Back to Journals » Open Access Journal of Contraception » Volume 15
Contraceptive Utilization and Its Associated Factors Among Married Women in West African Countries: A Population-Based Survey Using Multinomial Logistic Regression
Authors Terefe B , Jembere MM, Enyew EF, Chekole B
Received 27 November 2023
Accepted for publication 26 March 2024
Published 3 April 2024 Volume 2024:15 Pages 53—66
DOI https://doi.org/10.2147/OAJC.S451908
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Igal Wolman
Bewuketu Terefe,1 Mahlet Moges Jembere,2 Engidaw Fentahun Enyew,3,4 Bogale Chekole5
1Department of Community Health Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia; 2Department of Emergency and Critical Care Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia; 3Department of Anatomy, School of Medicine, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia; 4Department of Reproductive Health, Institute of Public Health, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia; 5Department of Comprehensive Nursing, College of Medicine and Health Sciences, Wolkite University, Wolkite, Southern Ethiopia, Ethiopia
Correspondence: Bewuketu Terefe, Department of Community Health Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Post Office Box: 196, Gondar, Amhara Region, Ethiopia, Tel +251918099504, Email [email protected]
Background: The international development agenda emphasizes universal access to family planning, as seen in Sustainable Development Goal 3.7. However, the use of modern contraceptive methods remains low in developing countries, specifically in West Africa. This study aimed to assess the current status of contraceptive use in the region, focusing on different methods.
Methods: We analyzed Demographic and Health Survey data from 13 West African nations (2012– 2022) involving 117,165 married women. Using binary and multiple multinomial logistic regression, we identified key factors associated with contraceptive use. Adjusted odds ratios with 95% confidence intervals were utilized, and significance was determined at p ≤ 0.2 for binary regression and p < 0.05 for multiple multinomial regression.
Results: About 80.86% of women did not use any method, while 16.56% of women used modern methods. Maternal age of 35– 49 years (RRR=0.77, 95% CI, 0.72,0.82), had given first birth after 20 years (RRR=0.80,95% CI, 0.77,0.83), cohabitation after 20 years old (RRR=1.24,95% CI, 1.18,1.29), being employed (RRR=1.38,95% CI, 1.33,1.43), women who have from 3– 5, and more than five living children (RRR=2.06,95% CI,1.97,2.16, and (RRR=2.57, 95% CI, 2.42,2.74), primary(RRR=1.59, 95% CI, 1.52,1.66), secondary/higher education (RRR=2.08, 95% CI, 1.99,2.18), antenatal visit (RRR= 1.38, 95% CI 1.28,1.49), institutional delivery(AOR=1.42, 95% CI, 1.35,1.49), husband working status (RRR=1.39, 95% CI, 1.28,1.51), media exposure(RRR=1.23, 95% CI, 1.19,1.28), visited health facility more than once (RRR=1.09, 95% CI, 1.05,1.13), rural women (RRR=0.89,95% CI,0.85,0.93), female households (RRR=0.79, 95% CI,0.76,0.83), richer (RRR=1.42, 95% CI,1.33,1.51), and richest wealth indexes (RRR=1.69,95% CI,1.58,1.82) were associated.
Conclusion: This study revealed a low level of contraceptive use among women in West Africa. Strengthening maternal reproductive health services, such as antenatal care, institutional delivery, and health visits, while also targeting mass media and disadvantaged women, has the potential to significantly increase the adoption of modern contraception techniques.
Keywords: contraceptive utilization, family planning, married women, West Africa, multinomial logistic regression
Introduction
Some contraceptive methods, including the male condom, withdrawal, and rhythm methods, have been used for millennia, whereas others, such as the pill and intrauterine device (IUD), have become popular since the 1960s.1,2 Vaginal rings, emergency contraception, subcutaneous injections, and implants became available decades later. Different pregnancy prevention needs, such as ceasing or delaying childbirth, should be provided with appropriate and effective techniques.1,3 The goal of contraceptive methods is to achieve contraception in the most comfortable and private way possible with the least cost and negative effects.4 A trained family planning (FP) service provider focuses on family health and the couple’s desire to either limit or space their children.5 Traditional contraceptive methods, such as the use of concoctions, non-emergency contraception douching, and locally prepared potions of cooked leaves and/or traditional rings and/or alcohol, are still used in underdeveloped nations.1,2 However, the adoption of contemporary contraceptive methods is growing in many nations, and many women continue to prefer less effective traditional contraceptive methods over more effective modern contraceptive methods because of concerns about the latter’s adverse effects.1
In 2019, 1.1 billion of the world’s 1.9 billion women of reproductive age have a need for FP, which means they are either current users of contraception 842 million use modern methods of contraception, and 80 million use traditional methods, or have an unmet need for FP 190 million women want to avoid pregnancy but do not use any contraceptive method. In 2019, 76 proportion of women fulfilled their FP needs by modern means Sustainable Development Goal (SDG indicator 3.7.1).1,6,7 Another 2017 World Health Organization(WHO) report estimated that 214 and 23 million reproductive-aged women had an unmet need for contraception methods and unintended pregnancies due to low-quality service, cultural opposition, and limited access and experience with side effects, respectively.8 The United Nations report shows that contraception use among women has been increasing in all world regions; however, it is in the lower range.9 Reports indicate that modern contraception methods prevented approximately 308 million unintended pregnancies, and 67 million unintended pregnancies could be averted if the unmet issue was resolved.10
