Back to Journals » Clinical Optometry » Volume 15
Demodex Blepharitis: A Survey-Based Approach to Investigate Knowledge, Attitudes, and Practices Among Optometrists in India
Authors Sharma N , Martin E, Pearce EI, Hagan S , Purslow C
Received 6 January 2023
Accepted for publication 3 March 2023
Published 11 April 2023 Volume 2023:15 Pages 55—64
DOI https://doi.org/10.2147/OPTO.S403837
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Mr Simon Berry
Nikhil Sharma,1 Eilidh Martin,1 Edward Ian Pearce,1 Suzanne Hagan,1 Christine Purslow2
1Department of Vision Sciences, Glasgow Caledonian University, Glasgow, Scotland, UK; 2School of Optometry and Vision Sciences, Cardiff University, Cardiff, Wales, UK
Correspondence: Edward Ian Pearce; Nikhil Sharma, Email [email protected]; [email protected]
Purpose: To investigate the knowledge, attitudes, and practice towards Demodex blepharitis among optometrists in India.
Methods: The study was conducted in the form of an online survey using Research Electronic Data Capture (REDCap). The survey link was distributed via direct e-mail and social media platforms, and it was comprised of 20 questions divided into two sections. The first section focused on the practitioners’ demographics and their views on the general health of the eyelid. The second section of the survey was specific and aimed at obtaining information on identifying and treating Demodex blepharitis, and was only completed by those respondents who looked for Demodex mites.
Results: The survey was completed by 174 optometrists. The prevalence of blepharitis in the general population was judged by the respondents to be 40%, whereas the prevalence of Demodex mites was estimated to be 29%. Interestingly, the prevalence of Demodex mites in people with blepharitis was estimated to be 30%. This estimated prevalence was substantially lower than that reported in the literature on the subject. 66% of participants believed Demodex mites to be a significant cause of ocular discomfort, whereas only 30% of participants would intervene to diagnose and manage Demodex blepharitis in their patients. Optometrists differed in their preferred method of diagnosis and management of Demodex infestation in eyelids.
Conclusion: The result of this survey suggests that Demodex blepharitis is a highly under-diagnosed condition in India, with nearly 30% of surveyed optometrists managing this condition. The study also observed a lack of awareness and consensus among surveyed optometrists with regards to diagnosis and appropriate treatment methods to control Demodex infestation in eyelids.
Keywords: demodex blepharitis, ocular surface, dry eye
Introduction
Anterior blepharitis, meibomian gland dysfunction (MGD), and dry eye disease (DED) are amongst the most common ocular surface disorders encountered in routine ophthalmic clinics.1 These conditions often co-exist with overlapping signs and symptoms and pose a significant challenge to eye care practitioners with regards to an accurate diagnosis and correct treatment methods.2,3 Eye care practitioners play a critical role in managing these ocular surface disorders. To provide high-quality eye care, clinicians must be familiar with the detection, diagnosis, and management of these ocular surface disorders to provide targeted treatment and appropriate symptomatic relief to their patients.4 The pathological mechanisms behind Demodex blepharitis are poorly understood and the effectiveness of commercially available treatment products have been debated in the literature.5,6 Demodex mites have been associated with the development of chronic blepharitis.7 Despite Demodex prevalence reaching upto 100% in elderly individuals, Demodex blepharitis remains an underdiagnosed condition among eye care practitioners.8,9
A similar problem was observed in the early 1990s, when a lack of definition, classification, detection and treatment protocol for dry eye disease (DED) was a clinical challenge for eye care practitioners.10 However, the National eye institute (NEI) workshop in 1995 was the first international effort to develop a standardized classification system, clinical diagnostic tests, and appropriate treatment methods to combat dry eyes.11 Blepharitis and its sub-types have similar issues, where a globally-accepted definition and population-based studies regarding its diagnosis and management are lacking.12,13 A lack of such protocols has, in some cases, resulted in inappropriate treatment and the worsening of signs and symptoms.14,15 Moreover, studies have reported the misdiagnosis of Demodex blepharitis as sebaceous gland carcinoma, vernal keratoconjunctivitis and bacterial keratitis.15–17 Therefore, to achieve better clinical outcomes, it is highly recommended that optometrists must be aware of the role Demodex can play in causing blepharitis.18
Recent studies in the US, UK and Turkey have provided an insight on the prevalence of blepharitis and/or its subtypes.10,19,20 Such data in the south Asian region is, however, lacking. However, variable prevalence rates in epidemiological studies concerning ocular surface diseases are shown in the literature.21–23 This has been attributed to the overlap in the signs and symptoms, and inconsistent diagnostic criteria.24 India has one of the oldest national programmes for the control of blindness primarily aimed at reducing the burden of blindness.25 Demodex blepharitis remains a cause of chronic eyelid pathology and is rarely sight threatening. To the best of study team’s knowledge no study has been conducted which determines practitioners’ knowledge, attitudes, and practices towards identifying and managing Demodex blepharitis. Therefore, this study aimed to investigate the awareness of Demodex blepharitis among optometrists’ in India, their perception of the prevalence, knowledge of clinical examination techniques used when examining patients, and the management strategies that they employ in their practice.
