Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 15
Dyslipidemia and Nutritional Status of HIV-Infected Children and Adolescents on Antiretroviral Treatment at the Comprehensive Chronic Care and Training Center of Jimma Medical Center
Authors Ambisa Lamesa T , Getachew Mamo A, Arega Berihun G, Alemu Kebede R, Bekele Lemesa E, Cheneke Gebisa W
Received 7 June 2023
Accepted for publication 26 August 2023
Published 11 September 2023 Volume 2023:15 Pages 537—547
DOI https://doi.org/10.2147/HIV.S418729
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Olubunmi Akindele Ogunrin
Tolera Ambisa Lamesa,1 Aklilu Getachew Mamo,1 Gebeyaw Arega Berihun,1 Regassa Alemu Kebede,1 Eba Bekele Lemesa,2 Waqtola Cheneke Gebisa1
1School of Medical Laboratory Science, Jimma University, Jimma, Ethiopia; 2Mycobacteriology Research Center, Jimma University, Jimma, Ethiopia
Correspondence: Tolera Ambisa Lamesa, Tel +251937187622, Email [email protected]
Background: Highly active antiretroviral treatment is beneficial to suppress human immune virus replication in infected individuals. However, dyslipidemia and other metabolic abnormalities have emerged due to antiretroviral treatment. The prevalence of dyslipidemia in children and adolescents on antiretroviral treatment varies from 20% to 70%. The lack of data on children and adolescents in Ethiopia was the rationale for conducting this study. We aimed to determine prevalence of dyslipidemia and nutritional status in children and adolescents on follow-up at Jimma medical center.
Materials and Methods: A hospital-based cross-sectional study was conducted with 150 children and adolescents on follow-up at Jimma medical center. A systematic sampling technique was employed. An interview was carried out to collect socioeconomic and demographic data and a review of medical records was carried out to collect patients’ clinical data. Anthropometric data were computed using the CDC growth chart. About 3– 5mL of fasting blood was collected to measure lipid profile. Multivariable logistic regression was performed to find the association between risk factors and lipid profile.
Results: The overall prevalence of dyslipidemia in this study was 72%. About 72% and 21.3% of study subjects had low high-density lipoprotein and high triglyceride, respectively. Significant associations were observed between BMI for age ≤ 5% (AOR: 2.02, 95% CI: 1.14– 3.66; P=0.015) and low high-density lipoprotein; greater than 150 months on treatment (AOR: 1.02, 95% CI: 1.00– 1.03; P=0.01) and high triglyceride; and BMI for age ≤ 5% (AOR: 1.86, 95% CI: 1.03– 1.37; P=0.04) and high triglyceride.
Conclusion: BMI for age < 5%, treatment duration of greater than 150 months, and parents’ educational level were significantly associated with dyslipidemia, so it is recommended that monitoring of those variables will help to reduce dyslipidemia and its complications in children and adolescents receiving treatment.
Keywords: HIV/AIDS, HAART, dyslipidemia, nutritional status, JMC
Introduction
The human immunodeficiency virus (HIV) pandemic is still spreading in the human population worldwide.1 The World Health Organization (WHO) estimated that, of about 1.7 million children under the age of 15 living with HIV, about 160,000 acquired the virus and 98,000 died from HIV-1-related causes in 2021.2
The introduction of antiretroviral therapy (ART) showed valuable results in HIV-infected individuals; it reduced morbidity and mortality, reduced the incidence of opportunistic diseases, increased length and quality of life, and improved neural development and linear growth in growing children.2–5
Protease inhibitors (PIs), like ritonavir (RTV), darunavir and atazanavir, are well known to cause high triglycerides (TG), high total cholesterol and low high-density lipoprotein cholesterol (HDL-C) levels.6 It was found that children and adolescents on a lopinavir/ritonavir (LPV/r) regimen had a four times greater chance of presenting with hypercholesterolemia and elevated TG levels when compared to those do not on ART.7,8 Atazanavir and darunavir are the newer protease inhibitors and have safer lipid profiles compared to LPV/r.8
Nucleoside reverse transcriptase inhibitors (NRTIs), especially stavudine, cause long-term metabolic and cardiovascular complications in children and adolescents. Longer duration of non-nucleoside reverse transcriptase inhibitor (NNRTI) exposure is modestly associated with high low-density lipoprotein cholesterol (LDL-C) among children and adolescents.6
The prevalence of metabolic abnormalities (including dyslipidemia) among children and adolescents who are taking ART varies between 20% and 70%, and the risk of developing hypercholesterolemia in children exposed to ART is twice as high as that for adults, depending on the current ART regimen.9
