Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 16
Determinants of Loss to Follow Up Among Adult People Living with HIV Enrolled in Antiretroviral Therapy in West Wollega Public Hospitals, Oromia, Ethiopia
Authors Benti Biratu S, Addis Gesese A
Received 7 July 2023
Accepted for publication 1 February 2024
Published 26 February 2024 Volume 2024:16 Pages 59—71
DOI https://doi.org/10.2147/HIV.S426196
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Olubunmi Akindele Ogunrin
Siraj Benti Biratu,1 Abreha Addis Gesese2
1Department of Public Health, College of Medicine and Health Sciences, Ambo University, Ambo, Ethiopia; 2Department of Clinical Nursing, Gambella Teachers Education and Health Science College, Gambella, Ethiopia
Correspondence: Abreha Addis Gesese, Email [email protected]
Background: Antiretroviral Treatment (ART) reduces morbidity and mortality in patients with human immunodeficiency virus (HIV). However, clients loss to follow-up (LTFU) from the treatment poses a paramount problem to the public, healthcare, and patient outcome. Thus, this study identified determinants of loss to follow-up to ART among adult clients in West Wollega hospitals, Oromia, Ethiopia, in 2021.
Methods: An unmatched case-control study was conducted and a systematic random sampling technique was used. Data were collected from patient charts by three BSC nurses and three card reporters using a structured checklist. Then, it was entered into Epi-data version 3.1 and analyzed using SPSS version 21. Descriptive statistics (frequency and percentage) were used to present the results. Bivariate and multivariable logistic regression analyses were performed using the backward stepwise method. Adjusted odds ratio (AOR) and p-values < 0.05 were used to declare significant association with loss to follow-up. Model fitness was checked using Hosmer-Lemeshow goodness-of-fit.
Results: A total of 399 (133 patients and 266 controls) participated in this study. Rural residents (AOR:3.46, 95% CI:1.65, 7.25), male patient (AOR: 2.65 95% CI 1.54,4.55), lack of formal education (AOR: 4.35, 95% CI 1.53, 12.41), base line CD4 ≤ 350 (AOR: 5.25, 95% CI 1.93,14.24), poor functional status (AOR: 4.298, 95% CI 5.33,34.62) and WHO stages III & IV (AOR: 2.65, 95% CI 1.68,4.19), and tuberculosis co-infection (AOR: 2.82, 95% CI 1.11,7.45) were determinant factors of loss to follow up.
Conclusion: Rural residence, male sex, daily laborer, no formal education, baseline CD4 count < 350 cells/mm3, baseline advanced WHO clinical stage, and TB co-infection were determinants of LTFU. Therefore, emphasis should be given to the identified factors along with awareness creation and health education sessions. Regular TB screening, optimal adherence regardless of their stay on ART, and follow-up study are recommended.
Keywords: ART, loss to follow-up, adults, determinants, People Living with HIV, West Ethiopia
Background
The continuous spread of HIV, which has already claimed 40.1 million lives worldwide, is a serious public health concern, with some nations reporting rising trends in new infections after years of reduction.1 In 2022, 630,000 (480 000–880 000) people died from HIV-related causes and 1.3 million (1.0–1.7 million) people acquired HIV. There were an estimated 39.0 million (33.1–45.7 million) people living with HIV at the end of 2022, two thirds of whom (25.6 million) are in the WHO African Region.2 In Ethiopia, the countrywide People Living with HIV (PLHIV) estimate as of 2021 is 616,105 with little distinction between urban and rural people. The Gambella region continues to have the highest HIV incidence; women aged 20 to 39 had a substantially higher prevalence (6.1–9.1%) than men (0.9–2.4%) and had the highest frequency among adult males between 40–44 age group (accounting for 5.7%).3
HIV has been transformed from a death sentence to a chronic manageable disease due to the introduction of ART.4 The Universal scale-up of ART has brought significant gains for millions of people and a reduction in new infections and HIV-associated morbidity and mortality.5 Of the UNAIDS Launch of 95–95−95 treatment target by 2030, 79% had access to ART, of which, 83% were virally suppressed, contributing to a 29% reduction in new HIV Infections between 2010–2016.6,7 According to the latest estimate, there was a need for ART in 2017 for 551,630 adults and 62,194 children under the age of 15 years in Ethiopia. ART coverage for people over the age of 15 has reached 75%, but the coverage remains low (34%) for children.8
