Back to Journals » Risk Management and Healthcare Policy » Volume 17
Concomitant of Cryptococcal Meningitis and COVID-19 in a Female Patient with Primary Nephrotic Syndrome and Type 2 Diabetes
Received 27 November 2023
Accepted for publication 26 January 2024
Published 31 January 2024 Volume 2024:17 Pages 279—285
DOI https://doi.org/10.2147/RMHP.S451991
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jongwha Chang
Dongrui Liang,1 Xiaodong Li2
1 2nd Department of Ophthalmology, Baoding No.1 Central Hospital of Hebei Medical University, Baoding, Hebei, People’s Republic of China; 2Department of Nephrology, Baoding No.1 Central Hospital of Hebei Medical University, Baoding, Hebei, People’s Republic of China
Correspondence: Xiaodong Li, Department of Nephrology, Baoding No.1 Central Hospital of Hebei Medical University, No. 320, Great Wall North Street, Baoding, Hebei, 071000, People’s Republic of China, Email [email protected]
Background: Patients with primary nephrotic syndrome (PNS) are at an increased risk of developing various infections due to the long-term use of immunosuppressive agents. Cryptococcal meningitis (CM) is an uncommon but severe complication that can occur in patients with PNS, particularly those receiving immunosuppressive medications.
Case Description: This case report describes a middle-aged female patient with PNS and type 2 diabetes mellitus (T2DM) who developed CM. She received a combination regimen of cyclophosphamide and prednisone, achieving partial remission of PNS. However, she later returned to the hospital with high fever and headache. At admission, her nasopharyngeal swab test was positive for severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) and she received therapy of dexamethasone and favipiravir, but her fever and headache were not improved. Following a lumbar puncture was performed for her and CM was diagnosed based on a positive Cryptococcus culture in the cerebrospinal fluid. The patient’s cyclophosphamides were temporarily discontinued, and antifungal therapy with amphotericin B liposome and fluconazole was initiated. Despite a noticeable increase in her blood glucose levels due to infection during her hospitalization, she showed improvement with intensified glycemic control treatment. The anti-infection showed significant effectiveness, and the patient’s proteinuria remained stable during follow-up.
Conclusion: The patient with PNS and T2DM was concurrently diagnosed with both CM and coronavirus disease 2019 (COVID-19), marking the first reported case of such co-infections in these patients. Prompt diagnosis and appropriate antifungal therapy are crucial for improved outcomes of PNS patients with CM and COVID-19.
Keywords: cryptococcal meningitis, primary nephrotic syndrome, type 2 diabetes mellitus, COVID-19
Introduction
An important opportunistic pathogen called Cryptococcus neoformans typically affects those who have compromised immune systems.1–3 Among HIV-negative patients with cryptococcal infection, studies indicated that 41–61% of these patients received immunosuppressive drugs, and most had systemic lupus erythematosus and cancer, and only a few patients had primary nephrotic syndrome (PNS).4 Children with PNS were discovered to have a 36.6–38% probability of concurrent cryptococcal infection, and about 0.3% rate of cryptococcal meningitis (CM).5 In PNS patients, steroid or immunosuppressive medication results in immunologic dysfunction, which enhances the risk of infection.6
Immune dysfunction in type 2 diabetes mellitus (T2DM) substantially raises the likelihood of contracting and experiencing a resurgence of infection caused by Cryptococcus neoformans.7 Documentation on the risk factors and consequences of cryptococcosis in T2DM is lacking. A broad range of cryptococcal infections of differing severity occurs in T2DM, with a consistently high mortality rate.8
CM is a relatively unusual and deadly condition that primarily affects individuals with compromised immune systems. The clinical symptoms associated with CM are often vague and non-specific, making it difficult to promptly identify and diagnose the infection.9 Consequently, delayed diagnoses pave the way for the infection to advance and result in severe neurological complications. Herein, we provide a rare case that reported a middle-aged female with PNS and T2DM experienced concomitant of CM and coronavirus disease 2019 (COVID-19).