Methodology
The study was conducted in the form of a cross-sectional, online survey from April 2020 to August 2020. The School of Health and Life Sciences at Glasgow Caledonian University gave ethical permission (approval code - HLS/LS/A19/039) to conduct the survey, in accordance with the tenets of the declaration of Helsinki.26 The survey adhered to General Data Protection Regulations.27 The confidentiality of the participants was strictly maintained, and all the responses were anonymous. Participation in the survey was voluntary and no incentives were provided. The link to the survey was sent via emails and social media platforms to optometrists in India, following the established guidelines by Checklist for Reporting Results of Internet E-Surveys (CHERRIES).28 Participants were recruited via email and social media platforms and were provided with an information sheet. Online implied consent meant agreeing to take part in the survey was accepted as their consent to participate.
A questionnaire was formulated by researching the recent literature and consulting an industry expert (Professor Christine Purslow). The draft questionnaire was piloted among the staff optometrists and doctoral candidates in the department of vision sciences to confirm the relevance, accuracy, and clarity of questions and to ensure questions would not be interpreted differently by the participants.
The survey was designed in Research Electronic Data Capture (REDCap, Vanderbilt University USA), Version 6.5.19, an online web application hosted at redcap.gcu.ac.uk.29,30 The survey comprised a total of 20 questions divided into two sections. The first section focused on the general health of the eyelid, associated pathology, and diagnostic techniques that optometrists followed in their practice. The second section of the survey consisted of 8 questions and was only completed by those respondents who confirmed that they routinely look for Demodex mites in their patients. This part of the survey was more specific towards identifying Demodex blepharitis, the diagnostic technique on the slit-lamp, clinical features (including signs and symptoms), confirming the presence of mites and choice and duration of treatment. A copy of the survey can be found in Appendix 1.
The Data was analysed using IBM SPSS version 26 (IBM, SPSS Inc. Chicago, IL USA). Only completed responses were analysed (174 out of 192). A Shapiro–Wilk test was conducted to check the normality of data, where appropriate. A one sample Chi-squared test was used to compare categorical data comprising of proportions. A Mann–Whitney test was used to compare data with a non-parametric distribution. The distribution across two ordinally related samples was compared using a Wilcoxon signed-rank test. To determine an association between two categorical variables, a chi square test was performed, and a Fisher’s exact test was performed where cell count was less than 5. A p-value of <0.05 was set for statistical significance. Practitioners’ demographics, place of practice, and years of qualification, were specified using descriptive statistics.
Results
A total of 174 optometrists completed the survey. Of the participants, 59.8% worked in hospitals, 8.0% worked in community practice, 18.4% were involved in academia and 13.8% worked in retail, multinational companies, and clinics. Most participants (68.4%) had less than 5 years of experience, whereas 27.6% had experience between 5–20 years and only 4% had experience of more than 20 years. When examining eyelids with a slit-lamp, 74% of participants preferred using 10x and 16x magnification. A total of 66% of participants confirmed Demodex mites to be a significant cause of ocular discomfort, while 25% remained neutral, and less than 10% disagreed. Overall, 40% of eye care practitioners reported Demodex mites to equally affect males and females, whereas 37% reported females to be more affected than males. Nearly 70% of optometrists had not receive any training in the detection and treatment of Demodex blepharitis, while the remaining optometrists (30%) reported receiving training in the form of a webinar, article, or lecture. Only 27% of respondents carried out a dry eye clinic. A total of 30% of respondents actively looked for Demodex mites in their patients.
