Back to Journals » Therapeutics and Clinical Risk Management » Volume 11
Distribution and resistance of pathogens in liver transplant recipients with Acinetobacter baumannii infection
Authors Gao F, Ye Q, Wan Q , Liu S, Zhou J
Received 5 February 2015
Accepted for publication 2 March 2015
Published 26 March 2015 Volume 2015:11 Pages 501—505
DOI https://doi.org/10.2147/TCRM.S82251
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Deyun Wang
Fei Gao, 1 Qifa Ye, 2,3 Qiquan Wan, 2 Shan Liu, 4 Jiandang Zhou 5
1Infectious Disease Department of Henan Province People’s Hospital, Zhengzhou, 2Department of Transplant Surgery, Third Xiangya Hospital, Central South University, Changsha, 3Department of Transplant Surgery, Zhongnan Hospital, Wuhan University, Wuhan, People’s Republic of China; 4Adelphi University College of Nursing and Public Health, New York, NY, USA; 5Department of Clinical Laboratory of Microbiology, Third Xiangya Hospital, Central South University, Changsha, People’s Republic of China
Background: Drug-resistant Acinetobacter baumannii has become a major problem in liver transplant recipients. The aim of this study was to investigate the clinical presentation, distribution, and drug susceptibility characteristics in liver recipients with A. baumannii infection.
Methods: We retrospectively investigated 17 liver recipients who developed A. baumannii infection between January 1, 2007 and December 31, 2014. The distribution of A. baumannii and drug susceptibility characteristics were reviewed.
Results: Infectious complications due to A. baumannii appeared in 17 liver recipients, with a total of 24 episodes. Approximately 63% (15/24) of A. baumannii infections occurred within 2 weeks after transplantation. The most common source of infection was multiple culture-positive sites (35.3%, n=6), followed by the intra-abdominal/biliary tract (23.5%, n=4) and lung (23.5%, n=4). Eight patients (47.1%) had a body temperature of 38°C or higher at the onset of A. baumannii infection. Nine, seven, and 12 recipients had a serum creatinine level of > 1.5 mg/dL, a white blood cell count of > 15,000/mm 3, and a platelet count of < 50,000/mm 3, respectively. There were five (29.4%) cases of septic shock and eight (47.1%) deaths. The rate of antibiotic resistance of A. baumannii to ten of 12 antibiotics investigated was more than 60%. Among the 24 infections caused by A. baumannii, 75% were carbapenem-resistant. The rods were relatively sensitive to tigecycline and cefoperazone-sulbactam.
Conclusion: The clinical manifestations of A. baumannii infection included a high body temperature, a decreased platelet count, an elevated white blood cell count, and onset in the early period after transplantation as well as high mortality. The antibiotic resistance rate of A. baumannii was extremely high. Prevention measures and combination antibiotic therapy are needed to improve the outcomes of liver recipients with A. baumannii infections.
Keywords: liver transplantation, Acinetobacter baumannii, infections, manifestation, drug resistance
Expression of Concern for this paper has been published
Erratum for this paper has been published
Introduction
Infection is still a leading contributor to patient morbidity and mortality in liver transplantation.1–3 Approximately four episodes of bacterial infection during the first post-transplantation month were reported per patient per year in liver recipients.4 A recent study reported that around 60% of liver recipients experienced early infection post-transplantation.5
Acinetobacter baumannii has emerged in recent years as a particularly problematic drug-resistant pathogen and can result in a wide range of infections, including bacteremia, pneumonia, urinary tract infection, and peritonitis. Previous studies demonstrated that 0.8%–15.9% of liver recipients developed A. baumannii bacteremia,6–15 and Nie et al reported that 3.7% of liver recipients developed intra-abdominal infection caused by A. baumannii.16 The overall mortality among liver recipients with Acinetobacter species infections ranged from 50% to 90%.14,15
Knowledge about A. baumannii infections is essential to improve global care for the liver transplant recipient. In this retrospective study, we investigated the clinical presentation, distribution, and drug susceptibility characteristics in liver recipients with A. baumannii infection.
