Back to Journals » Therapeutics and Clinical Risk Management » Volume 17
Different Effect of Lanthanum Carbonate and Sevelamer Hydrochloride on Calcium Balance in Patients with Moderate to Advanced Chronic Kidney Disease
Received 23 July 2021
Accepted for publication 28 September 2021
Published 2 November 2021 Volume 2021:17 Pages 1145—1151
DOI https://doi.org/10.2147/TCRM.S330649
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Agnieszka Makowka, Michal Nowicki
Department of Nephrology, Hypertension and Kidney Transplantation, Medical University of Lodz, Lodz, Poland
Correspondence: Michal Nowicki
Department of Nephrology, Hypertension and Kidney Transplantation, Medical University of Lodz, Central University Hospital, Pomorska Str 251, Lodz, 92-213, Poland
Tel +48 42 2014400
Fax +48 42 2014401
Email [email protected]
Objective: Opposite to lanthanum carbonate (LC), sevelamer hydrochloride (SH) may increase intestinal calcium absorption. The study compared the effects of LC and SH on serum and urine phosphate and calcium, and on hormones regulating mineral-bone metabolism.
Patients and Methods: A prospective randomized crossover study included 34 patients with eGFR < 60 mL/min. A single oral dose of LC (1,000 mg) or SH (2,400 mg) was administered in random order 15 minutes after a standardized meal fortified with 5 g calcium carbonate. Serum calcium, phosphate, and parathormone were measured before and 3, 6, 12, and 24 hours after each medication. Bone alkaline phosphatase (BAP), sclerostin, calcitriol, and FGF-23 were measured at baseline and after 12 and 24 hours. A 24-hour calcium and phosphate excretion was measured after each drug.
Results: Serum calcium increased 3 and 6 hours after SH then returned to baseline. After LC calcium was unchanged for up to 3 hours then transiently increased and eventually returned to baseline. The area under curve (AUC) of serum calcium for 12 hours after SH was larger than after LC (p=0.04). Serum phosphate decreased after each drug with a nadir 3 hours post-SH and 6 hours post-LC. AUC of serum phosphate was similar after both medications. PTH decreased transiently after both drugs. BAP did not change. FGF-23 was constant for the first 12 hours but later decreased after each drug.
Conclusion: A 2,400 mg SH and 1,000 mg LC are similarly effective in lowering serum phosphate in CKD, but LC induce in less intestinal calcium absorption after a meal. The trial was registered on February 23, 2018 in the clinicaltrial.gov database – NCT03451019.
Keywords: calcium, chronic kidney disease – mineral bone disorder, hyperphosphatemia, phosphate-binders, PTH
Introduction
Cardiovascular risk increases steeply with the progression of chronic kidney disease (CKD).1–3 Although the mechanisms linking CKD with cardiovascular disease are complex they appear to be closely associated with the development of the mineral and bone disorder (CKD–MBD).2,3
CKD–MBD starts to develop as early as in stage 2 CKD and advance in parallel with the progression of the disease. CKD–MBD is associated with a progressive decrease of serum calcitriol and Klotho concentration and a great increase of serum FGF-23 and PTH.2–4 Phosphate retention appears to be a primary mineral disturbance that leads both to the stimulation of the parathyroid glands to secrete PTH and the osteocyte to secrete FGF-23. Increased concentrations of phosphorus and FGF-23 are recognized as major risk factors of cardiovascular morbidity in CKD.5,6
Effective control of phosphate metabolism in CKD may be crucial in preventing the progression of vascular calcifications and cardiovascular disease.7,8 Dietary restriction of phosphate intake may be insufficient to maintain normal serum phosphate levels in these patients as it may cause or worsen protein and energy malnutrition. Thus, most CKD patients require oral phosphate binders to control hyperphosphatemia.