LTFU is a significant obstacle to the success of ART programs in settings with limited resources.9 Mortality and undocumented transfers were substantial among LTFU patients in sub-Saharan Africa.10 During the test and treatment era, the risk of loss to follow-up increased with time and was higher among patients who started ART within seven days of HIV diagnosis.11 Loss to follow-up is a term used to categorize patients no longer being seen in a chronic HIV care treatment program. It’s defined as not taking ART replenishment for last 90 days or more from last attendance for refill, but not classified as dead or transferred out,12 nor had a patient not returned to clinic for 6 months.13 Undocumented transfers should not be considered as LTFU because the clients are receiving treatment elsewhere. With high rates of LTFU, missed appointments, and ART program termination, it is difficult to meet the global 95–95-95 target to attain HIV free generation and HIV epidemic control in 2030. LTFU increases the risk of HIV viral load, AIDS-defining and non-AIDS-defining complications, and mortality,13,14 while also lowering immunological function and overall quality of life. It likely increases in patient loads and its attendant pressure on health care providers to support patient counseling.15 According to research conducted in sub-Saharan Africa, ART resistance has been a prevalent issue for people with HIV/AIDS (PLWHIA) because of LTFU, rising ART dropout rates,16 treatment fatigue caused by prolonged treatment durations, and financial consequences as a result of drug resistance and development of new drugs.17 LTFU remains difficult for HIV patients despite the major impact of ART, with varying prevalence across different countries: 36.6% in Cameroon,18 16% among women in Uganda,19 24% in Nigeria.20
Despite the disparities in the prevalence and high rates of LTFU across studies in Ethiopia, which ranges from 11.5–26.7%,12,16,20–22 there is limited evidence on the determinants of lost to follow-up among PLHIV in the study area. Determining the causes of anti-retroviral therapy LTFU is essential to achieve high treatment success rates, reduce viral load, prevent drug resistance, and prevent national financial instability. This will also assist program designers and other stakeholders in preventing the causes of ART LTFU. Thus, this study identified determinants of loss to follow-up of ART that would help in the management of PLHIV in West Wollega, Oromia, and Ethiopia in 2021.
Methods and Materials
Study Design, Area and Study Period
A hospital-based unmatched case-control study was conducted among ART patients in Gimbi, Nedjo, and Begi Hospitals, West Wollega Oromia, Ethiopia, between January 7–20-2021. West Wollega is one of the West Zones of the Oromia Region, which is bordered by West Kelem Wollega in the North, Benishangul Gumuz region in the East and Wollega in East and Illubabor Zone in the Southeast. The zone has an estimated total population of 1,351,979, of which 50.46% are females. The three Public Hospitals are located in Gimbi, Najjo, and Begi towns at distances of 441, 515, and 721 Kms, from Addis Ababa, the capital city of Ethiopia. Begi Hospital serves as the district hospital, with the Gimbi and Nedjo Hospitals acting as general hospitals for the town and nearby healthcare institutions. The West Wollega zone administration has three governmental hospitals, two Non-Governmental Organization (NGO) hospitals, 81 health clinics, and 533 health posts. 209 medical professionals and 176 administrative and support staff members among the approximately 2192 healthcare professionals and 607 administrative and support staff members. They typically see 104,000 clients per year and have 167 beds each. Currently, they offer comprehensive ART services to PLHIV.14
Population
All adult PLHIV (aged >15 years) who had been taking ART with a documented history of ART follow-up from March, 1/2018 to January 7/2021 were the source population for this study. Sampled cases and controls who had a documented history of ART follow-up in individual patient charts from March, 1/2018 to January 7/2021 were included in the study.
Cases: HIV-infected adults were aged >15 years old PLHIV, had a documented ART loss to follow-up and not taking ART refill for 3 months or longer from the last attendance for a refill and not yet classified as “dead” or “transferred-out” from March, 1/2018 to January 7/2021.
Controls: HIV-infected adults > 15 years of age and who had a documented history of ART follow-up and who were on regular ART follow-up from March, 1/2018 to January 7/2021.
Inclusion Criteria
For cases: All HIV-infected adults were aged >15 years old ART patient, had a documented history of ART loss to follow-up and not taking ART refill for 3 months or longer from the last attendance for a refill and not yet classified as “dead” or transferred-out from March, 1/2018 to January 7/2021.
For control: All HIV-infected adults aged >15 years received ART, with a documented history of ART follow-up and regular ART follow-up.
