Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 17
Association Between rs2278426 Polymorphism of the ANGPTL8 Gene and Polycystic Ovary Syndrome
Authors Wu H, Wang H, Sun L, Liu M, Wang H, Sun X, Zhang W
Received 17 January 2024
Accepted for publication 8 April 2024
Published 16 April 2024 Volume 2024:17 Pages 1749—1760
DOI https://doi.org/10.2147/DMSO.S455274
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Antonio Brunetti
Han Wu,1,* Hui Wang,2,* Lixia Sun,3,* Mengchen Liu,1 Haoran Wang,1 Xianchang Sun,4 Wenjuan Zhang1
1Center for Reproductive Medicine, The Second Affiliated Hospital of Shandong First Medical University, Taian, 271000, People’s Republic of China; 2Gynecological Minimally Invasive Surgery Center, The Affiliated Taian City Central Hospital of Qingdao University, Taian, 271000, People’s Republic of China; 3Department of Hematology, The Affiliated Taian City Central Hospital of Qingdao University, Taian, 271000, People’s Republic of China; 4Department of Physiology, Shandong First Medical University & Shandong Academy of Medical Sciences, Jinan, 250117, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Wenjuan Zhang, Center for Reproductive Medicine, The Second Affiliated Hospital of Shandong First Medical University, 366 Taishan Street, Taian, 271000, People’s Republic of China, Email [email protected] Xianchang Sun, Department of Physiology, Shandong First Medical University & Shandong Academy of Medical Sciences, 6699 Qingdao Road, Jinan, 250117, People’s Republic of China, Email [email protected]
Purpose: To study the relationship between the single nucleotide polymorphism (SNP) rs2278426 in the angiopoietin-like protein 8 gene (ANGPTL8) and polycystic ovary syndrome (PCOS).
Patients and methods: A total of 122 patients with PCOS and 108 controls were recruited for comparison of glucose, lipid, insulin, sex hormone, and ANGPTL8 levels. Polymerase chain reaction (PCR) and gene sequencing were performed for comparison of the frequency of the CC, CT, and TT rs2278426 genotypes and the rs2278426 allele distributions between the PCOS and control groups and between the obese and non-obese subgroups of the PCOS and control groups.
Results: The frequency of the T allele was significantly higher in the PCOS group than that in the controls (P = 0.037). In the dominant genetic model, the proportion of the CT+TT genotype in the PCOS group was significantly higher than that in the controls (P = 0.047). Subgroup analysis demonstrated that the T allele proportion was significantly higher in obese PCOS group than obese control group (P = 0.027). PCOS with the CT+TT genotype had significantly higher body mass index (BMI; P = 0.001), triglyceride (TG; P = 0.005), homeostasis model assessment of insulin resistance (HOMA-IR; P = 0.035), testosterone (P = 0.041), and ANGPTL8 (P = 0.037) levels and significantly lower high-density lipoprotein (HDL) levels (P = 0.025) than PCOS with the CC genotype. Obese PCOS group with the CT+TT genotype had significantly higher TG (P = 0.015), luteinizing hormone (LH; P = 0.030), fasting insulin (FINS; P = 0.039), HOMA-IR (P = 0.018), and ANGPTL8 (P = 0.049) levels than obese PCOS group with the CC genotype.
Conclusion: Polymorphisms of rs2278426 may induce glycolipid metabolic disorders by affecting ANGPTL8 levels and functions in Han Chinese females with obesity from the Shandong region, increasing the risk of PCOS in this population.
