Back to Journals » Lung Cancer: Targets and Therapy » Volume 14
CodeBreak 200: Sotorasib Has Not Broken the KRASG12C Enigma Code
Authors Zhang SS , Lee A , Nagasaka M
Received 3 January 2023
Accepted for publication 4 April 2023
Published 19 April 2023 Volume 2023:14 Pages 27—30
DOI https://doi.org/10.2147/LCTT.S403461
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sai-Hong Ignatius Ou
Shannon S Zhang,1 Alexandria Lee,1 Misako Nagasaka1,2
1University of California Irvine School of Medicine, Orange, CA, USA; 2St. Marianna University School of Medicine, Kawasaki, Japan
Correspondence: Misako Nagasaka, University of California Irvine School of Medicine, Orange, CA, USA, Email [email protected]
Abstract: Thirteen percent of non-small cell lung cancer (NSCLC) patients are estimated to have the KRAS G12C mutation. Sotorasib is a novel KRAS G12C inhibitor that has shown promising results in preclinical and clinical studies, granting its conditional approval by the FDA in May 2021. The phase I clinical trial resulted in a confirmed response of 32% and progression free survival (PFS) of 6.3 months while the phase II trial resulted in a confirmed response of 37.1% and a PFS of 6.8 months. It was also shown to be tolerable with most subjects experiencing grade one or two adverse events, most commonly diarrhea and nausea. The CodeBreaK 200 phase III trial data have recently resulted and showed an improved PFS with the use of sotorasib at 5.6 months compared to that of standard docetaxel of 4.5 months in locally advanced or unresectable metastatic KRAS G12C NSCLC previously treated with at least one platinum-based chemotherapy and checkpoint inhibitor. The lower than expected PFS of sotorasib from the phase III trial opens up opportunities for other G12C inhibitors to join the field. Indeed, adagrasib, another G12C inhibitor just recently gained FDA accelerated approval in NSCLC patients based on the KRYSTAL-1 study where the response rate was 43% with a median duration of response of 8.5 months. With novel agents and combinations, the field of KRAS G12C is quickly evolving. While sotorasib was an exciting start, there is more to do to break the KRAS G12C Enigma code.
Keywords: sotorasib, AMG 510, non-small cell lung cancer, docetaxel, CodeBreaK 100, CodeBreaK 200, KRASG12C
Introduction
KRAS mutation occurs in 15–30% of all lung adenocarcinoma patients in the United States, most of whom are smokers or former smokers.1 KRAS mutations in codon 12 are the most common, making up 91% of all KRAS mutations. There are multiple forms of the codon 12 KRAS mutations including G12C, G12V, G12D, G12A, and G12S. First line treatment for KRAS non-small cell lung cancer (NSCLC) is usually composed of immune checkpoint inhibition plus or minus chemotherapy. Second line treatment in patients who progress on first line treatment which included chemotherapy is typically docetaxel with or without ramucirumab. Sotorasib is an irreversible KRAS G12C inhibitor that is taken orally once daily in KRAS G12C NSCLC patients that has shown promising results in preclinical studies, phase I, and phase II trials. Sotorasib acts by binding to an inactive guanosine diphosphate (GDP) bound KRAS via a covalent bond to inhibit cell proliferation and promotes apoptosis.2 Here, we discuss the results of the new CodeBreaK 200 phase III trial in more details and put the data in context in the evolving field of KRAS G12C.