Dyslipidemia in children and adults increases the risk of developing cardiovascular disease.7,10 When atherogenic lipids are abnormally increased, they cause changes in the cardiovascular system that are independent cardiovascular risk factors and can be used as surrogates of atherosclerosis.11 In adolescents, elevated levels of LDL-C may cause permanent changes in coronary arteries, which play a role in ischemic heart disease development.11
In 2022, WHO reported that 149.2 million children aged under five had stunted growth, and 45.4 million had wasted growth. The number of children with stunting is declining in all regions except Africa. About three-quarters of all of all children malnutrition occurring in Asia. Malnutrition accounted for about 45% of deaths in under-five children worldwide in 2022. In the same year, anemia was reported in 40% of those under-five children.12 The prevalence of malnutrition in HIV-infected children in sub-Saharan Africa is 40%.13
The prevalence of malnutrition in HIV-infected children in sub-Saharan Africa is as high as 40%.13 This malnutrition is a risk factor for poor cognitive development, premature death, and other health consequences.14 Among children with severe malnutrition, the risk of death is three times higher in HIV-infected children compared to those who are not infected.15
There is evidence that HIV/AIDS patients have a greater chance of developing dyslipidemia due to both highly active antiretroviral therapy (HAART) and HIV itself. Other risk factors that may contribute to dyslipidemia in HIV/AIDS patients include family history of dyslipidemia, HIV clinical stage, duration of HAART, lifestyle, and nutritional status. When compared to those not treated with PI, HIV-positive children and adolescents are less likely to be malnourished but they develop dyslipidemia.16
The nutritional status of children and adolescents is compromised in developing countries. The nutritional status of children and adolescents on ART is associated with improvements in metabolic complications such as hyperlipidemia or hypercholesterolemia.17 Anthropometric status of children on HAART is influenced by age, preceding comorbidities, and by programmatic factors. By improving programmatic factors, the nutritional status of HIV-infected children improves.18
There is a scarcity of reports revealing the association of dyslipidemia with nutritional status in children and adolescents receiving HAART treatment in the study area. Therefore, we aimed to determine the prevalence of dyslipidemia and the association of dyslipidemia with associated risk factors including nutritional status of children and adolescents on follow-up at the Comprehensive Chronic Care and Training Center of Jimma Medical Center (JMC).
General Objective
To determine the association of dyslipidemia with nutritional status of children and adolescents on follow-up at the Comprehensive Chronic Care and Training Center of JMC from June 20 to October 10, 2022.
Specific Objectives
To determine the prevalence of dyslipidemia, factors associated with dyslipidemia, and the nutritional status of children and adolescents on follow-up at the Comprehensive Chronic Care and Training Center of JMC from June 20 to October 10, 2022.
Materials and Methods
Study Population
This hospital-based cross-sectional study included 150 children and adolescents who were on follow-up at the Comprehensive Chronic Care and Training Center of JMC, Ethiopia from June 20 to October 10, 2022.
Eligibility Criteria
The inclusion criteria were as follows: patients who were less than or equal to 19 years; patients who did not take appetite stimulants or did not undergo enteral or parenteral nutrition therapy, and patients who had been on treatment with HAART for at least three months before the study.
The following conditions were excluded: diabetic mellitus, liver disease, acute or chronic pancreatitis, and diarrhea. Patients who took lipid-lowering drugs and patients who developed illness within three months before the beginning of the study were excluded.
Study Participant Selection Process
Sampling Technique
Out of the 257 children and adolescents on HAART follow-up, 150 patients were selected by circular systematic sampling so that every other individual was selected (see Figure 1).
 |
Figure 1 Flow chart that shows sampling process. |
Sample Size Determination
To the best of our knowledge, it was not possible to find a study with a similar objective in Ethiopia. So, a study with similar objectives which was conducted in India19 was used. The overall prevalence of dyslipidemia in children and adolescents was 38.3 according to the Indian study. Sample size was calculated using the single proportion formula. Taking a 5% non-respondence rate, the sample size was 19 +150 =168.
