Back to Journals » Vascular Health and Risk Management » Volume 20
Echocardiographic Parameters and Complication Profiles Among Adult Patients with Rheumatic Heart Disease at Jimma Medical Center
Authors Berhanu H , Mossie A, Morankar SN, Gemechu TD, Tegene E
Received 28 November 2023
Accepted for publication 3 February 2024
Published 4 April 2024 Volume 2024:20 Pages 157—166
DOI https://doi.org/10.2147/VHRM.S451957
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Mirna N Chahine
Hiwot Berhanu,1 Andualem Mossie,1 Sudhakar Narayan Morankar,2 Tadesse Dukessa Gemechu,3 Elsah Tegene3
1Department of Biomedical Sciences, Faculty of Medical Science, Jimma Institute of Health, Jimma University, Jimma, Ethiopia; 2Ethiopian Evidence Based Health Care Center, Department of Health, Behavior and Society, Faculty of Public Health, Institute of Health, Jimma University, Jimma, Ethiopia; 3Department of Internal Medicine, Institute of Health, Jimma University, Jimma, Ethiopia
Correspondence: Hiwot Berhanu, Department of Biomedical-sciences, Faculty of Medical Sciences, Jimma Institute of Health, Jimma University, P.O.Box: Jimma University378, Jimma, Ethiopia, Tel +251917324642, Email [email protected]
Background: Despite the fact that patients with rheumatic heart disease (RHD) need early medical attention and follow-up, most patients in developing countries tend to present with debilitating complications. The objective of this study was to evaluate the echocardiographic features of adult individuals diagnosed with RHD and examine the associated complications among patients who started follow-up at Jimma Medical Center’s (JMC) cardiac follow-up clinic.
Methods: A prospective cross-sectional study was conducted at JMC between January 5 and April 15, 2023. Echocardiographic patterns were taken by senior cardiologists; socio-demographic variables, anthropometric measurements, and behavioral factors were collected through a structured questioner.
Results: The study recruited a total of 115 participants, of whom 86 (74.8%) were female and 29 (25.2%) were male. The mean age of the patients was 32.31 (SD± 12.16) years. The mitral valve was affected in 98.26% of cases, while the aortic and tricuspid valve abnormalities were diagnosed in 49.5% and 21.7%, respectively. The most frequent combinations of valve lesions were mitral regurgitation (MR) + mitral stenosis (MS) + aortic regurgitation (AR) (15.7%), followed by MR + AR + TR (8.7%). The occurrence of MR+MS+AR was higher in females (17.4%) compared to males (10.3%), whereas the occurrence of MS+MR was higher in males (24.1%) compared to females (20.9%). Females have a severely reduced ejection fraction compared to males (84.8% vs 15.2%, P = 0.044). Nearly two-thirds (63.5%) of individuals experienced RHD-related complications; the most commonly encountered complications were pulmonary hypertension (26.1%) and atrial fibrillation (19.1%).
Conclusion: RHD predominantly affects individuals in their active and productive years, particularly females. Most patients have multiple-valve lesions.
