Back to Journals » Patient Preference and Adherence » Volume 8
Combination of brinzolamide and brimonidine for glaucoma and ocular hypertension: critical appraisal and patient focus
Authors Nguyen QH
Received 15 March 2014
Accepted for publication 25 April 2014
Published 12 June 2014 Volume 2014:8 Pages 853—864
DOI https://doi.org/10.2147/PPA.S53162
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Quang H Nguyen
Division of Ophthalmology, Scripps Clinic, La Jolla, CA, USA
Abstract: Glaucoma is one of the leading causes of blindness and is characterized by optic nerve damage that results in visual field loss. Elevated intraocular pressure (IOP) has been associated with glaucoma progression; thus, IOP-lowering medications are the standard of care for glaucoma. Guidelines suggest monotherapy with IOP-lowering agents such as β-blockers (eg, timolol), prostaglandin analogs, carbonic anhydrase inhibitors (eg, brinzolamide), and α2-receptor agonists (eg, brimonidine). However, monotherapy may provide insufficient IOP reduction in some patients, thereby necessitating the use of multiple IOP-lowering medications. Multidrug regimens may be complex, may increase the risk of preservative-related ocular symptoms, and may potentially reduce overall drug exposure as a consequence of drug washout during closely timed sequential administrations; these difficulties may reduce overall drug efficacy and decrease patient persistence and adherence with multidrug treatment regimens. Fixed-combination medications that provide two IOP-lowering therapies within a single solution are available and may overcome some of these challenges. However, all currently available fixed combinations combine timolol with another IOP-lowering agent, indicating that additional fixed-combination alternatives would be beneficial. To meet this demand, a novel fixed combination of brinzolamide 1% and brimonidine 0.2% (BBFC) has recently been developed. In two randomized, double-masked, multinational clinical trials, BBFC had greater IOP-lowering efficacy than brinzolamide or brimonidine monotherapy after 3 months of treatment in patients with open-angle glaucoma or ocular hypertension. In both studies, the overall safety profile of BBFC was consistent with that of brinzolamide and brimonidine. Comparative studies with BBFC versus other IOP-lowering monotherapy and fixed-combination medications are not available, but the IOP reductions observed with BBFC are similar to or greater than those reported in the literature for other glaucoma treatments; thus, BBFC provides an additional fixed-combination therapeutic option for patients who require further efficacious IOP reduction and improved convenience and tolerability versus concomitant administration of two separate medications.
Keywords: adherence, fixed combination, persistence, Simbrinza®, tolerability
Introduction
In 2010, glaucoma accounted for over 8 million incidences of blindness worldwide and was one of the leading causes of blindness.1 By 2020, an estimated 79 million individuals worldwide will have been diagnosed with glaucoma.1 Glaucoma is characterized by elevated intraocular pressure (IOP), progressive optic neuropathy, and corresponding visual field loss.2,3 Lowering IOP to an individualized target level (typically a ≥25% reduction from initial IOP) and maintaining that level reduces the risk of vision loss and improves outcomes,4–6 even among patients with normal-tension glaucoma.4 Reduction of elevated IOP is currently the only therapeutic approach effective for the prevention of glaucoma progression.7
A wide array of IOP-lowering agents with different mechanisms of action are available, including β-blockers (eg, timolol), prostaglandin analogs (eg, latanoprost), carbonic anhydrase inhibitors (CAIs; eg, brinzolamide), and α2-adrenergic agonists (eg, brimonidine).5,8 These medications reduce IOP by decreasing aqueous production,5 increasing aqueous outflow,5,9 or both. β-blockers and CAIs reduce aqueous production by limiting blood flow to the iris root–ciliary body10 or through inhibition of sulfonamide-susceptible carbonic anhydrase isozymes, respectively.11 In contrast, prostaglandin analogs reduce IOP by increasing uveoscleral and trabecular meshwork outflow of aqueous humor,7,12 and α2-adrenergic agonists reduce aqueous production and augment aqueous outflow through the uveoscleral pathway.13
Standard first-line treatment for glaucoma consists of treatment with a single IOP-lowering medication;5,14 however, one prospective study showed that approximately 40% of patients require multiple IOP-lowering medications to reach and maintain their target IOP.15 Unfortunately, persistence (ie, continued use of medication over time) with IOP-lowering medications is low.16–19 A systematic review of 14 studies that evaluated persistence using survival analysis demonstrated that only 31% of patients remained on their initial therapy at the end of 12 months.16 Persistence may be affected by the medication and regimen prescribed. A retrospective United States health claims database study showed that persistence with prostaglandins, α2-receptor agonists, and CAIs for 3 years was greater than that with β-blockers.18 However, drug-related differences in persistence likely disappear within a specific drug class; for example, a retrospective, population-based review of a United States claims database showed that a similar percentage of patients were persistent with their prescribed prostaglandin analog medication during a 1-year period regardless of the specific agent prescribed (ie, latanoprost [69.4%], travoprost [70.6%], or bimatoprost [68.1%]).19 In addition to the specific medication given, the dosing regimen prescribed for an individual may affect persistence; patients with complex therapeutic regimens requiring separate administration of several therapeutic agents tend to have lower persistence.20,21
