Back to Journals » Integrated Blood Pressure Control » Volume 16
Drug Therapy Problems and Associated Factors Among Hypertensive Patients in North Wollo Public Hospitals, Northeast Ethiopia: Institutional-Based Cross-Sectional Study
Authors Baye T , Girmaw F , Ashagrie G , Kassaw AT
Received 10 April 2023
Accepted for publication 14 July 2023
Published 20 July 2023 Volume 2023:16 Pages 47—57
DOI https://doi.org/10.2147/IBPC.S416585
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Tenaw Baye, Fentaw Girmaw, Getachew Ashagrie, Abebe Tarekegn Kassaw
Department of Pharmacy, College of Health Science, Woldia University, Woldia, Ethiopia
Correspondence: Tenaw Baye, Email [email protected]
Background: Drug therapy problems (DTPs) are common in people with hypertension and may threaten the effective management of the disease. The purpose of this study was to determine the prevalence and predictors for DTPs in hypertensive people in North Wollo public hospitals.
Methods: On patients with hypertension, a cross-sectional study based in a health institution was carried out using an interviewer-administered structured questionnaire and medical record review from 6 November 2022 to 18 January 2023. All hypertensive patients, ages 18 and older, who underwent regular follow-ups for at least 12 months were included in the study using a simple random sampling method. Multivariate logistic regression analysis was used to establish the association between independent variables and the occurrence of DTPs. Unnecessary drug therapy, the need for additional drug therapy, ineffective drugs, dosage too low, dosage too high, adverse drug reactions, and noncompliance were the outcome variables.
Results: The study included 376 hypertensive patients. Of the total participants, 258 (68.6%) were female. The mean number of drug therapy problems per patient was 1.55 ± 0.307, with 298 participants (79.3%) reporting having at least one such problem. This study found that the need for additional drug therapy was the most prevalent problem (149, 39.66%). Polypharmacy (AOR = 2.487, 95% CI = 1.375– 4.499, p = 0.003), presence of comorbidity (AOR = 1.886, 95% CI = 1.035– 3.439, p = 0.038), and uncontrolled BP (AOR = 2.961, 95% CI = 1.669– 5.254, p = < 0.001) predicts the development of drug therapy problems.
Conclusion: Patients with hypertension who are on follow-up experience drug therapy problems frequently. Promoting the involvement of clinical pharmacists in designing, implementing, and monitoring therapeutic plans is recommended to decrease the occurrence of drug therapy problems.
Keywords: drug therapy problems, hypertension, hypertensive, public hospitals, Ethiopia
Introduction
Hypertension is referred to as a persistent elevation of arterial blood pressure (BP) of ≥140/90 mmHg.1 It is a chronic condition that is typically detected in individuals 50 years of age and older.2 It has been estimated that 7.1 million deaths each year are caused by HTN, or 13% of all fatalities worldwide.3 Growing sedentary lifestyles and lifestyle changes are reasons for the rise in morbidity and mortality in developing nations.4,5 Around 80% of this burden was experienced in low- and middle-income nations.5,6 In some economically developing nations, there is a very low degree of awareness, treatment, and control of HTN. Although there is a lack of comprehensive statistics, it has been estimated that 10.5% of Ethiopians have HTN.5,7
Several medications have been shown to treat HTN and the risk of associated serious cardiovascular problems. Drug therapy problems (DTPs) are common in HTN patients and may cause a serious risk for this group of patients. DTPs are classified into the following categories: unnecessary drug therapy, the need for additional drug therapy, ineffective drugs, dosage too low, dosage too high, adverse drug reactions, and noncompliance.8 These issues may have a significant impact on patients’ quality of life and lead to prolonged hospitalisation and raise overall healthcare costs.9
In pharmaceutical care, assessing DTPs is a crucial topic that can help address the consequences of improper drug therapy.2 The goal of identifying DTPs is to assist patients in achieving their therapeutic goals and the best outcomes from medication therapy. Patients with hypertension are among those who experience undesirable drug therapy side effects.8 Despite the presence of previous studies on this topic,10–13 they were conducted in single-study settings which can affect the generalizability of the study’s findings. In the interest of addressing this research gap, this investigation examined the prevalence and risk factors for drug therapy problems (DTPs) among hypertensive patients in public hospitals in North Wollo, northeastern Ethiopia.
