Back to Journals » Lung Cancer: Targets and Therapy » Volume 14
Effect of Lymphopenia on Tumor Response and Clinical Outcomes Following Chemoradiotherapy in Stage III Non-Small Cell Lung Cancer
Authors Deck J, Hartley M, Akhter M, Wang D, Bogart JA , Mix MD
Received 16 December 2022
Accepted for publication 27 April 2023
Published 19 May 2023 Volume 2023:14 Pages 47—55
DOI https://doi.org/10.2147/LCTT.S386344
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sai-Hong Ignatius Ou
Jared Deck,1 Marissa Hartley,1 Mohammad Akhter,1 Dongliang Wang,2 Jeffrey A Bogart,1 Michael D Mix1
1Department of Radiation Oncology, SUNY Upstate Medical University, Syracuse, NY, USA; 2Department of Public Health and Preventive Medicine, SUNY Upstate Medical University, Syracuse, NY, USA
Correspondence: Jared Deck, Department of Radiation Oncology, SUNY Upstate Medical University, 750 E Adams St, Syracuse, NY, 13202, USA, Tel +1 (315)-464-5276, Email [email protected]
Background: Prior studies suggest lymphopenia, systemic immune-inflammatory index, and tumor response all impact clinical outcomes in Stage III NSCLC. We hypothesized that tumor response after CRT would be associated with hematologic metrics and might predict clinical outcomes.
Materials and Methods: Patients with stage III NSCLC treated at a single institution between 2011 and 2018 were retrospectively reviewed. Pre-treatment gross tumor volume (GTV) was recorded then reassessed at 1– 4 months post-CRT. Complete blood counts before, during and after treatment were recorded. Systemic immune-inflammation index (SII) was defined as neutrophil × platelet/lymphocyte. Overall survival (OS) and progression free survival (PFS) were calculated using Kaplan-Meier estimates, and compared with Wilcoxon tests. A multivariate analysis of hematologic factors impacting restricted mean survival was then performed using pseudovalue regression, accounting for other baseline factors.
Results: 106 patients were included. After median follow-up of 24 months, median PFS and OS were 16 and 40 months, respectively. Within the multivariate model, baseline SII was associated with OS (p = 0.046) but not PFS (p = 0.09), and baseline ALC correlated with both PFS and OS (p = 0.03 and p = 0.02, respectively). Nadir ALC, nadir SII, and recovery SII were not associated with PFS or OS.
Conclusion: In this cohort of patients with stage III NSCLC, baseline hematologic factors were associated with clinical outcomes including baseline ALC, baseline SII and recovery ALC. Disease response was not well correlated with hematologic factors or clinical outcomes.
Keywords: lymphopenia, myelosuppression, chemoradiation, tumor response
Introduction
Non-small cell lung cancer (NSCLC) remains the leading cause of cancer-related death in the United States and worldwide with 1.7 million deaths globally, representing over 18% of all cancer deaths. Despite recent advances, 3-year overall-survival (OS) is less than 60%.1 Chemoradiotherapy (CRT) followed by immunotherapy has become a standard for definitive management of unresectable Stage III NSCLC. Oncologic therapies interact with the host immune system potentially altering clinical outcomes, though the complex interplay is not fully understood. The immune system plays a role in suppression of malignancy, but can be inhibited, allowing for cancer progression. Radiotherapy can enhance cancer cell antigenicity by upregulating DNA damage and cellular stress pathways, exposing immunogenic tumor-associated antigens to the immune system.2,3 Conversely, multimodality treatment with radiation can induce lymphopenia4–6 and dampen the immune response, because lymphocytes are key mediators of the response to cancer. Mature circulating lymphocytes are highly radiosensitive and exhibit significant DNA fragmentation at even low radiation doses (<1Gy).7,8 Multiple studies have associated lymphopenia with a detrimental impact on clinical outcomes in some cancer types5,6,9–11 while others have failed to show such a relationship.4 It has been proposed that radiation dose to the host immune system is associated with worse clinical outcomes in patients with Stage III NSCLC.12 The systemic immune-inflammatory index (SII = neutrophil × platelet/lymphocyte) is a marker that has been suggested to have prognostic influence in patients treated with locally advanced NSCLC, as well as other malignancies.13 Standard radiotherapy for Stage III NSCLC targets not only gross disease but often includes additional margin for at-risk regions as well as uncertainties in planning or treatment delivery, resulting in collateral effects on health tissue, including tissue involved in the immune response.