The prevalence of blepharitis in the general population was estimated by the respondents to be 40% and the prevalence of Demodex mites in the general population was estimated to be 29%. Interestingly, the prevalence of Demodex mites in people with blepharitis was estimated to be 30% (Figure 1).
Of the participants, 66% (n = 115) believed Demodex mites to be a significant cause of ocular discomfort (X2(4); p < 0.001), but only 30% of participants (n = 53) intervened to diagnose and manage the condition. However, no association was found between practitioners carrying out dry eye clinics and investigating for Demodex mites in their patients (X2(1); p > 0.05).
Among optometrists who looked for Demodex in their patients, to examine eyelids under the slit lamp, 70% of participants preferred using 10x and 16x magnifications, whereas to examine for Demodex mites this was 57%. In addition, only 38% of participants preferred using 25x and 40x magnification to examine for Demodex mites (p < 0.001, Figures 2a and b).
A total of 30% of optometrists (n =53), looked for Demodex mites in their patients. Optometrists reported that cylindrical dandruff (CD) (28.9%) was the most common clinical diagnostic feature, closely followed by crusts/flakes (28.1%) on the eyelashes, and itching was the most common symptom observed in Demodex blepharitis. The highest percentage of respondents (37%) agreed that the presence of CD on the eyelashes is confirmation of presence of Demodex blepharitis followed by lash manipulation (22%), epilation (19%), diagnosis by elimination (17%), and successful treatment (5%).
With regards to management strategies, most of the optometrists (40%) aimed for improving patient comfort, followed by improving meibomian gland secretion (20.8%) and elimination of mites (20.8%) (Figure 3). Standard lid hygiene was the first-choice management option for most optometrists (64%), followed by tea tree oil (TTO) wipes/cleansers (19%) and (17%) preferring a 50% mixture of TTO (Figure 4). Furthermore, the majority of optometrists (57%) preferred 3–4 weeks of treatment (Figure 5), twice a day (74%) (Figure 6).
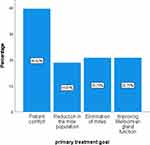 |
Figure 3 Bar chart showing the differences in the treatment strategies. Most of the optometrists preferred patient comfort. |
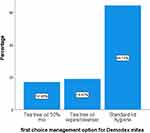 |
Figure 4 Bar chart showing preferred management options for Demodex mites. Standard lid hygiene was the first-choice management option for majority of optometrists. |
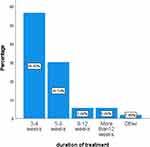 |
Figure 5 Bar chart showing the suggested duration of treatment for Demodex blepharitis. Majority of optometrists preferred 3–4 weeks of treatment. |
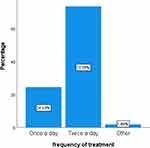 |
Figure 6 Bar chart showing the frequency of treatment. Majority of preferred that the treatment should be performed twice a day. |
Discussion
This study looked at practitioners’ awareness of investigating and managing Demodex blepharitis by optometrists in India. Previous data from a survey-based study in the United States reported optometrists and ophthalmologists managing 47% and 37% of their patients affected with blepharitis in clinical practice respectively, whereas in Great Britain, blepharitis accounted for more than 70% of cases in patients presenting with ocular inflammation.10,20 The results of this survey suggests that Demodex blepharitis is a highly under-reported condition in India, with nearly 30% of surveyed practitioners managing this condition. Demodex mites have been reported to cause chronic blepharitis and have been linked to escalating severity in DED and MGD.31 The prevalence of chronic blepharitis, as reported by Venturino et al, in their study was around 36%.14 Similarly, the prevalence of blepharitis in the general Indian population is estimated to be around 40% by the surveyed eye care practitioners in this study. Despite studies reporting Demodex mites to be present in healthy individuals, its potential as an opportunistic pathogen cannot be ignored. The relationship between an increased number of Demodex mites in causing blepharitis is well-established.32 In this study, we found that optometrists in India estimated Demodex mites to be present in 40% of the healthy population. Other studies have also reported a lower prevalence rate of Demodex mites in healthy controls.19,33 While Zeytun and Karakurt reported the prevalence of Demodex mites to be 31.4% in their study with 175 healthy participants, Zhong et al, reported the prevalence of Demodex mites to be less than 10% (D. Folliculorum – 8.47% and D. Brevis – 6.65%) in their study with 1700 healthy participants.19,33 Both of the studies, however, reported the ocular symptoms to be increased by the higher number of Demodex mites. In this study, the prevalence of Demodex mites in blepharitis was estimated to be 30%, whereas much higher prevalence rates have been previously reported by Zeytun and Karakurt (79.2%), by Venecia and Siong (73%), by Bhandari and Reddy (78.7%) and 83.7% by López-Ponce et al19,34–36 It is essential to take note that studies reporting the prevalence of Demodex mites are based on clinical observation whereas prevalence values reported in this study are estimates based on practitioner’s experience and can vary from region to region.
