Back to Journals » Patient Preference and Adherence » Volume 9
Dezocine for anesthesia and stress reduction in induced abortion
Authors Zheng M, Guo Y, Shan S, Yang S
Received 28 October 2014
Accepted for publication 23 December 2014
Published 3 March 2015 Volume 2015:9 Pages 369—372
DOI https://doi.org/10.2147/PPA.S76507
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Mengliang Zheng, Yanru Guo, Shiqiang Shan, Sen Yang
Department of Anesthesiology, Cangzhou Central Hospital, Hebei, People’s Republic of China
Background: The purpose of this study was to evaluate the efficacy of dezocine with regard to analgesic and stress reduction outcomes in women undergoing induced abortion.
Methods: A total of 126 women in early pregnancy (up to 14 weeks’ gestation) who underwent induced abortion at Cangzhou Central Hospital from May 2012 to May 2013 were randomly assigned to a control (propofol) group (n=63) or an intervention (propofol + dezocine) group (n=63). Wake-up time, orientation force recovery time, incidence of adverse reactions, postoperative visual analog scale (VAS) score, analgesic effect, and respiratory and circulatory monitoring before the operation, 5 minutes into the operation, and 5 minutes after the operation were compared between the two groups.
Results: The surgical procedure and anesthesia were performed successfully in all patients. Systolic and diastolic blood pressure and oxyhemoglobin saturation in the intervention group were significantly higher than in the control group; however, heart rate was significantly lower in the intervention group than in the control group 5 minutes into the operation (all P<0.05). There were no statistically significant differences in these parameters before surgery and after recovery. The postoperative VAS score (2.82±0.72), Ramsay score (2.65±0.65), and anesthetic effect in the intervention group were better than in the control group (3.90±0.84 and 2.21±0.49, respectively), and all differences were statistically significant (P<0.05). The wake-up time (3.41±0.79 minutes) and orientation force recovery time (4.28±0.92 minutes) were all significantly shorter (P<0.05) in the intervention group than in the control group, as was the incidence of adverse reactions (7.94% versus 26.98%, respectively).
Conclusion: Adverse reactions of propofol combined with dezocine in painless induced abortion are less while the analgesic effect is better.
Keywords: dezocine, painless induced abortion, stress, analgesic effect
Introduction
Painless induced abortion is widely used in the gynecology clinic, and is more acceptable for women than anesthetic-free induced abortion.1 Continuous parenteral analgesia in induced abortion leads to satisfactory pain reduction.2 Propofol is one of the most popular anesthetics in induced abortion, but has a poor analgesic effect, and can easily generate respiratory depression and other adverse reactions in high doses.3 Therefore, the search for safe and effective anesthesia continues. As a synthetic drug needing parenteral administration, dezocine is a competitive opioid receptor antagonist4 with few side effects. On the molecular level,5 dezocine interacts with three major opioid receptors, ie, μ, κ, and δ, with a strong affinity for μ and κ receptors but weaker affinity for the δ receptor. The unique molecular pharmacological profile of dezocine as a partial μ receptor agonist reduces its side effects in comparison with other opioids. Furthermore, dezocine is a widely used anesthetic in the People’s Republic of China, causes less severe adverse reactions, and has better analgesic effects than other anesthetics.6 However, studies regarding its use for anesthesia in induced abortion are scarce, and more clinical data is needed to guide its use. The aim of this study was to assess the efficacy of dezocine as an analgesic and its effect on stress reduction in induced abortion.
Materials and methods
Participants
This double-blind, prospective trial was carried out at Cangzhou Center Hospital in the People’s Republic of China. A total of 126 women in early pregnancy (less than 14 weeks’ gestation) who requested termination of pregnancy and were scheduled for induced abortion at Cangzhou Central Hospital from May 2012 to May 2013 were selected. All patients signed their informed consent and participated in the study voluntarily. Using a computer-generated table of random numbers, the women were randomly divided into two groups, ie, a control (propofol) group (n=63) and an intervention (propofol + dezocine) group (n=63). The inclusion criterion was American Society of Anesthesiologists physical status I–II. Exclusion criteria included known allergies, severe respiratory, neurological, or cardiovascular disease, narcotic drug dependence, hepatic or renal dysfunction, and recent history of immunosuppressant drug use.