Contraception methods play an important role in lowering the complications of infant and maternal morbidity and mortality caused by unplanned preventative pregnancies as well as the social expenses associated with them.11,12 This concept is also supported by the SDG, which emphasizes ensuring healthy lifestyles and advocating well-being for people of all ages.12–14
Several studies have investigated factors that influence contraceptive use in Sub-Saharan Africa. These include inadequate service quality and significant distance between health institutions and users’ homes.15–17 According to SSA research, many individual- and community-level factors, such as age, marital status, religion, household wealth index, joint contraception decisions, place of residence, employment status, community education level, and the number of children, have also been linked to contraceptive use in various countries.16–23 Women’s awareness, perception, and information exposure/reading newsletters listening to radio on contraceptive benefits have also been linked to SSA.16,21,23,24
To the best of our knowledge, no previous study has been conducted in West African countries using various contraception methods (no method, traditional, and modern). Using the most recent demographic and health survey (DHS) data, this study aimed to investigate contraception utilization in West African countries using generalized linear model regression among married women of reproductive age.
Methods
Study Setting, and Period
The Westernmost part of Africa is West Africa and Western Africa. The 16 countries of Benin, Burkina Faso, Cape Verde, The Gambia, Ghana, Guinea, Guinea-Bissau, Ivory Coast, Liberia, Mali, Mauritania, Niger, Nigeria, Senegal, Sierra Leone, and Togo are included in the United Nations definition of Western Africa, along with Saint Helena, Ascension, and Tristan da Cunha (a United Kingdom Overseas Territory).25,26 West Africa has an estimated total population of 419 million people by 2021 and 381,981,000 by 2017, with 189,672,000 females and 192,309,000 males.27 One of the fastest-expanding regions on the African continent, both economically and demographically, is the region in question.
We combined data from the women’s files of the 13 West African countries that participate in the Demographic and Health Surveys (DHS) program and for which data have been published in the previous five years: Benin, Burkina Faso, Ghana, Gambia, Guinea, Liberia, Mali, Mauritania, Niger, Nigeria, Senegal, Sierra Leone, and Togo. Every five years, surveys of low- and middle-income countries are conducted nationwide on DHS. The poll was conducted in West African nations between 2014 and 2022.
Data Sources and Sampling Procedures
Recent nationally representative DHS data collected from 13 West African countries were used as the data source for this study. Every five years, low- and middle-income nations participate in DHS surveys, which are consistently conducted using pre-tested, validated, and standardized techniques. Multi-country analysis was made possible using the same standard process for sampling, questionnaires, data collection, and coding.
The DHS uses a stratified two-stage sampling approach to guarantee national representation. Clusters/enumeration areas (EAs) that encompass the entire nation were randomly chosen from the sample frame in the first step (ie, typically created from the most recently available national census). The second stage involved systematically selecting houses from each cluster or EA and conducting interviews with selected households’ target demographics (women between the ages of 15 and 49 and men between the ages of 15 and 64, respectively). Women between the ages of 15 and 49 who are married and did not used any types of method, traditional or modern contraception utilization were included in this study. The pooled data analysis yielded a total weighted sample size of 117,165, with sample sizes ranging from 2067 in Liberia to 28,121 in Nigeria (Table 1).
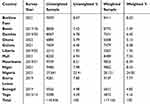 |
Table 1 Countries, Survey Year, and Samples of Demographic and Health Surveys Included in the Analysis for 13 West African Countries |
Data Management and Statistical Analysis
After receiving a letter from the http://www.dhsprogram.com website for West African DHS data set for its usage, the dataset was retrieved from the website. Stata version 17 and used to extract, recode, and analyze the data. Weighting was used throughout the study to ensure representativeness and non-response rate, as well as to obtain a suitable statistical estimate (robust standard error).28 In the bivariable analysis, variables with a p-value of ≤0.2 were considered for the multiple multinomial logistic regression analysis (Table 2). Then best-fitted model’s Adjusted Odds Ratio (AOR) with 95% CI was provided in the multivariable multinomial logistic model to identify the factors associated with the use of contraception using different methods. Descriptive studies, such as frequency counts and proportions for categorical data, were used to summarize descriptive data. Bivariate logistic regression was used to select candidate variables for multiple multinomial logistic regression. Using the variance inflation factor, a logistic regression was fitted to examine multicollinearity among the independent variables. The Hosmer–Lemeshow test was also employed to evaluate the overall fitness of the final regression model. The statistical significance of the final model was set at p < 0.05.