Materials and methods
We reviewed the medical records of 17 liver recipients diagnosed with A. baumannii infection between January 1, 2007 and December 31, 2014 at the Third Xiangya Hospital, Central South University, Changsha and Zhongnan Hospital, Wuhan University, Wuhan, both of which are university teaching hospitals in the People’s Republic of China. We enrolled all patients with definite clinical signs of infection from whom A. baumannii were isolated from clinical samples. All subjects received dual drug immunosuppression comprising corticosteroids and cyclosporine or tacrolimus. Demographic, clinical, and laboratory records for these recipients were retrospectively analyzed. The laboratory variables comprised serum creatinine and albumin levels, and white blood cell, platelet, and lymphocyte counts, which were collected within the first 24 hours after the culture was drawn. The follow-up time of all liver recipients was 1 month after the onset of A. baumannii infection. The ethics committees of the two hospitals involved approved the study.
Definition
A case was defined as a patient with A. baumannii infection according to the criteria established by the Centers for Disease Control and Prevention.17 Nosocomial infection was defined as an infection that was absent during preadmission assessments but detected at least 48 hours after admission to the hospital.18 Antibiotic therapy was considered appropriate if A. baumannii was susceptible in vitro to empiric antibiotics, which were administered within 48 hours of sampling for culture. Septic shock was diagnosed in recipients with A. baumannii infection who developed persistent dysfunction of at least one organ caused by hypoperfusion which was unresponsive to intravenous fluid challenge.19,20 Mortality was defined as infection-related when death was associated with clinical signs of active A. baumannii infection without evidence of any other cause.21
Microbiological examination
Specimens were taken from the liver recipients for routine bacterial culture and were immediately transported to the clinical microbiology laboratory. The Vitek-2 system (bioMérieux, Marcy l’Etoile, France) was used to identify A. baumannii. Antibiotic susceptibility was determined by the Kirby-Bauer method and minimum inhibitory concentration tests according to guidelines established by the Clinical Laboratory Standards Institute.22 A. baumannii with intermediate susceptibility to antibiotics was considered to be resistant. All 12 antibiotics used were commercially available products from Oxoid (Altrincham, UK), including aztreonam, piperacillin-tazobactam, cefoperazone-sulbactam, cefazolin, cefuroxime, ceftazidime, cefepime, amikacin, levofloxacin, meropenem, tigecycline, and trimethoprim-sulfamethoxazole.
Results
Over the study period, 24 episodes of A. baumannii infection occurred in 17 liver recipients. Within 2 weeks of transplantation, there were 62.5% (15/24) episodes of A. baumannii infection. The median time taken to develop A. baumannii infection was 11.5 (interquartile range 5–20) days after liver transplantation. Positive cultures of A. baumannii were obtained from the lung (n=8), intra-abdominal/biliary duct (n=8), blood (n=7), and the urinary tract (n=1). Most episodes of infections were nosocomial (95.8%, n=23). Fifty percent (12/24) of all episodes of infection were related to inappropriate antibiotic therapy.
The mean age of the 17 liver recipients with A. baumannii infection was 49.7±8.6 years with a male predominance (64.7%, n=11). The most common sites of infection were multiple culture-positive (35.3%, n=6). Of these, one patient each occurred bacteremia accompied by pneumonia and peritonitis, and bacteremia accompanied by urinary tract infection; two patients developed bacteremia accompanied by pneumonia; and two patients had bacteremia accompanied by peritonitis. Nine, seven, and 12 recipients has a serum creatinine level of >1.5 mg/dL, a white blood cell count of >15,000/mm3, and a platelet count of <50,000/mm3, respectively, at the onset of A. baumannii infection. About 24% of patients (4/17) had a serum albumin level of <35 g/L, and 17.6% (3/17) had a lymphocyte count of <0.5×109/L. There were five (29.4%) episodes of septic shock and eight (47.1%) deaths. Eight patients (47.1%) had a body temperature of ≥38°C at the onset of A. baumannii infection. Table 1 shows the demographic, laboratory, and clinical characteristics of the 17 liver recipients with A. baumannii infection.
  | Table 1 Demographic, laboratory, and clinical characteristics of 17 liver recipients with Acinetobacter baumannii infection |
The antibiotic resistance rate of all A. baumannii infections to ten of 12 antibiotics investigated was more than 60%. Seventy-five percent of A. baumannii infections were carbapenem-resistant and ceftazidime-resistant, but were relatively sensitive to tigecycline (resistance rate 4.2%) and cefoperazone-sulbactam (resistance rate 45.8%). Rods were most resistant to cefazolin (resistance rate 87.5%) and cefuroxime (resistance rate 83.3%).