Medication adherence (ie, following the agreed-upon treatment regimen)18,22–37 is also less than optimal among patients with glaucoma, even though reduced adherence with IOP-lowering medication has been linked with progressive visual field loss.22,38 Rates of adherence to IOP-lowering treatment among patients with glaucoma across multiple studies are shown in Table 1. Lack of patient adherence to their therapeutic regimen may ultimately decrease drug effectiveness. In a retrospective analysis of patient adherence in an ophthalmology clinic, 26.8% of patients did not achieve their target IOP as a result of nonadherence.39 The reasons for patient nonadherence are diverse. Treatment complexity (eg, treatment with >1 IOP-lowering drug) and patients’ attitude toward, and insufficient knowledge of, glaucoma have been associated with reduced adherence.23,24,26,28,32,36,40–42 Other factors that may disrupt medication use by patients include cost and insurance coverage, forgetting to take the medication, difficulty with instillation of drops, higher number of daily doses, initial medication drug class, and poor tolerability.18,24,27,29,36,41,42
Patients who require multiple concomitant medications to achieve and maintain IOP control may be more likely to deviate from their prescribed medication regimen. In a retrospective, open-label database review, addition of a second medication to a monotherapy regimen increased the time between medication refills by >2 weeks in some patients.43 Trouble remembering to take medication and having difficulty opening medication bottles were reported by more patients receiving multiple concomitant glaucoma treatments than those receiving one medication; these complaints were associated with reduced adherence.27 The efficacy, cost, and tolerability of multidrug regimens may also affect persistence and adherence. Persistence can be related to treatment efficacy because lack of efficacy often results in a switch in treatment. With administration of multiple medications, administration of a second drug within 5 minutes of an initial medication may cause substantial reductions in the concentration of the first drug because of washout of the first drug,44 thereby potentially reducing overall IOP-lowering efficacy.44 In a survey of patients using topical glaucoma medications, 23.5% of patients administered a second drop of medication within 5 minutes of the first drop, and 14% waited less than 2 minutes before instilling the second drop.45 Additionally, exposure to more than one preserved topical medication (and therefore a greater cumulative exposure to irritating preservatives) may increase ocular symptoms46,47 and may predispose patients to discontinue their therapy. Cost may also be a significant burden42 because each separate drug solution may be associated with an additional copay.48
To address the barriers to optimal adherence and persistence with IOP-lowering therapy, several fixed-combination medications, which allow instillation of two medications in a single solution, have been developed. Fixed-combination medications reduce the number of medication bottles required, may reduce costs, and provide a simplified dosing regimen, all of which may increase persistence20,21,49 and adherence.20,21 In a 2008–2009 United States study, Kaplan–Meier survival analysis of a prescription database demonstrated increased persistence with fixed-combination IOP-lowering medications compared with concomitant administration of two separate drugs (Figure 1).21 The same study reported greater adherence with fixed combinations (40.6%–42.7%) than separate administration of two medications (23.3%–34.9%) after 1 year of treatment.21
  | Figure 1 Kaplan–Meier analysis of treatment persistence among fixed and unfixed glaucoma medications. |
Prospective trials have shown that switching from concomitant administration of multiple separate medications to a fixed-combination therapy increases patient adherence.50,51 For example, when patients were switched from separate administration of latanoprost 0.005% and timolol 0.5% to a fixed combination of latanoprost 0.005%/timolol 0.5%, the percentage of patients who reported never missing a dose was significantly greater after the switch (71.0%) compared with before the switch (59.3%; P=0.0115).51 Because adherence relies on patients’ willingness to take their medication, it is important that patients prefer the medication they are prescribed over other equally efficacious alternatives. A reduction in ocular symptoms associated with the prescribed medication may have beneficial effects on patient preference and may increase adherence. Fixed combinations may have a better tolerability profile than concomitant administration of two agents with regard to ocular symptoms because cumulative exposure to irritating preservatives is reduced;52 therefore, the reduced ocular symptoms associated with fixed-combination medications may improve overall adherence.
A fixed-dose combination of a CAI, brinzolamide 1%, and an α2-adrenergic agonist, brimonidine 0.2% (BBFC; Simbrinza®; Alcon Laboratories, Inc., Fort Worth, TX, USA), has recently been developed to provide improved IOP-lowering efficacy, with a safety profile similar to its individual components. BBFC is approved for 3-times-daily dosing in the United States and is indicated for the reduction of elevated IOP in patients with primary open-angle glaucoma or ocular hypertension. This review highlights the efficacy and safety of this new fixed-combination medication and discusses its practical implications for patients.
Efficacy of BBFC
In clinical trials, BBFC administered three times daily (in accordance with the approved dosing regimens of brinzolamide and brimonidine in the United States) had a greater IOP-lowering effect than brinzolamide 1% or brimonidine 0.2% after 3 months of treatment in patients with open-angle glaucoma or ocular hypertension.53–56 In these trials, baseline IOP values were similar among all treatment groups. Between-group differences in IOP from baseline were based on prespecified analyses of least squares (LS) means instead of arithmetic means. LS means differ from arithmetic mean values in that they account for covariates (eg, correlated IOP measurements within patients) and are less sensitive to missing data; therefore, LS means may be better estimates of the overall average IOP within this patient population. In a randomized, Phase III, double-masked clinical trial of BBFC versus brinzolamide or brimonidine in patients with open-angle glaucoma or ocular hypertension, the LS mean IOP after 3 months of treatment was significantly lower with BBFC (17.0–20.5 mmHg) than with brinzolamide (20.0–21.6 