Materials and Methods
Study Setting and Participants
A health facility-based cross-sectional study design was employed in 376 patients with HTN in public hospitals of North Wollo from 6 November 2022 to 18 January 2023 G.C. North Wollo zone is found in Amhara regional state with Woldia as the central town. There are 6 public hospitals (1 general and 5 primary hospitals) in North Wollo. The study included all HTN patients, ages 18 and older, who underwent regular follow-up at ambulatory clinics of study hospitals for at least 12 months and whose medical records contained complete data. Individuals with hearing impairments and mental instability were excluded from the study.
Sample Size Determination
The minimum sample size required was determined using a single proportion formula. The estimated proportion of 55.6%,12 with a 5% margin of error (d) and 95% (zα/2 = 1.96) level of confidence, was considered. During the time that data was being collected, 2422 HTN patients had registered at the ambulatory clinics of North Wollo public hospitals.
Where: n = sample size
Z = statistic for 95% level of confidence
d = margin of error and
p = the estimated proportion of DTPs in hypertensive patients.
While the total number of hypertensive patients who were attending ambulatory clinics of public hospitals of north Wollo was 2422 during the data collection period, the correction formula was applied and the sample size would be:
where: nf = final sample size
ni = sample size for more than 10,000 population, and
N = population size.
Adding 15% for non-response, the final sample size was estimated to be 376.
Sampling Procedure
Three public hospitals, Woldia Comprehensive Specialized Hospital, Kobo Hospital, and Mersa Hospital, were selected randomly from six hospitals. By using simple random sampling, study participants were selected proportionate to the total number of hypertensive patients being treated in each study hospital until the desired sample size was reached.
Ethical Considerations
The ethical review committee of the College of Health Sciences, Woldia University offered approval for this study. The North Wollo zone health office and the hospital administrations were addressed in a formal letter of cooperation. Verbal informed consent accepted and approved by the Ethical Review Committee was obtained from all participants after delivering information about the purpose, risks, and benefits of the study. This study was conducted following the Declaration of Helsinki.
Data Collection Tool and Procedure
We created a structured questionnaire and a tool for data extraction. The socio-demographic characteristics questionnaire was initially prepared in English then translated into Amharic, the nation’s working language, and then back into English by an independent person to ensure translation accuracy. The socio-demographic data were collected through a face-to-face interview using a standardized Amharic version questionnaire that had been evaluated before. To avoid any potential misunderstandings, questions for clinical and medication-related data were collected by English version questionnaire from patient medical records. Under the supervision of the principal investigator, three nurse professionals working in the ambulatory clinics of each study hospital collected the data. DTPs were identified using the Joint National Committee (JNC-8) as a guide. Then, they were categorized using the Cipolle technique of DTP categorization. DTPs fall into four fundamental groups. They are adherence, indication, effectiveness, and safety.8 DTPs and their causes were identified using patient medical records and interviews.
Data Quality Control
To maintain the quality of the data a structured tool was used. A pretest was done on 5% of the samples (19 hypertensive patients) in a separate hospital, Wadila Hospital, and adjustments were made to the questionnaire before the data collection. One-day training about the purpose of the study, the data collection method, the contents of the data collection instrument, and how to identify participants based on eligibility criteria. Data collectors helped the study participants in the event of difficulties clearly understanding the questionnaire. The principal investigator checked the completeness of the questionnaire during data collection and before the data was entered into the computer. The principal investigator maintained strict control throughout the data collection period. During data management, storage, and analysis, all completed data were reviewed for accuracy and consistency.
Data Processing and Analysis
STATA version 17 was used to analyze the data. To summarize the study’s variables and assess the distribution of responses, descriptive statistics, such as frequency, percent, mean, and standard deviation (SD), were employed. For categorical data, percentages were used, and median, mean, and standard deviation were used for continuous data. We performed bivariate and multivariate logistic regression analyses to identify the variables associated with the incidence of DTPs.
Socio-demographic and clinical factors that have previously been linked to the development of DTPs were included in the bivariate logistic regression. We carried out a multivariate logistic regression for variables (p-value <0.25) in the first analysis, polypharmacy, co-morbidity, and uncontrolled BP to control confounding factors. To evaluate the association between independent variables and the occurrence of DTPs, the adjusted odds ratio (AOR) with 95% confidence intervals (CI) was calculated. What is considered statistically significant is p < 0.05.
Study Variables
Dependent Variable
Presence of DTPs (yes/no).
Independent Variable
Socio-demographic variables include age, gender, marital status, place of residence, level of education, occupational status; clinical and medication-related variables like number of medications prescribed, status of BP, and presence of co-morbidities.