Keywords: angiopoietin-like protein 8, insulin resistance, metabolic disorder, obesity, polycystic ovary syndrome, single nucleotide polymorphism
Introduction
Polycystic ovary syndrome (PCOS) is a reproductive endocrine disorder frequently affecting females of childbearing age that mainly manifests as menstrual disorder, hirsutism, obesity, and infertility. Possibly affecting females their entire lives, PCOS has become a significant global public health concern related to reproduction, diabetes, cardio-cerebrovascular events, reproductive system malignancy, and mental health.1–3. Despite extensive research, the exact etiology and pathogenesis of PCOS remain unknown. With the recent development of gene detection technology, much focus has been placed on genetic factors. Several PCOS-related susceptibility genes and single-nucleotide polymorphisms (SNPs) have been identified that may be key targets for exploring the cause, prevention, diagnosis, and treatment of PCOS.4
Characterized by the coding product angiopoietin-like protein 8 (ANGPTL8), also referred to as betatrophin, the ANGPTL8 gene contains 183 amino acid residues mainly secreted in the liver and lipids. Located in the 14th intron at the dedicator of cytokinesis 6 (DOCK6). ANGPTL8 corresponds to the open reading frame 80 of chromosome 19 (C19orf80). ANGPTL8 can affect glycolipid metabolism and energy metabolism by stimulating β-cell proliferation and regulating the activity of lipoprotein lipase (LPL) or the triglyceride lipase,5 and its aberrant expression has been shown to correlate with a variety of metabolic diseases.6,7 Upregulated serum ANGPTL8 levels have been observed in patients with PCOS and might be associated with insulin resistance (IR) and high androgen levels. Although these phenomena are often involved in the pathological and physiological processes of PCOS,8–11 little research has been conducted on the gene level.
Among the few studies conducted to date, two genome-wide association studies (GWASs) showed that ANGPTL8 contains three single nucleotide polymorphism (SNP) mutant loci related to lipid metabolism: rs2278426 (C>T), rs737337 (T>C), and rs145464906 (C>T).12,13 The mutant of rs145464906 (C>T), a low-frequency synonymous mutation (minor allele frequency [MAF] 0.01% to 0.1%) located at locus 361 of the gene coding region of ANGPTL8, has not been extensively studied due to the difficulty in its detection. Rs737337 (T>C) is a synonymous mutation located 2.8 kb upstream the transcription initiation locus of ANGPTL8 whose effects on metabolic diseases have been largely disputed. To date, rs2278426 (C>T), which is located in the second exon of ANGPTL8 gene, has been the most studied locus. GWASs have shown that rs2278426 is an important mutant locus related to glycolipid metabolism in the Taiwanese population.14 The polymorphism of this locus induces the abnormal structure and instability of ANGPTL8 protein, increasing the risk of metabolic diseases such as diabetes and obesity.15–17
Given that glycolipid disorder is a key determinant of PCOS, we speculate that rs2278426 polymorphism may be closely associated with PCOS. However, to date no studies have investigated the relationship between rs2278426 polymorphism and PCOS. To fill this research gap, we conducted a case-control study to examine the effects of rs2278426 polymorphism on the phenotypes of PCOS in a population of Han Chinese females of childbearing age.
Materials and Methods
Subjects
Between January 2020 and January 2022, 122 outpatients with PCOS and 108 healthy controls were recruited from the Department of Reproduction Medicine at the Second Affiliated Hospital of Shandong First Medical University. Both patient groups were subdivided by body mass index (BMI) into an obese/overweight (BMI ≥ 24 kg/m2) and a non-obese (BMI < 24 kg/m2) subgroup. Patients were diagnosed with PCOS using the Rotterdam Criteria formulated by the American Society for Reproductive Medicine and European Society of Human Reproduction and Embryology in 2003.18 Females treated for infertility during the same period who had regular menstrual cycles (<25 menstrual cycles in <35 days) were recruited as participants in the control group. All the controls had normal cyclic androgen levels and normal ovary shapes on ultrasonic examination. None of the patients had acute or chronic diseases, including thyroid dysfunction, cardiovascular diseases, autoimmune diseases, tumors, liver or renal dysfunction, mental abnormalities, or mental diseases. To maximally reduce interference from confounders, patients who had unhealthy habits that could interfere with reproductive function (eg, cigarette smoking or excessive alcohol consumption) or used contraceptives, hormones, glucocorticoids, ovulation-stimulating drugs, decompressive drugs, lipid-lowering drugs, antidiabetic drugs, or weight-loss drugs were excluded.
This study complied with the Declaration of Helsinki and was approved by the Ethics Committee of Shandong First Medical University (Ethics approval number 202,004,014). All participants were informed about the purpose of the study and signed an informed consent.
Methods
Measurement of Basic Indices
Clinical baseline data, including height, weight, and waist and hip circumference, were measured and BMI and waist-to-hip ratio calculated for all participants.