Keywords: rheumatic heart disease, echocardiography, complication, Ethiopia
Background
Rheumatic heart disease, a post-streptococcal complication of rheumatic fever (RF), is a disorder characterized by the impairment of one or multiple-heart valves, resulting in significant structural and hemodynamic abnormalities.1 According to the Global Burden of Disease Study, the prevalence of RHD was 142.6 per 100,000 people in 2015, largely impacting low- and middle-income countries.2 Despite the fact that patients with RF/RHD require early medical attention and follow-up, a significant number of patients in developing nations tends to present with debilitating complications such as heart failure, pulmonary hypertension, and arrhythmias.3
In the diagnosis and management of RHD, echocardiography has the ability to detect up to 10 times more cases compared to relying solely on clinical examination.4,5 Likewise, echocardiography is an indispensable tool by providing valuable information about the severity of valve lesions, left ventricular (LV) chamber size, LV function, and pulmonary artery pressure, which are important indicators of cardiac health.6 Moreover, strain echocardiographic imaging has gained popularity as a prognostic and diagnostic tool for patients with valvular heart disease by offering valuable functional insights about left atrial reservoir strain and improving understanding of cardiac function as compared to the conventional echocardiography techniques.7,8
A study conducted in Nigeria Savannah showed that mitral regurgitation was the most common echocardiographic diagnosis present in 65.9% of the patients, followed by aortic valve disease in 19.5% of cases.9 Similarly, according to the report of the Global Rheumatic Heart Disease Registry, the majority (63.9%) of patients with RHD had moderate-to-severe multivalvular disease, complicated by heart failure (33.4%), pulmonary hypertension (28.8%), atrial fibrillation (AF) (21.8%), stroke (7.1%), infective endocarditis (4%), and major bleeding (2.7%).10 In the same token, a study conducted in Nepal discovered that the majority of patients were women, accounting for 71.3% of the total sample, and the average age was 44.24±14.24 years. The majority of the patients were presented to have severe mitral stenosis (41.2%) followed by severe mitral regurgitation (19.8%).11
Ethiopia, a nation heavily affected by RHD, experiences a significant burden from the disease.12 Echocardiographic analysis across six major referral hospitals in Ethiopia has revealed that RHD constitutes as much as 40.5% of the reported cases.13 Similarly, a study conducted at Dabat Health Centre in the Amhara region reported the highest prevalence of RHD-related mortality worldwide, with a rate of 125.3 per 1000 people. The study also highlighted that the average age at the time of death was 22 years.14 Therefore, the objective of this study was to evaluate the echocardiographic parameters and related complications in patients diagnosed with rheumatic heart disease.
Materials and Methods
Study Design and Setting
From January 5 to April 15, 2023, a cross-sectional study was carried out at Jimma Medical Centre, which is an academic institution with various departments. The center serves 15 million outpatients and 16,000 inpatients each year, with various departments operating 24 hours a day. One of its departments, internal medicine, includes a cardiac unit. This unit admits an average of 102 patients per month who present with various complaints related to cardiac problems. Additionally, the hospital runs a cardiac clinic twice a week as part of its chronic follow-up services, providing ongoing care and support to individuals with chronic cardiac conditions.
Study Participants
The study included all patients who were consecutively under medical follow-up at the cardiac clinic during the designated study period and diagnosed with rheumatic heart disease. The patients included were aged 15 years and above and had their diagnosis verified through echocardiography imaging.
Echocardiographic Parameter
Following the recommendations established by the American Society of Echocardiography, two adult cardiologists evaluated rheumatic heart disease using a Toshiba AplioTM ultrasound system (TUS-A500, Shimoishigami, Japan).15 The diagnosis of RHD was made using the WHF echocardiographic imaging criteria. The criteria for valve regurgitation include morphological features (thickening, restricted leaflet motion, prolapse, coaptation defect, excessive leaflet tip motion) and pathological characteristics (seen in two views, jet length, velocity, pan-systolic/pan-diastolic jet in at least one envelope). The criteria for the diagnosis of mitral stenosis were signs of increased flow speed through the mitral valve, indicated by a mean pressure gradient greater than 4mmHg. Mitral stenosis severity was evaluated using planimetry and pressure half-time and classified as mild if the mitral valve area (MVA) exceeded 1.5 cm2, moderate if MVA ranged from 1.1 to 1.5 cm2, and severe if MVA was less than 1.0 cm2.16,17 The severity of valvular dysfunction was categorized as mild, moderate, and severe, following the guidelines provided by the American College of Cardiology/American Heart Association (ACC/AHA).18
Data Collection Tool and Procedures
Four trained BSc nurses, who were deployed at the cardiac clinic, collected the data. Socio-demographic variables, anthropometric measurements, and behavioral factors were assessed using an interviewer-administered structured questionnaire. The participants’ medical charts were used to gather the patients’ previous complications. The questioner was initially prepared in English, translated to two local languages (Amharic and Afaan Oromo) and retranslated back to the English language for consistency check.
Sample Size Determination and sampling Procedure
The sample size was determined using Epi Info STAT CALC version 7.2.4.0, considering the following assumptions: a prevalence of valvular dysfunction among RHD patient 7.5%, based on a previous study conducted in Nigeria,9 a confidence level of 95%, and a margin of error of 5%. Taking into account a non-response rate of 5%, a sample size of 115 was obtained.