Operational Definitions
Drug therapy problems (DTPs) – Unwanted incidents or problems that the patient encounters that are related to or are considered to be related to medication therapy, that prevent or delay him or her from attaining the intended therapeutic goals, and that need the professional’s judgment to manage.8
Hypertensive patient – a patient found to have high BP and currently using anti-hypertensive medication.14
Polypharmacy: means taking three or more medications per day.
Comorbidity: is defined as being diagnosed with one more disease in addition to hypertension.
Uncontrolled BP: If BP >140/90 mmHg, despite being on therapy for at least a given duration.
Results
Socio-Demographic Characteristics of Patients
A total of 376 hypertensive patients participated in the study. The majority of the participants, 258 (68.6%) were females, and 54.9% of the total participants were over 60 years old, with a median age of 61.03 years. Two hundred eleven (56.1%) participants were married, 158 (42%) had attended primary school, and 91 (24.2%) were unemployed. In terms of clinical characteristics, the majority of study participants (n = 263; 70.0%) had uncontrolled blood pressure; 263 (70.0%) had multiple comorbidities, and 197 (52.3%) were prescribed three or more antihypertensive drugs (Table 1).
 |
Table 1 Socio-Demographic and Clinical Characteristics of Hypertensive Patients, North Wollo Zone Public Hospitals, Northeast Ethiopia, January 2023 [n = 376] |
Medications Use
With a range of 1 to 3, the average number of hypertensive drugs per patient was 1.29 0.39. The antihypertensive drug that was most frequently prescribed was enalapril (161, 33.1%). Most participants on follow-up, 278 (73.9%), were on monotherapy. Enalapril with hydrochlorothiazide was the most frequently prescribed dual antihypertensive medication. Enalapril, hydrochlorothiazide, and furosemide were the only medications administered as part of a triple treatment (Table 2). The concurrent drugs that were frequently prescribed were anti-diabetics, 124 (33%), non-steroidal anti-inflammatory drugs (NSAIDs), 80 (21.4%), proton-pump inhibitors, 40 (10.7%), antibiotics, 17 (4.5%), others 57 (15.2%), and the rest were using only anti-hypertensive medications.
 |
Table 2 Most Frequently Prescribed Medications for HTN Treatment, North Wollo Zone Public Hospitals, Northeast Ethiopia, January 2023 [n = 376] |
Drug Therapy Problems and Associated Factors
A total of 582 DTPs were found in 298 participants (79.3%), with a mean of 1.55 ± 0.307. The need for additional drug therapy was the most commonly identified DTP, which were 149 (39.66%) [90 needed preventive drug therapy, and 59 needed synergistic drug effect], followed by noncompliance 111 (29.54%) [87 were due to forgetting to take medications and 24 were preferring not to take the medication] and drug interactions 97 (25.74%) [Enalapril and oral hypoglycemia were most frequently administered together in 42 patients, followed by Enalapril with Aspirin in 23 participants] (Figure 1).
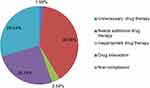 |
Figure 1 The most commonly identified types of drug therapy problems [n = 376]. |
Bivariate logistic regression revealed that co-morbidity, uncontrolled BP, and polypharmacy were strongly associated with the incidence of DTPs. Among 263 patients with co-morbidity, 227 (86.3%) were found to have at least one DTPs. According to the analytic model, study participants with comorbid diseases were 3.7 times more likely to experience DTPs than those without co-morbidity (COR = 3.730, 95% CI = 2.220–6.267, p = <0.001). Regarding the status of BP control, out of 263 participants with uncontrolled BP, 229 (87.1%) were found to have at least one DTPs. Thus, study participants who had uncontrolled BP were 4.3 times more likely to have DTPs compared with those who had controlled BP (COR = 4.295, 95% CI = 2.548–7.240, p = <0.001). Additionally, the occurrence of DTPs was associated with the number of medications taken per day. According to the findings of the study, 175 (88.8%) of the 197 participants who were taking three or more drugs per day had at least one DTPs. Thus, participants taking three or more drugs per day were 3.6 times more at risk of developing DTPs compared with participants taking less than three drugs (COR = 3.622, 95% CI = 2.101–6.242, p = <0.001) (Table 3).