 |
Table 2 Binary Multinomial Logistic Regression Analysis Results on Determinants of Methods of Contraceptive Utilizations Among Married Reproductive Age Women in West Africa |
Model Goodness Fits and Comparison
Three models, namely, binary logistic, ordinal, and multinomial logistic regressions, were used as candidate models. A strategy that was frequently used was the ordinal logistic regression mode since utilization of contraception in types of methods were listed as (no method, traditional methods, and modern methods). The assumption of the proportional odds model (POM) was not fulfilled; however, after we evaluated it for the Stata command or Brant test model, we deployed a multinomial logistic regression model. The three models and significant factors varied slightly from one another. POM assumptions, which indicate that the effects of all independent factors are constant across categories of the outcome variable, were used to select a suitable ordinal model for the data. The POM assumption was verified using the Stata command and the Brant test (p = 0.0001). The AIC, BIC, and LLR were also slightly larger in the ordinal logistic regression models than in the multinomial regression models. Therefore, we did not employ POM to determine whether the three methods of contraceptive use among married women and the independent variables were related. Therefore, the multinomial logistic model was found to be the best-fit model for the binary and ordinal logistic regressions.
Variance Inflation Factor (VIF) Analysis
Before proceeding to the analysis section, each dependent variable was assessed in terms of its variance inflation factors and tolerances (details are described in the Methods section). In the present study, the mean VIF was 1.18.
Variables of the Study
The Outcome Variable
The outcome variable of this study was the percentage of women who currently used any method (no method, traditional method, or modern method). In the DHS data, modern contraceptive methods include male and female sterilization, intramuscular injections, intrauterine contraceptive devices (IUCD), contraceptive pills, implants, male condoms, lactational amenorrhea, and emergency contraception. The outcome variable was classified into three categories and coded as “0” for no method, “1” for traditional, and “2” for modern types of contraceptive techniques. This was performed in accordance with the Guide to DHS Statistics.29
The Independent Variables
Independent variables: Various sociodemographic, maternal reproductive health, and child-related factors were included. These included maternal age, educational status, type of place of residence, marital status, household wealth index, current employment status, mass media exposure, ANC follow-up, place of delivery, breastfeeding status, knowledge of contraceptives, age at cohabitation, age at first birth, number of health visits and total children born, under five children, contraceptive utilization, age of the child, sex of the child, size at birth, twin status, birth order, gender of the household head, husband’s occupation, husband’s educational status, husband’s desire for children, and country.
Results
Sociodemographic Characteristics of the Study Participant
In this study, a total of 117,165 weighted married women of reproductive age were enrolled from 13 West African countries. Among the study participants, 45,972 (39.2%) were in the 25–34 years age group, which accounted for the majority. Regarding knowledge of contraceptive methods, the majority of mothers (110,850 or 94.6%) were informed about modern contraceptive methods. In terms of demographic characteristics, 73,025 (62.3%) resided in rural areas, 67,576 (57.7%) had no formal education, 24,172 (20.6%) belonged to poorer households based on the wealth index, 89,191 (76.1%) had institutional deliveries, and 105,021 (89.6%) had at least one ANC visit during their pregnancies. Furthermore, approximately 62,103 (53.0%) had no exposure to mass media (such as listening to radio, watching television, or reading magazines/newspapers), and 72,841 (62.2%) were currently employed or actively working. In terms of age at first cohabitation, 59,615 (50.9%) women had experienced it before reaching 20 years of age, and 61,504 (52.5%) had given birth before the age of 20. Additionally, around 67,655 (54.7%) had fewer than three children under the age of five in their households. The majority of households (99,589 or 85.0%) were led by male heads. Concerning husband-related characteristics, 66,649 (56.9%) had no formal education involvement, and 111,030 (94.8%) were currently working. Detailed information is presented in Table 3.
 |
Table 3 Socio-Demographic and Maternal Related Characteristics of Respondent’s Contraception Utilization Among Married Women in West African Countries (Weighted n=117,165) |
Prevalence of Contraceptive Utilization in West Africa
In this study, the overall utilization of modern contraception was approximately 16.56% (95% CI, 16.35, 16.77). However, about 80.86% (95% CI, 80.63, 81.08) of women did not use any contraceptive methods. Among the modern contraceptive methods, implants/Norplant and injections had the highest coverage percentages at 5.27% and 5.03%, respectively. On the other hand, diaphragms and female condoms had the lowest percentages, both being less than one percent. The highest rates of modern contraceptive utilization were found in Burkina Faso (32.25%), Ghana (26.04%), and Senegal (35.53%), respectively. Conversely, the lowest utilizations were observed in Guinea (9.62%), Nigeria (11.88%), and Niger (12.18%), respectively.