mmHg; P≤0.002 for all time points) or brimonidine (18.8–23.3 mmHg; P<0.001 for all time points) throughout the day (ie, 8 am, 10 am, 3 pm, and 5 pm; Table 2).53 Mean IOP reductions from baseline and percentage change in IOP from baseline were also greater with BBFC (5.7–8.8 mmHg; percentage reduction, 24.1%–34.9%) than with brinzolamide (4.1–6.2 mmHg; percentage reduction, 16.9%–22.6%) or brimonidine (3.5–6.5 mmHg; percentage reduction, 14.3%–25.8%).53 Similar results were observed in a separate randomized, double-masked Phase III trial with a 3-month safety extension (LS mean IOP at 3 months: BBFC, 17.2–21.1 mmHg; brinzolamide, 20.4–22.0 mmHg, P≤0.005 versus [vs] BBFC; brimonidine, 18.9–23.2 mmHg, P<0.0001 vs BBFC; Figure 2) and a pooled analysis of both Phase III trials (LS mean IOP at 3 months: BBFC, 17.1–20.8 mmHg; brinzolamide, 20.2–21.8 mmHg, P<0.0001 vs BBFC; brimonidine, 18.8–23.2 mmHg, P<0.0001 vs BBFC).54,55 Greater reductions in mean IOP with BBFC compared with brinzolamide or brimonidine were observed at week 2 (the first post baseline evaluation day) in both Phase III trials53,54 and continued for up to 6 months (mean reductions from baseline to month 6: 4.9–8.0 mmHg with BBFC, 4.1–5.8 mmHg with brinzolamide, and 3.0–6.3 mmHg with brimonidine).56 Thus, the therapeutic benefit of BBFC occurs shortly after initial administration (ie, within the first 2 weeks) and continues for up to 6 months. Taken together, these data suggest that BBFC effectively lowers and maintains clinically relevant IOP reductions (ie, reductions ≥1 mmHg).57 Although the IOP-lowering efficacy of some medications (eg, β-blockers, brimonidine) has been shown to fluctuate, often with decreased efficacy at night,58 BBFC provides effective IOP reduction throughout the day. Some other fixed-combination glaucoma medications have also demonstrated 24-hour control of IOP. For example, fixed combinations of dorzolamide and timolol, and brimonidine and timolol both significantly decrease IOP from baseline (mean IOP reduction: 2.9 mmHg and 2.2 mmHg, respectively).59 However, IOP reductions were greater during the night (6 pm and 2 am) with dorzolamide and timolol compared with brimonidine and timolol, which was to be expected given the decreased evening efficacy of both components.58,59 Given that significant IOP reductions with BBFC are still seen at 8 am (10 hours after dosing), it is likely that the nocturnal IOP-lowering efficacy of BBFC is being conferred by the brinzolamide, not the brimonidine, component.60,61 However, 24-hour IOP control studies need to be conducted to confirm this.
  | Table 2 Intraocular pressure across visits and time pointsa |
  | Figure 2 LS mean IOP during a 3-month clinical trial with a 3-month safety extension. |
The IOP reductions observed with BBFC in these clinical trials are similar to or greater than those observed with other monotherapy or fixed-combination treatments in other studies. Among IOP-lowering monotherapy treatments, prostaglandin analogs generally provide the greatest IOP-lowering efficacy (percentage IOP change from baseline at peak as determined in a meta-analysis of randomized clinical trials, 31%–33%), followed by β-blockers (23%–27%), an α2-adrenergic agonist (25%), and CAIs (17%–22%).62 Similar trends in percentage IOP reduction from baseline have been observed among fixed-combination therapies combining timolol with prostaglandin analogs (peak IOP reduction as shown in a meta-analysis, 35%–36%), an α2-adrenergic agonist (32%), or CAIs (31%–34%).63 With BBFC, peak percentage IOP reduction was approximately 32%–34%,53,54 which is similar to that previously published for prostaglandin analogs and greater than reports with α2-adrenergic agonist and CAI monotherapy.62 In addition, mean IOP reduction from baseline with BBFC at 3 months (5.4–8.8 mmHg) was similar to reductions observed with fixed-dose combinations containing timolol after 3 months of treatment (prostaglandin analogs plus timolol, 2.6–10.2 mmHg; CAIs plus timolol, 3.7–9.0 mmHg; α2-agonists plus timolol, ~5.5–7.5 mmHg; Table 3).53,54,64–75
Safety and tolerability of BBFC
Similar to other fixed-combination therapies,48,64,66,69,72,74–76 the overall safety profile of BBFC is consistent with that of its individual components (brinzolamide 1% and brimonidine 0.2%).53–56 In clinical trials, ocular events were the most common treatment-related adverse events (TRAEs) associated with BBFC and occurred with similar frequency in the BBFC and brinzolamide or brimonidine groups (Tables 4 and 5).53,54,56 In Phase III clinical trials, blurred vision (4.5%–6.1%) and eye irritation (2.8%–5.4%) were two of the most commonly reported ocular TRAEs with BBFC after 3 months of treatment.53,54 Blurred vision was the most common ocular TRAE observed with brinzolamide (6.2%–6.8%) at 3 months.53,54 The occurrence of blurred vision with BBFC and brinzolamide in some patients is unsurprising given that these medications are administered as ophthalmic suspensions. In contrast, the most frequently reported ocular TRAEs with brimonidine at 3 months were conjunctivitis (3.0%), dry eye (0.4%–2.7%), eye irritation (1.8%–2.6%), and ocular hyperemia (2.6%–4.1%).53,54 In both trials, the incidence of ocular hyperemia was more prevalent with brimonidine (2.6%–4.1%) than BBFC (0.9%–3.3%) or brinzolamide (0.4%–0.9%) at 3 months.53,54 After 6 months of treatment, eye irritation and eye allergy were the most common ocular TRAEs associated with BBFC (6.3% for both), whereas blurred vision (6.8%) and conjunctivitis (6.0%) were most frequent in the brinzolamide and brimonidine groups, respectively (Table 5).56 Eye allergy rates were 0.4% with brinzolamide and 2.1% with brimonidine at 6 months.56 The incidence of ocular hyperemia continued to be higher in the brimonidine group (3.8%) than the BBFC (2.7%) or brinzolamide (0.4%) groups after 6 months.56 In the two Phase III clinical trials, discontinuations because of nonserious TRAEs were more common with BBFC (up to 11.3%) than with brinzolamide (up to 2.1%) or brimonidine (up to 9.4%).53,54 The slightly greater occurrence of some TRAEs and TRAE-related discontinuations with BBFC in these studies may be attributable to exposure to multiple therapeutic agents (ie, brinzolamide and brimonidine) versus monotherapy.