To determine the variables associated with the occurrence of DTPs, multivariate logistic regression was used for variables with a p-value of <0.25 in the bivariate logistic analysis. Three variables (comorbidity, polypharmacy, and uncontrolled BP) were found to be significantly associated with the presence of DTPs in the bivariate logistic regression. Similarly, the multivariate logistic regression revealed that polypharmacy (AOR = 2.487, 95% CI = 1.375–4.499, p = 0.003), comorbidity (AOR = 1.886, 95% CI = 1.035–3.439, p = 0.038), and uncontrolled BP (AOR = 2.961, 95% CI = 1.669–5.254, p = <0.001) were significantly associated with the occurrence of DTPs (Table 4).
Discussion
The prevalence of DTPs and associated variables among HTN patients were evaluated in this study. The study’s findings indicated that 79.3% of participants had DTPs. This was lower than the study results obtained at Gebretsadik Shawo General Hospital, 84.4%,11 and Malaysia, 90.5%.15 However, it was higher than other study results reported from Dil-Chora Referral Hospital, 71.2%,10 Ayder comprehensive specialized hospital, 55.6%,12 Uganda, 61.8%,16 and Indonesia, 57%.17 The different rates of prevalence could be caused by variations in the study period, the number of professionals participating in DTP identification, and the size of the study population. Clinical pharmacists are essential in the detection of DTPs because of their education and sufficient pharmacotherapeutic understanding. Therefore, the hospital’s responsible authority should establish a setting that is favorable for the delivery of pharmaceutical care services.
The average number of DTPs per patient was 1.55 ± 0.307, which is lower than the study report in Jimma University Specialized Hospital, which was 3.13 However, it was higher than the results of the study in Gebretsadik Shawo General Hospital, 1.3,11 Ayder comprehensive specialized hospital, 1.48 ± 0.597,12 and Felege Hiwot Referral Hospital, 1.4.18 Such discrepancies could be due to the difference in the number of medications used in the studies.
The most common type of DTP identified was the need for additional drug therapy, which accounted for 39.66% of all cases. It was also common in the study conducted in Gebretsadik Shawo General Hospital (84.4%),11 Jimma University Specialized Hospital (84.0%),13 and Felege Hiwot Referral Hospital (90.69%).18 Comorbidity and the absence of specific and comprehensive disease management guidelines could be possible reasons. However, this was not in line with the study result done in Ayder Comprehensive Specialized Hospital, which found a need for additional drug therapy prevalence of 17.1%.12 The level of clinical pharmacist involvement in patient care and the experience and training of health professionals may be the causes of this variation. This study’s findings indicate that the “need for additional drug” can happen in the case of a diagnosis without an indication, as well as in the case of additive drug or preventative drug needs. Therefore, promoting the involvement of trained clinical pharmacists in designing, implementing, and monitoring therapeutic plans is recommended.
In this study, the second most common DTP (29.54%) was non-compliance with antihypertensive medications, which was lower than the results of studies done in Dil-Chora Referral Hospital, which was 32.8%.10 However, this was higher than the findings of studies conducted at Adama Hospital Medical College (19.5%),19 Uganda (19.1%),16 and Indonesia (13.6%).20 The difference in the prevalence of non-compliance with medications might be due to the presence of co-morbid conditions, polypharmacy, accessibility to health facilities, and differences in knowledge between people. Further, unaffordability and unavailability of prescribed drugs could be possible reasons. In agreement with other studies findings done in Dil-Chora Referral Hospital,10 Gebretsadik Shawo General Hospital,11 and Takoradi, Ghana,21 the major reason for non-compliance with medications was forgetting to take the medications at the right time. About 30–50% of antihypertensive drug non-adherence is common and is associated with uncontrolled BP.22 This suggests that healthcare providers should increase their adherence counseling efforts to raise knowledge and make people aware of BP control.
In more than half of the research participants, comorbidity was reported. The findings of this study demonstrated a substantial correlation between the occurrence of DTPs and the existence of comorbidities. According to the regression analysis, study participants who had more than one disease were 1.9 times more likely to experience DTPs than those who did not have any comorbid conditions. This may be because people who suffer from multiple medical conditions are more prone to experience polypharmacy, which could result in the patient taking more medicines. Due to the possible increased risk of adverse pharmacological effects, the patient may be forced to discontinue taking the recommended prescriptions. DTP development may be influenced by these and other factors. This finding was consistent with other study results.10,19,23,24
This study found that participants who were using three or more drugs per day had a higher risk of developing DTPs, which was in line with the results of other studies.10,19,23 The possibility of drug interactions that could change the appropriate dose range and its intended effects, as well as other important factors, could be possible reasons. They include intolerance to the additive adverse effects of taking medications at the same time. Medication reconciliation and a thorough evaluation of the patient’s medical history can dramatically minimize DTPs related to multiple comorbidities and polypharmacy.