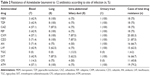
The drug resistance rate of A. baumannii was the highest in pneumonia and the rate of all A. baumannii infections to ten of the 12 antibiotics was ≥75%. The drug resistance rate of A. baumannii causing bacteremia was the lowest and the rate of all A. baumannii infections to seven of the 12 antibiotics was <50%. The antibiotic resistance rate of A. baumannii to the 12 antibiotics is shown in Table 2.
Discussion
Infection is still one of the most important complications in liver transplantation. van Delden et al reported that the prevalence of multidrug-resistant Acinetobacter is increasing, and is related to higher rates of treatment failure in solid organ transplant recipients.23 Shi et al reported that 62.5% of A. baumannii infections in bacteremic liver transplant recipients were multidrug-resistant rods.6
We found that the drug resistance rate of all A. baumannii infections to ten of the 12 antibiotics investigated was more than 60%. Drug susceptibility testing showed that A. baumannii was relatively susceptible to cefoperazone/sulbactam and tigecycline (drug resistance rate <50%). Seventy-five percent of A. baumannii infections were carbapenem-resistant in the present study, which is lower than the drug resistance rate of 82.4%–92.8% reported by previous studies targeting liver transplant recipients.12,14 The study by Bodro et al24 reported results similar to ours in solid organ transplant recipients with bacteremia. We also found that 75% of A. baumannii infections were ceftazidime-resistant, which is higher than the rate from a study suggesting that 50% of A. baumannii were ceftazidime-resistant.13
Most of the positive A. baumannii cultures were obtained from the lung (n=8) and intra-abdominal/biliary duct (n=8). Similarly, in a study of 37 liver transplant recipients, Kim et al reported the most common site of Acinetobacter infection to be the biliary tract (56.8%), followed by the pulmonary system (18.9%).14 The reason for the lungs being common foci for A. baumannii infection is that A. baumannii can utilize short, fimbrial-like protrusions on the bacterial cell surface to attach with great avidity to bronchial epithelial cells.25,26
We also found the drug resistance rate of A. baumannii in pneumonia was higher than at other sites, in line with reports suggesting that extensively drug-resistant A. baumannii almost exclusively caused respiratory infections in solid organ transplant patients.27–29
Carbapenem-resistant A. baumannii infections are associated with a high mortality rate in solid organ transplant recipients.14,27,28,30 The mortality in liver recipients with A. baumannii bacteremia can reach 100%.13 In the present study, we found that liver recipients with A. baumannii infection had a high mortality rate of 47.1%. Our findings might be explained by the high proportion of nosocomial infections, the strong resistance of pathogens to commonly used antibiotics, and the high proportion of infections treated with inappropriate antibiotic therapy. Zhong et al also suggested that Acinetobacter sepsis led to fatal outcomes due to its multidrug resistance.31
The exceedingly resistant A. baumannii in liver transplant recipients poses a new therapeutic challenge. Recurrence or persistence of A. baumannii infection despite treatment with susceptible antibiotics has also been described.28,30,32 Infections caused by carbapenem-resistant A. baumannii might be treated with cefoperazone-sulbactam and tigecycline according to our present findings. In immunocompetent patients with a sulbactam-susceptible Acinetobacter isolate, monotherapy with sulbactam was as effective as imipenem in the treatment of ventilator-associated pneumonia33 and bloodstream infection.34 Tigecycline, a glycylcycline derivative of tetracycline, has demonstrated success in the treatment of carbapenem-resistant A. baumannii infection.35
Monotherapy with an antibiotic has been reported to be associated with the emergence of resistant strains.36 Combination therapy for multidrug-resistant bacteria may be beneficial.37 One study reported a significantly higher survival rate in transplant recipients treated with a combination of colistin and carbapenem.28 However, combination of colistin and tigecycline is associated with a high rate of treatment failure and emergence of resistance.38,39 In addition, prevention measures are beneficial for liver recipients at high risk of infection. A. baumannii is a common isolate in the hospital environment.40 A. baumannii infection can be caused by cross-infection. Therefore, some measures, such as limiting use of respiratory machines, early removal of unnecessary central venous catheters, and preventing cross-infection can effectively reduce the risk of A. baumannii infection. Active surveillance for A. baumannii is also recommended in institutions with high rates of resistant A. baumannii to guide clinicians in their choice of effective perioperative prophylaxis in patients with suspected A. baumannii infection while the results of cultures are pending.
