Back to Journals » Clinical Ophthalmology » Volume 18
Comparison of the Residual Amount of an Ophthalmic Viscosurgical Device Among Different Types of Intraocular Lens Implants in vitro
Authors Oki T , Horiguchi H, Terauchi R, Gunji H, Nakano T
Received 14 February 2024
Accepted for publication 17 April 2024
Published 20 April 2024 Volume 2024:18 Pages 1083—1091
DOI https://doi.org/10.2147/OPTH.S458348
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Tetsutaro Oki, Hiroshi Horiguchi, Ryo Terauchi, Hisato Gunji, Tadashi Nakano
Department of Ophthalmology, The Jikei University School of Medicine, Minatoku, Tokyo, 105-8461, Japan
Correspondence: Tetsutaro Oki, Department of Ophthalmology, The Jikei University School of Medicine, 3-25-8, Nishi-shinbashi, Minatoku, Tokyo, 105-8461, Japan, Email [email protected]
Purpose: Although ophthalmic viscosurgical devices are quite important for safe cataract surgery, currently, postoperative residual ophthalmic viscosurgical devices can cause various complications. Previously, we developed a method to visualize residual ophthalmic viscosurgical devices after irrigation/aspiration in vitro and found that the amount of residual ophthalmic viscosurgical device on a single-piece intraocular lens was greater than that on a three-piece intraocular lens. In the present study, we compared the amounts of residual ophthalmic viscosurgical device among various foldable intraocular lenses to investigate the factors that determine the quantity of residual ophthalmic viscosurgical device.
Patients and Methods: Simulated cataract surgery was performed in pig eyes using an ophthalmic viscosurgical device labeled with fluorescent silica particles. After the simulated surgery procedure, the fluorescent silica attached to the intraocular lens was observed and quantified by inductively coupled plasma-atomic emission spectrometry after intraocular lens removal. The amount of residual ophthalmic viscosurgical device was compared among five representative single-piece intraocular lenses and one three-piece intraocular lens.
Results: The distribution and amount of the residual ophthalmic viscosurgical device differed for each intraocular lens. The amount of silicon in the lens capsule differed among the intraocular lens types.
Conclusion: The postoperative residual tendency of ophthalmic viscosurgical devices differed among various single-piece intraocular lenses. The behavior of the intraocular lenses within the capsule affected the residual tendency. The removal of ophthalmic viscosurgical device in the lens capsule should be tailored for each intraocular lens to improve efficiency.
Keywords: cataract surgery, intraocular lens, ophthalmic viscosurgical devices
Introduction
In cataract surgery, ophthalmic viscosurgical devices (OVDs) are injected inside the anterior chamber, where they perform various functions, such as facilitating continuous curvilinear capsulorhexis (CCC), protecting the corneal endothelium, and expanding the capsule during insertion of an intraocular lens (IOL).1,2 OVDs are polymer gels composed mainly of hyaluronic acid and ingredients, such as sodium chloride, disodium hydrogen phosphate hydrate, sodium dihydrogen phosphate, sodium phosphate, and a pH adjuster; they are used in ophthalmology and other specialties, such as orthopedics and plastic surgery. OVDs are not toxic to the human body,3,4 but after cataract surgery, various complications are caused by residual OVDs in the capsule. These include high intraocular pressure, IOL dislocation/displacement, endophthalmitis due to bacteria entering the eye with OVD, and toxic anterior segment syndrome.4–10
Therefore, cataract surgeons must pay close attention to postoperative residual OVDs in the eye. OVD is a colorless and transparent substance, but its presence can be recognized by its fluidity and texture if there is ample quantity in the capsule. However, it becomes difficult to determine when the amount remaining in the capsule is small owing to intraoperative irrigation and aspiration (I/A). Therefore, the OVD aspiration time depends on the surgeon’s timing based on experience.
To verify the efficiency of OVD removal, various methods to visualize OVDs, such as using OVDs mixed with sodium fluorescein and measuring the time required for removal, have been proposed.11–15 These methods are useful because they allow visualization of residual OVDs after I/A completion. However, the quantification of the actual amount of residual OVDs still remains an issue. Therefore, we developed a method to quantify the residual amount of OVD in the capsule.16 In vitro cataract surgery was performed using OVD mixed with a fluorescent dye labeled with fluorescent silica particles. After IOL insertion and subsequent I/A, the distribution of residual OVD in the capsular bag was objectively observed using ultraviolet (UV) light.16 In this previous study, photographs of the labeled residual OVD in IOL obtained using UV light revealed that OVD tended to remain at the center of the optic of the single-piece IOL. In addition, a comparison of single-piece IOLs and three-piece IOLs using an indirect quantification method devised by us revealed that OVD tended to remain more in the single-piece IOLs. Thus, it was considered that the difference in the amount of residual OVD could be attributed to differences in behavior during I/A owing to differences in the shape and stiffness of the IOLs.