Sample Size Determination, Sampling Technique and Procedure
Sample size was determined by using Epi Info version 3.1 by taking main predictor of loss to follow up to first line ART was Baseline CD4, from a previous study that considered the proportion of CD4 <350 were 77.9% and 66.8% among cases and controls, respectively. Case to Control ratio was 1:2, therefore, the sample size was 399 (133 cases and 266 controls).14
The study participants were PLHIV with registered ART cards, who were being treated at one of the three purposely chosen government hospitals in the West Wollega zone (Gimbi, Nedjo, and Begi). After determining the number of PLHIV in each hospital over the course of three years, the number of study subjects for each institution was distributed equally. As there were 2394 cases and controls on the list of hospitalized PLHIV from the ART follow-up form, the K value was computed as follows: K for cases = 682/133= 5.127 = 5 and for controls = 1712/266=6.436 = 6. Systematic random sampling technique was used to extract data by considering a subsequent sample used to replace the incomplete samples.
Variables of the Study
Dependent Variable
Loss to follow up of ART.
Independent Variables
Socio-demographic variables include age, sex, residence (urban/rural), marital status, religion, education level, occupation, and disclosure HIV status. Clinical variables include baseline CD4 count, current CD4 count, WHO clinical staging, baseline BMI, current BMI, history of TB, duration of HIV infection, baseline hemoglobin level, and functional status (ambulatory/working/bedridden). Behavior-related factors include chewing khat, alcohol use, and smoking. ART medication-related variables included adherence to treatment (good/fair/poor), line ART regimen, regimen change, ART duration, and cotrimoxazole prophylaxis use.
Operational Definitions
Loss to follow up: not taking ART refill for 3 months or longer from the last attendance for a refill and not yet classified as “dead” or “transferred-out”.
Adult : greater than 15 years old.
Baseline CD4 count: CD4 at the time of ART initiation.
Current CD4 count: most recent CD4 count at the time when the study was conducted.
Drop: Patients missing their appointment for drug pick up for more than 3 months.
Stop: Patients who remained on chronic HIV care but discontinued ART for various reasons.
Transferred out: Those patients who are transferred to other health care facilities.
Functional Status
Working: Able to perform usual work in or out of the house.
Ambulatory patient: Able to perform activities of daily living.
Bedridden: Not able to perform activities of daily living.
Adult First line regimen: Contain one of the following regimen; TDF + 3TC + DTG (FDC)* OR TDF + 3TC + EFV (FDC)** AZT + 3TC + EFV AZT + 3TC + NVP TDF + 3TC + NVP.14
Data Collection Tools and Techniques
A standardized checklist developed from the intake and follow-up form for the ART clinic at the Ethiopian Federal Ministry of Health and other relevant findings8,11,12 was used to retrieve data from the patient charts. Three BSC nurses working in the OPD gathered the data, and three card reporters were used to deliver cards from the card room. The investigator and supervisor supervised the entire data collection process daily.
Data Quality Control
The following steps were followed to ensure the accuracy of the data gathered by three nurses working in the OPD and three card reporters. Additionally, during the data extraction period, daily supervision by supervisors and investigators was conducted, and data collectors received one day of training to assess the accuracy of the data. After data extraction, the consistency and completeness of each questionnaire was reviewed.
Data Processing and Analysis
Data were cleaned, coded, and entered into Epi Info data version 3.1 before being examined using SPSS version 21. Data were reviewed for completeness. Patient demographic, clinical, and medication-related variables were described using descriptive statistics such as frequencies and percentages. Bivariate logistic regression analysis was applied to variables with a p-value of less than 0.25. To reduce confounding variables, the backward stepwise elimination method was used to fit the multivariable model to determine the independent predictors of loss to follow-up with ART. Adjusted Odds Ratio (AOR) and p-values <0.05 were used to declare statistical significance with the outcome variable. Finally, Hosmer-Lemeshow goodness-of-fit tests were used to evaluate the model’s fitness.
Result
Socio-Demographic Characteristics of Participants
A total of 399 PLHIV (133 clients and 266 controls) who received ART were included in this study. Of these participants, 170 (47.4%) were males and 229 (52.6%) were females. The median age at participant enrollment for cases was 32 years (IQR, 16–48 years), while the median age for controls was 31 years (IQR, 15–47 years). At the time of ART enrollment 63 (47.4%) cases and 98 (36.8%) controls were between the ages 25–34 years. Less than 25% of the case participants, 11 (8.3%), and 52 (19.5%) of the controls were above the age than 45 years.
