Back to Journals » Veterinary Medicine: Research and Reports » Volume 14
Comparison of Aural and Rectal Temperature in Dogs Presenting to an Emergency Room
Authors Smith R, Mastrocco A, Prittie J, Weltman J
Received 4 April 2023
Accepted for publication 15 July 2023
Published 26 July 2023 Volume 2023:14 Pages 125—131
DOI https://doi.org/10.2147/VMRR.S411935
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Young Lyoo
Rebecca Smith, Alicia Mastrocco, Jennifer Prittie, Joel Weltman
Department of Emergency and Critical Care, Animal Medical Center, New York, NY, USA
Correspondence: Rebecca Smith, Animal Medical Center, 510 E 62nd Street, New York, NY, 10065, Tel +1-908-246-7580, Email [email protected]
Purpose: To compare rectal and aural temperatures in canines presenting to a small animal emergency room.
Patients and Methods: We performed a prospective cohort study conducted between June 2022 and October 2022. One hundred and fifty-two dogs were evaluated that were presented to a private practice emergency room. Temperatures were obtained on presentation using both an aural Braun ExacTemp and a rectal Vet-Temp Rapid Digital Thermometer. The order of temperature measurement was randomized and recorded. Dogs were classified into three groups based on recorded temperature; normothermic (n = 105), hypothermic (n = 24), and hyperthermic (n = 23). Additional recorded parameters included: patient signalment, heart rate, respiratory rate, presence or absence of aural debris, coat length (classified as short, medium or long), body weight, body condition score, pain score, as well as venous lactate and non-invasive blood pressure, if performed.
Results: The overall aural temperatures were significantly lower than rectal temperatures. The average rectal and aural temperatures were 38.7°C (range 36.6– 40.7°C) and 38.3°C (range 35.7°C– 40.4°C), respectively. Among all canines, there was a moderate, statistically significant relationship between rectal and aural temperatures (r = 0.636; p < 0.001) and this relationship remained significant with a weaker relationship for normothermic dogs (r = 0.411; p < 0.001). For hyperthermic and hypothermic dogs, there was not a statistically significant relationship between rectal and aural temperatures. Hyperthermic dogs had a significantly higher respiratory rate than other groups and hypothermic dogs were more likely to have a short haircoat. Lastly, ambient temperature, but not humidity, influenced patient temperature.
Conclusion: Our study found aural temperatures were consistently lower than rectal temperatures in dogs with both normal and abnormal rectal temperatures. Aural thermometry may not be an acceptable method of temperature measurement in the emergency patient cohort.
Keywords: emergency, dogs, temperature, aural
Introduction
Evaluation of body temperature is an integral component of the physical exam. Currently, rectal temperature (RT) measurement is the gold standard in conscious veterinary patients.1 RT in these animals correlates well with the core body temperature as measured via more invasive techniques (ie, esophageal temperature and pulmonary arterial temperature).2 However, rectal thermometry has several disadvantages, including contribution to patient stress, potential for patient injury, and prolonged time for measurement compared to alternative non-invasive measures, such as aural or corneal temperature.1,3,4 Moreover, RT may be affected by the presence of feces, rectal diseases or tumors, and alterations in local blood flow in shock states.5
As the tympanic membrane shares blood flow with the hypothalamus, aural temperature (AT) measurement might be more representative of vital organ temperature than RT in the setting of hemodynamic compromise.6 AT is reportedly unaffected by the presence of aural debris or otitis externa in dogs.7 Veterinary studies evaluating AT in healthy anesthetized and hospitalized dogs have demonstrated variable reliability of ATs across reports.3,4,8–10 In the studies that showed poor correlation between these measurement techniques, AT underestimated RT.3,8,10,11
The reliability of aural thermometry in veterinary medicine remains controversial, and studies on its use in hyper- and hypothermic patients are few.8,9 Further, to the authors’ knowledge, there are no studies assessing the agreement between rectal and AT measurement in small animal patients presenting to an emergency room (ER). The goals of the current study were to compare rectal and ATs in emergent canine patients. We expect that dogs presenting to the ER will have good agreement between aural and RT when normothermic but that aural thermometry will underestimate RT in hypo- and hyperthermic patients.