Therefore, in the present study, we focused on the time taken by the IOL to expand from its folded state within the capsule when it is inserted intraocularly. During the actual surgery, the surgeon terminates the IA after subjectively judging that the OVD in the sac has been removed, and the early or late deployment time of the capsule may affect the surgeon’s judgment. Therefore, we compared the IA time for each IOL during the simulated surgery, indirectly quantified the amount of residual OVD, and measured the average spontaneous deployment time for each IOL in a simulated eye.
Materials and Methods
This study was led by a physician (T.O.) approved to conduct animal experiments in accordance with the ethical code established by the Jikei University School of Medicine.
The experiments were performed using previously published methods.16 Fluorescent silica particles (micromod Partikeltechnologie GmbH, Rostock, Germany) were used as OVD labels. Fluorescein isothiocyanate (excitation wavelength, 485 nm; emission wavelength, 515 nm) was encapsulated in silica shells with a 30-nm diameter and dispersed in a buffer solution with a density of 1 g/mL at a concentration of 100 mg/mL.
This was mixed with Healon (Johnson & Johnson, Chicago, IL, USA), a cohesive-type OVD, and the weight concentration of silicon (Assia, #9) was adjusted to 18.90 mg/g. This OVD was designated as a labeled OVD. Although the labeled OVD was initially pale yellow, its transparency became equivalent to that of a normal OVD during I/A in the capsular bag. Therefore, when labeled OVD was used, I/A duration could be left to the surgeon’s judgment, as in actual cataract surgery, since there was no color visible to aid in determining residual OVD.
A total of 30 ex vivo pig eyes were used. Experiments were conducted using six different IOLs, including five single-piece IOLs and one three-piece IOL, made of the same material (hydrophobic acrylic). We used the following IOLs: YA-60BBR, comprising a hydrophobic acrylic optic with poly(methyl methacrylate) (PMMA) haptics, a refractive index of 1.52, and an overall length of 12.5 mm (HOYA Co., Tokyo, Japan); iSert micro 255, comprising a hydrophobic acrylic optic and hydrophobic acrylic chemically bonded to blue PMMA haptic tips, with a refractive index of 1.52 and an overall length of 12.5 mm (HOYA Co.); SZ-1, comprising a yellow-tinted, hydrophobic, soft acrylic optic and haptics in the same material. A refractive index of 1.52, and an overall length of 13.0 mm (NIDEK Co., Tokyo, Japan); SN60WF, comprising hydrophobic acrylate/methacrylate copolymer optic and haptics, with a refractive index of 1.55 and overall length of 13.0 mm (Alcon, Inc., Geneva, Switzerland); ZCB00V, a hydrophobic, soft acrylic optic with haptics in the same material, a refractive index of 1.47, and an overall length of 13.0 mm (Johnson & Johnson); and W60, comprising a cross-linked acrylic ester copolymer optic and haptics in the same material, with a refractive index of 1.54 and an overall length of 12.5 mm (Santen Pharmaceutical Co., Ltd., Tokyo, Japan). The procedure was repeated five times for each IOL type, creating a group for each.
A 2.4-mm corneal incision was made using a slit knife (MANY INC, Tochigi pref., Japan), and a 5.6-mm CCC was created using a corneal CCC marker (M.E. Technica, Hokkaido, Japan). Phacoemulsification was performed using the ophthalmic small incision surgery system OS3 (Oertli Instrumente AG, Berneck, Switzerland) with the following parameters: power, 50%; flow rate, 25 mL/min; aspiration pressure, 400 mmHg; perfusion bottle height (intraocular pressure: IOP), 60 cm. Since the objective was to determine the amount of residual OVD in the lens capsule after surgery, an unlabeled OVD was injected into the anterior chamber to distinguish it from the labeled OVD in the capsule. To prevent misidentification, a different product with the same viscosity as that of Healon was used in the anterior chamber: Suvenyl 1% sodium hyaluronate, a cohesive OVD (Chugai Pharmaceutical Co., Ltd., Tokyo, Japan) with an average molecular weight of 1.5–3.9 million. After lens removal, the labeled OVD was injected into the capsule. The IOL was inserted into the capsule using a labeled OVD and an IOL-specific injector (YA-60BBR used the HOYA injector system and the E1 cartridge (HOYA Co., Tokyo, Japan). W60 used Accuject UniFit: WJ60M (Santen Pharmaceutical Co., Ltd.). Other IOLs used preset type injectors. Then, I/A was performed with the following parameters: flow rate, 25 mL/min; aspiration pressure, 400 mmHg; perfusion bottle height, 10 cm.