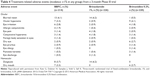  | Table 4 Treatment-related adverse events (incidence ≥1% in any group) from a 3-month Phase III trial |
  | Table 5 Treatment-related adverse events (incidence ≥1% in either group) from a 3-month clinical trial with a 3-month safety extension |
The lack of head-to-head comparative studies of BBFC and other IOP-lowering monotherapies and fixed-combination medications prevents the assessment of BBFC tolerability in terms of other IOP-lowering therapies, and differences in study design preclude direct comparisons between IOP-lowering medications evaluated in different clinical trials. However, the incidence of eye burning/stinging/irritation (which are often associated with β-blockers) appeared to be similar with BBFC compared with previous reports for timolol at 3 months (up to 5.4% with BBFC vs up to 18.1% [burning and stinging] with timolol) and slightly greater with BBFC than timolol at 6 months (6.3% with BBFC vs 4.5% [burning and stinging] with timolol).53,54,56,64,66,75 The incidence of other AEs (eg, blurred vision, which is commonly associated with CAIs) was slightly greater at month 3 with BBFC (up to 6.1%) than that previously reported with dorzolamide (4.0%).53,54,64 In general, the safety profile of BBFC appears to be similar to other currently marketed fixed-combination medications. Emergence or worsening of hyperemia was reported in up to 3.3% of patients receiving BBFC in two clinical trials,53,54 an incidence similar to that reported with prostaglandin analog/timolol fixed combinations across multiple studies (up to 2.8%).68,71,72 Additionally, the incidence of blurred vision with BBFC (up to 6.1%)53,54 was only slightly greater than that previously observed with CAI fixed combinations (brinzolamide/timolol, 3.4%; dorzolamide/timolol, 4%).64,75
As with all fixed-combination medications, BBFC increases IOP-lowering efficacy by providing two medications with different mechanisms of action in a single drop, with a potential decrease in cumulative exposure to preservatives. Preservatives, particularly benzalkonium chloride (BAK), have been associated with a variety of ocular symptoms, including dry eye,47,77,78 foreign body sensation in the eye,77 stinging/burning,77,78 tearing,77 reduced tear production,78 and hyperemia;77 thus, limiting exposure to preservatives by using fixed-combination medications instead of multiple individual medications may improve overall tolerability. For example, a recent systematic review and meta-analysis of randomized trials comparing fixed combinations of prostaglandins and timolol with concomitant administration of both medications showed that the relative risk of hyperemia was lower with the fixed combination than with the unfixed combinations (relative risk, 0.70; 95% confidence interval, 0.43–1.14).79 In a pooled analysis of two 3-month clinical trials, ocular symptoms that have been associated with preservatives (eg, dry eye and ocular hyperemia) occurred at a similar rate with BBFC (1.4% and 2.1% for dry eye and ocular hyperemia, respectively) compared with individual administration of brinzolamide (0.9% and 0.7%) or brimonidine (1.5% and 3.3%).55 Although it is possible that punctate keratitis, which was reported in only one of the Phase III trials (0.5%, 0.4%, and 1.4% with BBFC, brinzolamide, and brimonidine, respectively),53 may have contributed to the incidence of these ocular symptoms, this association remains unclear. These data suggest that despite exposure to additional medications (ie, two therapeutic agents instead of one), BBFC does not elicit any greater risk of ocular symptoms than its individual components. This observation may be explained by the reduced exposure to preservatives with BBFC versus administration of two separate preservative-containing medications.
Some IOP-lowering agents (eg, topical β-blockers and α2-receptor agonists) have been associated with significant alterations in blood pressure.80,81 For example, in a head-to-head trial in 27 patients with newly diagnosed primary open-angle glaucoma, brimonidine and timolol, but not dorzolamide or latanoprost, significantly reduced systolic and diastolic blood pressure from baseline;82 however, the clinical significance of these alterations is unknown. Interestingly, diastolic ocular perfusion pressure was low with timolol and brimonidine (53.0 mmHg and 46.2 mmHg, respectively), whereas values with dorzolamide (55.9 mmHg) and latanoprost (56.4 mmHg)82 exceeded the threshold associated with progression of primary open-angle glaucoma (ie, <55 mmHg).83 With BBFC, a slight decrease in mean systolic and diastolic blood pressure was observed in clinical studies; similar reductions were reported with brinzolamide and brimonidine and none were considered to be of clinical concern.53–56 Furthermore, individual blood pressure and pulse rate remained relatively stable (<1.5 bpm decrease in the BBFC, brinzolamide, and brimonidine groups).53–56 Some clinical studies of other available fixed-combination therapies, all of which contain timolol, have also reported no clinically significant changes in blood pressure from baseline.65,69 However, small but statistically significant mean alterations in heart rate and blood pressure from baseline have been reported with certain fixed-combination medications (eg, brimonidine/timolol66,73 and latanoprost/timolol).67
Additional considerations for BBFC
BBFC provides IOP-lowering efficacy greater than instillation of either of its components (brinzolamide or brimonidine), with potentially improved adherence and tolerability compared with concomitant administration of the separate medications. The increased convenience of dosing with one bottle instead of two may improve adherence and persistence and allow patients to achieve greater IOP control than dosing with separate components. IOP lowering may also be augmented with BBFC because it eliminates the potential of drug washout from sequential instillations of concomitant medications. In addition, reduced overall exposure to preservatives may increase patient comfort (and, as a result, potentially increase adherence to medication) and reduce the need for discontinuation or switching of therapies.
All currently available fixed-combination IOP-lowering medications provide similar IOP-lowering efficacy.53,54,63 However, all of these medications, except BBFC, contain the β-blocker timolol. Because glaucoma incidence increases with age,84 patients with glaucoma or ocular hypertension tend to have comorbid conditions or therapeutic regimens (eg, systemic β-blockers)85 that make them vulnerable to adverse drug reactions (eg, depression of systemic cardiovascular function observed with β-blockers).86–90 By providing effective IOP reduction with brinzolamide and brimonidine instead of timolol, BBFC expands the available fixed-combination options for patients who require efficacious IOP lowering and for those in whom use of β-blockers is contraindicated.