Factors Associated with Utilization of Contraceptive Among Married Women in West Africa
When holding all other variables constant, maternal age between 35 and 49 years was associated with 0.23 times decrease in the relative risk ratio (RRR=0.77, 95% CI, 0.72, 0.82) of using modern contraceptive methods instead of no methods. ”Similarly, women who gave birth for the first time after the age of 20 showed a lower relative risk ratio (RRR=0.80, 95% CI, 0.77, 0.83) for utilizing modern contraceptive methods compared to using no contraception. However, mothers who began their first cohabitation after the age of 20 exhibited a higher risk ratio (RRR=1.24, 95% CI, 1.18, 1.29) for using modern contraceptive methods rather than no methods. Additionally, employed mothers demonstrated a higher risk ratio (RRR=1.34, 95% CI, 1.33, 1.43) for utilizing modern contraceptive methods compared to using no contraception. Mothers who have 3–5 living children or more than five children showed a higher tendency to utilize modern contraceptive methods rather than no methods, with a relative risk ratio of (RRR=2.06, 95% CI, 1.99, 2.16) and (RRR=2.57, 95% CI, 2.42, 2.74) respectively, compared to participants with fewer than three children. In comparison to mothers who did not participate in formal education, those who attended primary and secondary/higher education demonstrated a higher relative risk ratio (RRR=1.59, 95% CI, 1.52, 1.66) and (RRR=2.08, 95% CI, 1.99, 2.18) respectively, indicating a greater likelihood of utilizing modern contraceptive methods rather than no methods. Similarly, having at least one ANC visit during pregnancy and giving birth at health institutions increased the relative risk of using modern contraceptive methods compared to not using any methods by 1.38 and 1.42 respectively (an increase of 38% and 42% respectively). Women whose husbands are currently employed have shown a higher relative risk ratio of using modern contraceptive methods compared to not using any method (RRR=1.39, 95% CI, 1.28, 1.51). Additionally, having exposure to mass media and visiting health facilities more than once in the past 12 months increased the relative risk of using modern contraceptive methods compared to not using any method by (RRR=1.23, 95% CI, 1.19, 1.28) and (RRR=1.09, 95% CI, 1.05, 1.13) respectively, as compared to their counterparts. Moreover, mothers from rural areas and households led by male heads were found to be less likely to utilize modern contraceptive methods, with relative risk ratios of (RRR=0.89, 95% CI, 0.85, 0.93) and (RRR=0.79, 95% CI, 0.76, 0.83) respectively, compared to using no methods. Similarly, in terms of household wealth indexes, mothers from poorer, middle, richer, and richest households have shown a higher likelihood of using modern contraceptive methods compared to women from the poorest household wealth index, with relative risk ratios of (RRR=1.07, 95% CI, 1.02, 1.13), (RRR=1.16, 95% CI, 1.10, 1.23), (RRR=1.37, 95% CI, 1.29, 1.45), and (RRR=1.53, 95% CI, 1.43, 1.64) respectively, indicating a greater likelihood of using modern contraceptive methods rather than not using any method (Table 4).
 |
Table 4 Multiple Multinomial Logistic Regression Analysis Results on Determinants of Methods of Contraceptive Utilizations Among Married Reproductive Age Women in West Africa |
Discussion
This study examined the prevalence and factors that influence the types of contraception methods used in West African nations with a history of low modern contraceptive use and high maternal mortality. In total, we found that only one every six married women used modern contraceptive methods. Majority married women did not use any contraceptive method. After controlling for confounders, variables such as maternal age, mass media exposure, wealth status, educational cohabitation year, age at first birth, female household head, number of living children, type of residence, having at least one antenatal follow-up, place of delivery, number of health visits during the year, husband, and maternal employment status were independently associated with the types of contraceptive methods used by married women. An explanation of the results is provided below for each of them in relation to the existing literature.
When all other variables were held constant, maternal age 35–49 years was associated with 0.23 times decrease in the relative ratio of using modern contraceptive method types rather than no method types. This study found the same findings as previous studies conducted in Malawi,30 Nigeria,31 Indonesia,32 and Ethiopia.33,34 This could be explained by the fact that as a mother gets older, her chances of having a baby decrease, even if she needs and desires to use contraceptives. On the other hand, as mothers age, their odds of completing their academic journey improve, as does their desire to have babies. They may also refrain from using contraception, because they are more likely to live alone and manage their finances and ways of thinking. They are also likely to have access to income sources. Furthermore, when all other variables were held constant, mothers who had completed their first cohabitation after the age of 20 years showed a higher tendency to use modern contraceptive methods rather than not using any type of contraceptive method. This could be related to the fact that as women’s age increases, they will have a better chance of completing their education, having more knowledge, awareness, and a good attitude, and having a culture of decision-making with their husband, employment, and empowerment.35
Women who had given their first birth after 20 years of age showed a lower relative risk ratio for utilizing modern contraceptive methods than for not using any methods for contraception. This outcome is similar to the results of studies conducted in Uganda.36 This is logical because these mothers did not give birth in the age range, they were supposed to give birth to, and they were now too old to try to have a baby before they stopped giving birth. Consequently, women at the ¥ 20 years were more likely to use contraceptives.
