Back to Journals » Therapeutics and Clinical Risk Management » Volume 15
Comparative Results Between “Epi-Off” Conventional and Accelerated Corneal Collagen Crosslinking for Progressive Keratoconus in Pediatric Patients
Authors Nicula CA , Rednik AM , Bulboacă AE , Nicula D
Received 24 July 2019
Accepted for publication 4 December 2019
Published 30 December 2019 Volume 2019:15 Pages 1483—1490
DOI https://doi.org/10.2147/TCRM.S224533
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Garry Walsh
Cristina Ariadna Nicula,1,2 Anca Maria Rednik,3 Adriana Elena Bulboacă,4 Dorin Nicula2
1Department of Ophthalmology, “Iuliu Hațieganu” University of Medicine and Pharmacy, Cluj-Napoca, Romania; 2Oculens Clinic, Cluj-Napoca, Romania; 3County Eye Hospital, Cluj-Napoca, Romania; 4Department of Physiopathology, “Iuliu Hațieganu” University of Medicine and Pharmacy, Cluj-Napoca, Romania
Correspondence: Cristina Ariadna Nicula
Department of Ophthalmology, “Iuliu Hatieganu” University of Medicine and Pharmacy, Cluj-Napoca, Romania
Tel +40 722849575
Email [email protected]
Purpose: The aim of our study was to evaluate the efficacy and safety of epi-off conventional and accelerated corneal collagen cross-linking in the treatment of progressive keratoconus in pediatric patients up to 4 years after treatment.
Patients and methods: Conventional (standard) CXL epi-off technique was performed in 37 eyes (S-CXL group) and accelerated CXL in 27 eyes (A-CXL group). Refraction, keratometry, cylindrical equivalent, spherical equivalent, slit lamp examination, pachymetry, corneal tomography, anterior segment ocular coherence tomography and visual acuity were performed up to 4 years.
Results: In the S-CXL group: the flat K values decreased from 47.41±3.39 D to 45.36±3.62 D at 4 years (p=0.004); steep K decreased from 51.98±4.11 to 50.21±4.81 D at 4 years (p=0.0078); mean K decreased with 1.99 D at 4 years (p=0.009). In the A-CXL group: the flat K values decreased from 46.97±4.17 D to 44.97±4.24 D at 4 years (p=0.048); steep K decreased from 50.55±4.10 D to 48.75±4.17 D at 4 years (p=0.0287); mean K decreased from 48.79±3.86 D to 46.86±4.11 D at 4 years (p=0.0356). The preoperative mean UCVA in the S-CXL group was 0.8 ±0.23 logMar and improved during the follow-up reaching 0.65 ±0.24 logMar at 4 years (p=0.072). The baseline mean UCVA in A-CXL group was 0.77±0.25 logMar and increased during the follow-up to 0.63 ±0.25 logMar at 4 years (p=0.0039). A similar improvement of BCVA was observed during the follow-up.
Conclusion: Epi-off conventional and accelerated CXL are efficient procedures for progressive keratoconus in pediatric patients. Accelerated and conventional CXL were comparable at all time points and both represent viable options for the therapy of KC in these patients.