Anesthesia methods
In the control group, anesthesia consisted of propofol 2–2.5 mg/kg maintained by intravenous injection. In the intervention group, anesthesia consisted of propofol 0.5–1.0 mg/kg + dezocine 0.1 mg/kg was used; dezocine was administered first followed by propofol 2–2.5 mg/kg. During surgery, we appended propofol 0.5–1.0 mg/kg when necessary, such as with emergent limb movement.
Intervention indices
Systolic blood pressure (BP), diastolic BP, heart rate, and oxygen saturation were recorded in each patient before surgery, 5 minutes into surgery and 5 minutes after surgery. Wake-up time, orientation force recovery time, and the incidence of vomiting, limb movement, respiratory depression and other adverse reactions were also recorded.
Clinical evaluations
Postoperative pain was assessed using a 10-point visual analog scale (VAS: no pain, 0; mild pain, 1–4; severe pain, 5–8; unbearable pain, 9–10).3 Using the Ramsay sedation scale, we assessed the degree of sedation 10 minutes after each procedure,7 including the following patient parameters: anxiety and agitation or restlessness (1); cooperation, orientation, and tranquility (2); responses to commands only (3); brisk response to light glabellar tap or loud auditory stimulus while asleep (4); sluggish response to light glabellar tap or loud auditory stimulus while asleep (5); or no response to light glabellar tap or loud auditory stimulus while asleep (6). Patient status during the operation was divided into three levels to evaluate the effect of anesthesia: fully still, without limb movements (1); relatively still, with slight limb movement that did not affect the operation (2); obvious limb movements that affected the operation (3).8
Data analysis
The data are shown as the mean ± standard deviation. Measured data of independent samples in both groups were conducted through a t-test, and the χ2 test was used to conduct counted data and a comparison between both groups. Results with P<0.05 were considered to be statistically significant. All data were analyzed using Statistical Package for the Social Sciences version 14.0 software (SPSS Inc, Chicago, IL, USA).
Ethics approval and informed consent
The study protocol was approved by the institutional human ethics committee at the hospital and written informed consent was obtained from each patient.
Results
Patient demographic and clinical characteristics
There were no significant differences between the two groups with regard to age, body weight, and weeks of gestation. In the control group, the mean patient age was 27.4±3.7 years, mean body weight was 56.3±6.7 kg, and mean gestational stage was 7.8±1.2 weeks; respective values in the intervention group were 25.6±4.2 years, 54.9±7.9 kg, and 8.2±0.7 weeks.
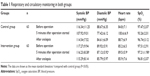
Respiratory and circulatory monitoring of patients in both groups
Systolic and diastolic BP, heart rate, and oxygen saturation were comparable before and after the procedure between the two groups (P>0.05). Five minutes after the procedure, systolic and diastolic BP and oxygen saturation were much higher in the intervention group than in the control group, with heart rate being lower in the intervention than in the control group; all values were statistically significant (P<0.05, Table 1).
Postoperative VAS and Ramsay scores
The mean postoperative VAS score in the intervention group (2.82±0.72) was significantly lower (P<0.05) than in the control group (3.90±0.84). The mean Ramsay score in the intervention group 10 minutes post procedure (2.21±0.49) was significantly lower (P<0.05) than in the control group (2.65±0.65). Achievement of level I anesthesia was significantly different (P<0.05) between the groups (95% in the intervention group versus 87% in the control group Table 2).
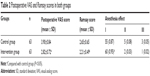  | Table 2 Postoperative VAS and Ramsay scores in both groups |
Wake-up time, orientation force recovery time, and incidence of adverse reactions
In the intervention group, the mean wake-up time (3.41±0.79 minutes) and orientation force recovery time (4.28±0.92 minutes) were shorter than in the control group (5.12±1.41 minutes and 6.02±0.972 minutes, respectively). The incidence of adverse reactions was significantly lower (P<0.05) in the intervention group than in the control group (7.94% versus 26.98%, respectively, Table 3).
  | Table 3 Wake-up time, orientation force recovery time, and incidence of adverse reactions in both groups |
Discussion
During an induced abortion procedure, vagal stimulation secondary to vaginal expansion and mechanical stimulation of the cervix and uterus leads to bradycardia, arrhythmia, and a blood pressure drop with its related symptoms, with some patients having hypotension-related syncope and convulsions during or shortly after the procedure.2,9,10 These effects can be improved by use of anesthesia during the operation. The anesthetic effect and safety of propofol has been well described, and it has been widely applied in induced abortion procedures; however, there still are some shortcomings with this agent. The addition of dezocine to propofol in induced abortion can compensate for these problems.