Regarding residence of clients, 105 (78.9%) cases and 119 (44.7%) controls live in rural areas. Regarding marital status, 67 (50.4%) cases and 80 (30.1%) controls were single, compared to 46 (34.6%) cases and 129 (48.5) controls married. Fifty six (42.1%) cases and 92 (34.6%) controls were Protestants in religion. Regarding educational status, 78 (58.6%) cases and 23 (8.6%) controls were with informal education. The majority (62.4%) of cases and 12 controls (4.5%) were daily laborers in occupation. Finally, 25.6% cases and 52.3% controls disclosed their HIV Sero status to a family member, partner, or anyone else (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Loss to Follow Up Among Adult People Living with HIV Enrolled in Antiretroviral Therapy in West Wollega Public Hospitals, Oromia, Ethiopia 2021 |
Behavioral Related Factors of Clients on ART Loss to Follow Up
Out of all individuals, 47 (35.3%) cases and 84 (31.6%) controls had a history of alcohol use, 42 (31.5%) cases and 182 (68.4%) controls had a history of smoking, and 53 (39.8%) cases and 76 (28.6%) controls had a history of chewing khat (Table 2).
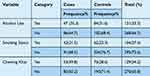 |
Table 2 Behavioral Related Factors of Loss to Follow Up Among Adult People Living with HIV Enrolled in Antiretroviral Therapy in West Wollega Public Hospitals, Oromia, Ethiopia 2021 |
Clinical Related Characteristics of Participants on ART Loss to Follow Up
Concerning the clinical characteristics of participants, 39 (29.3%) the cases and six (2.3%) controls were ambulatory, whereas four (3.5%) of the clients and 10 (7.5%) of the controls were bedridden in functional status. Regarding the participants’ current WHO clinical stage, 37 (27.8%) cases and 136 (51.1%) controls were stage I and stage II. Of the clients in this study, 70 (52.6%) cases and 25 (9.4%) controls were less than 18.5 kg/m2 in their BMI.
At the time ART was started, the Baseline CD4 count was <350 cells/mm3 in 89 (66.9%) clients and 50 (18.8%) controls. Ninety (67.7%) clients and 43 (32.3%) controls had a history of TB co-infection, and 114 cases (85%) and 76 controls (28.6%) had a history of substance use (Table 3).
 |
Table 3 Clinical Related Characteristics on Loss to Follow Up Among Adult People Living with HIV Enrolled in Antiretroviral Therapy in West Wollega Public Hospitals, Oromia, Ethiopia 2021 |
At the time ART was started, the baseline CD4 count was <350 cells/mm3 in 89 (66.9%) clients and 50 (18.8%) controls. Ninety clients (67.7%) and 43 controls (32.3%) had a history of TB co-infection, and 114 cases (85%) and 76 controls (28.6%) had a history of substance use (Table 3).
Anti-Retroviral Treatment Related Factors of Patients on ART
Cotrimoxazole was used as a preventative agent in 41 cases and 73 controls; 130 cases and 119 controls had a history of adverse medication reactions. Seventy-two (54.1%) of the cases and 15 (5.6%) of the controls received ART for more than 120 months (Table 4).
 |
Table 4 ART Related Factors of Loss to Follow up Among Adult People Living with HIV Enrolled in Antiretroviral Therapy in West Wollega Public Hospitals, Oromia, Ethiopia 2021 |
Determinants of Loss to Follow Up of ART Among Adult People Living with HIV
In the bivariate logistic regression, sex, marital status, residence area, occupational status, educational status, smoking history, substance use, baseline functional status, baseline WHO clinical stage, baseline body mass index, baseline CD4 count, history of TB co-infection, first-line ART regimen, HIV sero status disclosure, baseline hemoglobin, baseline functional status of the patient, adherence status, disclosure status, history of drug side effects, and duration of first-line ART were possible candidates for multivariable logistic regression analysis at P-value <0.25. Finally, rural residence, male sex, no formal education, duration of ART, stage III and IV baseline WHO clinical stage of HIV, baseline CD4 count <350cells/mm3, having history of TB co-infection, and poor adherence to antiretroviral drugs were associated with loss to follow-up at p<0.05 (Table 5).
Discussions
Based on the 95:95:95 target on the potential implications on HIV program and epidemic control, 86% [73>–98%] of all people living with HIV knew their status, 76% [65–89%] were receiving antiretroviral therapy and 71% [60–83%] had suppressed viral loads. With this in mind, early access to ART and support to remain on treatment is therefore critical not only to improve the health of people with HIV but also to prevent HIV transmission.6 Ethiopia focuses on training and upgrading of frontline, low and mid-level health workers that will staff primary health facilities. In line with this, appropriate HIV care and ART training, strong follow-up and effective clinical mentorship should continue.8 To ensure the consistency and maintain the quality of HIV care and ART services at all levels, knowing determinants of loss to follow up is significant. Thus, this study found that rural residence, male sex, no formal education, duration of ART, stage III and IV baseline WHO clinical stage of HIV, baseline CD4 count <350cells/mm3, having history of TB co-infection, and poor adherence to antiretroviral drugs were associated with loss to follow-up among PLHIV.