Data Analysis
The data was processed and analyzed using Epidata 3.1, and then transferred to SPSS version 25 for further analysis. The Kolmogorov–Smirnov test was used to evaluate the normality of variables and revealed that the data was normally distributed. The outputs of the analysis were then sorted by summarizing categorical and continuous data and finally resented using counts, percentages, and standard deviations. Chi-square test was utilized to compare the proportions of categorical variables, evaluating the statistical significance of the association and determining the level of significance.
Result
In the study, a total of 115 participants were recruited, of which 86 (74.8%) were female and 29 (25.2%) were male, representing a 1:2.5 sex ratio. The mean age of the patients was 32.31 ± 12.16 years, with an age range of 16 to 66 years. The age group with the highest proportion of patients with RHD was 25–34 years, accounting for 40 individuals (34.8%), following the age group of 35–44 years, with 31 patients (27.0%), as shown in (Table 1)
 |
Table 1 Socio-Demographic Characteristics of Patients with RHD at JMC Cardiac Clinic from January 5 to April 15, 2023 (n=115) |
Echocardiographic Parameters
Pathological Valve Lesions
In the majority of cases, the mitral valve was found to be the most involved, accounting for 98.26% of the cases. The aortic valves were the second most commonly involved valve, seen in 49.5% of the cases and tricuspid valve is involved in 21.7% of the cases. Among isolated valve involvement cases, mitral regurgitation was the most common, observed in 15 individuals (13%), followed by mitral stenosis, which accounted for 3 cases (2.6%), and aortic regurgitation, which was present in 1 case (0.9%). The majority of the patients were found to have multiple valve lesions. The most common combination of multiple valve diseases observed was MR+MS+AR and MR+AR+TR, accounting for 15.7% and 8.7% of the cases, respectively. The occurrence of MR+MS+AR was more common among females (17.4%) than in males (10.3%), while the occurrence of MS+MR was higher in males (24.1%) compared to females (20.9%). Combined MR+AR was present in 7.8% of patients with a p value of 0.008, as presented in (Table 2)
 |
Table 2 Classification of Valvular Lesions in Adults with Rheumatic Heart Disease at JMC Cardiac Clinic from January 5 to April 15, 2023 (n = 115) |
Severity of Valvular Dysfunction
Among the patients with RHD, mitral valve disease (MR or MS) was the most common valve disease present in 98.26% of the cases. Mitral regurgitation was identified as the most prevalent severe valvular lesion, representing 35.65% of all cases followed by aortic regurgitation (AR) at 18.26% as shown in (Table 3)
 |
Table 3 Severity of Valve Lesion Among Adults with RHD Attending at JMC Cardiac Clinic from January 5 to April 15, 2023 (n=115) |
Echocardiographic Parameters
Nearly one-fifth of the study participants (18.3%) has severely reduced left ventricular systolic function; the mean left ventricular systolic dimension (LVSd) was 54.4±8.3mm. Severely reduced left ventricular posterior wall end diastole and end systole (LVPWd) function is observed among 16.5% of the patients, and the mean LVPWd was 10.01±1.18 mm.
Twenty-six percent of the participants have severely reduced ejection fractions. Whereas the mean left ventricular ejection fraction (EF) in percentage was 55.2±9.13. High number of females have low level of ejection fraction compared to males (84.8% vs 15.2%, p = 0.044). One-third of the participants (28.7%) have a decreased tricuspid annular plane systolic excursion (TAPSE), and the mean TAPSE was 17.53±2.8mm.