Detection of Clinical Biochemical Immune Indices and Serum ANGPTL8 Concentration
For all subjects, elbow venous blood was collected after fasting on the second to fifth day of the menstrual cycle. Follicle-stimulating hormone (FSH), luteinizing hormone (LH), progesterone (P), prolactin (PRL), estradiol (E2), testosterone, and fasting insulin (FINS) levels were measured using a chemiluminescence (Siemens Healthcare Diagnostics, Erlangen, Germany). Fasting blood glucose (FBG), triglyceride (TG), cholesterol (TC), high-density lipoprotein (HDL), and low-density lipoprotein (LDL) levels were detected using a full-auto biochemical analyzer. Serum ANGPTL8 concentrations were monitored using an enzyme-linked immunosorbent assay (ELISA) analyzer (EIAab Science Co., Ltd., Wuhan, China), and 4-mL blood samples preserved in ethylene diamine tetraacetic acid (EDTA) were stored at −80°C. IR was evaluated using homeostasis model assessment of IR (HOMA-IR), according to which HOMA – IR= (FINS × FBG)/22.5.
Detection of ANGPTL8 Gene Polymorphism
Genomic DNA from peripheral blood cells was extracted using an Ezup columnar blood genomic DNA extraction kit (B518253; Sangon Biotech Co., Ltd., Shanghai, China). The target gene was obtained from polymerase chain reaction (PCR) amplification in which the forward primer was 5ʹ-CAGGAGTTCTATTGTGCGGC-3ʹ, and the reverse primer was 5ʹ-CCTGATGCAACTAT CGCACC-3ʹ.15 The PCR conditions were pre-denaturation at 95°C for 5 minutes, denaturation at 94°C for 30 seconds, annealing at 60°C for 30 seconds, and extension at 72°C for 50 seconds for 35 cycles followed by extension at 72°C for 8 minutes. The length of the amplified fragment was 387 bp, and the amplified PCR product was detected via 2% agarose gel electrophoresis. After the product was purified using a BigDye Terminator v3.1 (ABI Scientific, Sterling, VA, USA), two-way sequencing was performed with a 3730XL sequencing analyzer (ABI Scientific). Genotypes were identified by an experienced technician, and all samples were double genotyped with 100% concordance.
Statistical Analysis
Statistical analysis was performed using SPSS version 20.0 (IMB, Armonk, NY, USA). Quantitative data were tested using the Student’s t-test and expressed as the mean ± standard deviation (SD). Categorical data were tested using the χ2 test and expressed as the frequency and percentage. The Hardy–Weinberg genetic equilibrium was analyzed using the goodness-of-fit χ2 test. Distributions of genotype and allele frequency were estimated using direct counting. The differences among the three genotypes and allelic frequencies between the groups were compared using the χ2 test. The risk (odds ratio [OR]) of PCOS associated with genotype was calculated using logistic regression. The significance level for all statistical analyses was α = 0.05.
Results
Comparison of Clinical Indices Between PCOS and Control Groups
The BMI, FINS, HOMA-IR, TC, LDL, LH, LH/FSH, Testosterone, and ANGPTL8 levels of the PCOS group were all significantly higher than those of the control group (P < 0.05), whereas the HDL level was significantly lower (P = 0.001). There were no significant differences in other clinical indices between the two groups (Table 1).
 |
Table 1 Comparison of Clinical Indices Between PCOS and Control Groups |
Subgroup Comparison of Clinical Indices Between PCOS and Control Groups
Obesity has been identified as an independent risk factor for PCOS. To clarify and validate the effects of obesity on the PCOS and control groups, each group was divided by BMI into an obese and a non-obese subgroup for re-comparison of clinical indices. In the PCOS group, BMI (P < 0.001), WHR (P < 0.001), FBS (P = 0.001), FINS (P = 0.001), HOMA-IR (P < 0.001), TG (P < 0.001), LDL (P < 0.001), and ANGPTL8 (P < 0.001) levels were all significantly higher in the obese subgroup than the non-obese subgroup. In contrast, HDL (P < 0.001), LH (P < 0.001), and LH/FSH (P = 0.024) levels were significantly lower in the obese subgroup. In the control group, however, only BMI (P < 0.001), WHR (P < 0.001), and TG (P = 0.003) levels were significantly higher in the obese subgroup than the non-obese subgroup (Table 2).