Adult clients on first line ART in rural resident were 3.46 times more likely to be lost to follow up to the first line anti-retro viral therapy compared to adult ART patients in urban resident. This is in line with research conducted in Arba Minch General Hospital, Southern Ethiopia,12 in the Oromia area of Ethiopia,14 Northwest Ethiopia,22 and in Lilongwe, Malawi.23 This variance might be as a result of a number of factors, including accessibility and cost of transportation to and from the ART clinic, low level of client awareness of treatment, and risk related to the adherence of treatment and societal stigma related to a disease HIV/AIDS. Urban residents are more prone to self-referral to other health care facilities and not permanently live in the area, relatively. This might contribute to the lower rate of loss to follow-up for this study.
This study identified that males were almost twice as likely to be lost to follow-up with antiretroviral treatment when compared with females. This finding is similar to that in Northwest Ethiopia, in Lilongwe, Malawi, and rural Tanzania, where men were more likely to be lost to follow-up from ART.12,16,23,24 The proportion LTF was 8.2% at 12 months following enrollment, and was higher among women (8.4%) than men (7.1%).25 The possible reason might be due to the fact that women tend to get HIV care during and after pregnancy that plays crucial role for ART retention. Meanwhile, men are more likely exposed to substance use such as alcohol and khat that hinders them not to follow their ART care.21 Despite the higher odds of attrition in men, a study conducted in Central Kenya had a proportionately higher number of women. Which shows that a greater proportion of men than women were unaware of their HIV infection. Men may therefore have presented to HIV clinics with advanced HIV infection.26
Daily workers had a follow-up loss rate that was approximately nine times higher than that of their counter responders. Unemployment and lack of a fixed address were mentioned as additional factors in a study conducted in the Oromia Region that led to loss of follow-up in ART. Some patients relocated in pursuit of employment to different cities, nearby areas, and foreign countries. Some patients lack a fixed residence and are prostitutes who frequently switch which hotels they work in, and even move across towns. This may result in a lack of treatment follow-up.14 This may also result from a shortage of funds for necessary expenses such as food and transportation. Joblessness or unemployment may also represent markers of more advanced illness.21
According to a study conducted in Uganda, clients with low literacy levels could find it challenging to understand text messages serving as reminders, as well as a few other information education communications (IEC) products found in medical facilities that emphasize the importance of ongoing treatment.11 This is evidenced by this study that no formal education is associated with higher risk of lost to follow up. This is because those people who are uneducated may have difficulty understanding instructions and may not recognize the importance of ART drug adherence and complications related to discontinuation of ART drugs.
According to the study findings, clients with low baseline CD4 counts (350cells/mm3) were five times more likely than clients with baseline CD4 counts greater than 350cells/mm3 to lose to follow-up with first-line antiviral treatment. Studies conducted in Uganda, Northwest Ethiopia, Oromia, and the University of Gondar Comprehensive Specialized Hospital Northwest Ethiopia are analogous to this conclusion.11,12,14,21 Low immunity resulting from a low baseline CD4 cell count may be the cause, which may encourage the development of opportunistic infections and result in missed follow-up appointments.
Participants with poor functional status had a 4.3 times higher chance of being lost to follow-up. A study conducted in a comprehensive specialty hospital affiliated with the University of Gondar in Northwest Ethiopia revealed that ambulatory clients were at a risk of being lost to follow-up.21 Clients on ART with poor functional status who are ambulatory may have more advanced stages of illness, which increases the risk of losing track. The social, economic, and financial consequences of their incapacity to work may explain why ambulatory patients are more likely to experience LTFU. This could have an impact on hospital stay.
According to this study, PLHIV who had been on ART for at least 40 months and between 80 and 119 months had a decreased probability of being lost to follow-up. In Uganda, the cumulative incidence of LTFU increased with duration of follow up from 8.9% (95% CI, 8.2–9.6%) at 6 months to 20.2% (95% CI, 19.0–21.4%) at 48 months.11 In Tanzania shorter ART duration was linked to loss from follow up.24
When compared to stage I and stage II baseline WHO clinical stages, advanced WHO clinical stages III and IV at the time of ART commencement were more likely to develop loss to follow-up with antiretroviral medication which shows consistency with studies conducted elsewhere.6,8,11,14,22,24 This may be because the responses of PLHIV to antiretroviral treatment may be significantly affected by the high viral load and low CD4 cell count associated with advanced WHO clinical stages of HIV illness, which weaken immunity.