Mothers who have from 3–5, and more than five children had a higher tendency to utilize modern contraceptive methods than those who had fewer than three children. As the number of living children has increased, so has the likelihood of utilizing contemporary contraception. Previous research has also found that women with a large number of living children are more likely to use contemporary contraception.37–39 This could be explained by the fact that women do not want to use contraception until they have more children; subsequently, they do not want any more children and prefer to use family planning services. This study shows that when women reach their preferred family size, they use contraception.
Compared to mothers who were not enrolled in formal educational systems, those who had attended their primary and secondary/higher educational attainment showed a higher relative risk ratio of utilizing modern method types of contraceptives than using no method type of contraceptive. This study reported findings similar to those of studies conducted in Nigeria,31 East Africa40 and Ethiopia.33,34,41 Possible justifications include educated women having more information and a more positive attitude toward birth control than illiterate women. Furthermore, as these women learn, their ability to become more self-reliant grows and they are able to cope with society’s negative impacts. Alternatively, educated women may live in cities and have access to more family planning services.
Having at least one ANC visit during pregnancy and giving birth at a health institution increases the relative risk of the utilization of modern contraceptive methods rather than using any type of method. Mothers who had at least one antenatal care follow-up during their pregnancy and institutional delivery showed a better tendency to use contraceptives than those who did not have antenatal care follow-ups during their pregnancy period and delivered at home. This judgment is incongruent with other investigations of middle- and lower-income countries.42 Mothers with basic maternal and child health services might be more likely to benefit from a family planning package as they are better informed and counselled by health professionals than unsupervised.32 However, they may also have a better understanding of family planning.32 Furthermore, having visited health facilities more than once in the past 12 months has increased the relative risk of using modern contraceptive methods rather than not utilizing nothing, compared to their counterparts. The availability of health facilities in the community is also a significant factor in the increased use of modern contraceptives. This meant that not only was demand for healthcare programs important but so was supply, which was supported by other studies.43,44
Employed mothers have shown a higher risk ratio of utilizing modern contraceptive methods than utilizing no method of contraception, and women whose husbands are currently working have shown a higher relative risk ratio of using modern contraceptive methods than those who do not use any type of contraceptive method. Women and husbands who have worked in different occupations are more likely to share their knowledge and expertise on contemporary contraception with coworkers.37,45,46 It has also been discovered that media exposure has a beneficial effect on contemporary contraceptive use.
Furthermore, having mass media exposure have increased the relative risk of using modern contraceptive methods rather than not utilizing nothing as compared their counterparts. Because most African parents rarely discuss sexual and reproductive health (SRH) with their children, teenagers often rely on unofficial sources for SRH information.47,48 Mobile phones provide anonymous, confidential, and conveniently accessible locations to obtain sensitive SRH information.47,48 Mass media campaigns may encourage the use of contemporary contraceptives by increasing awareness, sensitization, and refuting myths, resulting in good health-seeking behavior.49
Residentials from rural areas and those households led by male heads have been found to utilize modern contraceptive methods less likely than using no method types. Our findings support those of several other studies that suggest that rural women are less likely to utilize contemporary contraception than their urban counterparts.50–52 This could be because health facility distance, knowledge and attitude barriers, less women’s empowerment,53 and cultural and other sociodemographic characteristics are more prevalent in rural areas than in metropolitan areas. The observed difference in association could be explained in part by a lack of health facilities and the long distances that rural adolescents must travel, resulting in a larger need for community health workers compared to better access to health services in urban regions.54,55
Similarly, regarding household wealth, keeping other variables constant, mothers who came from middle, richer, and richest households showed a higher likelihood of risk using modern contraceptive methods than women who came from the poorest household wealth index rather than not using the nay method types. We discovered that income was positively and strongly associated with the use of contemporary contraceptives, which is consistent with the findings of many other studies.33,53,56 The presence of a health center in the neighborhood was also a significant factor in the increased use of contemporary contraception. This meant that not only was demand for healthcare programs important but so was supply, which was supported by other studies.43,57
This study had both merits and weaknesses. This study employed nationally weighted representative data, which more accurately reflected the proportion of married women utilizing contraceptive methods and the factors that influence them at the national level. The temporal association between modern contraceptive use and the aforementioned predictor variables cannot be guaranteed because this study employed data from a single survey, and this information should be used with caution. Furthermore, due to a lack of qualitative data on DHS, the current study did not investigate the relationship between qualitative variables such as socio-cultural factors and types of methods of contraception utilization.
Conclusion
This study found an unusually low level of contemporary contraceptive use among women of reproductive age in West Africa. Variables such as maternal age, mass media exposure, wealth status, educational cohabitation year, age at first birth, female household head, number of living children, type of residence, having at least one antenatal follow-up, place of delivery, number of health visits during the year, husband, and maternal employment status were independently associated with the types of contraceptive methods used by married women. To achieve greater success, an intervention approach that promotes the use of modern contraceptive methods should consider these aspects. Future researchers should explore spatiotemporal, trend, and qualitative variables, such as sociocultural influences, which may have a significant impact on modern contraception utilization. Strengthening and utilizing any maternal reproductive health services (ANC, institutional delivery, health visits), as well as encouraging disadvantaged women, have great potential to boost the rate of modern contraception techniques.