This study result revealed that 229 (87.1%) participants reported having uncontrolled BP. As a result, people with uncontrolled BP were 2.9 times more likely to develop DTPs than participants with managed BP. That might be related to how patients behave when it comes to adherence. It is more likely that people with poor medication compliance will not be able to control their BP. Poor medication adherence can have an impact on the clinical results of HTN treatment; hence, 29.5% of identified DTPs had noncompliance (no adherence) with the recommended medications. According to the findings of other studies, there is a significant correlation between medication adherence levels and the control of BP.10,25 Hence, continuous monitoring of hypertensive patients is crucial for identifying any probable causes that could contribute to poor BP control while taking appropriate medication to lower the risk of developing cardiovascular problems and prevent the occurrence of DTPs caused by poor BP control.
Study Strengths and Limitation
The inclusion of a multi-center that might better represent the target populations (hypertensive patients in North Wollo) was the study’s strength. In addition, standardised DTP identifying criteria were employed in the study.
There were certain limitations to be aware of as well. Neither the impact of DTPs on the outcome of HTN nor interventions for identified DTPs were addressed.
Conclusion
The study shows a high prevalence (79.3%) of DTPs among hypertensive patients in public hospitals of north Wollo. The need for additional drugs and noncompliance were the most frequently reported DTPs. The occurrence of DTPs was significantly associated with the presence of comorbidities, polypharmacy, and uncontrolled BP. It is imperative to design and implement interventions aimed at reducing DTPs among hypertensive patients. One possible solution is to promote the involvement of trained clinical pharmacists in designing, implementing, and monitoring therapeutic plans.
Abbreviations
AOR, Adjusted Odd Ratio; BP, Blood pressure; CI, Confidence Interval; COR, Crude Odd Ratio; DTPs, Drug therapy problems; HTN, Hypertension; OR, Odds Ratio.
Data Sharing Statement
The datasets used for analysis during the current study are available from the corresponding author upon reasonable request.
Ethical Approval and Consent to Participate
Ethical approval for this study was obtained from the ethical review committee of the College of Health Sciences, Woldia University. An official letter of cooperation was written to the North Wollo zone health office and the hospital administrations. Verbal informed consent accepted and approved by the Ethical Review Committee was obtained from all participants after delivering information about the purpose, risks, and benefits of the study. This study was conducted following the Declaration of Helsinki.
Acknowledgments
We would like to thank the study subjects and data collectors. We also like to thank Woldia University for letting us carry out the study. Our sincere gratitude also extends to the personnel at the sample hospitals who assisted us in collecting data.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed on the journal to which the article will be submitted; gave final approval of the version to be published; and agreed to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
1. Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Clin Hypertens. 2014;16(1):14. doi:10.1111/jch.12237
2. Dymek J, Pelka P, Polak W, Golda A, Skowron A. Drug related problems among ambulatory patients diagnosed with arterial hypertension. Int J Clin Pharm. 2016;38:1021.
3. Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16(4):223–237. doi:10.1038/s41581-019-0244-2
4. Chiazor IE, Oparah AC. Assessment of hypertension care in a Nigerian Hospital. Trop J Pharm Res. 2012;11(1):137–145. doi:10.4314/tjpr.v11i1.18
5. Lawes CM, Vander Hoorn S, Rodgers A. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371(9623):1513–1518. doi:10.1016/S0140-6736(08)60655-8
6. Lalić J, Radovanović RV, Mitić B, Nikolić V, Spasić A, Koraćević G. Medication adherence in outpatients with arterial hypertension. Acta Fac Medicae Naissensis. 2013;30(4):209–218. doi:10.2478/afmnai-2013-0013
7. Opie LH, Seedat YK. Hypertension in sub-Saharan African populations. Circulation. 2005;112(23):3562–3568. doi:10.1161/CIRCULATIONAHA.105.539569
8. Cipolle RJ, Strand LM, Morley PC. Pharmaceutical Care Practice: The Patient-Centered Approach to Medication Management. McGraw Hill Professional; 2012.
9. AbuRuz SM, Bulatova NR, Yousef A-M-M, Al-Ghazawi MA, Alawwa IA, Al-Saleh A. Comprehensive assessment of treatment related problems in hospitalized medicine patients in Jordan. Int J Clin Pharm. 2011;33(3):501–511. doi:10.1007/s11096-011-9497-y
10. Hussen A, Daba FB. Drug therapy problems and their predictors among hypertensive patients on follow up in Dil-Chora Referral Hospital, Dire-Dawa, Ethiopia. hypertension. 2017;5(7):2712–2719.