 |
Table 2 Subgroup Comparison of Clinical Indices Between PCOS and Control Groups |
Distributions of SNPrs2278426 Genotypes and Alleles in PCOS and Control Groups
Testing of ANGPTL8 gene polymorphism in all participants revealed rs2278426 has three genotypes—CC, CT, and TT. The genotype distributions of rs2278426 were in Hardy–Weinberg equilibrium in the PCOS and control groups (P > 0.05) and did not significantly differ between the two groups. Analysis with a recessive inheritance model showed neither CC + CT nor TT frequency significantly differed between the PCOS and control groups (P = 0.077) but indicated a strong association between risk of PCOS and TT (OR = 2.383, 95% confidence interval [CI] = 0.890–6.381). Analysis with a dominant inheritance model demonstrated that the proportion of CT+TT in the PCOS group was significantly higher than that in the control group (44.27% vs 33.33%, P = 0.047). Risk analysis showed the risk of PCOS due to CT+TT was 1.728 times that that due to CC (95% CI = 1.006–2.968). Allele frequency analysis showed the frequency of the T allele in the PCOS group was significantly higher than that in the control group (28.28% vs 18.52%, P = 0.037) and the rs2278426 polymorphism increased the risk of PCOS (OR = 1.586, 95% CI =1.027–2.451). Details of the findings are listed in Table 3.
 |
Table 3 Distributions of SNPrs2278426 Genotypes and Alleles in PCOS and Control Groups |
Comparison of rs2278426 Genotypes and Allele Frequency in Obese and Non-Obese Subgroups
In the non-obese subgroups, the frequency of neither the three rs2278426 genotypes nor the alleles significantly differed between the PCOS and control groups (P = 0.42 and P = 0.219, respectively). Although the three rs2278426 genotypes did not significantly differ between the obese PCOS and obese control groups (P = 0.113), T allele frequency was significantly higher in the obese PCOS (34.43%) than obese control (21.30%) group. Relative risk analysis showed the risk of PCOS was higher in obese patients carrying the T allele than the C allele (OR = 1.940, 95% CI = 1.072–3.511; Table 4).
 |
Table 4 Comparison of rs2278426 Genotypes and Allele Frequency in Obese and Non-Obese Subgroups |
Comparison of Subgroup rs2278426 Genotype and Allele Frequency
Subgroup comparison of the difference in SNP distribution between the obese and non-obese PCOS subgroups revealed no significant differences regarding the three rs2278426 genotypes but a significantly higher T allele frequency in the obese PCOS (34.43%) than non-obese PCOS (22.13%) subgroup (Table 5).
 |
Table 5 Comparison of Subgroup rs2278426 Genotype and Allele Frequency |
Comparison of Clinical Indices in rs2278426 Genotypes in PCOS and Control Groups in Dominant Models
In the PCOS group, CT+TT carriers had significantly higher BMI (P = 0.01), TG (P = 0.05), Testosterone (P = 0.041), HOMA-IR (P = 0.035) and ANGPTL8 (P = 0.037) levels but significantly lower HDL levels (P = 0.025) than CC carriers. In the control group, CT+TT carriers had significantly lower HDL levels than CC carriers (P = 0.048), but none of the other clinical indices significantly differed between the groups (Table 6).
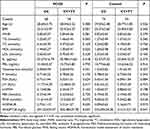 |
Table 6 Comparison of Clinical Indices in rs2278426 Genotypes in PCOS and Control Groups in Dominant Models |
Comparison of Clinical Indicators of rs2278426 Genotypes Among Different Subgroups
The results revealed that patients in the obese PCOS subgroup carrying CT+TT had significantly higher BMI (P = 0.019), TG (P = 0.015), LH (P = 0.030), FINS (P = 0.039), HOMA-IR (P = 0.018), and ANGPTL8 (P = 0.049) levels than those carrying CC. In contrast, patients in the non-obese PCOS subgroup carrying CT+TT had significantly lower HDL levels than those carrying CC (P = 0.020) but did not significantly differ in any of the other clinical indices (Table 7). None of the clinical indices significantly differed among the carriers of different genotypes in the obese and non-obese control subgroups (Table 8).