Recent evidence suggests tumor volume reduction as determined by modern RT image guidance such as cone beam computed tomography (CBCT) images may be correlated with clinical outcome.14 In this retrospective study, we aimed to investigate the relationship between lymphopenia, SII, and disease response based on CT imaging following completion of definitive chemoradiation (CRT) in stage III NSCLC. We hypothesized that tumor response after CRT would be associated with hematologic metrics, and might ultimately predict for clinical outcomes.
Materials/Methods
Using an IRB approved database, patients with stage III NSCLC treated at a single institution with definitive chemoradiation between 2011 and 2018 were reviewed using electronic medical record (EPIC), available diagnostic imaging, and treatment planning system (Varian Eclipse). No patients had received prior treatment. All patients fulfilling the following criteria were included: (1) ≥18 years of age, (2) pathologically proven NSCLC, (3) available complete blood counts before, during and after treatment, and (4) CT-based imaging immediately prior to and 1 to 4 months following treatment. Patients without accessible blood counts, imaging, or patients who did not complete therapy, were excluded.
Patients were censored at time of last follow up. Local recurrence was defined as failure within high dose radiation field. CT scans 1–4 months after completion of CRT were evaluated for initial response. Pre- and post-treatment CT scans were analyzed and contours were generated manually, allowing for calculation of tumor volume both before and after treatment. Lymphopenia, defined as an absolute lymphocyte count (ALC) <1.0 x103/µL, was graded according to Common Terminology Criteria for Adverse Events (CTCAE) version 5. Overall survival (OS) and progression free survival (PFS) were calculated using Kaplan-Meier estimates from the date of diagnosis for the entire cohort and also based on histology.
Since the assumption of proportional hazards does not hold, commonly used Log rank test and Cox model were not used. Instead, Wilcoxon tests were used to compare the survival times. A multivariate analysis of hematologic factors impacting restricted mean survival up to 60 months was then performed using pseudovalue regression, accounting for other baseline factors,15 including age, AJCC, T stage, N stage, histology, consolidation, GTV initial and GTV response. All analyses were performed using SAS© 9.4 and statistical tests with p values less than 0.05 were considered as statistically significant.
Results
Patient and Treatment Characteristics
Overall, 106 patients were included in the study. Median age was 62 years (range: 47–85) and 56% were female. Current, former, and never smokers represented 63%, 33%, and 4% of the patients, respectively. Patients had a median of 40 pack-years smoking history. 59% were stage IIIA (AJCC 7th Ed). Histologically, 42% had adenocarcinoma, 50% had squamous cell carcinoma, and 8% were poorly differentiated. At diagnosis, 89% were ECOG 0–1. Baseline demographic, tumor, and treatment characteristics are summarized in Table 1. All patients were treated with definitive concurrent chemoradiotherapy, and weekly carboplatin (AUC 2) and paclitaxel (50 mg/m2) was the most common chemotherapy regimen. Thoracic radiotherapy was given to a median dose of 60 Gy in 30 fractions, and 22 (20.8%) received a simultaneous integrated boost.
 |
Table 1 Baseline Clinical, Treatment, and Response Factors of 106 Patients with Stage III NSCLC |
Myelosuppression
Prior to starting treatment, the median baseline absolute lymphocyte count (bALC) was 1.49 x103/µL, the median absolute baseline neutrophil count (bANC) was 6.4 x103/µL, the median absolute baseline platelet count was 299 x109/L, and the median absolute baseline albumin was 4.0 g/dL. Median drop in ALC (dALC) during treatment was 1.13x103/µL. ALC typically declined precipitously following initiation of CRT, reaching its nadir by week 6–7, and recovered following the completion of CRT, although not to baseline (Figure 1). Patients reached approximately 50% of their pre-treatment lymphocyte count by two months post-treatment. Median drop in neutrophils, platelets and albumin were, 4.8 x103/µL, 173 x103/µL, and 0.4 g/dL, respectively. 54.7% and 32.1% of patients experienced Grade 3 and Grade 4 lymphopenia, respectively. 29.2% of patients experienced ≥ grade 3 leukopenia.