Case Description
A 57-year-old female patient complained with edema for 1 year and ardent fever for 3 days. She was diagnosed with T2DM 10 year ago. Based on the onset of her symptoms and laboratory test results, the patient was performed renal biopsy and diagnosed with membranoproliferative glomerulonephritis (MPGN) 1 year ago. Cyclophosphamide (100 mg/day) and prednisone (60 mg/day) were administered together in a combination regimen then. Following a partial remission of PNS, the prednisone dosage was steadily decreased to 20 mg/day within 6 months. Yet, the patient returned to our hospital because of high fever and headache 3 days ago. Physical examination at admission displayed the following: temperature of 38.8°C, blood pressure of 160/100 mmHg, negative meningeal irritation sign. The primary laboratory examination conducted at our hospital is detailed in Table 1. The results of lung imaging indicated normal findings, and there was no evidence of microbes in her blood samples. Non-contrast CT scan of the brain showed no evidence of abnormalities. Nevertheless, the patient tested positive for severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) through a nasopharyngeal swab reverse transcription-polymerase chain reaction (RT-PCR) test, leading to the initiation of treatment with dexamethasone and favipiravir for COVID-19. After 3 days, her fever showed no significant improvement and was accompanied by worsening headache. Physical examination revealed no apparent signs of meningeal irritation, so a neurologist was consulted to consider the possibility of meningitis. A lumbar puncture was performed for her and CM was diagnosed when a positive Cryptococcus culture was obtained in the cerebrospinal fluid (CSF) (Table 2). Further examination revealed her immune system compromised (Table 3). Cyclophosphamide for PNS were temporarily discontinued and prednisone was adjusted to 15 mg/day. Accordingly, amphotericin B liposome (60 mg, once a day) and fluconazole (200 mg, twice a day) were given for her then. We also administered symptomatic supportive treatment, which included improving her daily nutritional intake, giving her intravenous albumin and immunoglobulin, and managing her serum glucose and blood pressure levels. The patient continued to experience a persistent fever for 3 days, however, his body temperature gradually decreased and returned to normal after two weeks (Figure 1). In addition, we also observed a significant decrease in the lymphocyte counts of the patient upon admission, which returned to normal levels after two weeks of treatment (Figure 2). The patient’s hemoglobin A1c levels of admission were elevated, indicating her poor recent overall glucose control. Despite experiencing significantly elevated glucose levels upon admission, the patient’s glucose levels generally stabilized after receiving intensified glucose-lowering treatment. The results of the repeated lumbar puncture revealed a decrease in CSF pressure. The CSF appeared colorless and transparent, with no evidence of ink staining or fungal growth. Additionally, there was an improvement in the biochemical indicators of the CSF compared to previous results. Both the blood and CSF antigen titers for Cryptococcus neoformans were lower, indicating the effectiveness of the antifungal treatment for cryptococcosis. The patient experienced gastrointestinal adverse reactions during the antifungal medication process, including complaints of nausea and discomfort in the stomach. However, appropriate symptomatic treatment was provided, resulting in improvement. Then immunosuppressive agents were restarted at a low dosage due to her urinary proteins had obviously increased than before. Four weeks after discharge, her proteinuria was almost stable during the follow-up outpatient.