The results from this study suggest that around 70% of optometrists did not receive any training regarding Demodex detection and treatment, while others received it in form of a lecture, webinar or journal article. This could be one of the reasons for the reported low prevalence. Although 66% of practitioners agreed that Demodex was a significant cause of ocular discomfort, only 30% of practitioners intervened to diagnose and manage Demodex blepharitis. Therefore, it can be inferred that a lack of training and clinical skill set prevents surveyed optometrists in India from accurately diagnosing and managing the condition. If left untreated, Demodex has been linked to worsening ocular surface health by causing DED, chalazion, MGD, and corneal inflammation.37
The study showed that 32% of those surveyed used 16x magnification, 24% used 25x, 13% used 40x and 30% used a magnification of just 10x and 6x, to look for Demodex mites in their patients. Whereas previous research has suggested a higher magnification (25–40x) is crucial to view Demodex mites.31,38 Although statistical significance was reached with regards to the variation in preferred choice of magnification while observing eyelids and Demodex mites (p < 0.001), these differences may not be clinically significant. This is because 70% of participants preferred using 10x and 16x magnification to view eyelids, whereas only 40% among the same participants increased magnification to view Demodex mites. Therefore, it can be inferred that there is a lack of clinical knowledge, since nearly 60% of practitioners still use a low-to-moderate magnification to view Demodex mites. This relates back to the low number of surveyed practitioners who have received any training on the detection and management of Demodex blepharitis.
The presence of CD was reported to be the most common clinical feature observed in Demodex infestation, closely followed by crusts/flakes on the eyelashes. Similarly, the presence of CD was also the most favoured method for confirming the presence of Demodex mites, followed by lash manipulation and epilation. Studies have also shown a strong correlation between the presence of CD and Demodex infestation.33,39 For example, Muntz et al compared different techniques used to diagnose Demodex clinically and suggested that combining CD removal with eyelash manipulation gives a reliable estimate of number of mites in-situ.38 Therefore suggesting that these modified eyelash manipulation techniques are better indicators of Demodex numbers than conventional epilation. However, the literature still lacks a globally-accepted method for ocular Demodex detection and clinical findings are solely based on practitioner’s experience and/or available resources. A lack of consensus was observed among optometrists regarding the management of Demodex blepharitis. Optometrists reported patient comfort as their primary treatment goal. Nichols et al have argued that total eradication of this mite may not be necessary, since it is a part of the normal ecology of the eye, feeding on bacteria, and acting as an eyelash cleaner.40 In this study, standard lid hygiene was the primary choice of treatment reported as being employed by eye care practitioners to treat Demodex blepharitis. Standard lid hygiene includes warm compresses which aim to improve the general health of the eyelid, and not effective at eradicating Demodex mites.41 Whereas, many research studies suggest using tea tree oil (TTO),42–44 ivermectin45 and lotilaner46 to control Demodex infestation. A lack of standardised treatment protocols among eye care practitioners can lead to poor clinical results or delays in resolution. The majority of optometrists recommended 3–4 weeks of treatment twice a day. Similarly, Gao et al, recommended that treatment with TTO performed twice a day for 4 weeks reduces the symptoms and lowers the Demodex count.47 Therefore, it can be inferred that practitioners are advising management for a suitable time and a suitable frequency, but not necessarily with the appropriate agent to eliminate the mites. It has also been suggested that products containing TTO might not be available and authorised for clinical use in certain countries and since there are no established guidelines, there is an uncertainty towards managing Demodex blepharitis.48 A similar case of inappropriate management was observed in a survey study investigating computer vision syndrome (CVS), which reported confusion regarding treatment guidelines among eyecare practitioners and highlighted the need for an internationally-accepted diagnostic and grading system for CVS.49 Nevertheless, increasing clinician awareness may perhaps result in better investigation and management.