Clients with a history of TB co-infection were more likely to be lost to follow-up to antiretroviral treatment when compared to patients with no history of TB co-infection. According to research conducted in the Sheka Zone, Ethiopia, and sub-Saharan Africa, opportunistic infections, particularly pulmonary tuberculosis, cause ART to be lost to follow-up. This could be due to the emergence of tuberculosis while receiving antiretroviral therapy, which has a number of negative effects, including pill burden and drug-drug interactions that could result in the failure of first-line therapy and loss to follow-up.27,28
A study conducted in Gonder revealed that underweight patients were found to be at higher risk of LTFU. The possible reason as stated by a qualitative study could be many participants who cannot eat regularly, malnourished, drop out of care because of believing that “medication without proper food is ineffective or even harmful”.21 Unlikely this study found that individuals with a baseline BMI of 18.5 km/m2 and above were more likely to be lost to follow-up. This finding is comparable to those of previous studies.23,24,26 Lack of regular access to food, malnutrition, and weight loss due to interruption of care may be the causes.
Compared with their counterparts, clients who did not disclose their HIV/AIDS status had a 3.28 higher likelihood of leaving the treatment program. A study conducted in Kongo revealed that patients who did not share their HIV status had 2.28 times a higher hazard of being LTFU.29 Likely, this is supported by the findings of a study conducted at Karamara Hospital in Jigjiga, Eastern Ethiopia that loss to follow-up has also been linked to HIV disclosure.30 Clients may stick to their treatment significantly more if they disclose their status because adherence to ART treatment requires extensive support and care from various members of the community. Unavailability and incomplete registration of ART follow-up cards and ART clinic intake forms were limitations of this study.
Conclusion and Recommendation
This study found that rural residents, male sex, no formal education, duration of ART, stage III and IV baseline WHO clinical stage of HIV, baseline CD4 count <350cells/mm3, having history of TB co-infection, and poor adherence to antiretroviral drugs were associated with loss to follow-up in this study setting.
Therefore, the hospitals together with concerned bodies should pay more attention to clients on ART with a baseline advanced stage of HIV, baseline CD4<350cells/mm3 and TB co-infection. Health care professionals should create awareness and provide health education sessions for clients from rural residences and those with malnutrition cases. Regular screening of TB co-infection including other prevention and control measures should be strengthened. PLHIV on ART should be encouraged on optimal adherence to the medication regardless of their stay on ART. Further follow-up studies are required to identify determinants of lost to follow up among PLHIV focusing on multi-centered hospital studies.
Abbreviations
AIDS, Acquired Immuno Deficiency Syndrome; AOR, Adjusted Odds Ratio; ART Antiretroviral Treatment; BMI, Body Mass Index; BSC, Bachelor of Science; CD4, Cluster Differentiation 4; CI, Confidence Interval; CPT, Cotrimoxazole Preventive Therapy; EFV, Efavirenz; ETB, Ethiopian Birr; FMOH, Federal Ministry of Health; LTFU, Loss to follow up; NNRTI, Non-Nucleoside Reverse Transcriptase Inhibitors; NRTI, Nucleoside Reverse Transcriptase Inhibitors; OIS, Opportunistic Infections; OPD, Out Patient Department; PEPFAR, President Bush’s Emergency Plan for AIDS Relief; PLWHA, People Living With HIV/AIDS; RNA, Ribonucleic Acid; SPSS, Statistical Packages for social science; TB, Tuberculosis; TDF, Tenofovir; TO, Transfer Out; UNAIDS, United nation’s program on HIV/AIDS; WHO, World Health Organization and 3TC, Lamivudine.
Data Sharing Statement
The datasets analyzed in the current study have been included in the manuscript.
Ethical Considerations
Ethical clearance and approval for this study were obtained from the Research and Ethical Review Committee of the College of Medicine and Health Science, Ambo University. Permission to carry out this research was obtained from the hospital medical Director and ART focal person of each hospital before the data extraction. For all participants under the age of 18 years, parental/legal guardian informed consent was obtained. All other participants also provided informed consent. To maintain confidentiality, all collected data were coded and locked in a separate place and were used only for research purposes. Ethical considerations were also considered in to account throughout this study and complies with the Declaration of Helsinki.
Acknowledgments
First, we would like to express our deepest appreciation and sincere gratitude to the advisors, Mr. Habtamu Oljira and Dr. Magarsa Nagasa, for their unreserved advice and provision of relevant and timely comments and guidance on the overall research process from proposal development to final thesis writing, as well as data collectors and supervisors for their commitment and cooperation.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing e article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was not financially supported.