 |
Table 1 Lab Test in Our Hospital |
 |
Table 2 Cerebrospinal Fluid Test in Our Hospital |
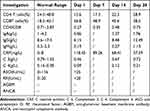 |
Table 3 Immunologic Test in Our Hospital |
 |
Figure 1 The fluctuations of the patient’s body temperature in hospital. |
 |
Figure 2 The changes of the patient’s serumlymphocytein hospital. |
Discussion
CM is unusual and frequently fatal complication in patients with chronic kidney disease.10–12The clinical features of CM are atypical, and if the diagnosis is usually neglected, the infection progresses untreated and neurological injury arises. Furthermore, there is limited information available about the clinical characteristics of PNS with CM to date. Typical clinical manifestations encompass nausea, vomiting, headache, signs of meningeal irritation, and fever, which was identified as an early and frequent indicator of CM.13 These symptoms are similar to those of other common infections, although fever may not be present in immunocompromised patients. Based on the extraction of Cryptococcus neoformans from the cerebrospinal fluid (CSF) or a positive India ink staining, CM was diagnosed.14 The opportunistic fungus pathogen Cryptococcus neoformans or Cryptococcus gattii, with C. neoformans predominating worldwide, causes CM, an infection of the meninges. CM is typically an immune-compromised condition with high morbidity and death rates, especially in those patients with HIV.15 Without anti-fungal therapy, the mortality rate in CM patients was reported to exceed 100%, and even after taking widely available anti-fungal medications, it can still be relatively high (20–60%).16 Moreover, widespread use of corticosteroids and other immunosuppressive medications, particularly broad-spectrum antibiotics, medical practitioners has steadily raised concerns about the occurrence of CM in the HIV-negative patients.12
Although immunosuppressive medications and corticosteroids are the primary treatment for PNS, these agents enhance immune system impairment. As a result, among those patients with PNS, infection is one of the most frequent complications, even CM, as well as invasive fungal infections. There have been some case reports of CM in PNS patients from various countries, with China having the majority of these reports due to the country’s high NS patient population.17 The induction, consolidation, and maintenance phases of CM treatment are designated in the updated Infectious Diseases Society of America recommendations published in 2010.18 For non-HIV and non-transplant patients, amphotericin B liposome plus 5-fluorocytosine is the optimum therapy option during the induction period.19 However, it is important to monitor and manage the potential side effects of these medications, including amphotericin B liposome, 5-fluorocytosine, and other anti-infective agents, during the treatment.
The 2016 Global Burden of Disease Study found that the number of global meningitis cases rose by 320,000 from 1990 to 2016. Current evidence suggests that diabetes may significantly increase the risk of meningitis, particularly in older adults.20 One specific fungal pathogen, Cryptococcus neoformans, is known to cause infection in immunocompromised individuals, including those with HIV, organ transplant recipients, hematological malignancies, and diabetes. Type 2 diabetes can compromise the immune system, especially when poorly controlled, potentially leading to the development of rare inflammatory diseases such as CM.21
This patient had a history of T2DM for many years. She was diagnosed with PNS and a renal biopsy confirmed her MPGN. She underwent long-term treatment with oral corticosteroids and cyclophosphamide. She complained with headache and high fever for this admission. After undergoing anti-infection treatment, the patient’s fever and headache showed no significant improvement. Therefore, clinically, the possibility of meningitis cannot be ruled out. A cerebrospinal fluid (CSF) test was conducted and indicated her CM. The treatment showed positive results, leading to improvement in the patient’s condition.
PNS is characterized by a range of clinical symptoms resulting from various glomerular disorders. These symptoms include significant proteinuria, reduced serum protein levels, excessive edema, elevated blood lipid levels, and ultimately a deficiency of immunoglobulins and complement proteins.22 Consequently, the immune system is compromised, leading to reduced effectiveness. While corticosteroids and immunosuppressive agents are the preferred medications for PNS management, they unintentionally further suppress the immune system, making infections a prevalent complication in PNS patients.23 The patient, who suffered from T2DM and PNS, had been receiving long-term oral administration of glucocorticoids and cyclophosphamide. Additionally, her glucose control was poor before admission. Both of them might lead to a significant decline in her immune function, which are the primary reason for her concurrent infections with COVID-19 and CM.
A retrospective study from China revealed that out of 226 patients with CM referred to the hospital, 29 were diagnosed with PNS.24 Among these 29 patients analyzed, 41.4% (12/29) were initially misdiagnosed with other complications. The overall mortality rate among these PNS patients with CM was 17.2% (5/29), with 60% (3/5) of the deceased patients being initially misdiagnosed. Treatment with amphotericin B plus 5-fluorocytosine (9/29) or amphotericin B plus fluconazole (7/29) effectively cleared the infection for these patients. Additionally, conducting repetitive testing is crucial for reaching a conclusive diagnosis in PNS patients suspected of having CM. Another study in China discovered that advanced age and elevated serum creatinine levels are risk factors contributing to the development of CM in PNS patients.25
To summarize, the clinical manifestations of PNS patients with CM can be complex and diverse. It is susceptible to misdiagnosis as tuberculous meningitis or viral meningitis. To avoid missed diagnoses, it is still crucial to inquire about the patient’s medical history in detail and pay attention to performing a lumbar puncture with ink staining of the cerebrospinal fluid. If necessary, repeated examinations should be performed to ensure accuracy.