Materials and Methods
All canine patients presenting to the ER were eligible for enrollment. Recorded patient parameters included: heart rate, respiratory rate, breed, presence of aural debris, coat length (classified as short, medium or long), weight, body condition score (1–9, where 1 is thin and 9 is obese; determined by Royal Canin Body Condition Score Chart)d, pain score (0–4, where 0 is comfortable and 4 is the most painful; determined by Colorado State University Canine Acute Pain Scale).e All dogs were included in the study. Temperatures were obtained on presentation using two sets of labelled study thermometers including: one aural Braun ExacTempa; and one rectal Vet-Temp Rapid Digital Thermometerb. For each patient, the aural thermometer probe tip was covered by a new disposable plastic barrier cup while the rectal thermometer was covered by a disposable plastic sheath and lubricated for rectal insertion (at least 2 cm along the rectal mucosa). Pre-calibrated ambient humidity and temperature indicatorsc were present in the vicinity of temperature measurements and environmental humidity and temperature were recorded during each patient temperature measurement.
The order of temperature measurement was randomized for each patient and the order of measurement and temperature values were recorded. All temperatures were measured by emergency and critical care staff (veterinary assistants, technicians, and clinicians) within five minutes of arriving to the treatment area. For the purposes of this study, dogs with a mean RT ranging from 37.8°C to 39.5°C were classified as normothermic (group 1, n = 105), whereas dogs with lower and higher RT measurements were classified as hypothermic (group 2, n = 24) and hyperthermic (group 3, n = 23), respectively.12 The study protocol was reviewed and approved by the Institutional Animal Care and Use Committee and owner consent was waived as acquirement of temperature was considered standard of care in the enrolled patients.
Statistical Analyses
Univariate statistics are presented for heart rate, respiratory rate, body condition score, pain score, whether the dog breed was brachycephalic, the presence of aural debris, and coat length, all as factors which may influence temperature. The statistical significance of variation in these measures across temperature groups was assessed using analysis-of-variance (ANOVA) for continuous measures and Pearson’s chi-squared tests for categorical variables. The difference between aural and RT was evaluated using a paired sample t-test. Normality of all key measures was evaluated using the Shapiro–Wilk test. Bartlett’s test for equal variance was used to assess the equal variance assumption. No measures violated the equal variances assumption, and only the respiratory rate exhibited signs of non-normality. To correct for this, the natural log of the measure was taken, which improved normality, and all analyses involving the respiratory rate were re-run using this measure as a sensitivity analysis. Findings did not substantively differ when logged respiratory rate was used instead of the original measure.
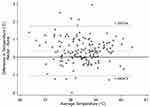
Pearson correlations were used to assess the strength of the relationship between rectal and AT overall and within each temperature group. To examine the agreement between rectal and AT, Bland-Altman plots were used and key values from these plots were reported. Lower and upper limits of the 95% levels of agreement are used to assess how well these two measures agree using a maximum clinically acceptable difference in temperature at 0.3 °C.