 |
Figure 1 Absolute Lymphocyte Count (x103/µL) for each patient during and following completion of chemoradiation. |
Clinical Outcomes
After median follow-up of 24 months (range: 4–97 months), median PFS (95% CI, 14–36) and OS (95% CI, 24–52) were 16 and 40 months, respectively. Local tumor recurrence (LR) was noted in 13.2% with a median time to LR of 26 months, and 27.4% of patients failed distally with a median time to distant recurrence of 17 months. Local recurrence occurred in 18.2% of patients with adenocarcinoma compared with 9.4% of patients with squamous cell carcinoma (p=0.104). Larger GTV (> 120 cc) was negatively associated with PFS (p=0.048) and OS (p=0.032). AJCC 7th edition stage grouping as well as T and N categories were highly associated with OS and PFS.
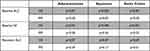
Estimates for OS and PFS based on baseline absolute lymphocyte count (ALC), baseline SII, and recovery ALC, dichotomized by median split and compared with Wilcoxon tests, are summarized in Figure 2. On univariate analysis, baseline ALC >1.5 x103/µL was associated with improved PFS (p=0.009) and improved OS (p=0.001). Additionally, baseline SII <1200 was associated with improved PFS (p=0.01) and OS (p=0.005). Neither ALC nor SII during nadir phase (weeks 5–7) were associated with PFS or OS. Recovery ALC (1–2 months post-CRT) was associated with improved PFS (p=0.01) but not OS (p=0.09). SII was not associated with PFS or OS during the recovery phase. When stratified by histology, squamous cell carcinoma baseline ALC >1.5 x103/µL was associated with improved PFS (p=0.05) and OS (p=0.003). Squamous cell carcinoma baseline SII <1200 was also associated with improved OS. Baseline ALC, baseline SII and recovery ALC were not statistically significant in the adenocarcinoma subset (Table 2). Within the multivariate model over restricted mean survival time up to 60 months, baseline SII remained significant for OS (p = 0.046) but not PFS (p = 0.09), and bALC remained associated with both PFS and OS (p = 0.03 and p = 0.02, respectively), after accounting for the confounding effects from age, AJCC, T stage, N stage, histology, consolidation, GTV initial and GTV response.
 |
Figure 2 Estimates for OS and PFS based on baseline absolute lymphocyte count (ALC), baseline SII, and recovery ALC, dichotomized by median split. |
Tumor and Response
Median pre- and post-GTV were 110 cc and 23 cc, respectively, with a median 74.3% median response (GTVres) from pre-treatment simulation scan to post-treatment imaging. Neither baseline nor nadir hematologic values were associated with magnitude of tumor response. Percent tumor response was not associated with PFS (p=0.258) or OS (p=0.185).
Discussion
The development of lymphopenia during chemoradiation is expected in patients with stage III NSCLC. The current study supports an association between baseline lymphocyte count and clinical outcomes, previously suggested by others in a range of cancer types.16–19 Our study was in agreement with Tong et al in suggesting that pre-treatment SII as an independent prognostic biomarker for OS.13
Our search for a signal of association between degree of myelosuppression and magnitude of tumor response did not yield significance. To our knowledge, this is the first attempt to evaluate this potential relationship. Moreover, depth of treatment-related immunologic nadir was not associated with clinical outcome in our patient population. This is consistent with findings in a recent study of patients undergoing CRT in oropharyngeal cancer from Ng et al where no association between the development of G3/G4 lymphopenia and overall survival was found.4 A contrary result was published regarding patients with esophageal cancer where grade 4 ALC nadir was associated with worse OS and disease-specific survival outcomes.20
Early response to treatment has recently been posited to predict for post-CRT survival.14,21 These findings were not replicated in this series, and our attempt to explain magnitude of response by baseline or treatment-induced lymphopenia was not fruitful. It is possible that a relationship does indeed exist, but could not be uncovered by our method of study. Notably, there are significant challenges associated with accurate disease-response volumetric assessment. For example, assigning a residual tumor volume following substantial response conflated with post-treatment changes is likely subject to significant inter-observer variability.