Disclosure
The authors declare that they have no competing interests for this work.
References
1. UNAIDS. UNAIDS fact sheet on the latest global and regional statistics on the status of the AIDS epidemic 1. Communications and Global Advocacy. [email protected] UNAIDS 2022 estimates and additional data are available at aidsinfo.unaids.org; 2022.
2. WHO fact sheet. HIV and AIDS. Available from: https://www.who.int/news-room/fact-sheets/detail/hiv-aids.
3. PEPFAR. Ethiopia country operational plan COP 2021 strategic direction summary. Available from: https://www.state.gov/wp-content/uploads/2021/09/Ethiopia_SDS_Final-Public_Aug-11-2021.pdf.
4. Johanna Harvey world AIDS Day 2017: aging with HIV. Available from: https://www.pennmedicine.org/news/news-blog/2017/november/world-aids-day-2017-aging-with-hiv.
5. De La Mata NL, Nguyen KV, Merati TP, et al. Trends in CD4 cell count response to first-line antiretroviral treatment in HIV-positive patients from Asia, 2003–2013: TREAT Asia HIV observational database low intensity transfer. Int J STD AIDS. 2017;28(13):1282–1291. PMID: 28632481; PMCID: PMC5805469. doi:10.1177/0956462417699538
6. Joint United Nations Programme on HIV/AIDS. Fast-Track: accelerating action to end the AIDS epidemic by, 2030 June 2015. Available from: https://www.unaids.org/sites/default/files/media_asset/201506_JC2743_Understanding_FastTrack_en.pdf.
7. Tiruneh YM, Galárraga O, Genberg B, Wilson IB. Retention in Care among HIV-Infected Adults in Ethiopia, 2005–2011: a mixed-methods study. PLoS One. 2016;11(6):e0156619. PMID: 27272890; PMCID: PMC4896473. doi:10.1371/journal.pone.0156619
8. FDRE/MOH. National guidelines for comprehensive hiv prevention, care and treatment; 2018. Available from: https://www.afro.who.int/publications/national-consolidated-guidelines-comprehensive-hiv-prevention-care-and-treatment.
9. Geng EH, Bangsberg DR, Musinguzi N, et al. Understanding reasons for and outcomes of patients lost to follow-up in antiretroviral therapy programs in Africa through a sampling-based approach. J Acquir Immune Defic Syndr. 2010;53(3):405–411.
10. Chammartin F, Zürcher K, Keiser O, et al. Outcomes of patients lost to follow-up in African antiretroviral therapy programs: individual patient data meta-analysis. Clinl Infect Dis. 2018;67(11):1643–1652. doi:10.1093/cid/ciy347
11. Kiwanuka J, Mukulu Waila J, Muhindo Kahungu M, Kitonsa J, Kiwanuka N, Fokam J. Determinants of loss to follow-up among HIV positive patients receiving antiretroviral therapy in a test and treat setting: a retrospective cohort study in Masaka, Uganda. PLoS One. 2020;15(4):e0217606. doi:10.1371/journal.pone.0217606
12. Gebremichael MA, Gurara MK, Weldehawaryat HN, Mengesha MM, Berbada DA. Predictors of loss to follow-up among hiv-infected adults after initiation of the first-line antiretroviral therapy at arba minch general hospital, southern Ethiopia: a 5-year retrospective cohort study. Biomed Res Int. 2021;2021:12. doi:10.1155/2021/8659372
13. Geng EH, Bangsberg DR, Musinguzi N, et al. Understanding reasons for and outcomes of patients lost to follow-up in antiretroviral therapy programs in Africa through a sampling-based approach. J Acquir Immune Defic Syndr. 2010;53(3):405–411. PMID: 19745753; PMCID: PMC3606953. doi:10.1097/QAI.0b013e3181b843f0
14. Megerso A, Garoma S, Eticha T, et al. Predictors of loss to follow-up in antiretroviral treatment for adult patients in the Oromia region, Ethiopia. HIV AIDS. 2016;8:83–92. PMID: 27175095; PMCID: PMC4854271. doi:10.2147/HIV.S98137
15. Opio D, Semitala FC, Kakeeto A, et al. Loss to follow-up and associated factors among adult people living with HIV at public health facilities in Wakiso district, Uganda: a retrospective cohort study. BMC Health Serv Res. 2019;19:628. doi:10.1186/s12913-019-4474-6
16. Mugisha V, Teasdale CA, Wang C, et al. Determinants of Mortality and Loss to Follow-Up among Adults Enrolled in HIV Care Services in Rwanda. PLoS One. 2014;9(1):e85774. doi:10.1371/journal.pone.0085774
17. World Health Organization. Global action plan on hiv drug resistance 2017-2021. HIV and Drug Resistance; 2021. Available from: https://apps.who.int/iris/rest/bitstreams/1086607/retrieve.