Data Sharing Statement
All the data concerning this study are presented in this document. The detailed dataset is freely accessible from www.dhsprogram.com website.
Ethical Considerations and Data Set Access
The study was conducted after obtaining a permission letter from www.dhsprogram.com on an online request to access West African DHS data after reviewing brief descriptions of the survey submitted to the DHS program. The datasets are treated at the highest confidence level. Based on the national legislation in Ethiopia, DHS-based studies do not require ethical clearance. The DHS program, which is implemented in collaboration with various national institutions, ensures that all surveys conducted comply with the ethical standards and guidelines set forth by the country’s legislation. DHS surveys follow rigorous protocols to protect the rights and privacy of participants. These protocols include obtaining informed consent from respondents, ensuring confidentiality, and maintaining the anonymity of the collected data. The surveys are designed to meet high ethical standards and prioritize the well-being and safety of participants. DHS program has been widely recognized and endorsed by international organizations, such as the United Nations and the World Health Organization, as a valuable source of data for evidence-based policies and programs. We did not manipulate or apply any microdata other than those used in this study. No patient or public involvement was involved in the study.
Acknowledgments
We would like to acknowledge the DHS program for providing permission for this study following research ethics.
Author Contributions
The conception, study design, execution, data collection, analysis, and interpretation of the research, as well as the drafting, revision, and critical review of the article, were all completed by the authors. Furthermore, authors were responsible for deciding which journal the article should be submitted to. Each author was also aware of every version of the article. Additionally, the authors committed to being accountable and responsible for the content of the article. They selected the journal for submission and approved the final draft of the manuscript.
Disclosure
The authors declared that there are no competing interests in this work.
References
1. United Nations DoEaSA, Population Division. Contraceptive Use by Method; 2019. Available from: https://www.un.org/development/desa/pd/sites/www.un.org.development.desa.pd/files/files/documents/2020/Jan/un_2019_contraceptiveusebymethod_databooklet.pdf.
2. Tietze C. History of contraceptive methods. J Sex Res. 1965;1(2):69–85. doi:10.1080/00224496509550473
3. World Health Organization. Counselling for maternal and newborn health care : a handbook for building skills. Available from: https://iris.who.int/handle/10665/44016.
4. Sitruk-Ware R, Nath A, Mishell DR Jr. Contraception technology: past, present and future. Contraception. 2013;87(3):319–330. doi:10.1016/j.contraception.2012.08.002
5. Bekele D, Fantahun M, Gutema K, Getachew H, Lambiyo T, Yitayal M For the Ethiopian Health Center Team; 2003.
6. Fabic MS, Choi Y, Bongaarts J, et al. Meeting demand for family planning within a generation: the post-2015 agenda. Lancet. 2015;385(9981):1928–1931. doi:10.1016/S0140-6736(14)61055-2
7. Kantorová V, Wheldon MC, Ueffing P, Dasgupta ANZ, Drake AL. Estimating progress towards meeting women’s contraceptive needs in 185 countries: a Bayesian hierarchical modelling study. PLoS Med. 2020;17(2):e1003026. doi:10.1371/journal.pmed.1003026
8. World Health Organization. Contraception fact sheet; 2021.
9. United Nations Department of Economic and Social Affairs PD. What is world fertility and family planning 2020 highlights?; 2020.
10. World Health Organnization. WHO recommendations on self-care interventions Self-administration of injectable contraception; 2020.
11. Atakro CA, Addo SB, Aboagye JS, et al. Contributing factors to unsafe abortion practices among women of reproductive age at selected district hospitals in the Ashanti region of Ghana. BMC Women’s Health. 2019;19(1):1–17. doi:10.1186/s12905-019-0759-5
12. Nyarko SH, Kabir R. Spatial variations and socioeconomic determinants of modern contraceptive use in Ghana: a Bayesian multilevel analysis. PLoS One. 2020;15(3):e0230139. doi:10.1371/journal.pone.0230139
13. Groups UND. The sustainable development goals are coming to life stories of country implementation and un support; 2016.
14. United Nations Department of Economic and Social Affairs. Family planning and the 2030 Agenda for sustainable development • data booklet; 2019.