 |
Table 7 Comparison of Clinical Indicators in rs2278426 Genotypes Between PCOS Subgroups |
 |
Table 8 Comparison of Clinical Indicators in rs2278426 Genotypes Between Control Subgroups |
Discussion
PCOS is a complex, polygenic, inherited disease caused by multiple interacting factors, including genetic, environmental, and inflammatory factors. Although affecting females throughout the lifecycle, PCOS has particularly negative effects on the reproductive health of the 6% to 15% of females of childbearing age who experience this condition. PCOS can also induce metabolic dysfunction, increasing long-term health risks,19–21 and although it has been intensively and extensively studied, patients with PCOS still face challenges, such as delayed diagnosis and lack of precise therapy.
With the recent development of genomics and gene detection technology, SNP has been extensively applied in genetic research for investigation of many diseases, including PCOS. Because of its low cost, high efficiency, and rapid results, SNP has become a key method in screening diagnosis and therapeutic disease targeting. Many SNP mutant loci closely related to PCOS have been discovered, providing a critical basis for investigating the mechanism and factors underlying PCOS.22,23 Given the genetic heterogeneity and phenotypic complexity of PCOS, continued screening of PCOS-related SNP loci is scientifically valuable and clinically significant.
Discovered in 2013, ANGPTL8 is a major glycoprotein with a molecular weight of approximately 27.5 kDa secreted by fat cells and the liver that contains 183 residues. Basic research has shown that ANGPTL8 can drive pancreas β cells to secrete insulin to regulate sugar metabolism, thereby playing a critical role in glycolipid metabolism by inhibiting the activity of lipoprotein lipase to regulate lipid metabolism.24–26 Clinical research has demonstrated that serum ANGPTL8 abnormality is closely related to diabetes, fatty liver, obesity, and metabolic syndrome.7,27–29
Our preliminary research revealed that abnormal elevation in serum ANGPTL8 levels may be related to IR and PCOS.8 Although our findings indicate that ANGPTL8 functional abnormality may be involved in the occurrence and development of metabolic diseases, including PCOS, the mechanisms underlying it remain unknown. In this study, we observed significantly higher serum ANGPTL8 levels in patients with PCOS versus the controls and in obese patients with PCOS versus non-obese patients. We also observed that changes in TC, LDL, HOMA-IR, and testosterone levels were similar to those in ANGPTL8 levels. Our findings accord with a previous study that reported a positive correlation between ANGPTL8 and TG, LDL, and IR levels and a negative correlation between ANGPTL8 and HDL levels.30 These findings provide evidence that glycolipid metabolic abnormality, IR, and hyperandrogenism are key factors stimulating ANGPTL8 secretion and that ANGPTL8 upregulation further aggravates glycolipid metabolic disorders and IR.
Increasing research indicates that serum ANGPTL8 level may be a biomarker of PCOS and that ANGPTL8 gene polymorphism is a key factor affecting ANGPTL8 protein expression and action.31,32 Currently, rs2278426 (C>T) is the most widely studied polymorphic site in the ANGPTL8 gene. Abu-Farha et al27 observed that ANGPTL8 rs2278426 polymorphism did not significantly affect ANGPTL8 concentrations in diabetes. However, a Dallas Heart Study reported that rs2278426 polymorphism was closely related to the cyclic ANGPTL8 level and that CT+TT genotype carriers had significantly higher cyclic ANGPTL8 level than CC genotype carriers.33
We observed significantly higher ANGPTL8 levels in patients with PCOS carrying the CT+TT genotype than in patients with PCOS carrying the CC genotype. In subgroup analysis, we also observed significantly higher ANGPTL8 levels in obese patients with PCOS carrying the CT+TT genotype than in non-obese patients with PCOS carrying the CC genotype. The significantly high ANGPTL8 levels in patients with PCOS may be closely related to the blood lipid abnormality and IR caused by high BMI and glycolipid metabolic disorders.34 We could not identify the exact effect of rs2278426 polymorphism on ANGPTL8 levels, but our results indicate that rs2278426 polymorphism may be a risk factor for PCOS in individuals with obesity.