Regarding fractional shortening, 26% of the patients have severely reduced systolic function, with a mean value of 30.47±6.03. Half of the patients have severely enlarged left atrium, and the mean left atrial diameter was 41.87±10.55mm as presented in (Table 4)
 |
Table 4 Echocardiographic Parameters Severity Classification Among Adults with RHD at JMC Cardiac Clinic from January 5 to April 15, 2023 (n = 115) |
Complication Related to Rheumatic Heart Disease
Among 115 patients, 73 (63.5%) have rheumatic heart disease-related complications. Pulmonary hypertension accounts for 26.1%, followed by atrial fibrillation (19.1%), left ventricular thrombus (6.1%), stroke (4.3%), valvular cardiomyopathy (4.3%), and infective endocarditis (3.5%) as presented in (Figure 1)
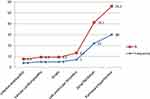 |
Figure 1 Complications related to rheumatic heart disease. |
Discussion
The current study, conducted within a hospital setting, presents data on the echocardiographic characteristics of rheumatic heart disease, the extent of valve dysfunction, and complications encountered in the Jimma Medical Center cardiac clinic. Our study investigated the age group with the highest proportion of patients with RHD, which was found to be between 25 and 44 years, accounting for the majority of the cases (61.8%). This study is consistent with the study conducted in the Northern Territory of Australia. Where the highest prevalence of RHD is typically observed during adulthood, specifically between the ages of 25 and 45.19 A similar, published study at the National Heart Center of Nepal by Koirala PC et al, reported as RHD to be more prevalent among individuals aged 10 to 40 years, with a higher occurrence among females.20
The gender distribution in this study demonstrated a male-to-female ratio of 1:2.5, indicating a higher proportion of female participants. Similar proportion of studies have been reported by Adem et al and21 and Zühlke, Liesl et al.10 Even though the exact reasons for this gender disparity are not fully understood, the higher percentage of RHD in females can be attributed to several factors, like stronger immune responses in females, potential genetic predispositions, and social and cultural factors such as limited healthcare access could be the possible explanations.
This study revealed that the mitral valve was the most affected valve, accounting for 98.2%, followed by the aortic valve, observed in 49.5% of the participants. Likewise, the study conducted at St Paul’s Hospital Millennium Medical college (SPMMC) also demonstrated that the mitral valve was the valve most frequently affected valve, accounting for 95.6% of individuals followed by aortic valve (61.5%) of individuals.22 In isolated valve involvement cases, the most common valvular impairment observed was mitral regurgitation, accounting for 13%, followed by mitral stenosis, which accounted for 2.6%, and aortic regurgitation, which was present in 0.9% of individuals. This study is comparable to the study conducted in Nigeria Savanna, which reported that mitral regurgitation (38.0%) is the commonest valve, followed by mitral stenosis (7.8%), and pure aortic regurgitation (3.1%).9 The most common combination of multiple valve diseases observed was MR+MS+AR accounting for 15.7% of the cases. Whereas a study conducted in central Nepal reported that combined mitral plus aortic valve lesions were the commonest contributing 9.78%.20
According to this study, the occurrence of MR+MS+AR was more common among females (17.4%) than in males (10.3%). This study is comparable to the study by Koirala PC et al, in which MR+MS+AR were higher in females (36.49%) compared to males (15.25%).20 Similarly, the current study also found that the occurrence of MS+ MR was higher in males (24.1%) compared to females (20.9%) and combined MR+AR was present in 7.8% of patients and was statistically significant in relation to sex with a p value of 0.008. This study supports the study conducted by Adem et al, where MS+MR was more prevalent among males (35.6%) than females (28.3%).22
In general, most of the individuals involved in the present study exhibited more severe valvular dysfunction than mild valvular dysfunction. In particular, MR and AR were identified as having severe levels of dysfunction. This study is consistent with a study conducted by SPMMC22 and a study in the northern part of Ethiopia.23 On the contrary, the current finding revealed that high number of severe form of valvular lesion compared to the study by a multisite echocardiography-based study conducted in Ethiopia24 and north India25 that indicate the majority of patients presented with mild valvular lesions. The variations in the studies could be due to the differences among study participants. The participants with severe forms of valvular dysfunction are from hospital settings and presented with symptoms of heart failure, while participants with mild valvular lesions are individuals at school and notably healthy individuals without symptoms.