Calcium-containing oral phosphate binders may induce hypercalcemia and thereby promote vascular calcification that adds to the risk of cardiovascular events.9,10
Therefore, drugs were searched for that would be effective in lowering serum phosphate and at the same time did not cause hypercalcemia. Those calcium-free binders that contain a resin such as sevelamer or a metal such as lanthanum may have a more favorable safety profile.9–19 A meta-analysis showed that sevelamer hydrochloride (SH) use was associated with the reduction in all-cause but not cardiovascular mortality compared to calcium-based binders.11 Toussaint et al10 showed a reduction of aortic calcification with lanthanum carbonate (LC) compared to calcium-based binder use.
A single study in healthy volunteers that compared calcium absorption after a single-dose of LC (1,000 mg) or SH (2,400 mg) showed that only the administration of the former reduced the amount of calcium absorbed from the intestine within 2 hours after its administration.20 However, similar studies have not been conducted in patients with CKD with kidney function impairment.
The aim of our study was to compare the effect of a single dose of LC and SH following an oral load of calcium carbonate on serum concentration and urine excretion of phosphate and calcium, and on the hormones that regulate mineral metabolism.
Patients and Methods
The study was a prospective comparative crossover randomized open-label trial. The effect of a single dose of 1,000 mg LC with 2,400 mg SH on serum and urine calcium and phosphate following the oral load of 5 g of calcium carbonate with a meal with standardized calcium and phosphate content was compared.
The study protocol has been approved by the local Bioethics Committee of the Medical University of Łódź and each patient gave informed written consent for participation in the study. The study was conducted in accordance with the Declaration of Helsinki.
Patient enrollment for the study started in March 2018, and the clinical part of the study was completed in December 2020. Thirty-four patients (18 male, 16 female, mean age 62±14 years) with eGFR ≤45 mL/min were included. The exclusion criteria included hypercalcemia (>ULN), serum phosphate >1.2-times upper limit of normal range and calcium-phosphate disturbances not associated with CKD, eg, Paget’s disease, severe osteoporosis, any bone fracture within 6 months before the study, previous diagnosis of multiple myeloma or any malignancy, liver or biliary tract disease, primary hyperparathyroidism, use of phosphate binder or other drug that may interfere with intestinal calcium absorption within 2 weeks before the qualification visit including use of active vitamin D (1-alpha, calcitriol, or vitamin D analog) less than 1 week before the qualification visit. Inactive vitamin D, ie, cholecalciferol or calcifediol, was allowed in a dose <800 IU/24 hours provided that it was continued in unchanged dose for the duration of the study. The patients were randomly allocated to two equal size arms in which they received either LC followed by SH or SH followed by LC.
A single oral dose of LC (1,000 mg) or SH (2,400 mg) was administered in a random order with a 48-hour wash-out period between the administration of phosphate binders. Each study medication was given 15 minutes after an oral intake of 5 g of calcium carbonate with a meal containing the standardized amount of calcium and phosphate. The study design is shown in Figure 1.
 |
Figure 1 Flowchart showing the study design. |
Serum calcium (Ca), phosphate (P), and parathyroid hormone were measured at baseline and 3, 6, 12, and 24 hours after the administration of each study drug. BAP, sclerostin (Scl), 1,25-OH2- vitamin D3, and FGF-23 were measured at baseline and 12 and 24 hours after each dose. The urine for the assessment of calcium, phosphate, and creatinine (Cr) excretion was collected for 24 hours after the administration of each study drug. Urine phosphate and calcium-to-urine creatinine ratios were calculated to assess phosphate and calcium excretion.
The 12-hour area under the curve (AUC) of serum calcium and phosphate was calculated using the trapezium method.
The descriptive statistics included the calculation of the arithmetic mean and standard deviation (SD) or median with 25–75% interquartile range. The changes of urine electrolytes induced by study medication was shown as mean with 95% confidence interval. Normality of the distribution of variables was examined with Shapiro–Wilk test. The means between groups were compared with two-sided t-test or Mann–Whitney test depending on variable distribution. ANOVA was used to analyze repeated measurements. P-value <0.05 was taken as significant.