Among individuals with type II diabetes, the frequency of the rs2278426 T allele is 17.8% in Han Chinese from Guangxi, 19.5% in Han Chinese from Jiangsu, 23.04% in Melao Chinese from Guangxi, 25.75% in Japanese populations, and 5% in European American populations.15,35 In our study, the frequency of the rs2278426 T allele was 18.52% in the control group. ANGPTL8 gene polymorphism among regions, populations, and races may be due to different ancestral environments or genetic selection pressures. Previous studies have shown that rs2278426 polymorphism increases risk of type II diabetes and cardiovascular diseases in Japanese, Egyptian, and Han Chinese populations.15,16,36 However, no studies before our study examined the relationship between rs2278426 polymorphism and PCOS.
Our results showed that despite the absence of significant differences between the PCOS and control groups regarding the three genotypes, the proportion of CT+TT genotypes in the PCOS group was significantly higher than that in the control group. As both the CT and TT genotypes contain the T allele, its frequency was higher in the PCOS group than the control group, suggesting that the T allele increases the risk of PCOS. Similar results have been obtained in other studies. However, the reason for the difference in alleles but not genotypes between the PCOS and control groups may be related to the sample size; if the number of participants were increased, the results may reach or lose statistical significance. Further subgroup analysis showed the frequency of the T allele was significantly higher in obese patients with PCOS than in either non-obese patients with PCOS or obese controls, which indicates that obese T allele carriers are at higher risk of PCOS. However, it is unknown whether polymorphism of this locus increases the risk of PCOS in individuals from other regions or races. It is thus necessary to validate our findings by examining whether rs2278426 polymorphism is associated with PCOS incidence in individuals of other ethnic groups and from other regions.
The Dallas Heart Study found significantly decreased HDL and LDL levels in African Americans and Hispanic Americans but not in European Americans carrying the rs2278426 T allele.33 Guo et al37 found that rs2278426 polymorphism in healthy Han Chinese of the Guangxi region was related to LDL downregulation. However, Ding et al35 reported that rs2278426 polymorphism in Han Chinese of the Jiangsu region was not significantly associated with lipid phenotype abnormality. We found significantly decreased HDL levels in Han Chinese carriers of the rs2278426 the T allele, which is consistent with a study of an Arab population.38 Moreover, in the PCOS group, we observed that the BMI and TG levels in CT+TT genotype carriers were significantly higher than those in CC genotype carriers.
Further subgroup analysis revealed significantly higher TG levels in obese patients with PCOS carrying the CT+TT genotype than in obese patients with PCOS carrying the CC genotype. This finding indicates that the increased risk of PCOS associated with CT+TT may be related to lipid metabolic disorder due to SNPrs2278426 polymorphism. Different studies have obtained differing results regarding the effect of rs2278426 polymorphism on lipid metabolism phenotypes, which may be attributed to differences in sample sizes, populations, and/or regions. Moreover, the linkage disequilibrium (LD) between rs2278426 and other pathogenic polymorphisms is another key cause for lipid metabolic abnormality and the difference in lipid phenotypes among populations.38,39
To explore the gene-level mechanism underlying ANGPTL8 regulation of sugar metabolism, we examined the effect of ANGPTL8 rs2278426 polymorphism on sugar metabolism. We found that HOMA-IR levels in patients with PCOS carrying the CT+TT genotype were significantly higher than those in patients with PCOS carrying the CC genotype. However, we found no significant differences among carriers of different rs2278426 genotypes in the control group. Subgroup analysis showed that the obese patients with PCOS carrying the CT+TT genotype had significantly higher HOMA-IR and FINS levels than those carrying the CC genotype.
Some of our results are consistent with those of Oldoni et al40 and Abu-Farha et al,41 both of whom reported that carriers of the rs2278426 TT/CT genotype have significantly higher serum insulin and HOMA-IR levels than carriers of the CC genotype. Studies of risk analysis have demonstrated that rs2278426 polymorphism increases risk of diabetes. Among them, Liu et al15 found that a large proportion of the Japanese population carrying the rs2278426 C/T and T/T genotypes experiences type II diabetes and glucose intolerance.