Study Variables
The study outcome variable was dyslipidemia. The effect variables include: age, sex, income, educational level, residence, economic status, parent’s educational level, current use of antiretroviral therapy, total duration on ART, treatment adherence, viral load, CD4+ cell count, WHO clinical stage, BMI age percentage, weight for age percentage and height for age percentage.
Data Collection for Socioeconomic and Demographic Markers, Immunologic Markers, Virological Markers, HAART Regimen and Health Status Data Collection
A structured interview was carried out by professional nurses with both participants and their families to collect socioeconomic and demographic characteristics, using the interviewer-administered questionnaire method.
Characteristics like viral load, WHO clinical stage, mode of transmission, current use of antiretroviral therapy, total months on ART, treatment adherence, viral load, and CD4+ cell count were obtained by medical record review.
Measurement of Anthropometric Parameters
Height was measured using a stadiometer and weight was taken using calibrated standard balance. BMI for age, weight for age, and height for age were computed from patients’ data using the CDC reference growth chart. The cut-off value for nutritional status was based on the percentiles of the CDC 2022 report providing the growth charts of children and adolescents from 2 to 20 years of age.20
Specimen Collection and Lipid Profile Measurements
Specimens of about 3–5 mL of fasting blood were collected from HIV-positive children and adolescents after a minimum of 12 hours fasting during their regular visits to JMC. Following the standard operating procedures and manual of the Cobas 6000 analyzer at the clinical chemistry unit of JMC, serum specimens were prepared from the collected whole blood, and the enzymatic colorimetric principle was used to quantify total cholesterol, high-density lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL) cholesterol, and triglycerides (TG) using Cobas c 501, a module of the Cobas 6000 analyzer series.
Dyslipidemia was defined according to the American Heart Association guidelines for primary prevention of atherosclerotic cardiovascular disease beginning in childhood.21 Accordingly, if a patient had any of the following, a label of dyslipidemia was assigned; hypercholesterolemia: total plasma cholesterol >170 mg/dl; hypertriglyceridemia; triglyceride >150 mg/dl; LDL cholesterol >130 mg/dl; HDL cholesterol <35 mg/dl.
Statistical Analysis
Data were entered into EpiData version 6.6.0.6 statistical software, and then the data in stata format were exported to SPSS version 25 for analysis.
The mean differences between HDL-C, LDL-C, and triglyceride and independent variables were tested by independent sample t-test. ANOVA with post hoc test was used to test the mean lipid level differences against independent variables that have more than two categories. A binary logistic regression analysis was carried out to select nominate variables at entry probability of ≤0.25. Only variables with a p-value of <0.05 remained in the final multivariable logistic regression model.
Results
Socioeconomic and Demographic Characteristics
Out of 150 respondents, 77 (51.3%) were boys and 73 (48.7%) were girls. The mean age of the study participants in years was 14.78 (SD=3.18). Most of the study participants resided in urban areas (n=124, 82.7%) rather than rural areas (n=26, 17.3%). Most of the study participants’ families were government employees (n=39, 26%). For about 41.3% of study participants’ families, primary school was the highest educational level achieved. The majority (54.7%) of study participants were from the middle average (2250–9080 birr per month) economic class. The details are available in Table 1.
 |
Table 1 Socioeconomic and Demographic Characteristics, Immunologic Markers, HAART Regimen and Health Status Characteristics of Children and Adolescents on ART Follow-Up at JMC, 2022 |
Patients’ Immunologic Markers, HAART Regimen, and Health Status
The majority of the study participants (139, 92.7%) had suppressed recent viral load. Above three-fourths of the study participants (77.3%) had good treatment adherence. Majority of the participants (68.7%) were on TDF+3TC+DTG combination therapy (Table 1).
Prevalence of Dyslipidemia
The overall prevalence of dyslipidemia in children and adolescents was 72%. About 108 (72%) of study subjects had low HDL-C (≤35mg/dL), 32 (21.3%) had triglyceride (≥130mg/dL), and there was no abnormality in total cholesterol and LDL-C.
Nutritional Status
In this study, abnormality in nutritional status was found and described as follows: height for age of <5% was found in 81 (54%) participants, weight for age of <5% was found in 65 (43.3%) participants, and BMI forage of >95% was found for 5 (3.3%) participants (Table 2).