Linear regression with White’s heteroscedasticity-corrected standard errors was used to determine the influence ambient temperature and humidity on patient rectal and AT. These models were also run controlling for heart rate, respiratory rate, body condition score, pain score, whether the dog breed was brachycephalic, the presence of aural debris, and coat length. The level of significance was set to a P-value of <0.05. Analyses were estimated using Stata 17.f
Results
One hundred and fifty-two dogs were enrolled in the study. Dogs in this study had an average heart rate of 128 beats per minute (range 40–240 beats per minute) and an average respiratory rate of 70 breaths per minute (range 16–180 breaths per minute). Approximately 23% (35/152) of dogs were brachycephalic and 23% (35/152) demonstrated aural debris on exam. Fifty-four percent (82/152) of dogs had short haircoats, 31% (47/152) medium length coats, and 15% (22/152) long length coats. The average body condition score was 5/9 and the average pain score was 0/4. The following factors were not different across temperature groups: heart rate; breed; presence of aural debris; sex; body condition score; and pain score (Table 1). Respiratory rate, however, did vary by temperature group, with hyperthermic dogs having significantly higher respiratory rates than normothermic or hypothermic dogs (p < 0.05). Coat length also varied across temperature groups, with hypothermic dogs being much more likely to have a short coat than normothermic or hyperthermic dogs (p < 0.05).
 |
Table 1 Patient Demographics |
The average rectal and ATs were 38.7°C (range 36.6–40.7°C) and 38.3°C (range 35.7°C–40.4°C), respectively. The difference between aural and RT is statistically significant (p < 0.001), with AT lower on average than RT. When evaluating the full sample of all enrolled canines, there was a moderate, statistically significant relationship between rectal and ATs (r = 0.636; p < 0.001). This relationship is weaker but still statistically significant for normothermic dogs (r = 0.411; p < 0.001). For hyperthermic and hypothermic dogs, there is not a statistically significant relationship between these two measures and aural thermometry consistently underestimates RT (Table 2).
 |
Table 2 Pearson’s Correlation Between Rectal and Aural Temperature by Temperature Group |
A maximum clinically acceptable difference was determined as 0.3°C and the difference between rectal and AT was greater than this difference (Figure 1). Further, via Bland-Altman analysis, it was determined that while agreement is strongest for normothermic dogs, weaker for hyperthermic, and even weaker for hypothermic dogs, for the overall sample and each temperature group, lower and upper levels of agreement are notably greater than 0.3°C (Table 3).
 |
Table 3 Agreement Between Rectal and Aural Temperature Using Bland-Altman Analysis by Temperature Type |
Lastly, there was a statistically significant relationship between ambient temperature and both rectal and AT, but no relationship between humidity and either rectal or AT. Controlling for heart rate, respiratory rate, body condition score, pain score, skull conformation, the presence of aural debris, or coat length did not alter either of these findings (Table 4).
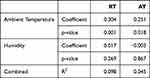 |
Table 4 Linear Regressions of Rectal and Aural Temperature on Ambient Temperature and Humidity |
Discussion
Various methods of temperature measurement have been evaluated in both human and veterinary medicine. Digital RT measurements are reliable and accurately core body temperature in human patients, however, less invasive methods are favored.13 In veterinary medicine, the use of rectal thermometers is also considered the gold standard for routine temperature measurement, likely because of their reported accuracy when compared to core temperature.1 As in humans, the use of a less invasive technique to obtain body temperature in canine patients, especially in an emergency setting, is alluring. The current study demonstrated that while rectal and AT measurements were similar in normothermic dogs, ATs were significantly different from RTs in hypothermic and hyperthermic patients presenting to the ER.
Tympanic (aural) thermometry has gained interest for use in human patients and provides safe and rapid temperature measurements.14,15 Aural thermometry should approximate core body temperature well, as the tympanic membrane and the hypothalamus share a blood supply via the carotid artery.16 Aural temperatures accurately reflect core temperatures in humans as shown by several studies that compared AT measurements to those made in the pulmonary artery and esophagus.17,18 Aural thermometers were also as reliable as rectal thermometers and more accurate than axillary measurements in pediatric patients.16 Other human studies, however, failed to demonstrate a clinically acceptable correlation between aurally and rectally measured temperatures. For instance, in adult human patients presenting to the ER, noninvasive measures of temperature (oral, tympanic membrane, and temporal artery) failed to achieve diagnostic accuracy when compared with rectal measurement. In this study, tympanic membrane temperature readings were the most accurate noninvasive measure, differing from rectal readings by about 0.4°C.19
In the adults in the aforementioned study (and also demonstrated in children presented to the ER), AT underestimated RT, similar to our study.19–21 The cause for these findings in people is unknown. Perhaps the presence of endolymph/perilymph or inflammation in human ears may lower the temperature obtained from this location. Aural debris did not affect temperature difference in our study. However, it is plausible that in canine patients, the amount of hair in the ear canal or the presence of inflammation in the ear canal may lead to lower AT readings.
