface. In agreement with our study, Lu et al16 found that combining sodium hyaluronate with pranoprofen, tobramycin, and dexamethasone improved the curative effect compared to when sodium hyaluronate was lacking. Yang and Wang23 reported that sodium hyaluronate combined with pranoprofen had effectively treated DED and was able to enhance tear secretion, keep ocular moisture, recover tear film stability, and improve the patients’ quality of life. Moreover, Duan and Tang24 investigated the clinical efficacy of sodium hyaluronate, compound dextran, and polyethylene glycol eye drops in the treatment of DED after cataract surgery and found that sodium hyaluronate outperformed the two other medications. This was supported also by the recent study of Chen et al25 who reported that sodium hyaluronate eye drops added in the early stage after phacoemulsification could restore the structure of tear film and improve the regularity of corneal surface. In their study, sodium hyaluronate at a concentration of 0.3% showed better efficacy than that of 0.1% concentration.
The obvious reproducibility of sodium hyaluronate eye drops in DED could be explained given their physical and chemical characteristics. Sodium hyaluronate, also referred to as hyaluronic acid, is a complex polysaccharide biomaterial with a high molecular weight. It is composed of repeated N-acetyl-glucuronide units and is commonly found in the form of a sodium salt. This biopolymer occurs naturally in all vertebrates and possesses the ability to attract and bind a significant quantity of water molecules. It has the capacity to stabilize the aqueous layer, prolong the duration before tear film disruption occurs, and has the capability to associate with fibrin, thereby enhancing the adherence and spreading of corneal epithelial cells. Consequently, it aids in the facilitation of corneal epithelium recovery.26 Sodium hyaluronate has the capacity to retain a considerable number of water molecules within its structure, which contributes to its outstanding water retention properties27 and can impede the rapid evaporation of water from the tear film.28 A sodium hyaluronate solution with a concentration of 0.3% possesses a molecular weight ranging from 500,000 to 1,200,000 Da. It exhibits enhanced adherence compared to a 0.1% solution, which constitutes its primary benefit. Furthermore, it has the capability to linger on the corneal surface for an extended duration, contributing to improved moisturization. Sodium hyaluronate of intermediate molecular weight, obtained through a refining process, is better equipped to attain an optimal equilibrium between effectiveness and comfort, which was used in the current study.
While our study has shed light on the comparative efficacy of treatment regimens for post-phacoemulsification DED, there are promising avenues for future research. Firstly, investigations into the long-term outcomes of the studied interventions could provide valuable insights into the sustained effectiveness and potential recurrence of DED symptoms. Additionally, the inclusion of diverse patient populations in future studies will contribute to a more comprehensive understanding of treatment responses across various demographics and clinical profiles. Exploring the impact of age, gender, and other factors on treatment outcomes may unveil nuanced patterns that can inform personalized approaches to DED management. Moreover, considering the rapid advancements in diagnostic technologies, incorporating novel tools for assessing DED severity and progression could refine the precision of treatment evaluations. Exploring the integration of cutting-edge diagnostic methods, such as Optical Coherence Tomography (OCT) and In Vivo Confocal Microscopy (IVCM), may enhance our ability to tailor interventions to individual patient needs. Furthermore, the exploration of emerging treatments and therapeutic modalities in future research is essential. Investigating the efficacy of innovative interventions or pharmaceutical agents that have shown promise in preclinical or early clinical studies could open new avenues for more effective and targeted DED management. Additionally, the design and implementation of randomized controlled trials (RCTs) in future research are essential for establishing a stronger evidence base. Rigorous RCTs will not only validate the comparative efficacy observed in our study but also provide more robust insights into causal relationships and treatment effectiveness.
This study is limited by the retrospective design, that did not allow randomization of participants or double blinding, and the short-term follow-up. However, parallel to the retrospective analysis, a crucial component of the study involved the initiation of a questionnaire-based assessment. This approach allowed for the capture of real-time insights, subjective experiences, and perspectives of the participants, which provided a multifaceted exploration of the effectiveness of sodium hyaluronate in the treatment of DED.