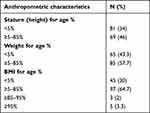 |
Table 2 Anthropometric Characteristics of Children and Adolescents on ART Follow-Up at JMC 2022 |
Lipid Profile Status vs HAART
Dyslipidemia was higher among those who used a combination of TDF, 3TC and ATV/R and TDF+3TC+DTG (Figure 2).
 |
Figure 2 Lipid profile status of children and adolescents according to the treatment regimen used at JMC, 2022. |
Dyslipidemia and Its Associated Factors
The mean differences in lipid levels with different variables are presented in Table 2. There was a significant mean triglyceride level difference according to BMI for age (P=0.02), mean HDL-C level difference according to HAART (p <0.001), mean HDL-C level difference according to BMI for age (p <0.001), and mean triglyceride level difference according to weight for age (p =0.02) (Table 3).
 |
Table 3 Anthropometric, Gender and Regimen Mean Differences in Children and Adolescents on HAART by Lipid Profile Level at JMC, 2022 |
In assessing the risk factors for dyslipidemia using binary logistic regression, the following factors showed a significant association with lipid level: residence of participant, parents’ educational level, type of HAART regimen, total duration of treatment, treatment adherence, parents’ economic status, weight for age, and BMI for age. However, in multivariable logistic regression, BMI for age of ≤5% (AOR: 2.02, 95% CI: 1.14–3.66, P=0.015) with HDL-C of <35 mg/dl, treatment duration (AOR: 1.02, 95% CI: 1.00–1.03, P=0.01) with triglyceride of ≥130mg/dl, BMI for age of ≤5% (AOR: 1.86 95% CI: 1.03–1.37, P=0.04) with triglyceride of ≥130 mg/dl, and parents’ primary and secondary educational level with normal lipid level were shown to be statistically significant associations.
Furthermore, children and adolescents with parents who had attended only primary school were 7.3 times more likely to have a normal lipid level, and those whose parents had attended secondary school were 5.15 times more likely to have a normal lipid level than those whose parents were illiterate (Table 4).
 |
Table 4 Multivariable Logistic Regression: Association of Independent Variables with Abnormal Lipid Level for HDL-C and Triglyceride and Non-Dyslipidemia |
Discussion
In the current study the prevalence of dyslipidemia among children and adolescents receiving antiretroviral treatment was 72%. Moreover, this study found that a BMI for age of ≤5% in children and adolescents and treatment duration were associated with abnormally low HDL-C.
The high prevalence of dyslipidemia in this study is consistent with the finding of other research conducted so far in South Africa (75%) and Uganda (74%).7,22 The consistency might be due to the fact that HAART commonly causes dyslipidemia, similarity in participants’ standard of living; similarity in the age group of participants; and similarity in the nature of the studies.
In this study, it was found that the children and adolescents receiving HAART had abnormal HDL-C as the most frequent abnormality (72%), followed by hypertriglyceridemia (21.3%); however, abnormalities in total cholesterol and LDL-C were not seen. This was not consistent with the study conducted in India, in which hypertriglyceridemia (22.2%) was reported as the most frequent abnormality, followed by abnormal HDL-C (3.7%).19 Hypertriglyceridemia was the most frequent (43.8%) abnormality followed by low HDL-cholesterol (38.8%) as reported in a cross-sectional study conducted in Bangkok.23 Around the globe, the prevalence of dyslipidemia among HIV-infected children receiving antiretroviral (ARV) therapy differs. The reasons for the high prevalence of dyslipidemia in the current study might be due to genetic differences.
The most common lipid abnormality in the current study was low HDL-C (72%). Comparing our results with others in the field, we found that our 72% low HDL-C rate was higher than those in South Africa (57%, 13%7,24) and Uganda (31.5%25). The difference might be due to genetic differences, and long treatment duration in the case of the current study. In the current study, a high prevalence of dyslipidemia was found in those taking TDF+3TC+ATV/r and TDF+3TC+DTG; this is consistent with research conducted in Brazil, El Salvador, and Latin American cohort studies.16,26,27
On assessing the risk factors for dyslipidemia, some studies did not find a significant relationship between low HDL-C and PI-based regimen, age, sex, WHO HIV clinical stage, and total duration of HAART,25 which is similar to the current study. But in the present study, a statistically significant association was observed between >150 months on a HAART regimen and abnormal triglyceride (AOR: 1.02, CI: 1.00–1.036, p=0.01).
In a study conducted in Tamil Nadu, India, total duration of ART was significantly associated with dyslipidemia (P=0.01).28 This is supported by the data of current study, in which treatment duration of >150 months was statistically significant among those who had TG of ≥150mg/dL (AOR: 1.02, CI:1.00–1.036, P=0.01).