In the study, we found significant differences in mean postoperative VAS and Ramsay scores between our intervention and control groups, which confirm the sedative and analgesic efficacy of dezocine. Studies showed that the analgesic effect of dezocine is stronger than that of morphine.10 Zhao et al and Jiao et al believed it is relevant that dezocine can effectively reduce sensitivity to pain caused by painful stimuli.8,11 In addition, wake-up time and orientation force recovery time were shorter in the intervention group than in the control group, and the incidence of adverse reactions was also lower in the intervention group. Respiratory cycle monitoring conditions in the intervention group were relatively good compared with those in the control group during the procedure, indicating that the adverse stress response of patients in the intervention group was less than that in the control group. Dezocine was found to have less potential for producing bronchoconstriction and respiratory depression.12 It can also induce smooth muscle relaxation and reduce side effects, such as nausea and vomiting.8,12
A recent study has demonstrated that dezocine is actually a κ-receptor antagonist rather than a κ-receptor agonist,3 and future studies are warranted. Our results show that dezocine has a good anesthetic effect with little influence on the circulatory and respiratory systems.
Conclusion
Our study further confirms that the use of dezocine as an anesthetic in induced abortion is safe and effective in pain reduction, causing few adverse reactions.
Disclosure
The authors report no conflicts of interest in this work.
References
Qianchen W, Xiuzhi Y. [Analysis on painless abortion of 200 cases]. Journal of Regional Anatomy and Operative Surgery. 2010;5:373–376. Chinese. | ||
Cunxue L. [Analgesia methods in the application of the induced abortion operation]. Guide of China Medicine. 2013;9:449–450. Chinese. | ||
Wei L, Caixia L, Jun T. [Effect observation of dezocine combined with propofol in painless abortion]. Chinese Journal of Clinical Rational Drug Use. 2013;9:40–42. Chinese. | ||
Yaomin Z, Guixia J, Wei Y. Preoperative administration of intramuscular dezocine reduces postoperative pain for laparoscopic cholecystectomy. J Biomed Res. 2011;25:356–361. | ||
Liu R, Huang XP, Yeliseev A, Xi J, Roth BL. Novel molecular targets of dezocine and their clinical implications. Anesthesiology. 2014;120:714–723. | ||
Wang C, Li L, Shen B, et al. A multicenter randomized double-blind prospective study of the postoperative patient controlled intravenous analgesia effects of dezocine in elderly patients. Int J Clin Exp Med. 2014;7:530–539. | ||
Wei P, Jinghong X, Jianan D. [Effect observation of dezocine combined with propofol in painless gastrointestinal endoscopy of the middle and old aged]. Modern Digestion and Intervention. 2014;1:60–61. Chinese. | ||
Zhao J, Huang L, Hu X. [Research on efficacy, and safety of dezocine combined with propofol in painless abortion]. Journal of Hainan Medical University. 2013;8:1156–1158. Chinese. | ||
Vallely LM, Homiehombo P, Kelly-Hanku A, Kumbia A, Mola GD, Whittaker A. Hospital admission following induced abortion in Eastern Highlands Province, Papua New Guinea – a descriptive study. PLoS One. 2014;9:e110791. | ||
Zhu Y, Jing G, Yuan W. Preoperative administration of intramuscular dezocine reduces postoperative pain for laparoscopic cholecystectomy. J Biomed Res. 2011;25:356–361. | ||
Jiao L, Liu R. [Comparison of pharyngalgia after general anesthesia tracheal intubation-maxillofacial surgery between dezocine and flurbiprofen axetil]. J Beijing Da Xue Xue Bao. 2014;1:104–106. Chinese. | ||
Renjun X, Ailan L, Jianying Y, et al. [Clinical research of continuous analgesia out of dura mater by dezocine combined with sufentanil and ropivacaine]. Hebei Medical Journal. 2013;2:189–191. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.