Our study has some limitations. Firstly, we do not have access to the patient’s renal biopsy pathology images as the examination was conducted in another hospital, and the patient was unable to provide the original images. However, we obtained her renal pathological diagnosis report. Thus, this does not affect the subsequent treatment for the patient. Secondly, the treatment cycle for CM is relatively long. We found that our treatment was effective, but further follow-up is required to observe any adverse drug reactions and potential recurrence of CM in this patient.
Conclusion
To the best of our knowledge, this is the first reported case of a patient with T2DM and DM developed concomitant of CM and COVID-19. In conclusion, as the number of immunocompromised patients has increased, a concomitant rise in patient morbidity and mortality from fungus infections has been noticed. Due to their immunosuppression, PNS patients are more prone to developing infections than other ones. Moreover, clinicians should think about performing a lumbar puncture if necessary when treating patients with PNS who experience unexplained fever and headache. Healthcare providers should maintain a high index of suspicion for such infections in immunocompromised individuals, allowing for timely diagnosis and appropriate management strategies to be implemented.
Date Availability Statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Ethics Statement
The patient provided her written informed consent to participate in this study. Written informed consent was obtained from the individual for the publication of any potentially identifiable images or data included in this article.
Acknowledgment
We acknowledge the contributions of the colleagues in Baoding No.1 Central Hospital that aided the efforts of the authors.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval for the version to be published; and agreed to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Iyer KR, Revie NM, Fu C, et al. Treatment strategies for cryptococcal infection: challenges, advances and future outlook. Nat Rev Microbiol. 2021;19(7):454–466. doi:10.1038/s41579-021-00511-0
2. Fisher KM, Montrief T, Ramzy M, et al. Cryptococcal meningitis: a review for emergency clinicians. Intern Emerg Med. 2021;16(4):1031–1042. doi:10.1007/s11739-020-02619-2
3. Temfack E, Boyer-Chammard T, Lawrence D, et al. New insights into Cryptococcus spp. biology and cryptococcal meningitis. Curr Neurol Neurosci Rep. 2019;19(10):81. doi:10.1007/s11910-019-0993-0
4. Ma H, Wang X, Yan H, et al. Dual intracranial infection with nocardia farcinica and Cryptococcus neoformans diagnosed by next-generation sequencing in a patient with nephrotic syndrome: a case report. Medicine. 2022;101(35):e30325. doi:10.1097/MD.0000000000030325
5. Nagotkar L, Shanbag P, Mauskar A, et al. Fulminant intracranial hypertension due to cryptococcal meningitis in a child with nephrotic syndrome. Indian J Crit Care Med. 2011;15(3):176–178. doi:10.4103/0972-5229.84905
6. Qu J, Zhou T, Zhong C, et al. Comparison of clinical features and prognostic factors in HIV-negative adults with cryptococcal meningitis and tuberculous meningitis: a retrospective study. BMC Infect Dis. 2017;17(1):51. doi:10.1186/s12879-016-2126-6
7. Lao M, Li C, Li J, et al. Opportunistic invasive fungal disease in patients with type 2 diabetes mellitus from Southern China: clinical features and associated factors. J Diabetes Investig. 2020;11(3):731–744. doi:10.1111/jdi.13183
8. Nsenga L, Kajjimu J, Olum R, et al. Cryptococcosis complicating diabetes mellitus: a scoping review. Ther Adv Infect Dis. 2021;8:20499361211014769. doi:10.1177/20499361211014769