In a pre-pubertal cohort of children in Durban, South Africa,18 it was found that the prevalence of stunting was 54% (95% CI: 46–62) and of being underweight was 37% (95% CI: 29–45). Their finding of stunting is in line with the 54% of stunting 30% of being underweight in the current study. This consistency might be due to equal sample size and identical treatment regimen used in both studies.
A report from a cohort of HIV-infected Latin Americans showed that the type of ART regimen received was associated with the risk of developing an abnormal triglyceride level. This is not in agreement specifically with triglyceride in the current study. The difference in nature of the study, in their case the majority of study participants were less than ten years old and the cut-off value for triglyceride of <10 years was <110 mg/dL, would explain the difference.29
A report from 15 sites in Brazil, Mexico, and Argentina indicated that children who were underweight had a significant risk of having higher triglyceride levels than children with a normal BMI (AOR: 2.1, 95% CI: 1.1–4.2).27 It is in line with the current study (AOR: 1.86, 95% CI: 1.03–3.37, P=0.04). Using the same method for defining dyslipidemia would be the reason for similarity in results.
This study did not find a significant association between lipid profile parameters and sex of participants, in contrast to a report from El Salvador in which boys were nearly twice more likely to have low HDL-C than girls (P=0.025). But, there is almost complete consistency in BMI for age of ≤5% being directly associated with high TG (our study = AOR: 1.86, 95% CI: 1.03–3.37, P=0.04; El Salvadoran study = AOR: 1.22, 95% CI: 1.04−1.45). In addition, HDL-C <35 mg/dl was also associated with BMI for age of ≤5% (AOR: 2.2, 95% CI: 1.14–3.66, P=0.015) in the current study.25
Most of the pediatric studies established an association between dyslipidemia and a PI-containing HAART regimen.27,30 Longitudinal analysis showed that an association between hypertriglyceridemia and PI-containing HAART regimen (p <0.001); BMI (p=0.10) and country of residence (p=0.02);30 and hypertriglyceridemia and low body mass index. In the current study, hypertriglyceridemia was also associated with BMI for age ≤5%. Unlike their study, the present study was single center research.30
According to a cross-sectional study conducted in Jakarta, Indonesia, involving 96 children younger than 17 years, most of the participants fell in the well-nourished category, and none were severely malnourished. Dyslipidemia was observed in 20% of malnourished subjects in their study.31 This finding is similar to the current study’s finding: BMI for age of ≤5% accounted for 23% of participants with dyslipidemia.
Another study that supports the present study was conducted in Abuja, Nigeria.32 Their study revealed that risk factors for dyslipidemia include BMI risk factor for total cholesterol, and BMI risk factor for high density lipoprotein cholesterol. In their case, BMI was a risk factor for total cholesterol, but in our case this is not true. It is possible that the difference could be explained by the fact that total cholesterol was reported only as normal in the present investigation.
In children and adolescents, HIV infection has decreased with HAART; at the same time, they suffer from dyslipidemia that is associated with the treatment and virus. The dyslipidemia results from treatment associated with drug regimens, nutritional status, and other risk factors as described by other research.
Conclusion
In the present study, high prevalence of dyslipidemia (72%) was found in children and adolescents on follow-up at Jimma Medical Center. Over half of study subjects were of short stature, almost a half were underweight, and a few had BMI for age of <5%. Treatment duration of >150 months, BMI for age of <5%, and parents’ educational level were significantly associated with dyslipidemia, so it is recommended that monitoring of those variables will help to reduce dyslipidemia and its complications in children and adolescents receiving treatment.
Abbreviations
3TC, Lamivudine; ABC, Abacavir; AIDS, Acquired immunodeficiency syndrome; ART, Antiretroviral treatment; BMI AZ, Body mass index for age z-score; CD4+, Cluster of differentiation four; d4T, Stavudine; HAART, Highly active antiretroviral treatment; HAZ, Height for age z-score; HDL-C, High density lipoprotein; HIV, Human Immunodeficiency virus; JMC, Jimma (University) Medical Center; LDL-C, Low density lipoprotein cholesterol; LPV, Lopinavir; NRT, Nucleoside reverse transcriptase inhibitors; NVP, Nevirapine; PI, Protease inhibitor; TC, Total cholesterol; TDF, Tenofovir disoproxil fumarate; TG, Triglyceride; WAZ, Weight for age z-score; WHO, World Health Organization; ZDV, Zidovudine.