Results
Serum calcium concentration increased slightly but significantly after a high-calcium meal followed by 2.4 g of SH from 2.28±0.14 to 2.31±0.16 and 2.32±0.2 mmol/l 3 and 6 hours post-dose, respectively (p=0.02). Serum calcium returned to baseline level in the following 6 hours. After the high-calcium meal followed by 1,000 mg of LC serum calcium did not significantly change from baseline (2.26±0.14) for up to 3 hours post-dose (2.26±0.18) but later (6 hours post-dose) increased to 2.29±0.19 mmol/l (p=0.02) and returned to baseline in the next 6 hours (Figure 2). AUC of serum calcium for 12 hours following SH administration was significantly larger than after LC (6.91±0.43 versus 6.82±0.51) (p=0.04).
 |
Figure 2 Serum calcium concentration over 24 hours following a single oral dose of sevelamer or lanthanum. |
Serum phosphate decreased rapidly after both drugs with a nadir at 3 hours after SH and at 6 hours after LC (1.20 ±0.26 mmol/l versus 1.19±0.27 mmol/l; ns) (Figure 3). AUC of serum phosphate was similar after both medications (3.51 versus 3.79 after SH and LC, respectively).
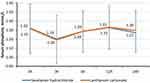 |
Figure 3 Serum concentration of phosphate after a single oral dose of sevelamer or lanthanum. |
Serum PTH decreased transiently after both drugs with a nadir at 3 hours post-dose but later increased above baseline levels (Figure 4).
 |
Figure 4 Plasma concentration of PTH after a single dose of sevelamer and lanthanum. |
As shown in Table 1, serum BAP remained unchanged after each drug. Serum FGF-23 was unchanged at 12 and 24 hours after each phosphate binder. Serum sclerostin did not significantly change during the study. 1,25-OH2 vitamin D3 (1,25(OH)2D3) remained stable after SH and LC.
Urine calcium to creatinine ratio did not change significantly for 24 hours after SH (mean change 16 mg/g; 95% CI [−23, 45]) or LC (mean change 12 mg/g; 95% CI [−15, 36]). There were also no statistically significant changes of urine phosphate/creatinine ratio after SH (mean change −88 mg/g [95% CI −354, 33]) or LC (mean change −96 mg/g [95% CI −244, 52]).
Discussion
Our study showed that both LC in a single oral dose of 1,000 mg and SH in the equipotent single-dose of 2,400 mg decreased serum phosphate concentration to a similar extent and caused a similar decrease of urine phosphate excretion. Such effects were seen in previous clinical studies that used the same doses of both phosphate binders, ie, 1,000 mg and 2,400 mg, respectively, as well as in several experimental animal studies.11,20,21
It was postulated that the treatment with LC may provide an additional benefit compared to SH due to lower risk of hypercalcemia.20 Our study may support that notion since we were able to show a small but significant increase of serum calcium concentration after a single dose of SH in patients with CKD with reduced GFR. In contrast, a dose of LC did not result in a significant change of serum calcium 3 hours after the drug dose. Although 3 hours later the increase of serum calcium after LC became significant, 12-hour AUC for serum calcium after drug doses remained significantly larger after SH than after LC. A similar observation was made by Behets et al20 after a single dose of 1,000 mg LC or 2,400 mg sevelamer carbonate; however that study included only healthy volunteers with normal renal function. We also measured the urine excretion of calcium that was similar after both binders. In contrast, Behets et al20 observed an increase of urinary calcium excretion after SH but not after LC.
These two observations may suggest the increased gastrointestinal absorption of calcium after SH compared to LC. Behets et al20 tried to further investigate the mechanism of this effect and demonstrated the direct inhibitory effect of lanthanum on calcium transport in the intestinal epithelium. The exact molecular mechanism was not elucidated in their study but another earlier experimental study showed that lanthanum carbonate may inhibit intestinal oxalate absorption and thus might limit calcium absorption due to increased calcium oxalate formation in the intestine.22
Furthermore, one systematic review confirmed that lanthanum but not SH led to significant reduction of serum calcium compared with calcium-based agents.16 That finding was, however, based only on the results of two studies and the difference between two binders was small, ie, −0.35 mg/dL, 95% CI=−0.64 to −0.25. The same analysis also provided the evidence that the use of both SH and LC in dialysis patients may reduce the number of hypercalcemic episodes compared to calcium-based phosphate binders. However, the studies included in that analysis were not designed and sufficiently powered to directly compare SH to LC-based binder.16
In another meta-analysis11 and in an animal experiment21 carried out in a model of kidney failure with a treatment period of 4 weeks no difference in the incidence of hypercalcemia between SH and LC was revealed.
