Back to Journals » Clinical Optometry » Volume 15
Combination of Bandage Contact Lens and Autologous Serum Eye Drop for the Treatment of Superior Limbic Keratoconjunctivitis
Authors Noor NA
Received 10 January 2023
Accepted for publication 17 April 2023
Published 20 April 2023 Volume 2023:15 Pages 75—80
DOI https://doi.org/10.2147/OPTO.S404164
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Mr Simon Berry
Nina Asrini Noor
JEC Eye Hospitals and Clinics, Jakarta, Indonesia
Correspondence: Nina Asrini Noor, JEC Eye Hospital Kedoya, Jalan Terusan Arjuna Utara No. 1, Kedoya, Jakarta, 11520, Indonesia, Tel +62 813 9520 9670, Email [email protected]
Purpose: To report clinical improvement after combined treatment of bandage contact lens and autologous serum eye drop in a patient with superior limbic keratoconjunctivitis (SLK) complicated with dry eye disease (DED) and meibomian gland dysfunction (MGD).
Patients and Methods: Case report.
Results: A 60-year-old woman was referred for unilateral chronic recurrent redness of the left eye not responding to topical steroids and cyclosporine 0.1% eye drop. She was diagnosed with SLK, which was complicated by the presence of DED and MGD. The patient was then commenced with autologous serum eye drop and fitted with silicone hydrogel contact lens in her left eye, and treated with intense pulsed light therapy for MGD in both eyes. Remission was seen Information Classification: General serum eye drop and bandage contact lens wear.
Conclusion: Long-term application of autologous serum eye drop combined with bandage contact lens can be used as an alternative treatment approach in SLK.
Keywords: autologous serum, bandage contact lens, cornea, dry eye, superior limbic keratoconjunctivitis
Introduction
Superior limbic keratoconjunctivitis (SLK) is an ocular surface disease of unknown etiology, which was first described in 1963 by Theodore, and is characterized by chronic inflammation of the superior limbus and superior bulbar conjunctiva.1 SLK predominantly affects women between the ages of 30 and 55 years.2,3 It usually affects both eyes, but often one eye is more severely involved than the other.2 Irritation, burning, redness, foreign body sensation, and photophobia are common complaints related to SLK. Although the pathogenesis of SLK is not fully understood, mechanical, infectious, and immunological etiologies have been postulated.3–6 SLK has been reported to be associated with dry eye disease (DED) and may present in conjunction with other conventional dry eye causes such as meibomian gland dysfunction (MGD).7 However, the reason why only a particular subset of patients develop SLK is still unclear.8
SLK has been treated with surgical and nonsurgical therapy. Surgical approaches include conjunctival resection with or without graft, cauterization, and cryotherapy. Nonsurgical treatments for SLK primarily aim to reduce mechanical friction and ocular surface irritation. This may include artificial tears, autologous serum eye drop (auto-SED), topical vitamin A, punctal occlusion, topical immunomodulators, pressure patching, and therapeutic bandage contact lens (BCL).9
Up to date, the literature reporting the use of combined BCL and auto-SED is limited to cases of persistent epithelial defects.10 Here, we report the first case of using auto-SED and BCL combined with intense pulsed light (IPL) therapy in a patient with SLK complicated by the presence of MGD.
Case Report
A 60-year-old woman was referred to the dry eye clinic at JEC Eye Hospital Kedoya for chronic recurrent redness of her left eye (LE) in the past 6 months prior to her visit. Her past medical history was negative for autoimmune disease and thyroid dysfunction. She had been using spectacles since her early adulthood period and was also diagnosed with anisometropia of the LE. She did not have any history of ocular surgery in either of her eyes. At the time of the referral, she had been using cyclosporine 0.1% eye drop once per day and fluorometholone eye drop four times per day for 1 month and tear substitute every three hours. However, she did not feel any improvement under these medications. The history of her right eye (RE) was unremarkable.