Conclusion
Glaucoma affects millions of individuals worldwide and is a leading cause of blindness.1 Reduction of IOP may prevent or delay visual field loss in patients with glaucoma or ocular hypertension;4,6 thus, monotherapy with IOP-lowering medications is standard-of-care treatment. However, many patients require multiple IOP-lowering therapies to reach their target IOP.15,91 Drug washout during concomitant administration of multiple medications44 and low adherence and persistence with complex glaucoma therapeutic regimens22,24,27 may reduce the effectiveness of multidrug regimens. Fixed-combination medications prevent drug washout, simplify dosing regimens, and may reduce costs,92 thereby potentially increasing medication adherence21,51,93,94 and persistence.20,21 BBFC provides IOP-lowering efficacy greater than or similar to various monotherapy and fixed-combination medications, with potentially improved convenience and better tolerability.
Acknowledgments
Medical writing support was provided by Jillian Gee, PhD, CMPP, of Complete Healthcare Communications, Inc. (Chadds Ford, PA, USA), and was funded by Alcon Laboratories, Inc.
Disclosure
Dr Nguyen is on the speakers bureau for Alcon Laboratories, Inc., and Allergan, Inc., (Irvine, CA, USA).
References
Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90(3):262–267. | ||
Casson RJ, Chidlow G, Wood JP, Crowston JG, Goldberg I. Definition of glaucoma: clinical and experimental concepts. Clin Experiment Ophthalmol. 2012;40(4):341–349. | ||
Peters D, Bengtsson B, Heijl A. Factors associated with lifetime risk of open-angle glaucoma blindness. Acta Ophthalmol. Epub 2013 Jul 10. | ||
Collaborative Normal-Tension Glaucoma Study Group. Comparison of glaucomatous progression between untreated patients with normal-tension glaucoma and patients with therapeutically reduced intraocular pressures. Am J Ophthalmol. 1998;126(4):487–497. | ||
American Academy of Ophthalmology Glaucoma Panel. Preferred Practice Pattern® Guidelines. Primary Open-Angle Glaucoma. San Francisco, CA: American Academy of Ophthalmology; 2010. | ||
The AGIS Investigators. The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol. 2000;130(4):429–440. | ||
Webers CA, Beckers HJ, Nuijts RM, Schouten JS. Pharmacological management of primary open-angle glaucoma: second-line options and beyond. Drugs Aging. 2008;25(9):729–759. | ||
Realini T. A history of glaucoma pharmacology. Optom Vis Sci. 2011;88(1):36–38. | ||
Nguyen QH. The role of prostaglandin analogues in the treatment of glaucoma in the 21st century. Int Ophthalmol Clin. 2004;44(2):15–27. | ||
Watanabe K, Chiou GC. Action mechanism of timolol to lower the intraocular pressure in rabbits. Ophthalmic Res. 1983;15(3):160–167. | ||
Mincione F, Scozzafava A, Supuran CT. The development of topically acting carbonic anhydrase inhibitors as anti-glaucoma agents. Curr Top Med Chem. 2007;7(9):849–854. | ||
Toris CB, Gabelt BT, Kaufman PL. Update on the mechanism of action of topical prostaglandins for intraocular pressure reduction. Surv Ophthalmol. 2008;53 Suppl 1:S107–S120. | ||
Arthur S, Cantor LB. Update on the role of alpha-agonists in glaucoma management. Exp Eye Res. 2011;93(3):271–283. | ||
European Glaucoma Society. Terminology and Guidelines for Glaucoma. 3rd ed. Bern, Switzerland: European Glaucoma Society. Available at: http://www.eugs.org/eng/EGS_guidelines.asp. Accessed January 24, 2014. | ||
Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):701–713. | ||
Reardon G, Kotak S, Schwartz GF. Objective assessment of compliance and persistence among patients treated for glaucoma and ocular hypertension: a systematic review. Patient Prefer Adherence. 2011;5:441–463. | ||
Arias A, Schargel K, Ussa F, Canut MI, Robles AY, Sanchez BM. Patient persistence with first-line antiglaucomatous monotherapy. Clin Ophthalmol. 2010;4:261–267. | ||
Nordstrom BL, Friedman DS, Mozaffari E, Quigley HA, Walker AM. Persistence and adherence with topical glaucoma therapy. Am J Ophthalmol. 2005;140(4):598–606. | ||
Wilensky J, Fiscella RG, Carlson AM, Morris LS, Walt J. Measurement of persistence and adherence to regimens of IOP-lowering glaucoma medications using pharmacy claims data. Am J Ophthalmol. 2006;141(1 Suppl):S28–S33. | ||
Higginbotham EJ, Hansen J, Davis EJ, Walt JG, Guckian A. Glaucoma medication persistence with a fixed combination versus multiple bottles. Curr Med Res Opin. 2009;25(10):2543–2547. | ||
Schwartz G, Burk C, Bennett T, Patel VD. Adherence and persistence with glaucoma therapy: brimonidine/timolol versus dorzolamide/timolol and various two-bottle combinations. J Clin Exp Ophthalmol. 2012;3(8):1–6. | ||
Rossi GC, Pasinetti GM, Scudeller L, Radaelli R, Bianchi PE. Do adherence rates and glaucomatous visual field progression correlate? Eur J Ophthalmol. 2011;21(4):410–414. | ||
Djafari F, Lesk MR, Harasymowycz PJ, Desjardins D, Lachaine J. Determinants of adherence to glaucoma medical therapy in a long-term patient population. J Glaucoma. 2009;18(3):238–243. | ||