18. Bekolo CE, Webster J, Batenganya M, et al. Trends in mortality and loss to follow-up in HIV care at the Nkongsamba Regional hospital, Cameroon. BMC Res Notes. 2013;6:512. doi:10.1186/1756-0500-6-512
19. Kamacooko O, Mayanja Y, Bagiire D, et al. Predictors of lost to follow-up in a “test and treat” programme among adult women with high-risk sexual behavior in Kampala, Uganda. BMC Public Health. 2020;20:353. doi:10.1186/s12889-020-8439-9
20. Bello SO, Abolodje E, Audu ES, Ikrama HI, Kelechi IM. The pattern of loss to follow-up among HIV – infected clients in a tertiary health facility in North Central Nigeria. Sri Lanka J Child Health. 2020;49(2):170–174.
21. Mekonnen N, Abdulkadir M, Shumetie E, Baraki AG, Yenit MK. Incidence and predictors of loss to follow-up among HIV infected adults after initiation of first line anti-retroviral therapy at University of Gondar comprehensive specialized Hospital Northwest Ethiopia, 2018: retrospective follow up study. BMC Res Notes. 2019;12(1):111. PMID: 30819236; PMCID: PMC6396485. doi:10.1186/s13104-019-4154-y
22. Birhanu MY, Leshargie CT, Alebel A, et al. Incidence and predictors of loss to follow-up among HIV-positive adults in northwest Ethiopia: a retrospective cohort study. Trop Med Health. 2020;48:78. doi:10.1186/s41182-020-00266-z
23. Tweya H, Oboho IK, Gugsa ST, Phiri S, Rambiki E, Banda R. Loss to follow-up before and after initiation of antiretroviral therapy in HIV facilities in Lilongwe, Malawi. PLoS One. 2018;13. doi:10.1371/journal.pone.0188488
24. Kalinjuma AV, Glass TR, Weisser M, et al.; KIULARCO Study Group. Prospective assessment of loss to follow-up: incidence and associated factors in a cohort of HIV-positive adults in rural Tanzania. J Int AIDS Soc. 2020;23(3):e25460. PMID: 32128998; PMCID: PMC7054631. doi:10.1002/jia2.25460
25. Gwynn RC, Fawzy A, Viho I, Wu Y, Abrams EJ, Nash D. Risk factors for loss to follow-up prior to ART initiation among patients enrolling in HIV care with CD4 + cell count ≥ 200 cells/μ L in the multi-country MTCT-Plus Initiative. BMC Health Serv Res. 2015;1–10. doi:10.1186/s12913-015-0898-9
26. Wekesa P, McLigeyo A, Owuor K, Mwangi J, Nganga E, Masamaro K. Factors associated with 36-month loss to follow-up and mortality outcomes among HIV-infected adults on antiretroviral therapy in Central Kenya. BMC Public Health. 2020;20(1):328. PMID: 32171279; PMCID: PMC7071670. doi:10.1186/s12889-020-8426-1
27. Shaweno T, Getnet M, Fikru C. Does time to loss to follow-up differ among adult tuberculosis patients initiated on tuberculosis treatment and care between general hospital and health centers? A retrospective cohort study. Trop Med Health. 2020;48:9. doi:10.1186/s41182-020-00198-8
28. Kebede HK, Mwanri L, Ward P, et al. Predictors of lost to follow up from antiretroviral therapy among adults in sub-Saharan Africa: a systematic review and meta-analysis. Infect Dis Poverty. 2021;10:33. doi:10.1186/s40249-021-00822-7
29. Akilimali PZ, Musumari PM, Kashala-Abotnes E, et al. Disclosure of HIV status and its impact on the loss in the follow-up of HIV-infected patients on potent anti-retroviral therapy programs in a (post-) conflict setting: a retrospective cohort study from Goma, Democratic Republic of Congo. PLoS One. 2017;12(2):e0171407. PMID: 28170410; PMCID: PMC5295697. doi:10.1371/journal.pone.0171407
30. Seifu W, Ali W, Meresa B. Predictors of loss to follow up among adult clients attending antiretroviral treatment at Karamara general hospital, Jigjiga town, Eastern Ethiopia, 2015: a retrospective cohort study. BMC Infect Dis. 2018;18:280. doi:10.1186/s12879-018-3188-4
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