On examinations, the best corrected visual acuity (BCVA) was 20/20 in the RE with S3.25 correction and 20/40 in the LE with S-18.00 correction. Intraocular pressure (IOP) of both eyes was within normal limits. At slit lamp examination, the LE showed significant conjunctival hyperemia and redundancy in the superior bulbar area (Figure 1). Positive fluorescein staining was observed on the superior bulbar conjunctiva and superior limbus. The lens of LE showed grade 2 nuclear sclerosis. There was plugging of meibomian gland orifices consistent with MGD in both eyes. The tear break-up time (TBUT) was shortened to 4 seconds in RE and 2 seconds in LE. Schirmer’s test without anesthesia was 5 mm on the RE and 2 mm on the LE at 5 minutes. Meibography (Oculus Keratograph 5M, Oculus, Wetzlar, Germany) was performed to evaluate the degree and severity of MGD in both eyes (Figure 2) which revealed grade 1 meibomian gland loss.
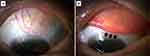 |
Figure 1 Slit lamp examination at initial presentation revealed (A) a localized hyperemia and (B) redundant folds (pointed with black arrows) of the superior bulbar conjunctiva. |
 |
Figure 2 Meibography examination revealed grade 1 meibomian gland loss on superior eyelid of (A) right eye and (B) left eye. |
Her final diagnosis at initial presentation was SLK, mixed type of dry eye disease related to aqueous deficiency and MGD, and senile cataract of the LE. Several treatment alternatives were discussed, including the option to continue cyclosporine 0.1% eye drop which she refused due to intolerable stinging sensations. She was also not keen on punctal occlusion. Accordingly, she opted for treatment combination of auto-SED 50% concentration and silicone hydrogel contact lens (Air Optix Aqua, Alcon, 33% water content) which acted as therapeutic BCL and myopia correction, together with non-preserved lubricants every 1 to 2 hours. She agreed to wear the contact lens during her working hours (6 to 8 hours per day) and administer auto-SED at home (at least 6 times per day), since it was bothersome for her to use the auto-SED at work. In terms of MGD, we decided to perform intense pulsed light (IPL) therapy using the E-Eye® device (E-Swin, Houdan, France), which was done in 3 sessions with 4-weeks interval. We also discussed the possibility of cataract surgery for her LE once the ocular surface condition has improved, to prevent worsening of symptoms after the surgery.
On review 3 months after her initial visit, the patient had symptomatic relief in her LE. Slit lamp examination revealed significant reduction of inflammation on the superior bulbar conjunctiva of the LE (Figure 3A), and no fluorescein staining was visible. Treatment regimens with auto-SED, contact lens wear, and non-preserved lubricants were continued.
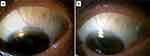 |
Figure 3 Slit lamp examination at (A) three months and (B) two years after treatment commencement showed significant reduction of the inflammation over the superior bulbar conjunctiva. |
Two years following her presentation, the patient remained asymptomatic. Mild superior conjunctival hyperemia without fluorescein staining was found on examination of the LE (Figure 3B). TBUT of both eyes were more than 5 seconds. Schirmer test was done, and the results were 6 and 5 mm of RE and LE, respectively. Meibography was suggested in order to evaluate the extent of meibomian gland loss after treatment. Unfortunately, she refused to do the examination. As for the treatment, she did not mind continuing to wear contact lens and administer auto-SED, especially now that she only needed to use the auto-SED 3 to 4 times per day.
Discussion
Previous study reported that SLK may be present in combination with other dry eye causes such as MGD and DED with decreased tear secretion.9 We found that our patient had unilateral SLK complicated by the presence of aqueous deficiency and MGD. Both the TBUT and Schirmer’s test results in our patient’s LE were poorer than her RE. Given the contribution of aqueous deficiency and MGD to the severity of SLK in this patient, identifying and treating both conditions was important. Punctal plugs insertion was suggested to the patient for the treatment of aqueous deficiency. Unfortunately, she did not consent for punctal occlusion.