Prajapati et al15 in turn reported an opposite effect in hemodialysis patients and found a small non-significant increase of serum calcium during SH treatment and a significant increase of serum calcium in LC-treated patients. However, the patients in that study were treated with different doses of phosphate binders, ie, 1,200 mg/24 hours SH and 1,500 mg/24 hours LC, and the treatment period was 3 months.
We did not reveal any difference in the effect of SH and LC on serum PTH. That finding could be explained by the small difference in the reported effect on serum calcium and a short duration of the observation. Also, Behets et al,20 in their single dose experiment, did not find any difference of the serum concentration of PTH between SH and LC.
Gonzalez-Parra et al23 conducted a study that included patients with stage 3 CKD. The patients received LC 750 mg thrice daily for 4 weeks but that did not lead to any significant change of serum PTH. Also Spasovsky et al24 did not report any significant effect of 1-year treatment with LC on serum PTH and BAP. Prajapati et al15 in turn found a significant decrease of PTH concentration after 12-week treatment with LC and SH in hemodialysis patients.
Patel et al16 found that SH treatment was associated with an increase of serum PTH compared to calcium-containing oral phosphate binders.
Iwata et al25 studied the effect of SH on selected markers of bone turnover in hemodialysis patients with adynamic bone disease and showed that the conversion from calcium binders to SH led to the increase of both PTH and BAP. These effects were only seen after 48 weeks of treatment.
The previously reported effects of oral phosphate binders on serum FGF-23 have been conflicting. Our study did not show any difference in FGF-23 concentration after a single dose of SH and LC. Gonzalez-Parra et al23 showed in a rat experiment that 4-week LC treatment significantly decreased serum FGF-23. Phan et al21 and Spatz et al26 found that neither 4 nor 12-week SH administration resulted in significant changes of serum FGF-23. The lack of effect of phosphate binders on serum FGF 23 in our study could be explained by its short duration, since the changes of this hormone are only seen after at least several days of treatment.27,28
Block et al8 assessed the effect of phosphate binders including calcium acetate 1.5 g elemental calcium, 2.7 g/d lanthanum carbonate, and 6.3 g/d sevelamer carbonate on bone turnover parameters in CKD patients. In their study, intact FGF-23, ie, the same as assessed in our study, decreased after SH and increased after calcium acetate but C–terminal FGF-23 did not change.8
1,25-OH vitamin D remained unchanged after SH in our study, but decreased 12 hours after LC and later returned to baseline. Pierce et al29 compared the effect of two non-calcium binders, ie, SH and LC on 1,25-OH vitamin D concentration in healthy volunteers treated with calcitriol and showed that after SH serum concentration of calcitriol was lower after the treatment in patients who received a combined LC and calcitriol therapy than in those who only received calcitriol. The authors suggested that the difference could be explained by the fact that only SH can bind the bile salts that may lead to the impairment of the absorption of fat-soluble molecules including vitamin D sterols.
Although our study included a small number of participants and assessed only the effect of a single dose, there was a significant difference in the effect of two non-calcium phosphate binders on serum calcium after a meal fortified with calcium carbonate without any difference in their effect on serum phosphate. The clinical relevance of this effect needs to be investigated in a longer and larger study.
Data Sharing Statement
The authors intend to provide full individual data of participants without identification data, upon request. Please send your request for original data to the e-mail address of Prof. Michał Nowicki: [email protected].