9. Temfack E, Rim JJB, Spijker R, et al. Cryptococcal antigen in serum and cerebrospinal fluid for detecting cryptococcal meningitis in adults living with human immunodeficiency virus: systematic review and meta-analysis of diagnostic test accuracy studies. Clin Infect Dis. 2021;72(7):1268–1278. doi:10.1093/cid/ciaa1243
10. Li Z, Liu Y, Chong Y, et al. Fluconazole plus flucytosine is a good alternative therapy for non-HIV and non-transplant-associated cryptococcal meningitis: a retrospective cohort study. Mycoses. 2019;62(8):686–691. doi:10.1111/myc.12944
11. Chen J, Chen P. Cryptococcal meningitis in patients with lupus nephritis. Clin Rheumatol. 2020;39(2):407–412. doi:10.1007/s10067-019-04844-3
12. Liang L, Liang Z, She D, et al. A case-control study of human immunodeficiency virus-negative patients with cryptococcemia and cryptococcal meningitis in a Chinese tertiary care hospital during 10 years. J Int Med Res. 2021;49(1):300060520984658. doi:10.1177/0300060520984658
13. Murphy LS, Lacy AJ, Smith AT, et al. Cryptococcal meningitis in an immunocompetent patient. Am J Emerg Med. 2020;38(11):
14. Liu J, Li M, Liang JY, et al. Autoimmune diseases in HIV-negative cryptococcal meningitis. Future Microbiol. 2021;16(16):1251–1259. doi:10.2217/fmb-2020-0318
15. Wykowski J, Galagan SR, Govere S, et al. Cryptococcal antigenemia is associated with meningitis or death in HIV-infected adults with CD4 100–200 cells/mm3. BMC Infect Dis. 2020;20(1):61. doi:10.1186/s12879-020-4798-1
16. Ngan NTT, Flower B, Day JN. Treatment of cryptococcal meningitis: how have we got here and where are we going? Drugs. 2022;82(12):1237–1249. doi:10.1007/s40265-022-01757-5
17. Li J, Zhang Q, Su B. Clinical characteristics and risk factors of severe infections in hospitalized adult patients with primary nephrotic syndrome. J Int Med Res. 2017;45(6):2139–2145. doi:10.1177/0300060517715339
18. Moosa MS, Lessells RJ. Toward simpler, safer treatment of cryptococcal meningitis. N Engl J Med. 2022;386(12):1179–1181. doi:10.1056/NEJMe2201150
19. Loyse A, Burry J, Cohn J, et al. Leave no one behind: response to new evidence and guidelines for the management of cryptococcal meningitis in low-income and middle-income countries. Lancet Infect Dis. 2019;19(4):e143–e147. doi:10.1016/S1473-3099(18)30493-6
20. Acharya R, Khanal K, Upadhyaya P, et al. Diabetes mellitus as a risk factor for cryptococcal meningitis in immunocompetent. IDCases. 2020;22:e00988. doi:10.1016/j.idcr.2020.e00988
21. Horiya M, Anno T, Kawada M, et al. Pyogenic psoas abscess on the dorsal side, and bacterial meningitis and spinal epidural abscess on the ventral side, both of which were induced by spontaneous discitis in a patient with diabetes mellitus: a case report. J Diabetes Investig. 2021;12(7):1301–1305. doi:10.1111/jdi.13461
22. Viallard JF. Management of hypogammaglobulinemia. Rev Med Interne. 2023;44(3):133–138. French. doi:10.1016/j.revmed.2023.01.010
23. Constantinescu AR, Mattoo TK, Smoyer WE, et al. Clinical presentation and management of nephrotic syndrome in the first year of life: a report from the pediatric nephrology research consortium. Front Pediatr. 2022;10:988945. doi:10.3389/fped.2022.988945
24. Hu D, Zhang Q, Jiang W, et al. Cryptococcal meningitis: a rare complication in HIV-negative patients with nephrotic syndrome in A Chinese teaching hospital. Mycopathologia. 2020;185(6):959–969. doi:10.1007/s11046-020-00482-5
25. Su B, Zhang Q, Lv J. Cryptococcal meningitis in adult patients with primary nephrotic syndrome. Clin Nephrol. 2018;90(6):390–395. doi:10.5414/CN109384
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