Our patient’s MGD was treated using IPL, which was first used to treat MGD in 2015.11 However, the protocols for IPL treatment differed greatly between studies.12 The protocol in this case report was as follows: five adjacent intense pulsed light flashes were applied to the skin area directly below the lower eyelid and on the temple of both eyes. Treatments were given three times at four-week intervals, with a pulse intensity of 12.1 J/cm2 based on the patient’s skin type as established by the Fitzpatrick grading scale.13 The treatments were carried out on clean skin, with a 5.0 mm layer of conductive gel applied to the treatment area and the patient wearing opaque safety goggles. According to the most current meta-analysis, IPL is a safe and effective treatment for patients with MGD-related dry eye.14 Previous study has indicated that IPL treatment reduced MG dropout by 4–5% after the treatment.15,16 Unfortunately, the patient refused to have the meibography examination repeated at the follow-up visit, hence the degree of improvement in this case study remained unknown.
The primary treatment option for our patient was nonsurgical therapy. Cyclosporine 0.1% eye drop was initiated by the previous physician, and should be able to treat both SLK and DED.17 However, she refused to continue the medication due to its side effects. Thus, the treatment combination of BCL and auto-SED was chosen.
Therapeutic contact lenses are frequently used in the treatment of a wide range of corneal and ocular surface diseases (OSDs) with a variety of purposes.18 The indications for therapeutic contact lenses in this case were to enhance corneal healing in dry eyes and to provide mechanical protection from friction caused by SLK. BCL is commonly used for extended wear. However, extended lens wear increases the risk of complications, including infective keratitis. To avoid such risk, daily lens wear was recommended for this patient rather than extended lens wear. Auto-SED was administered for the remainder of the day, during which she did not wear contact lenses. Although it did not fit the definition of bandage CL, which typically involves extended wear, it was demonstrated that even a shorter duration of lens wear might potentially benefit the patient in the same way as extended wear could.
The rationale for this combination came from a previous study that suggested a combination of BCL and auto-SED could be used in cases of persistent epithelial defects.10 The use of BCL can reduce the force from blinking onto the superior limbus as it has a lower mechanical stiffness and elastic modulus.19 BCL wear reduces the tactile corneal reflex, which would then decrease reflex blinking.20 This would protect the superior limbus from the mechanical friction associated with blinking and may also break the cycle in SLK. BCL may also help aqueous deficiency dry eye, which can accompany SLK, by ensuring a continuous precorneal tear film.21
Auto-SED application is now considered one of the treatment modalities for severe types of DED and SLK.22,23 Serum contains numerous factors that are present in the tear film, including vitamin A, epidermal growth factor (EGF), transforming growth factor β (TGF-β), insulin-like growth factor, and substance P. Serum also contains proteins in high concentrations, such as prealbumin, which may be essential to the stability of the tear film. Serum can supply the ocular surface with most of the components needed to maintain proliferation and differentiation.23
As previously mentioned, autologous serum drops were made.22 In summary, venipuncture was used to draw 40 mL of blood. To ensure full clotting, the containers are allowed at room temperature for 2 hours in an upright posture before being spun in a laboratory centrifuge at 3000 g for 15 minutes. The serum was isolated in a sterile manner and diluted to 50% with saline. The final preparation was placed in a 5-mL bottle with UV light protection. The patient was instructed to use the auto-SED at least six times each day, in addition to their regular routine of preservative-free lubricants. While in use, auto-SED can be stored for less than one month at 4°C and up to three months at 20°C. However, several studies have found that using drops from the same container in the fridge repeatedly increases the risk of bacterial and fungal infection.24,25 As a result, it was recommended that one serum bottle be used for up to one week and then discarded to prevent the risk of infection from repeated use of the same bottle.
In this case, auto-SED with a 50% concentration was chosen, instead of 20% or 100%. Recent literature indicates that auto-SED with higher concentration was more effective,26 which is why we did not use the 20% concentration for our patient. Auto-SED at 100% is associated with higher reduction of symptoms and corneal epitheliopathy,27 but 50% dilution was preferred for several reasons. Firstly, the human serum concentration of TGF-β, which has an antiproliferative effect, is five times higher than the amount of TGF-β in normal tears.28 Subsequently, high concentrations of this molecule may suppress corneal wound healing.27–29 Secondly, higher concentration of proteins in 100% auto-SED may alter the tear film osmolarity, which is an important pathogenic factor in DED.30 Lastly, auto-SED at 100% concentration requires double the amount of blood for its preparation compared to 50%. All things considered, we believed that 50% concentration was safer and more practical.