Regarding the echocardiographic findings, nearly one-fifth of the study participants (18.3%) have severely reduced left ventricular systolic dysfunction; the mean LVSd was 54.4±8.3mm; this study resembles a study by Rudiktyo et al, where the patients have a mean of 56.63 ± 8.57mm.26
This study discovered that the mean left ventricular posterior wall end diastole and end systole (LVPWd) was found to be 10.01±1.18mm. This finding is higher than a study conducted in Multan, Pakistan, where the mean LVPWd was reported as 7.13 ± 1.95mm27 and another study by Meel et al from South Africa also reported a mean LVPWd of 8.5 ± 1.5mm.28 Differences in LVPWd among studies may be attributed to various factors. Firstly, variations in the characteristics of the study populations, such as age, sex, and ethnicity, can influence ventricular wall thickness and contribute to different mean values.29 The other possible factor could be due to discrepancies in the measurement techniques employed to assess LVPWd can impact the accuracy of the measurements and variances in image acquisition, echocardiographic equipment, and measurement protocols.30
In our study, a quarter of the participants (26%) exhibited a severely reduced ejection fraction, while 49 individuals (42.6%) had a severely dilated left atrium, and 33 participants (28.5%) experienced a decline in tricuspid annular plane systolic excursion (TAPSE). Similarly, a study carried out in Dares Salaam, Tanzania, among RHD patients with arrhythmia revealed that 80 individuals (20.5%) had reduced TAPSE, 20 participants (5.1%) displayed a severely reduced ejection fraction, and 263 individuals (67%) exhibited a severely dilated left atrium.31
In terms of complications observed in our study, a majority of participants (63.5%) experienced complications related to RHD. Among these complications, pulmonary hypertension accounted for 26.1%, while atrial fibrillation occurred in 19.1% of cases. Other complications included left ventricular thrombus (6.1%), stroke (4.3%), valvular cardiomyopathy (4.3%), and infective endocarditis (3.5%). This study is comparable with a study conducted in Nigeria where the major RHD-related complications were pulmonary hypertension in 72.1% of cases, valvular cardiomyopathy in 31.8% of cases, and functional tricuspid regurgitation in 30.2%, atrial fibrillation in 10.1% of cases, while left ventricular thrombus occurred in 2.3% of cases.9 Whereas a study conducted in a tertiary hospital in Addis Ababa shows that complications related to RHD account for 83.6% of cases. The most common complication encountered was heart failure (61.4%), followed by pulmonary hypertension (59.3%), malnutrition (50.7%), and infectious endocarditis (3.6%).3
Limitation of the Study
The main limitation of a study is that it exclusively includes patients from a hospital setting, which can limit the ability to generalize the findings to the general population. The other limitation of the study is that it is unable to use cardiac MRI, which is a better tool for visualizing the valve anatomy. Likewise, the study used conventional echocardiography instead of strain echocardiography due to the unavailability of strain echocardiography, which could have provided additional functional information regarding left atrial reservoir strain in the study. Further studies should be designed to evaluate the potential role of strain echocardiographic imaging in patients with rheumatic heart disease.
Conclusion
The current study reveals that rheumatic heart disease predominantly affects individuals in their active and productive years, particularly females. A majority of the patients included in the study have multiple-valve lesions. Mitral valve was the commonest valve affected. Approximately two-thirds of patients experienced RHD-related complications, with pulmonary hypertension and atrial fibrillation being the most common. As a result, it is recommended to regularly conduct echocardiography for individuals diagnosed with RHD, with a particular emphasis on females and younger adults to facilitate early detection and treatment of the disease before complications arise.
Abbreviations
AR, aortic regurgitation; AS, aortic stenosis; EF, Ejection Fraction; FS, Fractional shortening; JMC, Jimma Medical; LV, left; LVIDd, left ventricular internal diameter end; LVPWd, left ventricular posterior wall end diastole and end systole; LVSd, left ventricular systolic dysfunction; MR, mitral regurgitation; MS, mitral stenosis; RF, rheumatic fever; RHD, Rheumatic heart disease; SPSS, Statistical Package for social science; TAPSE, Tricuspid annular plane systolic excursion; TR, tricuspid regurgitation.
Data Sharing Statement
Data will be accessible from the corresponding author upon request.
Ethics Approval and Consent to Participate
The study was conducted according to the Helsinki Declaration. Ethical approval of the research protocol was obtained from Jimma University Institute of Health with reference number JUIH/IRB/277/23. Informed consent was obtained from all participants before the start of the study. Participants were informed of their right to withdraw from the study at any time and that their participation was voluntary. All data collected was kept confidential and anonymous.
Acknowledgments
We would like to express our deepest gratitude to Jimma University, Institute of Health for offering the opportunity and technical support to undertake the study. We would also like to acknowledge the staff of cardiac clinic and our data collectors for their support during data collection. Our foremost appreciation also goes to the study participants for their willingness and cooperation.