Data Sharing Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request (in SPSS code).
Ethics Approval and Consent to Participate
This research was approved by the ethical review board of the Institute of Health, Jimma University on 27/05/2022, with an ethical clearance letter, protocol number IHRPGD/839. An official permission letter to conduct the study was obtained from Jimma University Medical Center administration office. The research has complied with the Declaration of Helsinki in obtaining written informed assent from each study subject over 8 years of age, and written informed consent was provided by parents or guardians after clear explanation of the study.
Acknowledgments
The authors acknowledge the parents/guardians and study personnel participating in this study. Also, we would like to thank Jimma University Institute of Health, staff of JMC clinical chemistry unit, and nursing staff in the comprehensive chronic care and training center of JMC for their valuable contribution in finalizing this research work.
Disclosure
This manuscript was prepared from a thesis entitled, “Antiretroviral treatment induced dyslipidemia versus the nutritional status of HIV-infected children and adolescents on follow-up at comprehensive chronic care and training center of Jimma medical center”, conducted at Jimma, Ethiopia. All of the data, results, and information in this manuscript are taken from the mentioned research. The authors report no conflicts of interest in this work.
References
1. Rodríguez-Galet A, Ventosa-Cubillo J, Bendomo V, et al. High drug resistance levels compromise the control of HIV infection in pediatric and adult populations in Bata, Equatorial Guinea. Viruses. 2023;15(1):1–22.
2. Gratão LHA, Do Nascimento GNL, Pereira RJ. Effects of HAARTin the nutritional status of children and adolescents infected by HIV in Brazil. Cien Saude Colet. 2021;26(4):1345–1354.
3. Taberna DJ, Navas-Carretero S, Martinez JA. Current nutritional status assessment tools for metabolic care and clinical nutrition. Curr Opin Clin Nutr Metab Care. 2019;22(5):323–328.
4. Dos Reis LC, De Carvalho Rondó PH, De Sousa Marques HH, et al. Anthropometry and body composition of vertically HIV-infected children and adolescents under therapy with and without protease inhibitors. Public Health Nutr. 2015;18(7):1255–1261.
5. Bhatti AB, Usman M, Kandi V. Current Scenario of HIV/AIDS, treatment options, and major challenges with compliance to antiretroviral therapy. Cureus. 2016;8(3):1–12.
6. Ergin HE, Inga EE, Maung TZ, Javed M, Khan S. HIV, antiretroviral therapy and metabolic alterations: a review. Cureus. 2020;12(5). doi:10.7759/cureus.8059
7. Viljoen E, MacDougall C, Mathibe M, Veldman F, Mda S. Dyslipidaemia among HIV-infected children on antiretroviral therapy in Garankuwa, Pretoria. South African J Clin Nutr. 2020;33(3):86–93.
8. Patel K, Lindsey J, Angelidou K, Aldrovandi G, Palumbo P. Metabolic effects of initiating lopinavir/ ritonavir-based regimens among young children. AIDS. 2018;32(16):2327–2336.
9. Da Salveira AE, De Oliveira Falco M. Nutritional treatment approach for children with HIV receiving ART. In: Health of HIV Infected People. Elsevier Inc.; 2015:291–306. doi:10.1016/B978-0-12-800769-3.00017-2
10. Rhoads MP, Smith CJ, Tudor-Williams G, et al. Effects of highly active antiretroviral therapy on paediatric metabolite levels. HIV Med. 2006;7(1):16–24. doi:10.1111/j.1468-1293.2005.00337.x
11. Pires A, Sena C, Seiça R. Dyslipidemia and cardiovascular changes in children. Curr Opin Cardiol. 2016;31(1):95–100. doi:10.1097/HCO.0000000000000249
12. World Health Organization. Nutrition; 2022. Available from: https://www.who.int/health-topics/nutrition#tab=tab_1.
13. Muenchhoff M, Healy M, Singh R, et al. Malnutrition in HIV-infected children is an indicator of severe disease with an impaired response to antiretroviral therapy. AIDS Res Hum Retroviruses. 2018;34(1):46–55. doi:10.1089/aid.2016.0261
14. Kimani-Murage EW, Norris SA, Pettifor JM, et al. Nutritional status and HIV in rural South African children. BMC Pediatr. 2011;11(1):23.