Friedman DS, Okeke CO, Jampel HD, et al. Risk factors for poor adherence to eyedrops in electronically monitored patients with glaucoma. Ophthalmology. 2009;116(6):1097–1105. | ||
Okeke CO, Quigley HA, Jampel HD, et al. Adherence with topical glaucoma medication monitored electronically: the Travatan Dosing Aid study. Ophthalmology. 2009;116(2):191–199. | ||
Rees G, Leong O, Crowston JG, Lamoureux EL. Intentional and unintentional nonadherence to ocular hypotensive treatment in patients with glaucoma. Ophthalmology. 2010;117(5):903–908. | ||
Sleath B, Robin AL, Covert D, Byrd JE, Tudor G, Svarstad B. Patient-reported behavior and problems in using glaucoma medications. Ophthalmology. 2006;113(3):431–436. | ||
Ung C, Zhang E, Alfaro T, et al. Glaucoma severity and medication adherence in a county hospital population. Ophthalmology. 2013;120(6):1150–1157. | ||
Vandenbroeck S, De Geest S, Dobbels F, Fieuws S, Stalmans I, Zeyen T. Prevalence and correlates of self-reported nonadherence with eye drop treatment: the Belgian Compliance Study in Ophthalmology (BCSO). J Glaucoma. 2011;20(7):414–421. | ||
Hong S, Kang SY, Yoon JU, Kang U, Seong GJ, Kim CY. Drug attitude and adherence to anti-glaucoma medication. Yonsei Med J. 2010;51(2): 261–269. | ||
Olthoff CM, Hoevenaars JG, van den Borne BW, Webers CA, Schouten JS. Prevalence and determinants of non-adherence to topical hypotensive treatment in Dutch glaucoma patients. Graefes Arch Clin Exp Ophthalmol. 2009;247(2):235–243. | ||
Loon SC, Jin J, Jin Goh M. The relationship between quality of life and adherence to medication in glaucoma patients in Singapore. J Glaucoma. Epub 2013 Nov 16. | ||
Rees G, Chong XL, Cheung CY, et al. Beliefs and adherence to glaucoma treatment: a comparison of patients from diverse cultures. J Glaucoma. Epub 2013 Jan 31. | ||
Buller AJ, Connell B, Spencer AF. Compliance: clear communication’s critical. Br J Ophthalmol. 2005;89(10):1370. | ||
Dreer LE, Girkin C, Mansberger SL. Determinants of medication adherence to topical glaucoma therapy. J Glaucoma. 2012;21(4):234–240. | ||
Kholdebarin R, Campbell RJ, Jin YP, Buys YM. Multicenter study of compliance and drop administration in glaucoma. Can J Ophthalmol. 2008;43(4):454–461. | ||
Nordmann JP, Baudouin C, Renard JP, et al. Measurement of treatment compliance using a medical device for glaucoma patients associated with intraocular pressure control: a survey. Clin Ophthalmol. 2010;4: 731–739. | ||
Forsman E, Kivela T, Vesti E. Lifetime visual disability in open-angle glaucoma and ocular hypertension. J Glaucoma. 2007;16(3):313–319. | ||
Vorwerk C, Thelen U, Buchholz P, Kimmich F. Treatment of glaucoma patients with insufficient intraocular pressure control: a survey of German ophthalmologists in private practice. Curr Med Res Opin. 2008;24(5):1295–1301. | ||
Friedman DS, Hahn SR, Gelb L, et al. Doctor-patient communication, health-related beliefs, and adherence in glaucoma results from the Glaucoma Adherence and Persistency Study. Ophthalmology. 2008;115(8): 1320–1327, 1327.e1–e3. | ||
Robin AL, Novack GD, Covert DW, Crockett RS, Marcic TS. Adherence in glaucoma: objective measurements of once-daily and adjunctive medication use. Am J Ophthalmol. 2007;144(4):533–540. | ||
Tsai JC, McClure CA, Ramos SE, Schlundt DG, Pichert JW. Compliance barriers in glaucoma: a systematic classification. J Glaucoma. 2003; 12(5):393–398. | ||
Robin AL, Covert D. Does adjunctive glaucoma therapy affect adherence to the initial primary therapy? Ophthalmology. 2005;112(5):863–868. | ||
Chrai SS, Makoid MC, Eriksen SP, Robinson JR. Drop size and initial dosing frequency problems of topically applied ophthalmic drugs. J Pharm Sci. 1974;63(3):333–338. | ||
Buller A, Hercules BL. Should patients choose their own eyedrops? Acta Ophthalmol Scand. 2006;84(1):150–151. | ||
Liang H, Brignole-Baudouin F, Pauly A, Riancho L, Baudouin C. Polyquad-preserved travoprost/timolol, benzalkonium chloride (BAK)-preserved travoprost/timolol, and latanoprost/timolol in fixed combinations: a rabbit ocular surface study. Adv Ther. 2011;28(4):311–325. | ||
Pisella PJ, Pouliquen P, Baudouin C. Prevalence of ocular symptoms and signs with preserved and preservative free glaucoma medication. Br J Ophthalmol. 2002;86(4):418–423. | ||
Higginbotham EJ. Considerations in glaucoma therapy: fixed combinations versus their component medications. Clin Ophthalmol. 2010;4:1–9. | ||
Hommer A, Thygesen J, Ferreras A, et al. A European perspective on costs and cost effectiveness of ophthalmic combinations in the treatment of open-angle glaucoma. Eur J Ophthalmol. 2008;18(5):778–786. | ||
Inoue K, Setogawa A, Higa R, Moriyama R, Wakakura M, Tomita G. Ocular hypotensive effect and safety of travoprost 0.004%/timolol maleate 0.5% fixed combination after change of treatment regimen from beta-blockers and prostaglandin analogs. Clin Ophthalmol. 2012;6:231–235. | ||
Inoue K, Okayama R, Higa R, Sawada H, Wakakura M, Tomita G. Ocular hypotensive effects and safety over 3 months of switching from an unfixed combination to latanoprost 0.005%/timolol maleate 0.5% fixed combination. J Ocul Pharmacol Ther. 2011;27(6):581–587. | ||