The I/A tip was pressed on the anterior surface of the IOL, and the tip was inserted behind the IOL until the surgeon confirmed the complete removal of the OVD.17 The I/A duration was measured and compared using a one-way analysis of variance (mean ± standard deviation; α = 0.05).
After IOL insertion, an incision was made at the posterior pole so that no load was applied to the resulting specimen. Then, the posterior pole was removed with surgical scissors. There was no convection of the fluid component in the anterior chamber and capsule, with no IOL dislocation. The specimen was prepared using an operating microscope (OPMI-1 FR, Carl Zeiss Meditec, AG, Jena, Germany), irradiated with UV light from behind, and observed in Miyake–Apple view18 using a digital camera (FDR-AX 30; SONY Co., Ltd., Tokyo, Japan) (Figure 1A). In our previous study,16 the labeled OVDs were visualized under UV light, and we observed that parts of the capsular bag and the single-and three-piece IOLs were prone to OVD retention. In the present study, we used the same methods to visualize the retention tendency of various single-piece IOLs (Figure 1B). The residual amount and distribution of OVD in the lens capsule were evaluated. The lens capsules were then removed from the specimens; for the experiments, five capsules were used for each IOL type. The capsules were completely dissolved in hydrogen fluoride using microwave irradiation (maximum temperature, 220°C), and the volume was fixed to 25 mL by adding ultrapure water. The Si concentration was determined by injecting the sample into an inductively coupled plasma atomic emission spectrometry analyzer (ICP-AES; Hitachi High-Tech Science Corporation SPS-3520UV Tokyo, Japan). The test was conducted thrice. Since the analytical solution had a fixed volume, the Si weight could be calculated from the analytical result (Si concentration). The amount of Si dissolved in the analysis solution was equivalent to five capsules. Thus, it was possible to calculate the average Si weight per capsule. Since the Si concentration of the labeled OVD injected into the capsule was known, the residual OVD weight relative to the residual Si weight was calculated.
To compare the observations, a lens capsule, in which only a labeled OVD was injected, was prepared, and I/A was performed without IOL insertion. All surgeries were performed by the same surgeon (T.O.), and the volumes of residual OVDs were expressed as mean ± standard deviation values. The results underwent multiple comparisons using the Tukey honestly significant difference (HSD) test (α = 0.05). All statistical analyses were performed using R software (The R Foundation for Statistical Computing, Vienna, Austria). The level of significance was set at P < 0.05.
As an additional experiment, a mock lens capsule was created. The expansion of IOLs used in the experiment was observed under constant conditions and constant temperature, and the amount of OVD remaining was compared among the IOLs to determine factors affecting the amount of residual OVD in IOLs of the same shape. First, the room temperature was set to 25°C. A transparent palette was prepared, and an O-ring (13-mm diameter) was placed in the center. The palette was filled with normal saline solution (adjusted using a digital thermometer [TANITA CORPORATION, Tokyo, Japan] to 25°C), OVD (at room temperature, 25°C) was used to fill the O-ring, and each IOL was set and inserted using OVD. The deployment time was defined as the time it took for the haptics at both ends to reach the inner wall of the O-ring, and the process was video recorded. The deployment time was measured from the obtained video. The experiment was performed five times for each IOL. The obtained deployment times were statistically compared. Given the small sample size, a non-parametric test was used. Statistical tests were performed using “R” using the Steel–Dwass test.
Results
Five simulated cataract surgeries were performed with each of the six IOLs. After performing cataract surgery in a simulated porcine eye, we visualized and quantified the amount of residual OVD with fluorescent Si. The observed images of each representative IOL after I/A completion with the behind-The-bag technique are shown in Figure 2. In the three-piece IOL YA-60BBR, striated residual OVD was observed on the posterior capsule and outside the lens optics; in iSert micro 255 and SZ-1, striated residual OVD was observed in the center of the optics; in W60, ZCB00V, and SN60WF, OVD was observed sparsely over the entire lens sac. In the control group, it was difficult to observe residual OVD.