Aural thermometry has previously been compared to rectal thermometry in both healthy and non-critically ill hospitalized dogs. As is seen in human medicine, study results are conflicting.3,4,8,9 In 300 dogs presenting for routine care, RT demonstrated a significant correlation with AT. However, additional statistical analyses identified a clinically unacceptable variation between the two methods. In these dogs, environmental humidity but not temperature influenced patient temperature measurements.8 Conversely, the current study identified that ambient temperature, but not humidity, influenced patient temperature.
Several additional studies failed to demonstrate agreement between rectal and AT measurement in healthy canine patients.4,9 Temperature measurement in eight purpose-bred dogs confirmed that RT most closely correlated with core body temperature as measured via pulmonary artery catheter. Aural temperatures in this study demonstrated marked variability and inaccuracy. Only 78% of aural measurements were within 1°C (1.8°F) of pulmonary arterial catheter readings, as compared to 99.7% of rectal measurements.9 In 88 healthy dogs, rectal and AT measurements exceeded their maximum clinically acceptable discrepancy of 0.5°C.4
Across the studies in healthy dogs, ATs underestimate those obtained rectally.4,9 In 250 hospitalized dogs, only a weak correlation between rectal and AT measurement was demonstrated. Aural temperature measurements also underestimated RT in these dogs.3 These results are similar to what was observed in the current study, wherein ATs were significantly lower than RTs in dogs presenting to the ER.
Previous human and canine studies have demonstrated that aural thermometry is less correlated with rectal thermometry when body temperature is abnormal. In exercising, hyperthermic people, aural thermometry did not reliably reflect core body temperature as measured by rectal thermometry.22 Similar results were found in human patients with exertional heat stroke, where aural thermometry was an inaccurate diagnostic tool and substitution for RT measurement was discouraged.23 In sick, febrile children, the AT underestimated the RT by 0.17–0.49°C (0.09–0.27°F), and achieved only a fair sensitivity, specificity, and positive predictive value to detect a fever.24 Two veterinary studies evaluated the tympanic membrane temperature in exercising, hyperthermic dogs and both concluded that tympanic membrane temperature was consistently lower than RT in these subjects.11,25 Interestingly, the current study demonstrated that hyperthermic dogs had a significantly higher respiratory rate than other temperature groups and that hypothermic dogs were more likely to have a short haircoat, which, to the author’s knowledge, has not previously been demonstrated. Consistent with previous studies’ findings, the current study also found a significant temperature difference between aural and rectal measurements in both hypothermic and hyperthermic ER canine patients.
One limitation of the present study was the use of RT as a surrogate for core body temperature. Further, our study did not assess for reliability of the aural thermometer as a measuring device, as defined as degree of stability among repeated measurements under identical conditions.26 Both inter- and intra-operator variability can affect repeatability of test results, and neither were assessed here. Repeated temperature measurements by the same investigator were specifically not pursued in this study as a means of making the results more clinically applicable. Future investigations specifically looking at reliability (as opposed to accuracy) of aural thermometry in veterinary patients are warranted. The order of temperature measurement was randomized in our study; however, excitement and stress elicited by either rectal or aural thermometry when this temperature was acquired first may have influenced the other measurement. An additional limitation of our study was the small sample size of dogs with temperatures outside of the normal reference range. Amongst all patients enrolled, only 47 dogs were assigned to a non-normothermic group (24 patients were hypothermic and 23 patients hyperthermic). Lastly, a veterinary-specific aural thermometer may be better suited for the variety of canine ear shapes and confirmations, and this type of thermometer was not investigated here.