Discussion
Sotorasib gained conditional FDA approval in May of 2021 due to encouraging preclinical and clinical study results.3 In preclinical studies, sotorasib was able to inhibit cells in vitro as well as suppress tumor growth in murine models.4 It also improved anti-tumor effects of chemotherapy and was shown by radioactive tracer to infiltrate multiple organs in rats including liver, kidney, thyroid, pancreas, and the adrenal glands.3 Mice treated with sotorasib did not grow tumors when re-challenged with KRAS G12C cells, indicating that adaptive immunity was present.4 The addition of an anti-checkpoint inhibitor also led to sustained tumor regression.5
CodeBreaK 100 was a phase I trial that evaluated the use of sotorasib in 59 NSCLC patients (18 years or older with locally advanced or metastatic disease), 42 colorectal cancer patients, and 28 patients with other cancer types. Patients received doses of 180mg, 360mg, 720mg, and 960mg of sotorasib. In the NSCLC cohort, 32% (19 of 59) of patients had confirmed responses and 56% of patients had stable disease.5 The median duration of response (DOR) was 10.9 months with a median progression free survival (PFS) of 6.3 months5 (Table 1). The side effect profile was tolerable with most subjects experiencing grade one or two adverse events, most commonly diarrhea and nausea. 11.6% of patients experienced grade three or four treatment related adverse events and there were no treatment related deaths.5
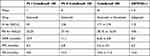 |
Table 1 CodeBreaK Studies and the KRYSTAL-1 Study |
In the phase II CodeBreaK 100 trial, 126 subjects with locally advanced or metastatic KRAS G12C NSCLC who had disease progression after platinum chemotherapy or checkpoint inhibition were treated with 960mg of sotorasib daily.6 The median PFS was 6.8 months with an overall response of 37.1% and disease control rate (DCR) achieved in 80.6% of patients6 (Table 1). The median DOR was 11.1 months and response was seen across all PD-L1 expression levels.6 Common adverse events included diarrhea, nausea, fatigue, arthralgia, and transaminitis.6
In the recently resulted CodeBreaK 200 phase III trial, patients with locally advanced, unresectable, or metastatic KRAS G12C NSCLC who underwent prior treatment with platinum chemotherapy and checkpoint inhibitor were randomized to receive 960mg of sotorasib or 75mg/m2 of IV docetaxel.7 Patients who had active brain metastases and ECOG performance status scores of >1 were excluded. Patients were stratified based on prior lines of therapy, race (Asian versus non-Asian), and history of CNS involvement. The protocol was revised to reduce the number of patients to 330, allowing crossover from docetaxel to sotorasib. Sotorasib demonstrated a higher median PFS of 5.6 months compared to docetaxel of 4.5 months (HR = 0.66 [95% CI: 0.51, 0.86]) across all subgroups.7 Sotorasib also boasted a higher ORR (28.1%) and DCR (82.5%) compared to that of docetaxel (13.2% and 60.3% respectively) (95% CI: 8.6–19.2%).7 Furthermore, patients treated with sotorasib had a quicker time to respond (1.4 months versus 2.8 months of docetaxel) and longer duration of response (8.36 months versus 6.8 months of docetaxel).7 The overall survival in the sotorasib group was 10.6 compared to 11.3 months in the docetaxel group7 (Table 1). Overall survival was not statistically different between the two arms although it is important to note that the study was not powered for OS. Sotorasib had less grade three or higher events (33.1%) compared to docetaxel (40.4%).7 Common adverse events in patients who received sotorasib were diarrhea, transaminitis, and nausea. Common adverse events for patients who received docetaxel were fatigue, nausea, diarrhea, and anemia. Time to deterioration (cough, dyspnea, physical functioning, and global health status) was longer in patients who received sotorasib compared to patients who received docetaxel.7
Despite an increase in PFS, ORR, and DCR in the sotorasib group, it unfortunately performed below expected results. In phase I and II trials, patients who received sotorasib had a PFS of 6.3 and 6.8 months, respectively.5,6 However, in the phase III trial, the median PFS in the sotorasib group was approximately one month less at 5.6 months.7 Phase I and II trials also showed similar DOR at 10.9 and 11.1 months, respectively.5,6 The phase III trial DOR in the sotorasib group was again lower at 8.36 months.7 The overall survival between the two groups were not significantly different, which may have been due to the 34% crossover. Although there could be differences in the baseline characteristics of those enrolled, sotorasib still underperformed compared to previous trials. In some instances, results from earlier phase studies may end up being superior compared to later phase studies, as there may be a bias in patient selection. Those with better tumor biology (who have progressed on multiple lines of therapy yet with a good performance status) typically qualify for early phase studies, “weeding out” rapid progressors with poor prognoses as they may not be candidates for early phase trials with demanding pharmacokinetics.