11. Gizaw K, Dubale M. Drug related problems and contributing factors among adult ambulatory patients with cardiovascular diseases at Gebretsadik Shawo General Hospital, Bonga, South west Ethiopia. J Natural Sci Res. 2017;7(1):9–16.
12. Weldegebreal AS, Tezeta F, Mehari AT, Gashaw W, Dessale KT, Legesse NY. Assessment of drug therapy problem and associated factors among adult hypertensive patients at Ayder comprehensive specialized hospital, Northern Ethiopia. Afr Health Sci. 2019;19(3):2571–2579. doi:10.4314/ahs.v19i3.33
13. Tigabu BM, Daba D, Habte B. Drug-related problems among medical ward patients in Jimma university specialized hospital, Southwest Ethiopia. J Res Pharm Pract. 2014;3(1):1. doi:10.4103/2279-042X.132702
14. Lampert ML, Kraehenbuehl S, Hug BL. Drug-related problems: evaluation of a classification system in the daily practice of a Swiss University Hospital. Pharm World Sci. 2008;30(6):768–776. doi:10.1007/s11096-008-9213-8
15. Zaman Huri H, Fun Wee H. Drug related problems in type 2 diabetes patients with hypertension: a cross-sectional retrospective study. BMC Endocr Disord. 2013;13(1):1–12. doi:10.1186/1472-6823-13-2
16. Babirye M, Yadesa TM, Tamukong R, Obwoya PS. Prevalence and factors associated with drug therapy problems among hypertensive patients at hypertension clinic of Mbarara Regional Referral Hospital, Uganda: a| cross-sectional study. Ther Adv Cardiovasc Dis. 2023;17:17539447231160319. doi:10.1177/17539447231160319
17. Kusumawardani LA, Andrajati R, Nusaibah A. Drug-related problems in hypertensive patients: a cross-sectional study from Indonesia. J Res Pharm Pract. 2020;9(3):140. doi:10.4103/jrpp.JRPP_20_16
18. Tegegne GT, Gelaw BK, Defersha AD, Yimam B, Yesuf E. Drug therapy problem among patients with cardiovascular diseases in Felege Hiwot referral Hospital, Northeast, Bahir Dar Ethiopia. IAJPR. 2014;4:2828–2838.
19. Hussein M, Lenjisa J, Woldu M, Tegegne G, Umeta G, Dins H. Assessment of drug related problems among hypertensive patients on follow up in Adama Hospital Medical College, East Ethiopia. Clinic Pharmacol Biopharmaceut. 2014;3(122):2. doi:10.4172/2167-065X.1000122
20. Wicaksono TA, Nugraheni A, Wahyudi F, Ardhianto P. Factors associated with medication adherence in hypertension in the Ngluwar Public Health Center in Magelang Regency. Diponegoro Med J. 2021;10(6):426–432.
21. Shittu RO, Musa SA, Louis OO, Sule AG, Aremu IB, Isiaka-Lawal S. Adherence to anti-hypertensive medications and associated factors among patients in a Nigerian family practice setting. Int J Med Res Pharm Sci. 2015;2(5):1–12.
22. Lane D, Lawson A, Burns A, et al. Nonadherence in hypertension: how to develop and implement chemical adherence testing. Hypertension. 2022;79(1):12–23. doi:10.1161/HYPERTENSIONAHA.121.17596
23. Khdour M R, Jarab A S, Adas H O, Samaro E Z, Mukattash T L, Hallak H O. Identification of drug-related problems: a prospective study in two general hospitals. Curr Clin Pharmacol. 2012;7(4):276–281. doi:10.2174/157488412803305795
24. Oliveira-Filho AD, Barreto-Filho JA, Neves SJF, Lyra DPD. Association between the 8-item Morisky Medication Adherence Scale (MMAS-8) and blood pressure control. Arq Bras Cardiol. 2012;99(1):649–658. doi:10.1590/S0066-782X2012005000053
25. Moharamzad Y, Saadat H, Shahraki BN, et al. Validation of the Persian version of the 8-item Morisky Medication Adherence Scale (MMAS-8) in Iranian hypertensive patients. Glob J Health Sci. 2015;7(4):173. doi:10.5539/gjhs.v7n4p173
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.