Keywords: conventional crosslinking, accelerated crosslinking, keratoconus, pediatric patients
Introduction
Keratoconus (KC) is a degenerative corneal disorder characterized by corneal thinning, conical protrusion, irregular astigmatism and visual impairment.1 It has been shown that KC presents a higher prevalence and has a higher aggressiveness in pediatric patients compared to adults, affecting the quality of life.2–8 Pediatric KC has several distinctive management issues in comparison to the adult KC regarding the diagnosis, poor compliance and different treatment patterns.3 The major concern is the accelerated progression of the disease in the pediatric age group. Chatzis and Hafezi2 found that 88% of pediatric KC patients had a progression from the initial visit, suggesting that it may be inappropriate to wait for signs of progression as commonly done in adults to offer treatment.3
The biomechanical rigidity of the cornea is inversely related to age and children with KC are eye rubbers, especially those with coexisting vernal keratoconjunctivitis.3 Diagnosis and therapy of KC at an early age may be more beneficial than waiting until patients have a more advanced disease requiring corneal transplantation.4 Also, taking into consideration that the prognosis of corneal transplantation in children is poorer than in adults, a treatment to stop or slow the progression could be beneficial.5
Corneal cross-linking (CXL) was introduced by Wollensak et al6 in the 1990s as a new therapeutic option to stop KC progression. CXL is a technique that uses the photochemical reaction between the ultraviolet A (UVA) light and riboflavin within the corneal stroma and leads to the development of chemical bonds between collagen fibrils strengthening the cornea and slows or stops the progression of keratoconus and other corneal ecstasies.7,8 Although favorable results have been reported with CXL in adults with KC,8–13 limited data is available in pediatric population on the effectiveness of CXL.5,11,14–19 Furthermore, whether conventional CXL therapy is the election therapy for pediatric patients with KC or whether accelerated “epi-off” CXL procedure is also an alternative is still under debate.
Therefore, the aim of our study was to compare the long-term efficacy and safety of conventional and accelerated “epi-off” CXL procedure in pediatric patients with progressive keratoconus up to 4 years following the procedure.
Materials and Methods
A retrospective, observational, single-center study was performed at the Oculens Clinic in Cluj-Napoca, Romania. 64 eyes of 64 patients with progressive KC aged 12 to 18 years of age treated between January 2013 and December 2014 were included. Based on the procedure used, patients were divided in 2 groups: conventional group (37 eyes of 37 patients) who underwent CXL by conventional (standard) “epi-off” technique (S-CXL group) and accelerated group (27 eyes of 27 patients) who underwent CXL by accelerated “epi-off” CXL procedure (A-CXL group).
The inclusion criteria were: age between 12-18 years, both genders, progressive KCN of different stages (according to the Krumreich classification), an average corneal thickness of at least 400 µm at the thinnest corneal point and cooperative to topical anesthesia. Progression of KCN was defined as an increase in steep K values at the apex of KCN of 1 diopter (D) in 1 year or a mean central change in K readings of >1.5 D in three consecutive topographies during the previous/over a 6 months, or an increase of 0.5 or more in the manifest refraction spherical equivalent over 6 months period.20 In cases with KCN stages III and IV the CXL procedure was performed without waiting for progression of the disease. Were excluded patients with previously intracorneal ring placement, history of herpetic keratitis, corneal pachymetry less than 400 microns, central corneal scar or Vogt striae.
Before the procedure a complete ocular assessment was performed, including uncorrected visual acuity (UCVA) and best corrected visual acuity (BCVA) with spectacles, refractometry (manifest and cycloplegic), keratometry (flat, steep and mean K; Topcon autorefractor-kerato-meter, KR 8900), slit-lamp exam (Slit Lamp BX 900, Haag-Streit AG), eye fundus examination, intra-ocular pressure by applanation tonometry, ultrasonic pachymetry (Sonomed 300PPachymeter), corneal tomography (Pentacam® HR Premium; Oculus Optikgerate GmbH, Wetzlar, Germany) and endothelial cell counting (Konan SP-9000, Hyogo, Japan). The keratometric data and astigmatism were measured on topography. Visual acuity was measured as Logarithm of Minimum Angle of Resolution. Patients were requested to discontinue the wear of soft contact lens 2 weeks and of rigid gas-permeable contact lens for 4 weeks before evaluation or surgery.
After approval of the Oculens clinic ethics committee under the principles of the Helsinki declaration and signing of specific informed consent from the legal guardian, the patients underwent the epi-off conventional or accelerated CXL procedure.