Author Contributions
HB: designed the study, analyzed it, interpret the result and prepare the manuscript for publication. AM: Participated in designing the study, supervision of the research project and review the draft of the manuscript. ET: supervised the data collection, interpreted the Echocardiography. TDG: supervised the data collection, interpreted the Echocardiography. SNM: provided constructive comments and review the draft of the manuscript. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Franczyk B, Gluba-Brzózka A, Rysz-Górzyńska M, Rysz J. The role of inflammation and oxidative stress in rheumatic heart disease. Int J Mol Sci. 2022;23(24):15812. doi:10.3390/ijms232415812
2. Watkins DA, Johnson CO, Colquhoun SM, et al. Global, regional, and national burden of rheumatic heart disease, 1990–2015. N Engl J Med. 2017;377(8):713–722. doi:10.1056/NEJMoa1603693
3. Desta TT, Gezachew A, Eshetu K. Descriptive analysis of rheumatic heart disease related complications in pediatric patients at tertiary hospital, Addis Ababa. Ethiopia Pediatric Health Med Ther. 2023;14:45–57. doi:10.2147/PHMT.S396854
4. Marijon E, Ou P, Celermajer DS, et al. Prevalence of rheumatic heart disease detected by echocardiographic screening. N Engl J Med. 2007;357(5):470–476. doi:10.1056/NEJMoa065085
5. Marijon E, Celermajer DS, Tafflet M, et al. Rheumatic heart disease screening by echocardiography: the inadequacy of world health organization criteria for optimizing the diagnosis of subclinical disease. Circulation. 2009;120(8):663–668. doi:10.1161/CIRCULATIONAHA.109.849190
6. Seitler S, Zuhair M, Shamsi A, et al. Cardiac imaging in rheumatic heart disease and future developments. Eur Hear J Open. 2023;3(2):1–11. doi:10.1093/ehjopen/oeac060
7. Sonaglioni A, Nicolosi GL, Rigamonti E, Lombardo M. Incremental prognostic role of left atrial reservoir strain in asymptomatic patients with moderate aortic stenosis. Int J Cardiovasc Imaging. 2021;37(6):1913–1925. doi:10.1007/s10554-021-02175-6
8. Cvijic M, Voigt JU. Application of strain echocardiography in valvular heart diseases. Anatol J Cardiol. 2020;23(5):244–253. doi:10.14744/AnatolJCardiol.2020.09694
9. Sani MU, Karaye KM, Borodo MM. Prevalence and pattern of rheumatic heart disease in the Nigerian Savannah: an echocardiographic study. Cardiovasc J Afr. 2007;18(5):295–299.
10. Zühlke L, Engel ME, Karthikeyan G, et al. Characteristics, complications, and gaps in evidence-based interventions in rheumatic heart disease: the Global Rheumatic Heart Disease Registry (the REMEDY study). Eur Heart J. 2015;36(18):1115–1122. doi:10.1093/eurheartj/ehu449
11. Nepal R, Bista M, Dhungana SP. Patterns of rheumatic heart disease and treatment practices at tertiary care center in Nepal: a descriptive cross-sectional study. J Nepal Med Assoc. 2020;58(230):784–788. doi:10.31729/jnma.5405
12. Berhanu H, Mekonnen Y, Workicho A, et al. The prevalence of rheumatic heart disease in Ethiopia: a systematic review and meta-analysis. Trop Dis Travel Med Vaccines. 2023;9(1):1–11. doi:10.1186/s40794-023-00192-y
13. Yadeta D, Guteta S, Alemayehu B, et al. Spectrum of cardiovascular diseases in six main referral hospitals of Ethiopia. Heart Asia. 2017;9(2):1–5. doi:10.1136/heartasia-2016-010829
14. Günther G, Asmera J, Parry E. Death from rheumatic heart disease in rural Ethiopia. Lancet. 2006;367(9508):391. doi:10.1016/S0140-6736(06)68128-2
15. Mitchell C, Rahko PS, Blauwet LA, et al. Guidelines for performing a comprehensive transthoracic echocardiographic examination in adults: recommendations from the American society of echocardiography. J Am Soc Echocardiogr. 2019;32(1):1–64. doi:10.1016/j.echo.2018.06.004