Recovery ALC was associated with improved PFS and a trend towards improved OS, suggesting that the immune system’s ability to rebound might be helpful in anticipating clinical outcome. Others have shown that lower radiation doses to the circulating blood pool, lymphoid organs, and heart are associated with reduced hematologic immunosuppression.22,23 The negative clinical outcomes associated with persistent chemoradiation induced lymphopenia following treatment suggest novel approaches to minimize radiation dose to lymphocyte-related organs at risk while maintaining target coverage deserve further consideration.
It has been postulated that treatment-related lymphopenia may be related to radiation techniques including dose rate and target size. As early as the 1970s, lymphopenia was noted to be inversely proportional to fraction number, even when total radiation dose was held constant.24 Techniques such as stereotactic body radiotherapy (SBRT), hypofractionation, proton therapy, ultra-high dose rate (FLASH) RT and de-intensification through reduction of dose, volume, or systemic therapy may reduce the lymphotoxic effects.18,25 Recent studies suggest that reducing lung V5-V10 may be important for optimization of immune response given the high sensitivity of lymphocytes to low levels of radiation, especially in patients with XRCC1 rs25487 genotype.26,27 In RTOG 0617, dose escalation to 74 Gy compared to 60 Gy resulted in an unexpected trend towards inferior local control 61.8 → 54.3% (p=0.07) and OS 32.1 → 23% (p=0.06).28 One potential explanation suggests that dose escalation may inhibit the host immune response by reducing populations of lymphocytes.29 Indeed, Colton et al, and Ladbury et al suggested that the immune system could be avoided as an organ at risk, potentially impacting clinical outcomes.12,30
Although most patients in this study did not receive immunotherapy, durvalumab is now standard of care in the adjuvant setting and studies are ongoing (eg ECOG-ACRIN 5181) investigating its role in the concurrent setting. Despite adoption of anti-PDL1 therapy within contemporary guidelines, multiple real-world factors limit its utilization, with recent published immunotherapy initiation rates as low as 65%.31 The effects of lymphopenia in patients receiving immunotherapy is not well established, but it has been suggested that peri-immunotherapy lymphopenia may predict for worse clinical outcomes.18,32 As the role of immunotherapy grows, so does the need to better understand the interplay between the host immune system, radiation therapy, and systemic therapy. Strategies for adapting radiotherapy timing and technique to minimize lymphopenia may offer an opportunity to further advance clinical outcomes.
Limitations to this study include those inherent to any retrospective study from a single institution with a relatively small sample size, especially when stratifying by histology. Additionally, blood draws and imaging were not standardized so there was some heterogeneity in their frequency and timing relative to radiation treatments. Finally, evaluation of tumor response while seeking association with hematologic parameters is complex. Thus, caution is advised in interpreting these results, and larger validation studies are likely required to more thoroughly evaluate or corroborate any potential interaction.
Conclusions
In this cohort of patients with stage III NSCLC treated with definitive chemoradiation, several baseline and recovery hematologic factors were associated with clinical outcomes including baseline ALC, baseline SII and recovery ALC. Treatment related hematologic nadir were not associated with clinical outcome. Further understanding of the interplay between the immune system, hematologic toxicity, and clinical outcomes following CRT is needed.
Human Ethics Statement
Prior to starting the study, ethical approval was obtained by Upstate Medical University Institutional Review Board for the Protection of Human Subjects and project was determined to be EXEMPT FROM IRB REVIEW according to federal regulations. The data accessed complied with all relevant data protection and privacy regulations.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Gray JE, Villegas A, Daniel D, et al. Three-Year Overall Survival with Durvalumab after Chemoradiotherapy in Stage III NSCLC-Update from PACIFIC. J Thorac Oncol. 2020;15(2):288–293. doi:10.1016/j.jtho.2019.10.002
2. Lhuillier C, Rudqvist NP, Elemento O, Formenti SC, Demaria S. Radiation therapy and anti-tumor immunity: exposing immunogenic mutations to the immune system. Genome Med. 2019;11(1):40. doi:10.1186/s13073-019-0653-7
3. Portella L, Scala S. Ionizing radiation effects on the tumor microenvironment. Semin Oncol. 2019;46(3):254–260. doi:10.1053/j.seminoncol.2019.07.003
4. Ng SP, Bahig H, Jethanandani A, et al. Lymphopenia during radiotherapy in patients with oropharyngeal cancer. Radiother Oncol. 2020;145:95–100. doi:10.1016/j.radonc.2019.12.023
5. Grossman SA, Ellsworth S, Campian J, et al. Survival in Patients With Severe Lymphopenia Following Treatment With Radiation and Chemotherapy for Newly Diagnosed Solid Tumors. J Natl Compr Canc Netw. 2015;13(10):1225–1231. doi:10.6004/jnccn.2015.0151
6. Grossman SA, Ye X, Lesser G, et al. Immunosuppression in patients with high-grade gliomas treated with radiation and temozolomide. Clin Cancer Res. 2011;17(16):5473–5480. doi:10.1158/1078-0432.Ccr-11-0774
7. Sellins KS, Cohen JJ. Gene induction by gamma-irradiation leads to DNA fragmentation in lymphocytes. J Immunol. 1987;139(10):3199–3206.