Kitazawa Y, Smith P, Sasaki N, Kotake S, Bae K, Iwamoto Y. Travoprost 0.004%/timolol 0.5%-fixed combination with and without benzalkonium chloride: a prospective, randomized, doubled-masked comparison of safety and efficacy. Eye (Lond). 2011;25(9):1161–1169. | ||
Katz G, Dubiner H, Samples J, Vold S, Sall K. Three-month randomized trial of fixed-combination brinzolamide, 1%, and brimonidine, 0.2%. JAMA Ophthalmol. 2013;131(6):724–730. | ||
Nguyen QH, McMenemy MG, Realini T, Whitson JT, Goode SM. Phase III randomized 3-month trial with an ongoing 3-month safety extension of fixed-combination brinzolamide 1%/brimonidine 0.2%. J Ocul Pharmacol Ther. 2013;29(3):290–297. | ||
Realini T, Nguyen QH, Katz G, Dubiner H. Fixed-combination brinzolamide 1%/brimonidine 0.2% vs monotherapy with brinzolamide or brimonidine in patients with open-angle glaucoma or ocular hypertension: results of a pooled analysis of two phase III studies. Eye (Lond). 2013;27(7):841–847. | ||
Whitson JT, Realini T, Nguyen QH, McMenemy MG, Goode SM. Six-month results from a phase III randomized trial of fixed-combination brinzolamide 1% + brimonidine 0.2% versus brinzolamide or brimonidine monotherapy in glaucoma or ocular hypertension. Clin Ophthalmol. 2013;7:1053–1060. | ||
Leske MC, Heijl A, Hussein M, et al. Factors for glaucoma progression and the effect of treatment: the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2003;121(1):48–56. | ||
Quaranta L, Katsanos A, Russo A, Riva I. 24-hour intraocular pressure and ocular perfusion pressure in glaucoma. Surv Ophthalmol. 2013; 58(1):26–41. | ||
Konstas AG, Quaranta L, Yan DB, et al. Twenty-four hour efficacy with the dorzolamide/timolol-fixed combination compared with the brimonidine/timolol-fixed combination in primary open-angle glaucoma. Eye (Lond). 2012;26(1):80–87. | ||
Liu JH, Medeiros FA, Slight JR, Weinreb RN. Comparing diurnal and nocturnal effects of brinzolamide and timolol on intraocular pressure in patients receiving latanoprost monotherapy. Ophthalmology. 2009;116(3):449–454. | ||
Ishikawa M, Yoshitomi T. Effects of brinzolamide vs timolol as an adjunctive medication to latanoprost on circadian intraocular pressure control in primary open-angle glaucoma Japanese patients. Clin Ophthalmol. 2009;3:493–500. | ||
van der Valk R, Webers CA, Schouten JS, Zeegers MP, Hendrikse F, Prins MH. Intraocular pressure-lowering effects of all commonly used glaucoma drugs: a meta-analysis of randomized clinical trials. Ophthalmology. 2005;112(7):1177–1185. | ||
Cheng JW, Cheng SW, Gao LD, Lu GC, Wei RL. Intraocular pressure-lowering effects of commonly used fixed-combination drugs with timolol: a systematic review and meta-analysis. PLoS ONE. 2012;7(9):e45079. | ||
Boyle JE, Ghosh K, Gieser DK, Adamsons IA. A randomized trial comparing the dorzolamide-timolol combination given twice daily to monotherapy with timolol and dorzolamide. Dorzolamide-Timolol Study Group. Ophthalmology. 1998;105(10):1945–1951. | ||
Brandt JD, Cantor LB, Katz LJ, et al. Bimatoprost/timolol fixed combination: a 3-month double-masked, randomized parallel comparison to its individual components in patients with glaucoma or ocular hypertension. J Glaucoma. 2008;17(3):211–216. | ||
Craven ER, Walters TR, Williams R, et al. Brimonidine and timolol fixed-combination therapy versus monotherapy: a 3-month randomized trial in patients with glaucoma or ocular hypertension. J Ocul Pharmacol Ther. 2005;21(4):337–348. | ||
Higginbotham EJ, Feldman R, Stiles M, Dubiner H; Fixed Combination Investigative Group. Latanoprost and timolol combination therapy vs monotherapy: one-year randomized trial. Arch Ophthalmol. 2002;120(7):915–922. | ||
Higginbotham EJ, Olander KW, Kim EE, et al. Fixed combination of latanoprost and timolol vs individual components for primary open-angle glaucoma or ocular hypertension: a randomized, double-masked study. Arch Ophthalmol. 2010;128(2):165–172. | ||
Hughes BA, Bacharach J, Craven ER, et al. A three-month, multicenter, double-masked study of the safety and efficacy of travoprost 0.004%/timolol 0.5% ophthalmic solution compared to travoprost 0.004% ophthalmic solution and timolol 0.5% dosed concomitantly in subjects with open angle glaucoma or ocular hypertension. J Glaucoma. 2005;14(5): 392–399. | ||
Hutzelmann J, Owens S, Shedden A, Adamsons I, Vargas E. Comparison of the safety and efficacy of the fixed combination of dorzolamide/timolol and the concomitant administration of dorzolamide and timolol: a clinical equivalence study. International Clinical Equivalence Study Group. Br J Ophthalmol. 1998;82(11):1249–1253. | ||
Palmberg P, Kim EE, Kwok KK, Tressler CS; Canada and United States Fixed Combination Latanoprost/Timolol Study Group. A 12-week, randomized, double-masked study of fixed combination latanoprost/timolol versus latanoprost or timolol monotherapy. Eur J Ophthalmol. 2010;20(4):708–718. | ||