There are certain limitations to this study which need to be considered. Firstly, the scope of health issues can vary from country to country and hence the primary workforce would be more inclined towards resolving conditions that require immediate attention. In India, cataracts and refractive errors remain the primary cause of avoidable blindness and visual impairment.50 Secondly, the study team also acknowledges that the study was conducted at the peak of the Covid-19 pandemic when most daily activities were moved online. Therefore, survey links from this study could have been easily overlooked due to overwhelming online activities.
Conclusion and Future Work
The study reported a lack of awareness and consensus among optometrists surveyed in India, with regards to diagnosis and appropriate treatment methods to control Demodex infestation. To achieve better clinical outcomes, further research is required to assess the practitioner’s perspective on the global prevalence of Demodex blepharitis. The study also observed a need to develop a standardized protocol in examining and managing patients suffering from Demodex blepharitis and this would need to be in conjunction with improved practitioner awareness and education. To understand eye care practitioners’ perspective regarding Demodex blepharitis globally, similar studies are being conducted by the study team for eye care practitioners in the United Kingdom, Australia, and New Zealand. Findings from these studies will be compared and could help the study team to determine the best evaluation and treatment techniques, so that internationally-approved guidelines can be drawn up and disseminated globally for better and more consistent patient care.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Benitez-del-Castillo JM. How to promote and preserve eyelid health. Clin Ophthalmol. 2012;6:1689. doi:10.2147/OPTH.S33133
2. Jeng BH. 7 - diagnostic techniques in ocular surface disease. Ocular Surf Dis. 2013;47–54. doi:10.1016/B978-1-4557-2876-3.00007-9
3. Guillon M, Maissa C, Wong S. Eyelid margin modification associated with eyelid hygiene in anterior blepharitis and meibomian gland dysfunction. Eye Contact Lens. 2012;38(5):319–325. doi:10.1097/ICL.0b013e318268305a
4. Weidmayer S, McGinty-Tauren M. A close look at common LID LESIONS. (EYELID HEALTH LUMPS & BUMPS). Rev Optometry. 2019;156(11):38.
5. Smith RE, Flowers CW. Chronic blepharitis: a review. CLAO J. 1995;21(3):200.
6. Lindsley K, Matsumura S, Hatef E, Akpek EK. Interventions for chronic blepharitis. Cochrane Database Syst Rev. 2012;5:CD005556.
7. Kheirkhah A, Blanco G, Casas V, Tseng SCG. Fluorescein dye improves microscopic evaluation and counting of demodex in blepharitis with cylindrical dandruff. Cornea. 2007;26(6):697–700. doi:10.1097/ICO.0b013e31805b7eaf
8. Rufli T, Mumcuoglu Y. The hair follicle mites demodex folliculorum and demodex brevis: biology and medical importance. Dermatology. 1981;162(1):1–11. doi:10.1159/000250228
9. Hom MM, Mastrota KM, Schachter SE. Demodex: clinical cases and diagnostic protocol. Optometry Vision Sci. 2013;90(7):e198–e205. doi:10.1097/OPX.0b013e3182968c77
10. Lemp MA, Nichols KK. Blepharitis in the United States 2009: a survey-based perspective on prevalence and treatment. Ocular Surf. 2009;7(2):S1–S14. doi:10.1016/S1542-0124(12)70620-1
11. Lemp MA, Lemp MA. Report of the national eye institute/industry workshop on clinical trials in dry eyes. CLAO J. 1995;21(4):221–232.