Conclusion
To the authors’ knowledge, our study is the first comparison of rectal and AT measurements in canines presenting to an ER. Similar to previous human and veterinary studies, our main results call into question routine substitution of AT measurements for RT measurements. The present study did not provide evidence that AT is interchangeable with RT in hypo- and hyperthermic patients presenting to the ER. It did, however, find a weak statistically significant relationship between rectal and aural thermometry in normothermic dogs.
Caution must be used when interpreting AT in hypo- or hyperthermic dogs in the ER, as ATs were consistently lower than RTs in these patients. While there was some correlation in normothermic patients, approximately 30% of the dogs presenting to the ER during the study period exhibited abnormal body temperatures, and in these pets, aural thermometry was not representative of RT and may not be an acceptable method of temperature measurement in this patient cohort.
Ethics Statement
The study protocol was reviewed and approved by the Institutional Animal Care and Use Committee and owner consent was waived as acquirement of temperature was considered standard of care in the enrolled patients.
Acknowledgments
Walter Campbell for his excellence in statistical analysis.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kahng E, Brundage C. Comparing alternatives to canine rectal thermometry at the axillary, aural and ocular locations. Open Vet J. 2020;9(4):301–308. doi:10.4314/ovj.v9i4.4
2. Novak L, Burova J, Stankova L, Rado M. Changes in Tracheal, Oesophageal and RT over 60 Minutes Anaesthesia in Non-Heated Dogs, Spontaneously Breathing or Mechanically Ventilated. Vet Med. 2021;66(7):287–291. doi:10.17221/229/2020-VETMED
3. Gomart SB, Allerton FJ, Gommeren K. Accuracy of different temperature reading techniques and associated stress response in hospitalized dogs. J Vet Emerg Crit Care. 2014;24(3):279–285. doi:10.1111/vec.12155
4. Sousa MG, Carareto R, Pereira-Junior VA, Aquino MC. Comparison between auricular and standard rectal thermometers for the measurement of body temperature in dogs. Can Vet J. 2011;52(4):403–406.
5. Niven D, Gaudet J, Laupland K, et al. Accuracy of peripheral thermometers for estimating temperature: a systematic review and meta-analysis. Ann Intern Med. 2015;163(10):768–777. doi:10.7326/M15-1150
6. Kreissl H, Neiger R. Measurement of body temperature in 300 dogs with a novel noncontact infrared thermometer on the cornea in comparison to a standard rectal digital thermometer. J Vet Emerg Crit Care. 2015;25(3):372–378. doi:10.1111/vec.12302
7. González AM, Mann FA, Preziosi DE, Meadows RL, Wagner-Mann CC. Measurement of body temperature by use of auricular thermometers versus rectal thermometers in dogs with otitis externa. J Am Vet Med Assoc. 2002;221(3):378–380. doi:10.2460/javma.2002.221.378
8. Konietschke U, Kruse BD, Müller R, Stockhaus C, Hartmann K, Wehner A. Comparison of auricular and RT measurement in normothermic, hypothermic, and hyperthermic dogs. Tierarztl Prax Ausg K Kleintiere Heimtiere. 2014;42(1):13–19. doi:10.1055/s-0038-1623741
9. Greer RJ, Cohn LA, Dodam JR, Wagner-Mann CC, Mann FA. Comparison of three methods of temperature measurement in hypothermic, euthermic, and hyperthermic dogs. J Am Vet Med Assoc. 2007;230(12):1841–1848. doi:10.2460/javma.230.12.1841
10. Southward ES, Mann FA, Dodam J, Wagner-Mann C. A comparison of auricular, rectal and pulmonary artery thermometry in dogs with anesthesia induced hypothermia. J Vet Emerg Crit Care. 2006;16:172–175. doi:10.1111/j.1476-4431.2005.00158.x
11. Hall EJ, Carter AJ. Comparison of rectal and tympanic membrane temperature in healthy exercising dogs. Comparative Exercise Physiol. 2017;13(1):37–44. doi:10.3920/CEP160034