15. Fruhauf T, Zimmerman L, Kibira SPS, et al. Measuring family planning quality and its link with contraceptive use in public facilities in Burkina Faso, Ethiopia, Kenya and Uganda. Health Policy Plann. 2018;33(7):828–839. doi:10.1093/heapol/czy058
16. Wang W, Mallick L. Understanding the relationship between family planning method choices and modern contraceptive use: an analysis of geographically linked population and health facilities data in Haiti. BMJ Global Health. 2019;4(Suppl 5):e000765. doi:10.1136/bmjgh-2018-000765
17. Shiferaw S, Spigt M, Seme A, et al. Does proximity of women to facilities with better choice of contraceptives affect their contraceptive utilization in rural Ethiopia? PLoS One. 2017;12(11):e0187311. doi:10.1371/journal.pone.0187311
18. Cronin CJ, Guilkey DK, Speizer IS. The effects of health facility access and quality on family planning decisions in urban Senegal. Health Econom. 2018;27(3):576–591. doi:10.1002/hec.3615
19. Hong R, Montana L, Mishra V. Family planning services quality as a determinant of use of IUD in Egypt. BMC Health Serv Res. 2006;6(1):1–8. doi:10.1186/1472-6963-6-79
20. Zimmerman LA, Bell SO, Li Q, et al. Individual, community and service environment factors associated with modern contraceptive use in five Sub-Saharan African countries: a multilevel, multinomial analysis using geographically linked data from PMA2020. PLoS One. 2019;14(6):e0218157. doi:10.1371/journal.pone.0218157
21. Wulifan JK, Brenner S, Jahn A, De Allegri M. A scoping review on determinants of unmet need for family planning among women of reproductive age in low and middle income countries. BMC Women’s Health. 2015;16(1):1–15.
22. Olakunde BO, Pharr JR, Chien L-C, Benfield RD, Sy FS, Haider MR. Individual-and country-level correlates of female permanent contraception use in sub-Saharan Africa. PLoS One. 2020;15(12):e0243316. doi:10.1371/journal.pone.0243316
23. Ahinkorah BO, Jeter JW, Dabbs WS, Stevens AB, Heidel RE, Chamberlin SM. Predictors of modern contraceptive use among adolescent girls and young women in sub-Saharan Africa: a mixed effects multilevel analysis of data from 29 demographic and health surveys. Contrac Reprod Med. 2020;5(1):1–12. doi:10.1186/s40834-020-00104-x
24. Ettarh RR, Kyobutungi C. Physical access to health facilities and contraceptive use in Kenya: evidence from the 2008–2009 Kenya demographic and health survey. Afr J Reproduct Health. 2012;16(3):47–55.
25. Masson MPR, Pattillo MCA Monetary Union in West Africa (ECOWAS). International monetary fund; 2001.
26. Division UNS. Standard Country Areas and Codes Classifications; 2014. Available from: https://unstats.un.org/unsd/methodology/m49/.
27. Division UNDoEaSAP. World Population Prospects 2022; 2022. Available from: https://population.un.org/wpp/.
28. Elkasabi M Sampling and Weighting with DHS Data; 2015. Available from: https://blog.dhsprogram.com/sampling-weighting-at-dhs/.
29. Croft T, Marshall AM, Allen CK, et al. Guide to DHS Statistics: DHS-7 (Version 2). Rockville, MD: ICF; 2020.
30. Palamuleni ME. Socio-economic and demographic factors affecting contraceptive use in Malawi. Afr J Reproduct Health. 2013;17(3):91–104.
31. Bolarinwa OA, Tessema ZT, Frimpong JB, Seidu -A-A, Ahinkorah BO, Moise IK. Spatial distribution and factors associated with modern contraceptive use among women of reproductive age in Nigeria: a multilevel analysis. PLoS One. 2021;16(12):e0258844. doi:10.1371/journal.pone.0258844
32. Kistiana S, Gayatri M, Sari DP. Determinants of modern contraceptive use among young married women (age 15–24) in Indonesia. Global J Health Sci. 2020;12(13):1–37. doi:10.5539/gjhs.v12n13p37
33. Tiruneh FN, Chuang K-Y, Ntenda PA, Chuang Y-C. Factors associated with contraceptive use and intention to use contraceptives among married women in Ethiopia. Women Health. 2016;56(1):1–22. doi:10.1080/03630242.2015.1074640
34. Lakew Y, Reda AA, Tamene H, Benedict S, Deribe K. Geographical variation and factors influencing modern contraceptive use among married women in Ethiopia: evidence from a national population based survey. Reproductive Health. 2013;10(1):1–10. doi:10.1186/1742-4755-10-52
35. Osuafor GN, Maputle SM, Ayiga N. Factors related to married or cohabiting women’s decision to use modern contraceptive methods in Mahikeng, South Africa. African J Primary Health Care Family Med. 2018;10(1):1–7. doi:10.4102/phcfm.v10i1.1998
36. Wasswa R, Kabagenyi A, Ariho P. Multilevel mixed effects analysis of individual and community level factors associated with modern contraceptive use among married women in Uganda. BMC Public Health. 2021;21(1):1–13. doi:10.1186/s12889-021-11069-0
37. Abate MG, Tareke AA. Individual and community level associates of contraceptive use in Ethiopia: a multilevel mixed effects analysis. Arch Public Health. 2019;77(1):1–12. doi:10.1186/s13690-019-0371-z
38. Idris H. Factors affecting the use of contraceptive in Indonesia: analysis from the National socioeconomic survey (susenas). KEMAS. 2019;15(1):117–123. doi:10.15294/kemas.v15i1.14098
39. Rutaremwa G, Kabagenyi A, Wandera SO, Jhamba T, Akiror E, Nviiri HL. Predictors of modern contraceptive use during the postpartum period among women in Uganda: a population-based cross sectional study. BMC Public Health. 2015;15(1):1–9. doi:10.1186/s12889-015-1611-y
40. Bakibinga P, Matanda DJ, Ayiko R, et al. Pregnancy history and current use of contraception among women of reproductive age in Burundi, Kenya, Rwanda, Tanzania and Uganda: analysis of demographic and health survey data. BMJ open. 2016;6(3):e009991. doi:10.1136/bmjopen-2015-009991
41. Sorato MM. Assessment of modern contraceptive method utilization and associated factors among women of reproductive age group in Arba Minch Town, SNNPR, Ethiopia. EC Gynaecol. 2017;6:36–53.