This study was limited by its retrospective design and small sample size. A further limitation was possible underestimation of A. baumannii infection because some cases received empiric courses of antimicrobial therapy before specimens for bacterial culture were obtained. Finally, this was a two-center study, so the external validity of our findings might be compromised.
Conclusion
The clinical manifestations of A. baumannii infection included high body temperature, decreased serum albumin levels, low platelet and lymphocyte counts, elevated white blood cell counts, and onset in the early period after liver transplantation, as well as high mortality. The antibiotic resistance rate of A. baumannii was extremely high in liver recipients. To improve the outcomes of liver recipients with A. baumannii infection, prevention and combination antibiotic therapy can be beneficial.
Disclosure
The authors report no conflicts of interest in this work.
References
Kim SI. Bacterial infection after liver transplantation. World J Gastroenterol. 2014;20:6211–6220. | ||
Dummer JS, Singh N. Infections in solid organ transplant recipients. In: Mandell GL, Bennett JE, Dolin R, editors. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. 7th ed. Philadelphia, PA, USA: Churchill Livingstone; 2010. | ||
Fishman JA. Infection in solid-organ transplant recipients. N Engl J Med. 2007;357:2601–2614. | ||
Kusne S, Dummer JS, Singh N, et al. Infections after liver transplantation. An analysis of 101 consecutive cases. Medicine (Baltimore). 1988;67:132–143. | ||
Soong RS, Chan KM, Chou HS, et al. The risk factors for early infection in adult living donor liver transplantation recipients. Transplant Proc. 2012;44:784–786. | ||
Shi SH, Kong HS, Xu J, et al. Multidrug resistant gram-negative bacilli as predominant bacteremic pathogens in liver transplant recipients. Transplant Infect Dis. 2009;11:405–412. | ||
Falagas ME, Snydman DR, Griffith J, et al. Exposure to cytomegalovirus from the donated organ is a risk factor for bacteremia in orthotopic liver transplant recipients. Clin Infect Dis. 1996;23:468–474. | ||
Sganga G, Spanu T, Bianco G, et al. Bacterial bloodstream infections in liver transplantation: etiologic agents and antimicrobial susceptibility profiles. Transplant Proc. 2012;44:1973–1976. | ||
Wan QQ, Ye QF, Ming YZ, et al. The risk factors for mortality in deceased donor liver transplant recipients with bloodstream infections. Transplant Proc. 2013;45:305–307. | ||
Kim S, Kim YJ, Jun YH, et al. Epidemiology and risk factors for bacteremia in 144 consecutive living-donor liver transplant recipients. Yonsei Med J. 2009;50:112–121. | ||
Iida T, Kaido T, Yagi S, et al. Posttransplant bacteremia in adult living donor liver transplant recipients. Liver Transpl. 2010;16:1379–1385. | ||
Kim HK, Park YK, Wang HJ, et al. Epidemiology and clinical features of post-transplant bloodstream infection: an analysis of 222 consecutive liver transplant recipients. Infect Chemother. 2013;45:315–324. | ||
Bert F, Larroque B, Paugam-Burtz C, et al. Microbial epidemiology and outcome of bloodstream infections in liver transplant recipients: an analysis of 259 episodes. Liver Transpl. 2010;16:393–401. | ||
Kim YJ, Yoon JH, Kim SI, et al. High mortality associated with Acinetobacter species infection in liver transplant patients. Transplant Proc. 2011;43:2397–2399. | ||
Otan E, Aydin C, Usta S, et al. Acinetobacter infection in a liver transplantation intensive care unit. Transplant Proc. 2013;45:998–1000. | ||
Nie K, Ran R, Tan W, et al. Risk factors of intra-abdominal bacterial infection after liver transplantation in patients with hepatocellular carcinoma. Chin J Cancer Res. 2014;26:309–314. | ||
Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36:309–332. | ||
Florescu DF, Qiu F, Langnas AN, et al. Bloodstream infections during the first year after pediatric intestinal transplantation. Pediatr Infect Dis J. 2012;31:700–704. | ||
Levry MM, Fink MP, Marshall JC, et al; for the International Sepsis Definitions Conference. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definition Conference. Intensive Care Med. 2003;29:530–538. | ||