The cross-linking procedure was performed in the operating room in sterile conditions. The “epi-off“ CXL technique was used for conventional procedure. During the procedure, a single 3.0 mL of the riboflavin 0.1%-dextran 20% solution was opened. The power of the illuminator (Peschke Meditrade GmbH, Huenenberg, Switzerland CXL system) was verified. The eye was prepared with topical anesthesia (Alkaline solution), 3–4 drops, and 15–20 mins before cross-linking. A corneal de-epithelization of 9 mm diameter optical zone was performed, followed by the instillation of one drop of alkaline solution and instillation of riboflavin 0.1% every 3 mins for 30 mins before irradiation. Pachymetry was performed after epithelial removal to ascertain that corneal depth was more than 400 microns. The central part of the cornea was further exposed to UVA light (Peschke Meditrade GmbH, Huenenberg, Switzerland CXL system) and riboflavin was applied every 3 mins for a period 30 mins, under a power of 3 mW/cm2 for conventional CXL (Dresden protocol). For accelerated CXL instillation of riboflavin 20 mins every 2 mins, followed by exposure to UVA light for 10 mins, under a power of 9mw/cm2 and instillation of riboflavin every 2 mins was performed. Care was taken to protect the limbus from inadvertent UV exposure in both groups. In 2 cases of KC stage 4 with a corneal thickness between 370 to 376 μ, it was used hypotonic riboflavin in order to increase corneal thickness more than 400μ. The cornea surface was irrigated with balanced salt solution after irradiation. At the end of the procedure, topical antibiotics and steroids were instilled. A silicone hydrogel bandage soft contact lens (Pure Vision, Bausch, and Lomb) was applied following the treatment and was removed after 3–4 days.
After the procedure, all patients underwent therapy with topical antibiotics (ciprofloxacin eye drops) four times/day for 3 days steroids (fluorometholone acetate 0.1%) four times/day for one month and artificial tears two times/day for 2 to 3 months. Slit lamp examination was performed at day 1, at 4 days, 1 month, 6 months, 12 months, 24 months, 36 months and 72 months after the procedure. Uncorrected visual acuity (UCVA), best corrected visual acuity (BCVA) with spectacles and manifest refraction were measured at 6 months, 12 months, 24 months, 36 months and 72 months. Pentacam corneal analysis was performed at 6, 12, 24, 36 and 72 months after the procedure.
Statistical Analysis
Quantitative data were tested for normality with Kolmogorov–Smirnov test at a significance level of 5%. Quantitative data that proved to follow the normal distribution and thus were presented as mean ± standard deviation; qualitative data were reported as number and percentages. Repeated measurements ANOVA test was used to evaluate the effect of applied treatment (A-CXL and S-CXL, respectively) over repeated follow-up (baseline, 1 year, 2 years, 3 years and 4 years) on five measurements. The follow-up measurements for each group were compared to baseline values using paired t-test. The comparison between groups with different treatment was done for baseline and each follow-up with Student’s t-test for independent samples. A p-value <0.05 was considered statistically significant.
Results
At baseline, the mean age of patients included in the analysis was 16.43±1.281 (range: 12 and 18 years) in the S-CXL group and 16.77±1.527 (range: 12 and 18 years) in A-CXL group (p for difference between groups = 0.702). In the S-CXL group were included 24 males and in the A-CXL group 20 males. Regarding the stage of keratoconus (Amsler-Krumeich staging) in the S-CXL group 24.3% of the patients were in stage I, 54.1% stage II, 18.9% were in stage III and 2.7% were in stage IV. In the A-CXL group, 37.0% of patients were in stage I, 37.0% were in stage II, 22.2% stage III and 3.7% stage IV. 58.6% had a history of rubbing eyes, 10 eyes (6.4%) had an associated vernal keratoconjunctivitis (VKC), 20 eyes (12.8%) had atopy, 4 were rigid contact lens users (1.32%) and 10% had a positive family history for KCN. In the group of eye rubbers, in 38.6% of cases was performed standard CXL and in 20% accelerated CXL. In 4.26% atopic eyes was performed accelerated CXL and in 8.52% standard CXL.
There was no statistically significant difference between study groups in terms of preoperative flat keratometry (K1; p=0.801), steep keratometry (K2; p=0.200) and mean keratometry (Kavg; p=0.438). Compared to the preoperative status, K1, K2 and Kavg were statistically significantly lower at year 1 and maintained significantly lower at all-time points.