16. Reméanyi B, Wilson N, Steer A, et al. World Heart Federation criteria for echocardiographic diagnosis of rheumatic heart disease-an evidence-based guideline. Nat Rev Cardiol. 2012;9(5):297–309. doi:10.1038/nrcardio.2012.7
17. Omran AS, Arifi AA, Mohamed AA. Echocardiography in mitral stenosis. J Saudi Hear Assoc. 2011;23(1):51–58. doi:10.1016/j.jsha.2010.07.007
18. Baumgartner H, Hung J, Bermejo J, et al. Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice. J Am Soc Echocardiogr. 2009;22(1):1–23. doi:10.1016/j.echo.2008.11.029
19. Lawrence JG, Carapetis JR, Griffiths K, Edwards K, Condon JR. Acute rheumatic fever and rheumatic heart disease: incidence and progression in the Northern Territory of Australia, 1997 to 2010. Circulation. 2013;128(5):492–501. doi:10.1161/CIRCULATIONAHA.113.001477
20. Koirala PC, Sah RK, Sharma D. Pattern of rheumatic heart disease in patients admitted at tertiary care centre of Nepal. Nepal Hear J. 2018;15(1):29–33. doi:10.3126/njh.v15i1.19713
21. Adem A, Gemechu TD, Jarso H, Reta W. Rheumatic heart disease patients’ adherence to secondary prophylaxis and associated factors at hospitals in Jimma zone, southwest Ethiopia: a multicenter study. Patient Prefer Adherence. 2020;14:2399–2406. doi:10.2147/PPA.S281413
22. Adem A, Mulatu HA. Echocardiographic pattern of rheumatic heart disease among adults at St. Paul’s Hospital Millennium Medical College cardiac unit, Addis Ababa, Ethiopia: a cross-sectional study. MJH. 2022;1:2.
23. Engida HB, Mamuye MA, Yehun YT, et al. Patterns of cardiovascular diseases among cardiac disease suspected patients in Bahir Dar City, Ethiopia: rheumatic heart disease in patients suspected with Heart diseases Patterns Of Cardiovascular Diseases Among Cardiac Disease. Ethiop Med J. 2022;60(1):19–26.
24. Yadeta D, Hailu A, Haileamlak A, et al. Prevalence of rheumatic heart disease among school children in Ethiopia: a multisite echocardiography-based screening. Int J Cardiol. 2016;221:260–263. doi:10.1016/j.ijcard.2016.06.232
25. Raina SK. Analyzing trends- A comment on epidemiological trends of RF/RHD in school children of Shimla in North India. Indian J Med Res. 2013;138:564.
26. Rudiktyo E, Yonas E, Cramer MJ, Siswanto BB, Doevendans PA, Soesanto AM. Impact of rheumatic process in left and right ventricular function in patients with mitral regurgitation. Glob Heart. 2023;18(1). doi:10.5334/gh.1192
27. Shahid S, Khurram H, Billah B, Akbar A, Shehzad MA, Shabbir MF. Machine learning methods for predicting major types of rheumatic heart diseases in children of Southern Punjab, Pakistan. Front Cardiovasc Med. 2022;9:1–10. doi:10.3389/fcvm.2022.996225
28. Meel R, Peters F, Khandheria BK, Libhaber E, Essop M. Atrial-ventricular function in rheumatic mitral regurgitation using strain imaging. Echo Res Pract. 2020;7(2):9–17. doi:10.1530/ERP-19-0034
29. Chen C, Sung KT, Shih SC, et al. Age, gender and load-related influences on left ventricular geometric remodeling, systolic mid-wall function, and NT-ProBNP in asymptomatic Asian population. PLoS One. 2016;11(6):1–15.
30. Letnes JM, Eriksen-Volnes T, Nes B, Wisløff U, Salvesen Ø, Dalen H. Variability of echocardiographic measures of left ventricular diastolic function. The HUNT study. Echocardiography. 2021;38(6):901–908. doi:10.1111/echo.15073
31. Makatu CD, Mutagaywa RK, Peter P, Barongo A, Kifai E. Prevalence, clinical characteristics and echocardiographic parameters of arrhythmias among patients with rheumatic heart disease attending Jakaya Kikwete Cardiac Institute: a prospective cohort study. BMC Cardiovasc Disord. 2023;23(1):1–9. doi:10.1186/s12872-023-03427-0
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