Pfeiffer N; European Latanoprost Fixed Combination Study Group. A comparison of the fixed combination of latanoprost and timolol with its individual components. Graefes Arch Clin Exp Ophthalmol. 2002;240(11):893–899. | ||
Sherwood MB, Craven ER, Chou C, et al. Twice-daily 0.2% brimonidine-0.5% timolol fixed-combination therapy vs monotherapy with timolol or brimonidine in patients with glaucoma or ocular hypertension: a 12-month randomized trial. Arch Ophthalmol. 2006;124(9):1230–1238. | ||
Strohmaier K, Snyder E, DuBiner H, Adamsons I. The efficacy and safety of the dorzolamide-timolol combination versus the concomitant administration of its components. Dorzolamide-Timolol Study Group. Ophthalmology. 1998;105(10):1936–1944. | ||
Kaback M, Scoper SV, Arzeno G, et al. Intraocular pressure-lowering efficacy of brinzolamide 1%/timolol 0.5% fixed combination compared with brinzolamide 1% and timolol 0.5%. Ophthalmology. 2008;115(10):1728–1734. | ||
Diestelhorst M, Larsson LI; European Latanoprost Fixed Combination Study Group. A 12 week study comparing the fixed combination of latanoprost and timolol with the concomitant use of the individual components in patients with open angle glaucoma and ocular hypertension. Br J Ophthalmol. 2004;88(2):199–203. | ||
Jaenen N, Baudouin C, Pouliquen P, Manni G, Figueiredo A, Zeyen T. Ocular symptoms and signs with preserved and preservative-free glaucoma medications. Eur J Ophthalmol. 2007;17(3):341–349. | ||
Kuppens EV, de Jong CA, Stolwijk TR, de Keizer RJ, van Best JA. Effect of timolol with and without preservative on the basal tear turnover in glaucoma. Br J Ophthalmol. 1995;79(4):339–342. | ||
Quaranta L, Biagioli E, Riva I, et al. Prostaglandin analogs and timolol-fixed versus unfixed combinations or monotherapy for open-angle glaucoma: a systematic review and meta-analysis. J Ocul Pharmacol Ther. 2013;29(4):382–389. | ||
Schuman JS. Clinical experience with brimonidine 0.2% and timolol 0.5% in glaucoma and ocular hypertension. Surv Ophthalmol. 1996;41 Suppl 1:S27–S37. | ||
Melamed S, David R. Ongoing clinical assessment of the safety profile and efficacy of brimonidine compared with timolol: year-three results. Brimonidine Study Group II. Clin Ther. 2000;22(1):103–111. | ||
Quaranta L, Gandolfo F, Turano R, et al. Effects of topical hypotensive drugs on circadian IOP, blood pressure, and calculated diastolic ocular perfusion pressure in patients with glaucoma. Invest Ophthalmol Vis Sci. 2006;47(7):2917–2923. | ||
Bonomi L, Marchini G, Marraffa M, Bernardi P, Morbio R, Varotto A. Vascular risk factors for primary open angle glaucoma: the Egna-Neumarkt Study. Ophthalmology. 2000;107(7):1287–1293. | ||
Heijl A, Bengtsson B, Oskarsdottir SE. Prevalence and severity of undetected manifest glaucoma: results from the early manifest glaucoma trial screening. Ophthalmology. 2013;120(8):1541–1545. | ||
Schuman JS. Effects of systemic beta-blocker therapy on the efficacy and safety of topical brimonidine and timolol. Brimonidine Study Groups 1 and 2. Ophthalmology. 2000;107(6):1171–1177. | ||
Bauer K, Brunner-Ferber F, Distlerath LM, et al. Assessment of systemic effects of different ophthalmic beta-blockers in healthy volunteers. Clin Pharmacol Ther. 1991;49(6):658–664. | ||
Javitt JC, Schiffman RM. Clinical success and quality of life with brimonidine 0.2% or timolol 0.5% used twice daily in glaucoma or ocular hypertension: a randomized clinical trial. Brimonidine Outcomes Study Group I. J Glaucoma. 2000;9(3):224–234. | ||
Kass MA, Gordon MO, Hoff MR, et al. Topical timolol administration reduces the incidence of glaucomatous damage in ocular hypertensive individuals. A randomized, double-masked, long-term clinical trial. Arch Ophthalmol. 1989;107(11):1590–1598. | ||
Uusitalo H, Kahonen M, Ropo A, et al. Improved systemic safety and risk-benefit ratio of topical 0.1% timolol hydrogel compared with 0.5% timolol aqueous solution in the treatment of glaucoma. Graefes Arch Clin Exp Ophthalmol. 2006;244(11):1491–1496. | ||
Waldock A, Snape J, Graham CM. Effects of glaucoma medications on the cardiorespiratory and intraocular pressure status of newly diagnosed glaucoma patients. Br J Ophthalmol. 2000;84(7):710–713. | ||
McCarty CA, Mukesh BN, Kitchner TE, et al. Intraocular pressure response to medication in a clinical setting: the Marshfield Clinic Personalized Medicine Research Project. J Glaucoma. 2008;17(5):372–377. | ||
Hommer A. Role of fixed combinations in the management of open-angle glaucoma. Expert Rev Pharmacoecon Outcomes Res. 2011;11(1):91–99. | ||
Dickson M, Plauschinat CA. Compliance with antihypertensive therapy in the elderly: a comparison of fixed-dose combination amlodipine/benazepril versus component-based free-combination therapy. Am J Cardiovasc Drugs. 2008;8(1):45–50. | ||
Taylor AA, Shoheiber O. Adherence to antihypertensive therapy with fixed-dose amlodipine besylate/benazepril HCl versus comparable component-based therapy. Congest Heart Fail. 2003;9(6):324–332. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