When auto-SED and BCL are used concurrently, it should be kept in mind that combined treatment, especially when using hydrogel contact lens, may cause increased development of deposits on the contact lens surface, likely to be albumin. Alternatively, silicone hydrogel contact lenses can be used as BCL. Although lipid deposition may occur due to their relatively hydrophobic surface, silicone hydrogel lenses show significantly reduced protein deposition, which could be an advantage for their combined use with auto-SED.10 Therefore, contact lens with silicone hydrogel material was chosen in this case.
At the most recent follow-up, not only was SLK improved, but also dry eye disease, as TBUT and Schirmer test scores were shown to be improved compared to initial examinations. Each treatment modality targeted a different pathology. Auto-SED and BCL were directed towards SLK and DED in general, whereas IPL therapy was directed especially at MGD. Unfortunately, this case report could not provide clinical findings that supported the improvement of MGD after IPL treatment. Nevertheless, improvement of overall symptoms and signs was observed in this patient.
Conclusion
This case report described our experience with BCL and auto-SED for the management of SLK combined with IPL treatment for MGD-related DED. The treatment combination could act as an alternative to the conventional treatment regimen and provide improvement in SLK, complicated by the presence of mixed form of DED.
Ethics and Consent Statement
Review and approval for case report study was not required by IRB in our institution. However, informed consent to publish this case report was obtained from the patient in writing.
Disclosure
The author reports no conflicts of interest in this work.
References
1. Theodore FH. Superior limbic keratoconjunctivitis. Eye Ear Nose Throat Mon. 1963;42:25–28.
2. Nelson JD. Superior limbic keratoconjunctivitis (SLK). Eye. 1989;3:180–189. doi:10.1038/eye.1989.26
3. Cher I. Superior limbic keratoconjunctivitis: multifactorial mechanical pathogenesis. Clin Experiment Ophthalmol. 2000;28:181–184. doi:10.1046/j.1442-9071.2000.00284.x
4. Theodore FH. Superior limbic keratoconjunctivitis. Arch Ophthalmol. 1983;101:1627–1629. doi:10.1001/archopht.1983.01040020629032
5. Theodore FH. Further observations on superior limbic keratoconjunctivitis. Trans Am Acad Ophthalmol Otolaryngol. 1967;71:341–351.
6. Matsuda A, Tagawa Y, Matsuda H. TGF-beta 2, tenascin, and integrin beta 1 expression in superior limbic keratoconjunctivitis. Jpn J Ophthalmol. 1999;43:251–256. doi:10.1016/S0021-5155(99)00021-0
7. Vu CHV, Kawashima M, Yamada M, et al. Influence of meibomian gland dysfunction and friction-related disease on the severity of dry eye. Ophthalmology. 2018;125(8):1181–1188. doi:10.1016/j.ophtha.2018.01.025
8. Goto E, Shimmura S, Shimazaki J, Tsubota K. Treatment of superior limbic keratoconjunctivitis by application of autologous serum. Cornea. 2001;20(8):807–810. doi:10.1097/00003226-200111000-00006
9. Lahoti S, Weiss M, Johnson DA, Kheirkhah A. Superior limbic keratoconjunctivitis: a comprehensive review. Surv Ophthalmol. 2022;67(2):331–341. doi:10.1016/j.survophthal.2021.05.009
10. Schrader S, Wedel T, Moll R, Geerling G. Combination of serum eye drops with hydrogel bandage contact lenses in the treatment of persistent epithelial defects. Graefes Arch Clin Exp Ophthalmol. 2006;244(10):1345–1349. doi:10.1007/s00417-006-0257-y
11. Toyos R, McGill W, Briscoe D. Intense pulsed light treatment for dry eye disease due to meibomian gland dysfunction; a 3-year retrospective study. Photomed Laser Surg. 2015;33(1):41–46. doi:10.1089/pho.2014.3819