8. Stratton JA, Byfield PE, Byfield JE, Small RC, Benfield J, Pilch Y. A comparison of the acute effects of radiation therapy, including or excluding the thymus, on the lymphocyte subpopulations of cancer patients. J Clin Invest. 1975;56(1):88–97. doi:10.1172/jci108084
9. Balmanoukian A, Ye X, Herman J, Laheru D, Grossman SA. The association between treatment-related lymphopenia and survival in newly diagnosed patients with resected adenocarcinoma of the pancreas. Cancer Invest. 2012;30(8):571–576. doi:10.3109/07357907.2012.700987
10. Lin AJ, Gang M, Rao YJ, et al. Association of Posttreatment Lymphopenia and Elevated Neutrophil-to-Lymphocyte Ratio With Poor Clinical Outcomes in Patients With Human Papillomavirus-Negative Oropharyngeal Cancers. JAMA Otolaryngol Head Neck Surg. 2019;145(5):413–421. doi:10.1001/jamaoto.2019.0034
11. Campian JL, Sarai G, Ye X, Marur S, Grossman SA. Association between severe treatment-related lymphopenia and progression-free survival in patients with newly diagnosed squamous cell head and neck cancer. Head Neck. 2014;36(12):1747–1753. doi:10.1002/hed.23535
12. Ladbury CJ, Rusthoven CG, Camidge DR, Kavanagh BD, Nath SK. Impact of Radiation Dose to the Host Immune System on Tumor Control and Survival for Stage III Non-Small Cell Lung Cancer Treated with Definitive Radiation Therapy. Int J Radiat Oncol Biol Phys. 2019;105(2):346–355. doi:10.1016/j.ijrobp.2019.05.064
13. Tong YS, Tan J, Zhou XL, Song YQ, Song YJ. Systemic immune-inflammation index predicting chemoradiation resistance and poor outcome in patients with stage III non-small cell lung cancer. J Transl Med. 2017;15(1):221. doi:10.1186/s12967-017-1326-1
14. Jabbour SK, Kim S, Haider SA, et al. Reduction in Tumor Volume by Cone Beam Computed Tomography Predicts Overall Survival in Non-Small Cell Lung Cancer Treated With Chemoradiation Therapy. Int J Radiat Oncol Biol Phys. 2015;92(3):627–633. doi:10.1016/j.ijrobp.2015.02.017
15. Andersen PK, Klein JP, Rosthøj S. Generalised Linear Models for Correlated Pseudo-Observations, with Applications to Multi-State Models. Biometrika. 2003;90(1):15–27.