Kollef MH, Micek ST. Strategies to prevent antimicrobial resistance in the intensive care unit. Crit Care Med. 2005;33:1845–1853. | ||
Wan Q, Ye Q, Zhou J. Mortality predictors of bloodstream infections in solid-organ transplant recipients. Exp Clin Transplant. 2013;11:211–214. | ||
Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Disk Susceptibility Tests, 16th Informational Supplement. CLSI document M100-S16. Wayne, PA, USA: Clinical and Laboratory Standards Institute; 2006. | ||
van Delden C, Blumberg EA. Multidrug resistant gram-negative bacteria in solid organ transplant recipients. Am J Transplant. 2009;9 Suppl 4:S27–S34. | ||
Bodro M, Sabé N, Tubau F, et al. Risk factors and outcomes of bacteremia caused by drug-resistant ESKAPE pathogens in solid-organ transplant recipients. Transplantation. 2013;96:843–849. | ||
Lee HW, Koh YM, Kim J, et al. Capacity of multidrugresistant clinical isolates of Acinetobacter baumannii to form biofilm and adhere to epithelial cell surfaces. Clin Microbiol Infect. 2008;14:49–54. | ||
Lee JC, Koerten H, van den Broek P, et al. Adherence of Acinetobacter baumannii strains to human bronchial epithelial cells. Res Microbiol. 2006;157:360–366. | ||
Reddy P, Zembower TR, Ison MG, et al. Carbapenem-resistant Acinetobacter baumannii infections after organ transplantation. Transpl Infect Dis. 2010;12:87–93. | ||
Shields RK, Clancy CJ, Gillis LM, et al. Epidemiology, clinical characteristics and outcomes of extensively drug-resistant Acinetobacter baumannii infections among solid organ transplant recipients. PLoS One. 2012;7:e52349. | ||
Nunley DR, Bauldoff GS, Mangino JE, et al. Mortality associated with Acinetobacter baumannii infections experienced by lung transplant recipients. Lung. 2010;188:381–385. | ||
de Gouvêa EF, Martins IS, Halpern M, et al. The influence of carbapenem resistance on mortality in solid organ transplant recipients with Acinetobacter baumannii infection. BMC Infect Dis. 2012;12:351. | ||
Zhong L, Men TY, Li H. Multidrug-resistant gram-negative bacterial infections after liver transplantation – spectrum and risk factors. J Infect. 2012;64:299–310. | ||
Martins N, Martins IS, de Freitas WV, et al. Severe infection in a lung transplant recipient caused by donor-transmitted carbapenem-resistant Acinetobacter baumannii. Transpl Infect Dis. 2012;14:316–320. | ||
Wood GC, Hanes SD, Croce MA, et al. Comparison of ampicillin-sulbactam and imipenem-cilastin for the treatment of Acinetobacter ventilator-associated pneumonia. Clin Infect Dis. 2002;34:1425–1430. | ||
Jellison TK, McKinnon PS, Rybak MJ. Epidemiology, resistance, and outcomes of Acinetobacter baumannii bacteremia treated with imipenem-cilastin or ampicillin-sulbactam. Pharmacotherapy. 2001;21:142–148. | ||
Taccone FS, Rodriguez-Villalobos H, De Backer D, et al. Successful treatment of septic shock due to pan-resistant Acinetobacter baumannii using combined antimicrobial therapy including tigecycline. Eur J Clin Microbiol Infect Dis. 2006;25:257–260. | ||
Cai Y, Chai D, Wang R, et al. Colistin resistance of Acinetobacter baumannii: clinical reports, mechanisms and antimicrobial strategies. J Antimicrob Chemother. 2012;67:1607–1615. | ||
Sun HY, Shields RK, Cacciarelli TV, et al. A novel combination regimen for the treatment of refractory bacteremia due to multidrug-resistant Pseudomonas aeruginosa in a liver transplant recipient. Transpl Infect Dis. 2010;12:555–560. | ||
Ku K, Pogue JM, Moshos J, et al. Retrospective evaluation of colistin versus tigecycline for the treatment of Acinetobacter baumannii and/or carbapenem-resistant Enterobacteriaceae infections. Am J Infect Control. 2012;40:983–987. | ||
Shields RK, Kwak EJ, Potoski BA, et al. High mortality rates among solid organ transplant recipients infected with extensively drug-resistant Acinetobacter baumannii: using in vitro antibiotic combination testing to identify the combination of a carbapenem and colistin as an effective treatment regimen. Diagn Microbiol Infect Dis. 2011;70:246–252. | ||
Mermel LA. Prevention of intravascular catheter-related infections. Ann Intern Med. 2002;132:391–402. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.