12. Silverstein DC. Hopper K. Small Animal Critical Care Medicine. Elsevier; 2015.
13. El-Radhi AS, Patel S. An evaluation of tympanic thermometry in a paediatric emergency department. Emerg Med J. 2006;23(1):40–41. doi:10.1136/emj.2004.022764
14. Purssell E, While A, Coomber B. Tympanic thermometry--normal temperature and reliability. Paediatr Nurs. 2009;21(6):40–43. doi:10.7748/paed2009.07.21.6.40.c7151
15. Sener S, Karcioglu O, Eken C, Yaylaci S, Ozsarac M. Agreement between axillary, tympanic, and mid-forehead body temperature measurements in adult emergency department patients. Eur J Em Med. 2012;19(4):252–256. doi:10.1097/mej.0b013e32834c5841
16. Kocoglu H, Goksu S, Isik M, Akturk Z, Bayazit YA. Infrared tympanic thermometer can accurately measure the body temperature in children in an emergency room setting. Int J Pediatr Otorhinolaryngol. 2002;65(1):39–43. doi:10.1016/S0165-5876(02)00129-5
17. Milewski A, Ferguson KL, Terndrup TE. Comparison of pulmonary artery, rectal, and tympanic membrane temperatures in adult intensive care unit patients. Clin Pediatr. 1991;30:13–16. doi:10.1177/0009922891030004S05
18. Staven K, Saxhyolm H, Erichsen NS. Accuracy of infrared ear thermometry in adult patients. Int Care Med. 1997;23:100–105. doi:10.1007/s001340050297
19. Bijur PE, Shah PD, Esses D. Temperature measurement in the adult emergency department: oral, tympanic membrane and temporal artery temperatures versus RT. Emerg Med J. 2016;33(12):843–847. doi:10.1136/emermed-2015-205122
20. Muma BK, Treloar DJ, Wurmlinger K, Peterson E, Vitae A. Comparison of rectal, axillary, and tympanic membrane temperatures in infants and young children. Ann Emerg Med. 1991;20(1):41–44. doi:10.1016/S0196-0644(05)81116-3
21. Yeoh WK, Lee JKW, Lim HY, Gan CW. Re-visiting the tympanic membrane vicinity as core body temperature measurement site. PLoS One. 2017;12(4):e0174120. doi:10.1371/journal.pone.0174120
22. Huggins R, Glaviano N, Negishi N, Casa DJ, Hertel J. Comparison of rectal and aural core body temperature thermometry in hyperthermic, exercising individuals: a meta-analysis. J Athl Train. 2012;47(3):329–338. doi:10.4085/1062-6050-47.3.09
23. Morrissey MC, Scarneo-Miller SE, Giersch GEW, Jardine JF, Casa DJ. Assessing the Validity of Aural Thermometry for Measuring Internal Temperature in Patients With Exertional Heat Stroke. J Athl Train. 2021;56(2):197–202. doi:10.4085/1062-6050-0449.19
24. Paramita T, Karyanti MR. A comparison of axillary and tympanic membrane to RTs in children. Paediatricia Indonesiana. 2017;57(1):47–51. doi:10.14238/pi57.1.2017.47-51
25. Zanghi BM. Eye and Ear Temperature Using Infrared Thermography Are Related to RT in Dogs at Rest or With Exercise. Front Vet Sci. 2016;19(3):111.
26. Wassertheil-Smoller S. Biostatistics and Epidemiology: A Primer for Health and Biomedical Professionals. 3rd. ed. New York: Springer-Verlag; 2004:161–167.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.