Conclusion
In conclusion, our investigation into the management of post-phacoemulsification DED has yielded substantial insights. The integration of sodium hyaluronate eye drops with tobramycin and dexamethasone eye drops has emerged as a promising therapeutic approach, demonstrating markedly superior efficacy outcomes when compared to the use of tobramycin and dexamethasone eye drops alone.
The observed enhancements encompassed various facets of treatment response, including a higher percentage of cure, elevated levels of high effectiveness, and a notable decrease in the percentage of ineffectiveness. This signifies not only the immediate impact on DED symptoms but also hints at the potential for long-term benefits. Continued research, including larger-scale randomized controlled trials and long-term follow-ups, will be pivotal in further validating these results and elucidating the nuanced mechanisms underlying the observed improvements.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Addisu Z, Solomon B. Patients’ preoperative expectation and outcome of cataract surgery at Jimma university specialized hospital – department of ophthalmology. Ethiop J Health Sci. 2011;21(1):47–55. doi:10.4314/ejhs.v21i1.69044
2. Pager CK. Expectations and outcomes in cataract surgery: a prospective test of 2 models of satisfaction. Arch Ophthalmol. 2004;122(12):1788–1792. doi:10.1001/archopht.122.12.1788
3. Day AC, Donachie PHJ, Sparrow JM, et al. The royal college of ophthalmologists’ national ophthalmology database study of cataract surgery: report 1, visual outcomes and complications. Eye. 2015;29(4):552–560. doi:10.1038/eye.2015.3
4. Ishrat S, Nema N, Chandravanshi SCL. Incidence and pattern of dry eye after cataract surgery. Saudi J Ophthalmol. 2019;33(1):34–40. doi:10.1016/j.sjopt.2018.10.009
5. Hamed MA, Aldghaimy AH, Mohamed NS, Amer AA. The incidence of post phacoemulsification surgery induced dry eye disease in upper Egypt. Clin Ophthalmol. 2022;16:705–713. doi:10.2147/OPTH.S358866
6. Naderi K, Gormley J, O’Brart D. Cataract surgery and dry eye disease: a review. Eur J Ophthalmol. 2020;30(5):840–855. doi:10.1177/1120672120929958
7. Kasetsuwan N, Satitpitakul V, Changul T, Jariyakosol S, Wedrich A. Incidence and pattern of dry eye after cataract surgery. PLoS One. 2013;8(11):e78657. doi:10.1371/journal.pone.0078657
8. Stapleton F, Alves M, Bunya VY, et al. TFOS DEWS II epidemiology report. Ocul Surf. 2017;15(3):334–365. doi:10.1016/j.jtos.2017.05.003
9. Huang Q, Yang Y, Liao T, et al. Association between asthma with dry eye disease: a protocol for systematic review and meta-analysis. Medicine. 2020;99(41):e22519. doi:10.1097/MD.0000000000022519
10. Toyos R, McGill W, Briscoe D. Intense pulsed light treatment for dry eye disease due to meibomian gland dysfunction; a 3-year retrospective study. Photomed Laser Surg. 2015;33(1):41–46. doi:10.1089/pho.2014.3819
11. Hirayama M, Ogawa M, Oshima M, et al. Functional lacrimal gland regeneration by transplantation of a bioengineered organ germ. Nat Commun. 2013;4(1):2497. doi:10.1038/ncomms3497
12. Bandello F, Coassin M, Di Zazzo A, et al. One week of levofloxacin plus dexamethasone eye drops for cataract surgery: an innovative and rational therapeutic strategy. Eye. 2020;34(11):2112–2122. doi:10.1038/s41433-020-0869-1
13. Chang DH, Christie WC, Loden JC, Smith PJ, Jackson BE. Clinical evaluation of a bacterially derived sodium hyaluronate 2.3% ophthalmic viscosurgical device. J Cataract Refract Surg. 2019;45(12):1789–1796. doi:10.1016/j.jcrs.2019.08.007
14. Chen N, Zhang JS, Zhang TX, Shao YS, Zhang F. The effect of sodium hyaluronate on the corneal biomechanics of patients with cataract and dry eye before operation. Int J Gen Med. 2021;14:2377–2384. doi:10.2147/IJGM.S297369
15. D’Souza S, James E, Swarup R, et al. Algorithmic approach to diagnosis and management of post-refractive surgery dry eye disease. Indian J Ophthalmol. 2020;68(12):2888–2894. doi:10.4103/ijo.IJO_1957_20
16. Ramos L, Barreira N, Mosquera A, et al. Break-up analysis of the tear film based on time, location, size and shape of the rupture area. In: Kamel M, Campilho A, editors. Image Analysis and Recognition. Berlin, Heidelberg: Springer; 2013:695–702. Lecture Notes in Computer Science.