Next, we quantified the amount of residual OVDs using an ICP-AES analyzer. For each IOL used in the simulated surgery, the lens capsule of each of the five eyes was lysed, and samples were prepared by adding ultrapure water. Similarly, samples were prepared from the lens capsule of the control group. The obtained samples were measured three times each. The residual amount of OVD per lens capsule was calculated from the analyzed Si concentration and Si concentration (18.89 mg/g) of fluorescent silica nanobeads mixed OVD used for the simulated surgery. The results were as follows: 232.0 ± 4.5, 243.1 ± 1.3, 383.8 ± 11.1, 536.1 ± 6.6, 554.7 ± 8.2, and 578.9 ± 11.2 μg for SZ-1, YA-60BBR, iSert micro 255, ZCB00V, SN60WF, and W60, respectively (Table 1). Each group underwent multiple comparisons. The comparisons were performed using the Tukey HSD test (α = 0.05). The residual amount of OVD was significantly different among all IOLs except between the YA-60BBR and SZ-1 groups and between the SN60WF and ZCB00V groups.
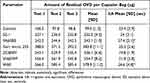 |
Table 1 Ophthalmic Viscosurgical Device |
To align the conditions with those of the actual surgery, I/A was performed until the surgeon decided that he had removed enough OVD. The mean ± standard deviation values of the duration of I/A in the capsule with the inserted IOL was 24.0 ± 3.1, 27.4 ± 2.1, 25.2 ± 2.6, 19.8 ± 1.9, 21.8 ± 2.8, and 26.6 ± 4.8 s for SZ-1, YA-60BBR, iSert micro 255, ZCB00V, SN60WF, and W60, respectively, with significant between-group differences (P = 0.004, one-way analysis of variance). Each group also underwent multiple comparisons. The duration of I/A in the ZCB00V group was significantly shorter than that in the YA-60BBR (P = 0.007) and W60 groups (P = 0.02).
Assuming that the expansion time of each IOL could affect the amount of residual OVD, a simulated lens capsule was created, the deployment of the IOLs used in the experiment was observed under constant conditions and temperature, and the natural deployment time of each IOL was measured. Measurements were taken 10 times for each IOL, and the average deployment time was calculated. The results are shown in Figure 3. The mean ± standard deviation values of deployment times for each IOL were 10.2 ± 1.6, 0, 40.1 ± 3.3, 54.6 ± 3.3, 37.8 ± 2.9, and 60.7 ± 3.7 s for SZ-1, YA-60BBR, iSert micro 255, ZCB00V, SN60WF, and W60, respectively. While there was no statistically significant difference between the SN60WF and iSert micro 255 groups (P = 0.75, Steel–Dwass test), there was a statistically significant difference in deployment time between the other groups. Correlations between the mean I/A time and mean deployment time and the amount of residual OVD for each IOL were examined. Statistics were based on an analysis of covariance. The results showed that there was no significant difference in the effect of I/A time on the amount of residual OVD (P = 0.14) and suggested that the IOL deployment time could be an influencing factor (P < 0.05). We hypothesized that the time it takes for the IOL to deploy in the eye might be related to the amount of residual OVD.
Discussion
Summary of Results
In the present study, using a method for indirectly quantifying OVD by labeling the OVD with known chemical substances, based on our previous study,16 we compared the amounts of residual OVDs in single-piece IOLs made by five different manufacturers. We observed that the distribution tendency of residual OVDs in the sac differed depending on the IOL type, and the amounts of residual OVDs in the five types of single-piece IOLs were different even for the same type of IOLs. Furthermore, we found that IOL deployment time could influence the residual amount of the OVD.
Factors Affecting the Amount of Residual OVDs
Efficient I/A methods for OVD removal and differences in their removal efficiencies owing to differences in molecular weights of OVDs have been discussed.12–15 However, there is no consensus on the I/A time required to remove aggregated OVDs filled in the intraocular lens capsule at the time of IOL insertion. In the present study, the actual I/A time that was determined by the surgeon did not affect the amount of residual OVDs. All of the five different types of single-piece IOLs used in this study had the optics and haptic optic portions in one piece, but each had a different refractive index and glass transition temperature, and some IOLs had a coating on the surface. Some IOLs had design information disclosed on IOL coatings, while others did not. Coatings on optical surfaces may affect the affinity between IOLs and OVDs, and the possibility that these characteristics indirectly affect the tendency and amount of residual OVDs needs to be investigated in the future. Moreover, differences in the shape of the injector might have affected the way the IOL folded as it passed through the injector, and differences in the way the IOL folded might have affected not only the amount of OVD filled into the injector that was inserted into the eye with the IOL but also the way the IOL unfolded in the lens sac. As a result, the shape of the injector might have affected the amount of residual OVD. This observation should be verified with future studies that will use the same injector.