16. Grassberger C, Hong TS, Hato T, et al. Differential Association Between Circulating Lymphocyte Populations With Outcome After Radiation Therapy in Subtypes of Liver Cancer. Int J Radiat Oncol Biol Phys. 2018;101(5):1222–1225. doi:10.1016/j.ijrobp.2018.04.026
17. Suzuki R, Lin SH, Wei X, et al. Prognostic significance of pretreatment total lymphocyte count and neutrophil-to-lymphocyte ratio in extensive-stage small-cell lung cancer. Radiother Oncol. 2018;126(3):499–505. doi:10.1016/j.radonc.2017.12.030
18. Cho Y, Park S, Byun HK, et al. Impact of Treatment-Related Lymphopenia on Immunotherapy for Advanced Non-Small Cell Lung Cancer. Int J Radiat Oncol Biol Phys. 2019;105(5):1065–1073. doi:10.1016/j.ijrobp.2019.08.047
19. Kleinberg L, Sloan L, Grossman S, Lim M. Radiotherapy, Lymphopenia, and Host Immune Capacity in Glioblastoma: a Potentially Actionable Toxicity Associated With Reduced Efficacy of Radiotherapy. Neurosurgery. 2019;85(4):441–453. doi:10.1093/neuros/nyz198
20. Davuluri R, Jiang W, Fang P, et al. Lymphocyte Nadir and Esophageal Cancer Survival Outcomes After Chemoradiation Therapy. Int J Radiat Oncol Biol Phys. 2017;99(1):128–135. doi:10.1016/j.ijrobp.2017.05.037
21. Grewal AS, Min EJ, Long Q, et al. Early Tumor and Nodal Response in Patients with Locally Advanced Non-Small Cell Lung Carcinoma Predict for Oncologic Outcomes in Patients Treated with Concurrent Proton Therapy and Chemotherapy. Int J Radiat Oncol Biol Phys. 2020;106(2):358–368. doi:10.1016/j.ijrobp.2019.10.019
22. Contreras JA, Lin AJ, Weiner A, et al. Cardiac dose is associated with immunosuppression and poor survival in locally advanced non-small cell lung cancer. Radiother Oncol. 2018;128(3):498–504. doi:10.1016/j.radonc.2018.05.017
23. Joseph N, McWilliam A, Kennedy J, et al. Post-treatment lymphocytopaenia, integral body dose and overall survival in lung cancer patients treated with radical radiotherapy. Radiother Oncol. 2019;135:115–119. doi:10.1016/j.radonc.2019.03.008
24. MacLennan IC, Kay HE. Analysis of treatment in childhood leukemia. IV. The critical association between dose fractionation and immunosuppression induced by cranial irradiation. Cancer. 1978;41(1):108–111. doi:10.1002/1097-0142(197801)41:1<108::aid-cncr2820410116>3.0.co;2-z
25. McLaughlin MF, Alam M, Smith L, Ryckman J, Lin C, Baine MJ. Stereotactic body radiation therapy mitigates radiation induced lymphopenia in early stage non-small cell lung cancer. PLoS One. 2020;15(11):e0241505. doi:10.1371/journal.pone.0241505
26. Tang C, Liao Z, Gomez D, et al. Lymphopenia association with gross tumor volume and lung V5 and its effects on non-small cell lung cancer patient outcomes. Int J Radiat Oncol Biol Phys. 2014;89(5):1084–1091. doi:10.1016/j.ijrobp.2014.04.025
27. Xie X, Lin SH, Welsh JW, et al. Radiation-induced lymphopenia during chemoradiation therapy for non-small cell lung cancer is linked with age, lung V5, and XRCC1 rs25487 genotypes in lymphocytes. Radiother Oncol. 2020;154:187–193. doi:10.1016/j.radonc.2020.09.002
28. Bradley JD, Hu C, Komaki RR, et al. Long-Term Results of NRG Oncology RTOG 0617: standard- Versus High-Dose Chemoradiotherapy With or Without Cetuximab for Unresectable Stage III Non-Small-Cell Lung Cancer. J Clin Oncol. 2020;38(7):706–714. doi:10.1200/jco.19.01162
29. Jin JYHC, Xiao Y, et al. Higher radiation dose to immune system is, nonesmall cwpsipwsI, group clcAssoapc. J Med. 2017;99:S151–152.
30. Ellsworth SG. Field size effects on the risk and severity of treatment-induced lymphopenia in patients undergoing radiation therapy for solid tumors. Adv Radiation Oncol. 2018;3(4):512–519. doi:10.1016/j.adro.2018.08.014
31. Bruni A, Scotti V, Borghetti P, et al. A Real-World, Multicenter, Observational Retrospective Study of Durvalumab After Concomitant or Sequential Chemoradiation for Unresectable Stage III Non-Small Cell Lung Cancer. Front Oncol. 2021;11:744956. doi:10.3389/fonc.2021.744956
32. Karantanos T, Karanika S, Seth B, Gignac G. The absolute lymphocyte count can predict the overall survival of patients with non-small cell lung cancer on nivolumab: a clinical study. Clin Transl Oncol. 2019;21(2):206–212. doi:10.1007/s12094-018-1908-2
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.