17. Karampatakis V, Karamitsos A, Skriapa A, et al. Comparison between normal values of 2- and 5-minute Schirmer test without anesthesia. Cornea. 2010;29(5):497–501. doi:10.1097/ICO.0b013e3181c2964c
18. Ogawa Y, Kim SK, Dana R, et al. International chronic ocular graft-vs-host-disease (GVHD) consensus group: proposed diagnostic criteria for chronic GVHD (Part I). Sci Rep. 2013;3(1):3419. doi:10.1038/srep03419
19. Lu H, Guan Y, Su Y, et al. Effect of sodium hyaluronate eye drops combined with tobramycin, dexamethasone and pranoprofen eye drops in the treatment of dry eye after phacoemulsification. Indian J Ophthalmol. 2022;70(12):4319–4324. doi:10.4103/ijo.IJO_1652_22
20. Baudouin C, Aragona P, Van Setten G, et al. Diagnosing the severity of dry eye: a clear and practical algorithm. Br J Ophthalmol. 2014;98(9):1168–1176. doi:10.1136/bjophthalmol-2013-304619
21. Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15(3):276–283. doi:10.1016/j.jtos.2017.05.008
22. Miháltz K, Faschinger EM, Vécsei-Marlovits PV. Effects of lipid- versus sodium hyaluronate-containing eye drops on optical quality and ocular surface parameters as a function of the meibomian gland dropout rate. Cornea. 2018;37(7):886–892. doi:10.1097/ICO.0000000000001523
23. Yang G, Wang Y. Diagnostic and therapeutic advances in biomedical research and pharmaceutical science. Indian J Pharm Sci. 2021;83(5):S1–S5.
24. Duan ZH, Tang YF. The clinical effects of sodium hyaluronate, polyethylene glycol, and dextran-70 eye drops in relieving dry eye after phacoemulsification. Medicine. 2021;100(25):e26358. doi:10.1097/MD.0000000000026358
25. Chen N, Zhang JS, Zhang TX, Fan BL, Ning Y. The effect of sodium hyaluronate on tear film stability in patients with dry eye syndrome after cataract surgery. Graefes Arch Clin Exp Ophthalmol. 2023;261(4):1011–1017. doi:10.1007/s00417-022-05880-7
26. Cai JY, Li L, Liu XY, et al. Effect of sodium hyaluronate on early changes of tear film after phacoemulsification. Int Eye Sci. 2008;8:932–934.
27. Tifany JM, Winter N, Bliss G. Tear film stability and tear surface tension. Curr Eye Res. 1989;8(5):507–515. doi:10.3109/02713688909000031
28. Nakamura M, Hikida M, Nakano T, et al. Characterization of water retentive properties of hyaluronan. Cornea. 1993;12(5):433–436. doi:10.1097/00003226-199309000-00010
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