Although there were some efficacy shown in CodeBreaK 200, with a PFS difference between sotorasib and docetaxel being just one month, it is reasonable to question the value. Based on Leighl who has compared the differences in cost between the two therapies, sotorasib costs over $17,000 USD per month while docetaxel costs $1700 UDS per month.8 This financial gap for one month of small improvement in PFS allows for many other competitors to join the field, such as adagrasib, which had an ORR of 43% and PFS of 6.5 months in the phase II KRYSTAL-1 trial9 (Table 1). Indeed, adagrasib, just recently gained FDA accelerated approval in NSCLC patients in December 2022.
Additionally, many patients with KRAS G12C NSCLC have co-mutations which alter the tumor microenvironment via upregulation and downregulation of immunologic cell types. In a phase II trial, patients with co-mutations in KEAP1 plus or minus STK11 genotype had lower susceptibility to sotorasib.6 14% of patients with the KEAP1 co-mutation responded and 23% of patients with STK11 and KEAP1 co-mutations responded to therapy.6 In this patient population, further evaluation of mechanisms of resistance and ways to overcome these mechanisms should be studied. Other mechanisms of resistance to sotorasib includes resistance at upstream sites (EGFR, HER2, FGFR), downstream (MAPK/MEK pathway) sites, via bypass mechanisms (MET amplification), and fusion mutations (ALK, RET, BRAF, RAF1, FGFR3).10 They can occur within the binding pocket, additional mutations within KRAS, or even histologic transformation of cancer cells from adenocarcinoma to squamous cell carcinoma. Current methods to counter these resistance mechanisms include combination therapies of sotorasib with checkpoint inhibition therapy, MEK inhibitors, and/or other TKIs although we must be mindful of potential added toxicities with the combination. Severe immune related hepatitis in a patient who received sotorasib following immunotherapy has been reported.11 Afatinib is a pan-ErbB TKI that has been shown to enhance efficacy of tumor suppression with sotorasib as KRAS G12C mutation can lead to EGFR or HER activation.12 Trametinib is a MEK inhibitor that, when combined with sotorasib, led to further decrease in size of tumor volumes in a pre-clinical study.13
Furthermore, there is limited data in sotorasib’s CNS penetration as clinical trials excluded patients with active central nervous system metastases. Since sotorasib has been made commercially available, it would be important to accumulate real-world data in this setting. In addition, sotorasib is only approved in NSCLC but other tumors can have G12C including colorectal cancer (2.5%) and biliary cancer (2.3%).14 In the hase I CodeBreaK 100 Trial, other tumor types outside of NSCLC did not show as much of a response to sotorasib as NSCLC. Patients with pancreatic, endometrial, appendiceal, and melanoma with KRAS G12C mutations were included in the study. The median DOR was 5.4 months in these other tumor types with only 7.1% of the colorectal patients demonstrating confirmed response.5 Similarly, the phase II study of sotorasib demonstrated an objective response rate of only 9.7% in patients with previously treated G12C positive colorectal cancer.15
Thus, there is still a long road ahead with studying and optimizing the clinical use of sotorasib. With novel agents and combinations, the field of KRAS G12C is quickly evolving. While sotorasib was an exciting start, there is more to do to break the KRAS G12C Enigma code.
Conclusion
Results from preclinical data and clinical studies have undoubtedly allowed sotorasib to be a top competitor for KRAS G12C NSCLC patients who progress after first line therapy. Unfortunately, the phase III trial results produced lower PFS and ORR values than the CodeBreaK 100 phase I and II trials. In addition, overall survival between the two groups did not differ significantly. Has sotorasib broken the Enigma code? No, or at least not yet, although it was an exciting start in the field of G12C inhibitors. The field of KRAS is rapidly evolving and there is more to be unveiled. Given the financial cost of sotorasib, limited data on CNS penetration, multiple resistance mechanisms that have formed, and the modestly positive results from the phase III trial, multiple other KRAS G12C competitors continue to be studied for use in KRAS G12C NSCLC as well as other tumor types.