12. Amescua G, Akpek EK, Farid M, et al. Blepharitis preferred practice pattern®. Ophthalmology. 2019;126(1):P56–P93. doi:10.1016/j.ophtha.2018.10.019
13. Bruce jackson W. Blepharitis: current strategies for diagnosis and management. Can J Ophthalmol. 2008;43(2):170–179. doi:10.3129/i08-016
14. Venturino G, Bricola G, Bagnis A, Traverso CE. Chronic blepharitis: treatment patterns and prevalence. Invest Ophthalmol Vis Sci. 2003;44:U226.
15. Patel N, Mathur U, Gandhi A, Singh M. Demodex blepharokeratoconjunctivitis affecting young patients: a case series. Indian J Ophthalmol. 2020;68(5):745–749. doi:10.4103/ijo.IJO_1402_19
16. Galea M, Sharma R, Srinivasan S, Roberts F, Galea M. Demodex blepharitis mimicking eyelid sebaceous gland carcinoma. Clin Exp Ophthalmol. 2014;42(2):208–210. doi:10.1111/ceo.12116
17. Shah PP, Stein RL, Perry HD. Update on the management and treatment of demodex blepharitis. Cornea. 2021;41:934–939. doi:10.1097/ICO.0000000000002911
18. Din N, Patel NN. Blepharitis — a review of diagnosis and management. Int J Ophthal Pract. 2012;3(4):150–155. doi:10.12968/ijop.2012.3.4.150
19. Zeytun E, Karakurt Y. Prevalence and load of demodex folliculorum and demodex brevis (acari: demodicidae) in patients with chronic blepharitis in the province of erzincan, Turkey. J Med Entomol. 2019;56(1):2. doi:10.1093/jme/tjy143
20. Edwards RS. Ophthalmic emergencies in a district general hospital casualty department. Br J Ophthalmol. 1987;71(12):938. doi:10.1136/bjo.71.12.938
21. Millán A, Viso E, Gude F, Parafita-Fernández A, Moraña N, Rodríguez-Ares MT. Incidence and risk factors of dry eye in a Spanish adult population: 11-year follow-up from the salnés eye study. Cornea. 2018;37(12):1527–1534. doi:10.1097/ICO.0000000000001713
22. Lin P, Tsai S, Cheng C, Liu J, Chou P, Hsu W. Prevalence of dry eye among an elderly Chinese population in Taiwan: the shihpai eye study. Ophthalmology. 2003;110(6):1096–1101. doi:10.1016/S0161-6420(03)00262-8
23. Hashemi H, Khabazkhoob M, Kheirkhah A, et al. Prevalence of dry eye syndrome in an adult population. Clin Exp Opthalmol. 2014;42(3):242–248. doi:10.1111/ceo.12183
24. Onwubiko SN, Eze BI, Udeh NN, Arinze OC, Onwasigwe EN, Umeh RE. Dry eye disease: prevalence, distribution and determinants in a hospital-based population. Contact Lens Anterio. 2013;37(3):157–161. doi:10.1016/j.clae.2013.09.009
25. Verma R, Khanna P, Prinja S, Rajput M, Arora V. The national programme for control of blindness in India. Australas Med J. 2011;4(1):1–3. doi:10.4066/AMJ.2011.505
26. World Medical Association. World medical association declaration of Helsinki. ethical principles for medical research involving human subjects. Bull World Health Organ. 2001;79(4):373.
27. GDPR. Data protection; 2018. Available from: https://www.gov.uk/data-protection.
28. Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet E-surveys (CHERRIES). J Med Internet Res. 2004;6(3):e34. doi:10.2196/jmir.6.3.e34
29. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi:10.1016/j.jbi.2008.08.010
30. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi:10.1016/j.jbi.2019.103208
31. Wolffsohn JS, Arita R, Chalmers R, et al. TFOS DEWS II diagnostic methodology report. Ocul Surf. 2017;15(3):539–574. doi:10.1016/j.jtos.2017.05.001
32. Moran E, Foley R, Powell F. Demodex and rosacea revisited. Clin Dermatol. 2016;35(2):195–200. doi:10.1016/j.clindermatol.2016.10.014
33. Zhong J, Tan Y, Li S, et al. The prevalence of Demodex folliculorum and Demodex brevis in cylindrical dandruff patients. J Ophthalmol. 2019;2019:1–7. doi:10.1155/2019/8949683
34. de Venecia AB, Lim Bon Siong R. Demodex sp. infestation in anterior blepharitis, meibomian-gland dysfunction, and mixed blepharitis. Philipp J Ophthalmol. 2011;36(1):15–22.