Convection occurring in the lens capsule during I/A has been reported previously, indicating that convection of I/A in the capsule affects the behavior of the IOL.19,20 It has also been documented that during the actual I/A procedure, the IOL rotates while unfolding in the lens capsule.21 In a previous report, we mentioned that the behavior of the IOL within the lens sac during I/A might affect the amount of residual OVD.16 We hypothesized that IOL behavior would be affected by differences in haptic geometry. In the present study, we used five different IOLs with the same shape but different hardness and coating and considered that not only the shape of the support but also the deployment time and additional characteristics might affect the behavior of the IOL in the capsule. The results show that the residual tendency of OVDs is influenced by the characteristics of IOLs. Particularly, it was considered that the OVD tended to stay between the center of the optical part of the IOL, which was the center of rotation of the IOL, and the center of the posterior capsule and the optical part, from where it was difficult to aspirate the OVD.
It has also been reported that incomplete removal of OVDs can induce high intraocular pressure and inflammation postoperatively4–8,10 and that the risk of developing complications may be reduced by devising a method to remove OVDs.10 Understanding the characteristics and causes of residual OVD after cataract surgery is important for improving surgical techniques, devising more efficient methods of OVD removal, and avoiding complications related to residual OVD.
Future Direction and Limitations
In recent years, femtosecond laser-based cataract surgery has made it possible to automate the creation of anterior capsulotomy and corneal incision wounds using machines, which were previously performed manually. Currently, machines and injectors can also semi-automate perform IOL insertion. Advances in surgical machines and artificial intelligence may improve intraoperative safety, including safety during I/A, and reduce intraoperative variability in surgical procedures if cataract surgery becomes more automated. The present study suggests that effective I/A may require not only uniform methods but also different methods for different IOLs. Future discussion of these issues may lead to more effective automated programs.
However, the present study had some limitations. To approximate the actual surgical situation, I/A time was determined by the surgeon subjectively when it was deemed sufficient; I/A and OVD removal procedures are usually performed based on the subjective judgment of the surgeon. As it is difficult to standardize the surgeons’ techniques in actual cataract surgery, the technique used in the present study may not be used in all cataract surgeries. All data used to quantify the residual amount of OVD were from experiments on porcine eyes. In actual cataract surgery, not only the IOL and aspiration technique but also the condition of the lens capsule, such as the strength of the zonular fibers, may be factors related to the occurrence of residual OVD. Additionally, only Healon OVDs were used in this study. Although high-molecular-weight OVDs, such as the Healon OVD, are commonly employed during the insertion of IOLs, the definition of residual OVD during actual surgery should consider combinations with other types of OVDs as well. Future research should be conducted to investigate the effects of various other OVDs.
Conclusions
In this study, we compared the amounts of residual OVD after insertion of monofocal IOLs from different manufacturers, revealing variations based on IOL type and even within the same IOL type. In addition, we discovered that the deployment time of IOLs may influence the amount of residual OVD. Factors such as the integration of the optic and haptic parts of IOLs, refractive index, glass transition temperature, and surface coatings may also affect residual OVD levels. This study suggests the importance of understanding residual OVD characteristics and its causes after cataract surgery to improve surgical techniques, develop more efficient OVD-removal methods, and prevent complications related to residual OVDs.
Data Sharing Statement
The datasets generated during the current study are not publicly available but are available from the corresponding author on reasonable request.
Acknowledgments
The authors would like to thank Dr. Mizobuchi for useful discussions on this research.
The study ”Comparison of the residual amount of an ophthalmic viscosurgical device with different types of intraocular lens implants in vitro” was presented at the 30th annual meeting of the Japanese Society of Cataract Refractive Surgery, Tokyo, Japan, in June 2015.
Funding
This study did not receive any financial support.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Arshinoff SA, Jafari M. New classification of ophthalmic viscosurgical devices--2005. J Cataract Refract Surg. 2005;31:2167–2171. doi:10.1016/j.jcrs.2005.08.056
2. Higashide T, Sugiyama K. Use of viscoelastic substance in ophthalmic surgery - focus on sodium hyaluronate. Clin Ophthalmol. 2008;2:21–30.