Disclosure
Dr Misako Nagasaka reports personal fees from AstraZeneca, Daiichi Sankyo, Novartis, EMD Serono, Pfizer, Lilly, Genentech, Mirati, Caris Life Sciences, Takeda, Janssen, and Blueprint Medicine; personal fees, non-financial support from AnHeart Therapeutics, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Riely GJ, Kris MG, Rosenbaum D, et al. Frequency and distinctive spectrum of KRAS mutations in never smokers with lung adenocarcinoma. Clin Cancer Res. 2008;14(18):5731–5734. doi:10.1158/1078-0432.CCR-08-0646
2. Lanman BA, Allen JR, Allen GJ, et al. Discovery of a Covalent Inhibitor of KRASG12C (AMG 510) for the Treatment of Solid Tumors. J Med Chem. 2020;63:52–65. doi:10.1021/acs.jmedchem.9b01180
3. Center for drug evaluation and research application number 214665Orig1s000. Drug Approval Package: Lumakras; 2020. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2021/214665Orig1s000TOC.cfm.
4. Canon J, Rex K, Saiki AY, et al. The clinical KRAS(G12C) inhibitor AMG 510 drives anti-tumor immunity. Nature. 2019;575:217–223. doi:10.1038/s41586-019-1694-1
5. Hong DS, Fakih MG, Strickler JH, et al. KRASG12C inhibition with sotorasib in advanced solid tumors. NEJM. 2020;383(13):1207–1217. doi:10.1056/NEJMoa1917239
6. Skoulidis F, Li BT, Dy GK, et al. Sotorasib for lung cancers with KRAS p.G12C mutation. NEJM. 2021;384(25):2371–2381. doi:10.1056/NEJMoa2103695
7. Johnson ML, Johannes de Langen A, Waterhouse D, et al. Sotorasib versus Docetaxel For Previously Treated Non-Small Cell Lung Cancer with KRAS G12C mutation: CodeBreak 200 Phase 3 Study. ESMO Congress. 2022;401(10378):733–746.
8. Leighl N. Beyond chemotherapy – every step counts. ESMO congress; 2022.
9. Sabari JK, Park H, Tolcher AW, et al. KRYSTAL-1: a phase I/II trial of adagrasib (MRTX849) in combination with TNO155 in patients with advanced solid tumors with KRAS G12C mutation. J Clin Oncol. 2021;39:TPS146–TPS146. doi:10.1200/JCO.2021.39.3_suppl.TPS146
10. Zhang SS, Nagasaka M. Spotlight on sotorasib (AMG 510) for KRASG12C positive non-small cell lung cancer. Lung Cancer. 2021;12:115–122. doi:10.2147/LCTT.S334623
11. Begum P, Goldin RD, Possamai LA, Popat S. Severe immune checkpoint inhibitor hepatitis in KRAS G12C-mutant NSCLC potentially triggered by sotorasib: case report. JTO Clin Case Rep. 2021;2(9):100213.
12. Gandara. AACR-NCI-EORTC conference; 2021.
13. Koga T, Suda K, Fujino T, et al. KRAS secondary mutations that confer acquired resistance to KRAS G12C inhibitors, sotorasib and adagrasib, and overcoming strategies: insights from in vitro experiments. J Thorac Oncol. 2021;16(8):1321–1332. doi:10.1016/j.jtho.2021.04.015
14. Loong HH, Du N, Cheng C. KRAS G12C mutations in Asia: a landscape analysis of 11.951 Chinese tumor samples. Transl Lung Cancer Res. 2020;9:5. doi:10.21037/tlcr-20-455
15. Fakih MG, Kopetz S, Kuboki Y, et al. Sotorasib for previously treated colorectal cancers with KRASG12C mutation (CodeBreaK100): a prespecified analysis of a single-arm, Phase 2 trial. Lancet Oncol. 2022;23(1):115–124. doi:10.1016/S1470-2045(21)00605-7
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