12. Cote S, Zhang AC, Ahmadzai V, et al. Intense pulsed light (IPL) therapy for the treatment of meibomian gland dysfunction. Cochrane Database Syst Rev. 2020;3(3):CD013559. doi:10.1002/14651858.CD013559
13. Fitzpatrick T. The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol. 1988;124:869–871. doi:10.1001/archderm.1988.01670060015008
14. Liu C, Zhou Q, Gao ZQ. Efficacy of intense pulsed light and meibomian gland expression treatments in meibomian gland dysfunction: a meta-analysis of randomized controlled trials. Medicine. 2022;101(51):e32292. doi:10.1097/MD.0000000000032292
15. Yin Y, Gong L. Reversibility of gland dropout and significance of eyelid hygiene treatment in meibomian gland dysfunction. Cornea. 2017;36(3):332–337. doi:10.1097/ICO.0000000000001042
16. Yin Y, Liu N, Gong L, Song N. Changes in the meibomian gland after exposure to intense pulsed light in Meibomian Gland Dysfunction (MGD) patients. Curr Eye Res. 2018;43(3):308–313. doi:10.1080/02713683.2017.1406525
17. Sahin A, Bozkurt B, Irkec M. Topical cyclosporine a in the treatment of superior limbic keratoconjunctivitis: a long-term follow-up. Cornea. 2008;27(2):193–195. doi:10.1097/ICO.0b013e318033bd25
18. Lim L, Lim EWL. Therapeutic contact lenses in the treatment of corneal and ocular surface diseases-a review. Asia Pac J Ophthalmol. 2020;9(6):524–532. doi:10.1097/APO.0000000000000331
19. Mondino BJ, Zaidman GW, Salamon SW. Use of pressure patching and soft contact lens in superior limbic keratoconjunctivitis. Arch Ophthalmol. 1982;100:1932–1934. doi:10.1001/archopht.1982.01030040912008
20. Burton H. Somatic sensations from the eye. In: Hart WM, editor. Adler’s Physiology of the Eye. St Louis: Mosby-Year Book; 1992:90.
21. John T, Mobilia EF, Kenyon KR. Therapeutic soft contact lens. In: Ruben M, Guillon M, editors. Contact Lens Practice. London: Chapman and Hall; 1994:
22. Tsubota K, Goto E, Fujita H, et al. Treatment of dry eye by autologous serum application in Sjögren’s syndrome. Br J Ophthalmol. 1999;83:390–395. doi:10.1136/bjo.83.4.390
23. Tsubota K, Satake Y, Ohyama M, et al. Surgical reconstruction of the ocular surface in advanced ocular cicatricial pemphigoid and Stevens-Johnson syndrome. Am J Ophthalmol. 1996;122:38–52. doi:10.1016/S0002-9394(14)71962-2
24. Poon AC, Geerling G, Dart JK, Fraenkel GE, Daniels JT. Autologous serum eyedrops for dry eyes and epithelial defects: clinical and in vitro toxicity studies. Br J Ophthalmol. 2001;85(10):1188–1197. doi:10.1136/bjo.85.10.1188
25. Tananuvat N, Daniell M, Sullivan LJ, et al. Controlled study of the use of autologous serum in dry eye patients. Cornea. 2001;20(8):802–806. doi:10.1097/00003226-200111000-00005
26. Semeraro F, Forbice E, Braga O, Bova A, Di Salvatore A, Azzolini C. Evaluation of the efficacy of 50% autologous serum eye drops in different ocular surface pathologies. Biomed Res Int. 2014;2014:826970. doi:10.1155/2014/826970
27. Cho YK, Huang W, Kim GY, Lim BS. Comparison of autologous serum eye drops with different diluents. Curr Eye Res. 2013;38(1):9–17. doi:10.3109/02713683.2012.720340
28. Gupta A, Monroy D, Ji Z, et al. Transforming growth factor beta-1 and beta-2 in human tear fluid. Curr Eye Res. 1996;15(6):605–614. doi:10.3109/02713689609008900
29. Terai K, Call MK, Liu H, et al. Crosstalk between TGF-β and MAPK signaling during corneal wound healing. Investig Opthalmol Vis Sci. 2011;52(11):8208. doi:10.1167/iovs.11-8017
30. Lemp MA, Bron AJ, Baudouin C, et al. Tear osmolarity in the diagnosis and management of dry eye disease. Am J Ophthalmol. 2011;151(5):792–798.e1. doi:10.1016/j.ajo.2010.10.032
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