Acknowledgments
Trial registration: 23/Feb/2018 - clinicaltrial.gov database - NCT03451019.
Funding
The study was investigator-driven and was supported by an unrestricted grant from Shire.
Disclosure
The authors declare no conflicts of interest.
References
1. Chue CD, Townend JN, Moody WE, et al. Cardiovascular effect of sevelamer in stage 3 in CKD. J Am Soc Nephrol. 2013;24:842–852. doi:10.1681/ASN.2012070719
2. Demer L, Tintut Y. The bone-vascular axis in chronic kidney disease. Curr Opin Nephrol Hypertens. 2010;19:349–353. doi:10.1097/MNH.0b013e32833a3d67
3. Russo D, Miranda I, Ruocco C, et al. The progression of coronary artery calcification in predialysis patients on calcium carbonate or sevelamer. Kidney Int. 2007;72:1255–1261. doi:10.1038/sj.ki.5002518
4. Yono S, McKee MD, Murry C, et al. Phosphate regulation of vascular smooth muscle cell calcification. Circ Res. 2000;29:E10–E17.
5. Hrushka KA, Mathew S. The role of the skeleton and phosphorus in the CKD mineral bone disease. Adv Chronic Kidney Dis. 2011;18:98–104. doi:10.1053/j.ackd.2011.01.001
6. Cunningham J, Locatelli F, Rodriquez M. Secondary hyperparathyroidism: pathogenesis, disease progression, and therapeutic options. Clin J Am Soc Nephrol. 2011;6:913–921. doi:10.2215/CJN.06040710
7. Suki WN, Zabaneh R, Cangiano JL, et al. Effects of sevelamer and calcium-based phosphate, binders on mortality in hemodialysis patients. Kidney Int. 2007;72:1130–1137. doi:10.1038/sj.ki.5002466
8. Block GA, Wheeler DC, Persky MS, et al. Effects of phosphate binders in moderate CKD. J Am Soc Nephrol. 2012;23:1407–1415. doi:10.1681/ASN.2012030223
9. Wada K, Wada Y. Evaluation of aortic calcification with lanthanum carbonate vs. calcium-based phosphate binders in maintenance hemodialysis patients with type 2 diabetes mellitus: an open-label randomized controlled trial. Ther Apher Dial. 2014;18:353–360. doi:10.1111/1744-9987.12153
10. Toussaint ND, Lau KK, Polkinghorme KR, Kerr PG. Attenuation of aortic calcification with lanthanum carbonate versus calcium-based phosphate binders in hemodialysis: a pilot randomized controlled trial. Nephrology. 2011;16:290–298. doi:10.1111/j.1440-1797.2010.01412.x
11. Ruospo M, Ruospo M, Palmer SC, et al. Phosphate binders for preventing and treating chronic kidney disease-mineral and bone disorder (CKD-MBD). Cochrane Database Syst Rev. 2018. doi:10.1002/14651858.CD006023.pub3
12. Zhai C-J, Yang X-W, Sun J, Wang R. Efficacy and safety of lanthanum carbonate versus calcium-based phosphate binders in patients with chronic kidney disease: a systematic review and meta-analysis. Int Urol Nephrol. 2015;47(3):527–535. doi:10.1007/s11255-014-0876-x
13. Liu Y-L, Lin -H-H, Yu -C-C, et al. A comparison of sevelamer hydrochloride with calcium acetate on biomarkers of bone turnover in hemodialysis patients. Ren Fail. 2006;28(8):701–707. doi:10.1080/08860220600925388
14. Wang C, Liu X, Zhou Y, et al. New conclusion regarding comparison of sevelamer and calcium-based phosphate binders in coronary-artery calcification for dialysis patients: a meta-analysis of randomized controlled trials. PLoS One. 2015;10:e0133938.