The repeated measurements ANOVA shows a significant contribution of applied treatment to K1 (p=0.0016), Kavg (p=0.0025) and mean cylinder (p=0.0263) and tendency to a significant contribution to K2 (p=0.0535), spherical equivalent (p=0.0887).
In the S-CXL group, K1 dropped from 47.41±3.39D to 46.76±3.59D at 1 year (p=0. 0098), to 46.14±3.55D at 2 years (p=0.010), to 45.65±3.64D at 3 years (p=0.030) and to 45.36±3.62D at 4 years (p=0.004). In the A-CXL group, K1 dropped from 46.97±4.17D to 46.33±4.48D at 1 year (p= 0.037), to 45.77±4.25 D at 2 years (p=0.045), to 45.24±4.23D at 3 years (p=0.03) and to 44.97±4.24 D at 4 years (p=0.048) (Figure 1). There were no statistically significant differences between groups in terms of K1 decrease at 1 year (p=0.897), 2 years (p=0.512), 3 years (p=0.487), and 4 years (p= 0.514).
 |
Figure 1 Evolution of K1 in both groups. |
K2 dropped in the S-CXL group from 51.98±4.11D to 51.49±4.60D at 1 year (p=0.0045), to 51.20±4.58D at 2 years (p=0.033), to 50.83±4.65D at 3 years (p=0.007) and to 50.21±4.81D at 4 years (p=0.0078). In the A-CXL group, K2 dropped from 50.55 ±4.10D to 49.93±4.64D at 1 year (p=0.0072), to 49.52±4.26 D at 2 years (p=0.0051), to 49.05±4.18 at 3 years (p=0.0101) and to 48.75±4.13D at 4 years (p=0.0287) (Figure 2). There were no statistically significant differences between groups in terms of K2 at 1 year (p=0.1411), 2 years (p=0.1984), 3 years (p=0.0986) and 4 years (p=0.1122).
 |
Figure 2 Evolution of K2 in both groups. |
For Kavg, the decrease was similar in both groups at all follow-ups points analyzed. In the S-CXL group Kavg dropped from 49.68±3.56D to 49.13±3.83D at 1 year (p=0.0071), to 48.67±3.84D at 2 years (p=0.0094), to 48.24±3.98D at 3 years (p=0.0051) and to 47.79±3.98 D at 4 years (p=0.0099). In A-CXL group Kavg dropped from 48.79±3.86D to 48.13 ±4.26 D at 1 year (p=0.0096), to 47.63±4.11 D at 2 years (p=0.012), to 47.15±4.09D at 3 years (p=0.0399) and to 46.86±4.11D at 4 years (p=0.0356) (Figure 3).
 |
Figure 3 Evolution of Kavg in both groups. |
In the S-CXL group, mean cylinder decreased from −4.98±2.80D to −4.73±2.78 at 1 year (p=0.032), to −4.49±2.55D at 2 years (p=0.0041), to −4.27±2.61D at 3 years (p= 0.022) and to −4.11±2.59D at 4 years (p=0.0091). In A-CXL group mean cylinder decreased from −4.37±2.45 D to −4.12±2.35 D at 1 year (p=0.044), to −3.89±2.58 D at 2 years (p=0.0088), to −3.70±2.48 D at 3 years (p=0.0079) and to –3.57±2.51 D at 4 years (p=0.0143) (Figure 4). There was no statistically significant difference between the cylinder decrease in both groups at 1 year (p=0.4176), at 2 years (p=0.4002), at 3 years (p=0.3966) and at 4 years (p=0.4029).
 |
Figure 4 Evolution of mean cylinder in both groups. |
Compared to baseline, in the S-CXL group, the spherical equivalent (SE) decreased from −6.90±4.31D to −6.34±4.31D at 1 year (p=0.047), to –6.28 ± 4.33D at 2 years (p=0.036), to −6.23±4.24D at 3 years (p=0.017) and to −6.18± 4.25D at 4 years (p=0.0087). In the A-CXL group, SE decreased from baseline −5.73±4.55D to −5.30±4.59D at 1 year (p=0.0313), to −5.23±4.19D at 2 years (p=0.0075), to –5.16±4.26 D at 3 years (p=0.0072) and to-5.15±4.26 D at 4 years (p=0.016) (Figure 5). No statistically significant difference between groups was observed at any time points at 1 year (p=0.3561); at 2 years (p=0.3561), at 3 years (p=0.3247) and at 4 years (p=0.346).