3. Gerberich AJ, Ipema HJ. A primer on ocular viscosurgical devices. Am J Health Syst Pharm. 2021;78:2020–2032.
4. Steiner RF. Ophthalmic viscosurgical devices: physical characteristics, clinical applications, and complications. In: Cataract Surgery.
5. Sholohov G, Levartovsky S. Retained ophthalmic viscosurgical device material in the capsular bag 6 months after phacoemulsification. J Cataract Refract Surg. 2005;31:627–629.
6. Miller KM, Oetting TA, Tweeten JP, et al. Cataract in the adult eye preferred practice pattern. Ophthalmology. 2022;129:P1–P126.
7. Mamalis N, Edelhauser HF, Dawson DG, Chew J, LeBoyer RM, Werner L. Toxic anterior segment syndrome. J Cataract Refract Surg. 2006;32:324–333.
8. Durand ML. Endophthalmitis. Clin Microbiol Infect. 2013;19:227–234.
9. Shimada H, Arai S, Nakashizuka H, Hattori T, Yuzawa M. Reduction of anterior chamber contamination rate after cataract surgery by intraoperative surface irrigation with 0.25% povidone-iodine. Am J Ophthalmol. 2011;151:11–17.e1.
10. Oshika T, Ohashi Y. Endophthalmitis after cataract surgery: effect of behind-The-lens washout. J Cataract Refract Surg. 2017;43:1399–1405. doi:10.1016/j.jcrs.2017.08.009
11. Auffarth GU, Holzer MP, Vissesook N, Apple DJ, Völcker HE. Removal times and techniques of a viscoadaptive ophthalmic viscosurgical device. J Cataract Refract Surg. 2004;30:879–883. doi:10.1016/j.jcrs.2003.08.031
12. Auffarth GU, Holzer MP, Visessook N, Apple DJ, Völcker HE. Removal times for a dispersive and a cohesive ophthalmic viscosurgical device correlated with intraocular lens material. J Cataract Refract Surg. 2004;30:2410–2414. doi:10.1016/j.jcrs.2004.03.039
13. Assia EI, Apple DJ, Lim ES, Morgan RC, Tsai JC. Removal of viscoelastic materials after experimental cataract surgery in vitro. J Cataract Refract Surg. 1992;18:3–6. doi:10.1016/S0886-3350(13)80376-8
14. Bissen-Miyajima H. In vitro behavior of ophthalmic viscosurgical devices during phacoemulsification. J Cataract Refract Surg. 2006;32:1026–1031. doi:10.1016/j.jcrs.2006.02.039
15. Oshika T, Okamoto F, Kaji Y, et al. Retention and removal of a new viscous dispersive ophthalmic viscosurgical device during cataract surgery in animal eyes. Br J Ophthalmol. 2006;90:485–487. doi:10.1136/bjo.2005.085969
16. Gunji H, Ohki T. Quantification of residual ophthalmic viscosurgical device after irrigation/aspiration in experimental cataract surgery in vitro. J Cataract Refract Surg. 2019;45:1324–1329. doi:10.1016/j.jcrs.2019.03.025
17. Mitani A, Suzuki T, Tasaka Y, et al. Evaluation of a new method of irrigation and aspiration for removal of ophthalmic viscoelastic device during cataract surgery in a porcine model. BMC Ophthalmol. 2014;14:129.
18. Pereira FA, Werner L, Milverton EJ, Coroneo MT. Miyake-Apple posterior video analysis/photographic technique. J Cataract Refract Surg. 2009;35:577–587.
19. Abouali O, Bayatpour D, Ghaffariyeh A, Ahmadi G. Simulation of flow field during irrigation/aspiration in phacoemulsification using computational fluid dynamics. J Cataract Refract Surg. 2011;37:1530–1538.
20. Kaji Y, Yamashita M, Sakakibara J, Oshika T. Visualization of irrigation fluid flow and calculation of its velocity distribution in the anterior chamber by particle image velocimetry. Graefes Arch Clin Exp Ophthalmol. 2012;250:1023–1027.
21. Hyon JY, Yeo HE. Rotational stability of a single-piece hydrophobic acrylic intraocular lens during removal of ophthalmic viscosurgical devices. Am J Ophthalmol. 2010;149:253–257.e1.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