15. Prajapati VA, Galani VJ, Shah PR. A comparative study of phosphate binders in patients with end stage kidney disease undergoing hemodialysis. Saudi J Kidney Dis Transpl. 2014;25:530–538. doi:10.4103/1319-2442.132167
16. Patel L, Bernard LM, Elder GJ. Sevelamer Versus Calcium-Based Binders for Treatment of Hyperphosphatemia in CKD: A Meta-Analysis of Randomized Controlled Trials. Clin J Am Soc Nephrol. 2016;11(2):232-44. doi:10.2215/CJN.06800615
17. Taylor MJ, Elgazzar HA, Chaplin S, Goldsmith D, Molony DA. A economic evaluation of sevelamer in patients new to dialysis. Curr Med Res Opin. 2008;24:601–608. doi:10.1185/030079908X260853
18. Chertow GM, Burke SK, Raggi P. Sevelamer attenuates the progression of coronary and aortic calcification in hemodialysis patients. Kidney Int. 2002;62:245–252. doi:10.1046/j.1523-1755.2002.00434.x
19. Zhang C, Wen J, Li Z, Fan J. Efficacy and safety of lanthanum carbonate on chronic kidney disease-mineral and bone disorder in dialysis patients: a systematic review. BMC Nephrol. 2013;14:226. doi:10.1186/1471-2369-14-226
20. Behets GJ, Dams G, Damment SJ, Martin P, De Broe ME, D’Haese PC. Differences in gastrointestinal calcium absorption after the ingestion of calcium-free phosphate binders. Am J Physiol Renal Physiol. 2014;306:61–67. doi:10.1152/ajprenal.00219.2013
21. Phan O, Maillard M, Malluche HH, Stehle J-C, Funk F, Burnier M. Effect of sucroferric oxyhydroxide compared to lanthanum carbonate and sevelamer carbonate on phosphate homeostasis and vascular calcifications in rat model of chronic kidney disease. BioMed Res Int. 2015;2015:515606. doi:10.1155/2015/515606
22. Robijn S, Vervaet BA, Hoppe B, D’Haese PC, Verhulst A. Lanthanum carbonate inhibits intestinal oxalate absorption and prevents nephrocalcinosis after oxalate loading in rats. J Urol. 2013;189:1960–1966. doi:10.1016/j.juro.2012.12.004
23. Gonzalez-Paara E, Egonzalez-Causa ML, Galan A, et al. Lanthanum carbonate reduces FGF-23 in chronic kidney disease stage 3 patients. Nephrol Dial Transplant. 2011;26:2567–2571. doi:10.1093/ndt/gfr144
24. Spasovski GB, Sikole A, Gelev S, et al. Evolution of bone and plasma concentration of lanthanum in dialysis patients before, during 1 year of treatment with lanthanum carbonate and after 2 years of follow-up. Nephrol Dial Transplant. 2006;21:2217–2224. doi:10.1093/ndt/gfl146
25. Iwata Y, Wada T, Yokoyama H, et al. Effect of sevelamer hydrochloride on markers of bone turnover in Japanese dialysis patients with low biointact PTH levels. Ren Fail. 2006;28:701–707.
26. Spatz C, Roe K, Lehman E, Verma N. Effect of a non-calcium-based phosphate binder on fibroblast growth factor 23 in chronic kidney disease. Nephron Clin Pract. 2013;123:61–66. doi:10.1159/000351811
27. Muras K, Masajtis-Zagajewska A, Nowicki M. Diabetes modifies effect of high-phosphate diet on fibroblast growth factor-23 in chronic kidney disease. J Clin Endocrinol Metab. 2013;98:E1901–E1908. doi:10.1210/jc.2013-2418
28. Oliveira RB, Cancela ALE, Graciolli FG, et al. Early control of PTH and FGF23 in normophosphatemic CKD patients: a new target in CKD-MBD therapy? Clin J Am Soc Nephrol. 2010;5:286–291. doi:10.2215/CJN.05420709
29. Pierce D, Hossack S, Poole L, et al. The effect of sevelamer carbonate and lanthanum carbonate on the pharmacokinetics of oral calcitriol. Nephrol Dial Transplant. 2011;26:1615–1621. doi:10.1093/ndt/gfq598
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