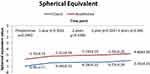 |
Figure 5 Evolution of spherical equivalent in both groups. |
The preoperative mean UCVA in the S-CXL group was 0.8±0.23 logMar and improved during the follow-up reaching 0.65±0.24 logMar at 4 years (p=0.072). The baseline mean UCVA in A-CXL group was 0.77±0.25 logMar and increased during the follow-up to 0.63±0.25 logMar at 4 years (p=0.0039). A similar improvement of BCVA was observed during the follow-up. The preoperative BCVA in the S-CXL group was 0.57 ±0.20 logMar and improved to 0.45 ±0.20 logMar at 4 years (p=0.0009). The baseline mean BCVA in A-CXL group was 0.54 ± 0.21logMar and increased to 0.44 ± 0.21logMar at 4 years (p=0.0098; Figure 6). The improvement of UCVA and BCVA was similar in both groups (p=0.4211 for UCVA and p=0.5486 for BCVA).
 |
Figure 6 Evolution of UCVA and BCVA in both groups. |
There were no complications noted after neither of the procedures. Moderate haze was noticed in the majority of patients and subsided completely after 3 months after surgery. Two eyes from two patients included in A-CXL group with a history of eye rubbing showed progression at the end of 4 years.
Discussions
In our study, we aimed to evaluate the evolution of pediatric patients with progressive KCN up to 4 years following “epi-off” conventional and accelerated CXL procedure. Results of our study showed a statistically significant reduction in all K readings from baseline at all follow-ups that maintained at 4 years in both groups. Furthermore, no statistically significant difference in K readings improvement was observed between groups.
At 4 years after CXL, there was a mean reduction in K1 value of 2.05D in the flattest meridian in the S-CXL group and of 2.00D in the A-CXL group. There was a reduction of 1.77 D in the S-CXL group and1.80 D in the A-CXL group in the steepest meridian. Our results are similar with those reported in other studies. In their prospective study, Arora et al15 applied standard CXL in 15 eyes of 15 pediatric keratoconus patients with moderate keratoconus in one eye and advanced disease in the fellow eye. Mean change in apical K (1.01±2.40 D) was also significant (p=0.004). In a prospective, international study Vinciguerra et al11 showed a significant reduction (p<0.05) in keratometry in the steepest and flattest meridian at 24 months following the procedure. Similarly, in a prospective non-randomized Phase II open trial Caporrossi et al13 showed a statistically significant improvement in K readings and asymmetry index values that maintained at 36 months post CXL. In a retrospective study on 59 eyes from 42 children and teenagers, Panos et al4 showed after 3 years of follow-up period a significant K max reduction after 24 months and lost significance at 36 months. In the study with the longest follow-up, Mazzotta et al19 evaluated the efficacy and safety of standard CXL procedure during a 10-year follow-up in 62 eyes of 47 keratoconic pediatric patients. They showed the stability of KC in 80 of the patients, while the progression rate was 24%. In our study progression was present only in two cases with KCN stage III and 13 and respectively 24 years of age, from A-CXL group. The low rate of progression can be explained by the corneal thickness above 400μ and the 4th year period of follow-up. Maybe in time we can assist to a higher rate of progression.