35. Bhandari V, Reddy JK. Blepharitis: always remember demodex. Middle East Afr J Ophthalmol. 2014;21(4):317. doi:10.4103/0974-9233.142268
36. López-Ponce D, Zuazo F, Cartes C, et al. High prevalence of demodex spp. infestation among patients with posterior blepharitis: correlation with age and cylindrical dandruff. Archivos de la Sociedad Española de Oftalmología. 2017;92(9):412–418. doi:10.1016/j.oftale.2017.07.002
37. Bitton E, Aumond S. Demodex and eye disease: a review. Clin Exp Optom. 2020;103:1–10. doi:10.1111/cxo.13123
38. Muntz A, Purslow C, Wolffsohn JS, Craig JP, Muntz A. Improved demodex diagnosis in the clinical setting using a novel in situ technique. Contact Lens Anterior Eye. 2019. doi:10.1016/j.clae.2019.11.009
39. Gao Y, Di Pascuale MA, Li W, et al. High prevalence of demodex in eyelashes with cylindrical dandruff. Invest Ophthalmol Vis Sci. 2005;46(9):3089. doi:10.1167/iovs.05-0275
40. Nicholls S, Oakley C, Tan A, Vote B. Demodex species in human ocular disease: new clinicopathological aspects. Int Ophthalmol. 2017;37(1):303–312. doi:10.1007/s10792-016-0249-9
41. Fromstein S, Harthan J, Patel J, Opitz D. Demodexblepharitis: clinical perspectives. Clin Optometry. 2018;10:57–63. doi:10.2147/OPTO.S142708
42. Liu J, Sheha H, Tseng SC. Pathogenic role of demodex mites in blepharitis. Curr Opin Allergy Clin Immunol. 2010;10(5):505. doi:10.1097/ACI.0b013e32833df9f4
43. Mastrota KM. It might be mites: rising concern about demodex mites compels clinicians to be on the alert. (FOCUS ON: dry eye)(disease/disorder overview). Optometry Times. 2013;5(9):18.
44. Joseph P. This mite be trouble: demodex infestation requires timely, appropriate treatment, as it can cause a number of ocular complications. (Cornea+Contact lens Q+A). Rev Optometry. 2014;151(1):64.
45. Brown M, Hernández-Martín A, Clement A, Colmenero I, Torrelo A. Severe demodex folliculorum-associated oculocutaneous rosacea in a girl successfully treated with ivermectin. JAMA Dermatol. 2014;150(1):61–63. doi:10.1001/jamadermatol.2013.7688
46. Gonzalez-Salinas R, Karpecki P, Yeu E, et al. Safety and efficacy of lotilaner ophthalmic solution, 0.25% for the treatment of blepharitis due to demodex infestation: a randomized, controlled, double-masked clinical trial. Contact Lens Anterior Eye. 2022;45(4):101492. doi:10.1016/j.clae.2021.101492
47. Gao Y, Xu D, Huang L, Wang R, Tseng SCG. Treatment of ocular itching associated with ocular demodicosis by 5% tea tree oil ointment. Cornea. 2012;31(1):14–17. doi:10.1097/ICO.0b013e31820ce56c
48. Navel V, Mulliez A, Benoist d’Azy C, et al. Efficacy of treatments for demodex blepharitis: a systematic review and meta-analysis. Ocular Surf. 2019;17(4):655–669. doi:10.1016/j.jtos.2019.06.004
49. Bali J, Navin N, Thakur BR. Computer vision syndrome: a study of the knowledge, attitudes and practices in Indian ophthalmologists. Indian J Ophthalmol. 2007;55(4):288–294. doi:10.4103/0301-4738.33042
50. De Souza N, Cui Y, Looi S, et al. The role of optometrists in India: an integral part of an eye health team. Indian J Ophthalmol. 2012;60(5):401–405. doi:10.4103/0301-4738.100534
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