15. Penda CI, Moukoko ECE, Nolla NP, Evindi NOA, Ndombo PK. Malnutrition among HIV infected children under 5 years of age at the laquintinie hospital Douala, Cameroon. Pan Afr Med J. 2018;30:1–7.
16. Berchielli M, Tremeschin IMH, De Moura IBV, et al. Nutritional status and lipid profile of HIV-positive children and adolescents using antiretroviral therapy. Clinics. 2011;66(6):997–1002.
17. Solórzano Santos F, Gochicoa Rangel LG, Palacios Saucedo G, Vázquez Rosales G, Miranda Novales MG. Hypertriglyceridemia and hypercholesterolemia in human immunodeficiency virus-1-infected children treated with protease inhibitors. Arch Med Res. 2006;37(1):129–132.
18. Chhagan MK, Kauchali S, Van den Broeck J. Clinical and contextual determinants of anthropometric failure at baseline and longitudinal improvements after starting antiretroviral treatment among South African children. Trop Med Int Heal. 2012;17(9):1092–1099.
19. Mandal A, Mukherjee A, Lakshmy R, Kabra SK, Lodha R. Dyslipidemia in HIV infected children receiving highly active antiretroviral therapy. Indian J Pediatr. 2016;83(3):226–231.
20. Kuczmarski RJ. CDC growth charts for the United States: methods and development national center for health statistics. Vital Health Stat. 2000;11(246):1–90.
21. Kavey RW, Daniels SR, Lauer RM, Atkins DL, Hayman LL, Taubert K. American Heart Association guidelines for primary prevention of atherosclerotic cardiovascular disease beginning in childhood. Circulation. 2003;107(11):1562–1566.
22. Nampijja D, Kumbakumba E, Francis Bajunirwe JK. Dyslipidemia and its correlates among HIV infected children on HAART attending Mbarara regional referral hospital. Int Clin Pathol J. 2017;176(5):139–148.
23. Santiprabhob J, Tanchaweng S, Maturapat S, et al. Metabolic disorders in HIV-infected adolescents receiving protease inhibitors. Hindawi BioMed Res. 2017;2017:1–14.
24. Innes S, Abdullah KL, Haubrich R, Cotton MF, Browne SH. High prevalence of dyslipidemia and insulin resistance in HIV-infected prepubertal African children on antiretroviral therapy. Pediatr Infect Dis J. 2016;35(1):1–19.
25. Nampijja D, Kumbakumba E, Francis Bajunirwe JK. Dyslipidemia and its correlates among HIV infected children on HAART attending Mbarara regional referral hospital Dorah. Physiol Behav. 2017;176(5):139–148.
26. Brewinski M, Megazzini K, Freimanis Hance L, et al. Dyslipidemia in a cohort of HIV-infected Latin American children receiving highly active antiretroviral therapy. J Trop Pediatr. 2011;57(5):324–332.
27. Sonego M, Sagrado MJJ, Escobar G, et al. Dyslipidemia, diet and physical exercise in children on treatment with antiretroviral medication in El Salvador: a cross-sectional study. Pediatr Infect Dis J. 2016;35(10):1111–1116.
28. Kalyanasundaram AP, Jacob SM, Hemalatha R, Sivakumar MR. Prevalence of lipodystrophy and dyslipidemia among patients with HIV infection on generic ART in rural South India. J Int Assoc Physicians AIDS Care. 2012;11(5):329–334.
29. Diering M, Mitchell F. Association of dyslipidemia and glucose abnormalities with antiretroviral treatment in a cohort of HIV-infected Latin American Children. Physiol Behav. 2018;176(1):139–148.
30. Carter RJ, Wiener J, Abrams EJ, Farley J, Nesheim S, Paul Palumbo MB. Dyslipidemia among perinatally HIV-infected children enrolled in the PACTS-HOPE Cohort, 1999Y2004: a longitudinal analysis. J Acquir Immune Defic Syndr. 2006;41(4):453–460.
31. Wicaksana P, Kurniati N, Pardede S. Dyslipidemia among HIV-positive children receiving antiretroviral therapy in Indonesia. HIV AIDS Rev. 2021;20(1):47–51.
32. Okechukwu A, Lawson J, Dalilo M. Dyslipidemia in HIV infected children and adolescents on highly active antiretroviral therapy in Abuja, Nigeria. J Adv Med Med Res. 2017;24(3):1–11.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