The efficacy of CXL procedure is also evaluated by visual acuity, which is an important parameter for the quality of life of patients. In our study, postoperative UCVA and BCVA were statistically significantly improved than preoperative values at analyzed follow-ups (p<0.001 for follow-ups). Our results were similar with those showed by Arora et al15 who evaluated the efficacy of standard CXL in 15 eyes of 15 pediatric patients. In their study mean UCVA improved significantly from 1.00±0.30 to 0.72±0.29 log MAR (p=0.035) and mean BCVA from 0.56±0.21 to 0.30±0.15log MAR (p=0.003) after 12 months. In another prospective non-randomized study in which were enrolled 44 eyes, Caporossi et al21 demonstrated that functional data at 36 months following standard CXL had an increase of +0.18 and +0.16 Snellen lines for UVCA and BCVA, respectively, in the group with corneal thickness >450μm and of +0.14 and +0.15 Snellen lines in the groups with corneal thickness <450 µm. Results of accelerated procedures were reported by Ozurghan et al22 in a retrospective study in which were enrolled 44 eyes and 38 pediatric patients. The authors that uncorrected distance visual acuity improved significantly from 0.52±0.36 to 0.39±0.26 logMar (p=0.002) and corrected distance visual acuity improved significantly from 0.38±0.24 to 0.30±0.20 logMar (p<0.001) during the 24 months follow-up.
In terms of comparative efficacy, in our study, both procedures led to similar imprint keratometric and visual acuity parameters. Our results are similar to those reported by Eissa and Yassin23 in a prospective randomized contralateral eye study comparing accelerated vs. conventional CXL – the only comparative study that we identified in which were enrolled only pediatric patients with KC. In 68 eyes of 34 patients, aged 9–16 years, followed for 1 year, the authors showed that both procedures are effective and safe in the therapy of KC in pediatric patients. However, the authors showed a higher improvement in corneal steepness and in visual acuity with accelerated procedure.23 In our study steep keratometry showed a similar statistically significant improvement at follow-ups with both procedures with no difference between groups. Also, UCVA improved from 0.77 logMAR to 0.63 logMAR in accelerated group and from 0.8 logMAR to 0.65 logMAR in conventional group. BCVA showed similar evolution in both groups with no statistically significant differences between groups.
This paper has several limitations that should be acknowledged. Data were collected retrospectively so the patients were not randomly assigned to the treatment. The efficacy of the applied treatment method was evaluated just up to 4 years after the intervention but our team would quantify the evaluation of the patient to up to 10 years follow-up to evaluate the long-term efficacy. A more extensive follow-up could also allow the identification of those factors or covariates that could potentially affect the risk of KC progression or long-term efficacy. However, the strength of our paper resides in the relatively large sample size compared to previous reports and a 4-years follow-up of these pediatric patients, adding to previous knowledge on this subject.
Conclusion
In conclusion, our study showed that CXL is safe and efficient in pediatric patients with KC. Accelerated and conventional CXL were comparable at all follow-ups points and both represent reliable options for the therapy of KC in these patients.
Disclosure
The authors report no funding and no conflicts of interest in this work.
References
1. Rabinovits YS. Keratoconus. Surv Ophthalmol. 1998;42(4):297–319. doi:10.1016/S0039-6257(97)00119-7
2. Chatzis N, Hafezi F. Progression of keratoconus and efficacy of pediatric [corrected] corneal collagen cross-linking in children and adolescents. J Refract Surg. 2012;28(11):753–758. doi:10.3928/1081597X-20121011-01
3. Kankariya VP, Kymionis GD, Diakonis VF, Yoo SH. Management of pediatric keratoconus - evolving role of corneal collagen cross-linking: an update. Indian J Ophthalmol. 2013;61(8):435–440. doi:10.4103/0301-4738.116070
4. Panos GD, Kozeis N, Balidis M, Moschos M, Hafezi F. Collagen crosslinking for paediatrickeratoconus. Open Ophthalmol J. 2017;11:211–216. doi:10.2174/1874364101711010211
5. Vanathi M, Panda A, Vengayil S, Chaudhuri Z, Dada T. Pediatric keratoplasty. SurvOphthalmol. 2009;54(2):245–271.
6. Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet: an induced collagen crosslinking for the treatment of keratoconus. AmJOphthalmol. 2003;135(5):620–627.
7. Suri K, Hammersmith KM, Nagra PK. Corneal collagen cross-linking: ectasia and beyond. CurrOpinOphthalmol. 2012;23(4):280–287.