42. Dev R, Kohler P, Feder M, Unger JA, Woods NF, Drake AL. A systematic review and meta-analysis of postpartum contraceptive use among women in low-and middle-income countries. Reproductive Health. 2019;16(1):1–17. doi:10.1186/s12978-019-0824-4
43. Bongaarts J. The impact of family planning programs on unmet need and demand for contraception. Stud Fam Plann. 2014;45(2):247–262. doi:10.1111/j.1728-4465.2014.00387.x
44. Van den Broeck G. Women’s employment and family planning in rural Uganda. Women Health. 2020;60(5):517–533. doi:10.1080/03630242.2019.1671948
45. Mandiwa C, Namondwe B, Makwinja A, Zamawe C. Factors associated with contraceptive use among young women in Malawi: analysis of the 2015–16 Malawi demographic and health survey data. Contrac Reprod Med. 2018;3(1):1–8. doi:10.1186/s40834-018-0065-x
46. Devita VD, Rosliza A, Suriani I. Prevalence of modern contraceptive use among reproductive women with hypertension and diabetes in a government hospital in BATAM, Indonesia and its socio-demographic determinants. Int J Public Health Clin Sci. 2018;5(4):297.
47. Nwagwu WE. The Internet as a source of reproductive health information among adolescent girls in an urban city in Nigeria. BMC Public Health. 2007;7(1):1–13. doi:10.1186/1471-2458-7-354
48. Sserwanja Q, Musaba MW, Mutisya LM, Mukunya D. Rural-urban correlates of modern contraceptives utilization among adolescents in Zambia: a national cross-sectional survey. BMC Women’s Health. 2022;22(1):1–10. doi:10.1186/s12905-022-01914-8
49. Ajaero CK, Odimegwu C, Ajaero ID, Nwachukwu CA. Access to mass media messages, and use of family planning in Nigeria: a spatio-demographic analysis from the 2013 DHS. BMC Public Health. 2016;16(1):1–10. doi:10.1186/s12889-016-2979-z
50. Islam AZ, Mondal MNI, Khatun ML, et al. Prevalence and determinants of contraceptive use among employed and unemployed women in Bangladesh. Int J MCH AIDS. 2016;5(2):92. doi:10.21106/ijma.83
51. Anyatonwu OP, San Sebastián M. Rural-urban disparities in postpartum contraceptive use among women in Nigeria: a Blinder-Oaxaca decomposition analysis. Int J Equ Health. 2022;21(1):1–8. doi:10.1186/s12939-022-01674-9
52. Unumeri G, Ishaku S, Ahonsi B, Oginni A. Contraceptive use and its socio-economic determinants among women in North-East and North-West Regions of Nigeria: a comparative analysis. Afr Popul Stud. 2015;29:2.
53. Wado YD. Women’s autonomy and reproductive health-care-seeking behavior in Ethiopia. Women Health. 2018;58(7):729–743. doi:10.1080/03630242.2017.1353573
54. Shelley KD, Belete YW, Phiri SC, et al. Implementation of the community health assistant (CHA) cadre in Zambia: a process evaluation to guide future scale-up decisions. J Commun Health. 2016;41(2):398–408. doi:10.1007/s10900-015-0110-5
55. Zulu JM, Hurtig A-K, Kinsman J, Michelo C. Innovation in health service delivery: integrating community health assistants into the health system at district level in Zambia. BMC Health Serv Res. 2015;15(1):1–12. doi:10.1186/s12913-015-0696-4
56. Sano Y, Antabe R, Atuoye KN, Braimah JA, Galaa SZ, Luginaah I. Married women’s autonomy and post-delivery modern contraceptive use in the Democratic Republic of Congo. BMC Women’s Health. 2018;18(1):1–7. doi:10.1186/s12905-018-0540-1
57. Nalwadda G, Mirembe F, Byamugisha J, Faxelid E. Persistent high fertility in Uganda: young people recount obstacles and enabling factors to use of contraceptives. BMC Public Health. 2010;10(1):1–13. doi:10.1186/1471-2458-10-530
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