8. O’Brart DP. Corneal collagen cross-linking: a review. J Optom. 2014;7(3):113–124. doi:10.1016/j.optom.2013.12.001
9. Nicula C, Pop R, Rednik A, Nicula D. 10-Year results of standard cross-linking in patients with progressive keratoconus in Romania. J Ophthalmol. 2019;2019:8285649. doi:10.1155/2019/2431481
10. Wittig-Silva C, Whiting M, Lamoureux E, Lindsay RG, Sullivan LJ, Snibson GR. A randomized controlled trial of corneal collagen cross-linking in progressive keratoconus: preliminary results. J Refract Surg. 2008;24:S720–S725. doi:10.3928/1081597X-20080901-15
11. Vinciguerra P, Albé E, Frueh BE, Trazza S, Epstein D. Two-year corneal cross-linking results in patients younger than 18 years with documented progressive keratoconus. Am J Ophthalmol. 2012;154:520–526. doi:10.1016/j.ajo.2012.03.020
12. Grewal DS, Brar GS, Jain R, Sood V, Singla M, Grewal SP. Corneal collagen crosslinking using riboflavin and ultraviolet-A light for keratoconus: one-year analysis using Scheimpflug imaging. J Cataract Refract Surg. 2009;35(3):425–432. doi:10.1016/j.jcrs.2008.11.046
13. Caporossi A, Mazzotta C, Baiocchi S, Caporossi T, Denaro R, Balestrazzi A. Riboflavin-UVA-induced corneal collagen cross-linking in pediatric patients. Cornea. 2012;31:227–231. doi:10.1097/ICO.0b013e31822159f6
14. Soeters N, van der Valk R, Tahzib NG. Corneal cross-linking for treatment of progressive keratoconus in various age groups. J Refract Surg. 2014;30(7):454–460. doi:10.3928/1081597X-20140527-03
15. Arora R, Gupta D, Goyal JL, Jain P. Results of corneal collagen cross-linking in pediatric patients. J Refract Surg. 2012;28:759–762. doi:10.3928/1081597X-20121011-02
16. Bakshi E, Barkana Y, Goldich Y, Avni I, Zadok D. Corneal cross-linking for progressive keratoconus in children: our experience. Int J Keratoco Ectatic Corneal Dis. 2012;1:53–56.
17. Zotta PG, Moschou KA, Diakonis VF, et al. Corneal collagen cross-linking for progressive keratoconus in pediatric patients: a feasibility study. J Refract Surg. 2012;28:793–799. doi:10.3928/1081597X-20121011-08
18. Buzzonetti L, Petrocelli G. Transepithelial corneal cross-linking in pediatric patients: early results. J Refract Surg. 2012;28:763–767. doi:10.3928/1081597X-20121011-03
19. Mazzotta C, Traversi C, Baiocchi S, et al. Corneal collagen cross-linking with riboflavin and ultraviolet light for pediatric keratoconus: ten-year results. Cornea. 2018;37(5):560–566. doi:10.1097/ICO.0000000000001505
20. Shetty R, Nagaraja H, Jayadev C, Pahuja NK, Kurian Kummelil M, Nuijts RM. Accelerated corneal collagen cross-linking in pediatric patients: two-year follow-up results. Biomed Res Int. 2014;2014:894095. doi:10.1155/2014/894095
21. Caporossi A, Mazzotta C, Baiocchi S, Caporossi T. Long-term results of riboflavin ultraviolet A corneal collagen cross-linking for keratoconus in Italy: the Siena eye cross study. Am J Ophthalmol. 2010;149:585–593. doi:10.1016/j.ajo.2009.10.021
22. Ozgurhan EB, Kara N, Cankaya KI, Kurt T, Demirok A. Accelerated corneal cross-linking in pediatric patients with keratoconus: 24-month outcomes. J Refract Surg. 2014;30(12):843–849. doi:10.3928/1081597X-20141120-01
23. Eissa SA, Yassin A. Prospective, randomized contralateral eye study of accelerated and conventional corneal cross-linking in pediatric keratoconus. Int Ophthalmol. 2019;39(5):971–979. doi:10.1007/s10792-018-0898-y
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