Based on our findings and recent research advances, we speculate that Han Chinese females from the Shandong region carrying the CT+TT genotype, especially those with obesity, have increased risk of PCOS associated with IR or sugar metabolism disorder caused by rs2278426 polymorphism. However, the mechanism of rs2278426 polymorphism involved in sugar metabolism is not fully clear. In addition to the structural and functional changes in ANGPTL8 protein caused by rs2278426 polymorphism, another cause may be the LD between rs2278426 and other mutant loci. Admittedly, given the polygenic heritance of PCOS and the large differences in SNPs among different populations and regions, more research into how the LD between rs2278426 and other pathogenic polymorphisms affects PCOS is needed.
To our knowledge, this is the first study of the association between rs2278426 and PCOS. By affecting ANGPTL8 levels and functions and thereby increasing the risk of PCOS, rs2278426 polymorphism may be involved in glycolipid metabolic disorders, particularly in females with obesity. Our findings indicate that this polymorphism might be a novel biomarker for screening females at high risk of PCOS. Nevertheless, our findings are limited by our examination of only two subgroups classified according to BMI in the subgroup analysis. Similarly, they are limited by the small sample of participants whom we examined, which may have affected the significance of the results. To overcome these limitations, we will examine larger samples of more detailed subgroups based on BMI to further clarify the association between rs2278426 and other SNPs of ANGPTL8 and PCOS in future studies.
Funding
This study was supported by the Natural Science Foundation of Shandong Province (ZR2016HL04); the Development of Science and Technology Plan of Shandong Province Medicine and Health Care (2015WS0100); Science and Technology Innovation Development Project of Taian City (2020NS266).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Shetty C, Rizvi S, Sharaf J, et al. Risk of gynecological cancers in women with polycystic ovary syndrome and the pathophysiology of association. Cureus. 2023;15(4):e37266. doi:10.7759/cureus.37266
2. Joham AE, Norman RJ, Stener-Victorin E, et al. Polycystic ovary syndrome. Lancet Diabetes Endocrinol. 2022;10(9):668–680. doi:10.1016/S2213-8587(22)00163-2
3. Wekker V, van Dammen L, Koning A, et al. Long-term cardiometabolic disease risk in females with PCOS: a systematic review and meta-analysis. Hum Reprod Update. 2020;26(6):942–960.
4. Ajmal N, Khan SZ, Shaikh R. Polycystic ovary syndrome (PCOS) and genetic predisposition: a review article. Eur J Obstet Gynecol Reprod Biol X. 2019;3:100060. doi:10.1016/j.eurox.2019.100060
5. Sylvers-Davie KL, Davies BSJ. Regulation of lipoprotein metabolism by ANGPTL3, ANGPTL4, and ANGPTL8. Am J Physiol Endocrinol Metab. 2021;321(4):E493–E508. doi:10.1152/ajpendo.00195.2021
6. Rong Guo X, Li Wang X, Chen Y, et al. ANGPTL8/betatrophin alleviates insulin resistance via the Akt-GSK3β or Akt-FoxO1 pathway in HepG2 cells. Exp Cell Res. 2016;345(2):158–167. doi:10.1016/j.yexcr.2015.09.012
7. Navaeian M, Asadian S, Ahmadpour Yazdi H, et al. ANGPTL8 roles in proliferation, metabolic diseases, hypothyroidism, polycystic ovary syndrome, and signaling pathways. Mol Biol Rep. 2021;48(4):3719–3731. doi:10.1007/s11033-021-06270-8
8. Wenjing Z, Chenxu L, Jun G, Yunmin D, Xianchang S, Wenjuan Z. Clinical study on the relationship between betatrophin and polycystic ovary syndrome. Chin J Reprod Contracep. 2018;38(4):288–293.
9. Calan M, Yilmaz O, Kume T, et al. Elevated circulating levels of betatrophin are associated with polycystic ovary syndrome[J]. Endocrine. 2016;53(1):271–279. doi:10.1007/s12020-016-0875-z
10. Pu D, Li L, Yin J, et al. Circulating ANGPTL8 is associated with the presence of metabolic syndrome and insulin resistance in polycystic ovary syndrome young women. Mediators Inflamm. 2019;2019:6321427. doi:10.1155/2019/6321427
11. Varikasuvu SR, Panga JR, Satyanarayana MV. Circulating angiopoietin-like 8 protein (ANGPTL8/Betatrophin) in patients with polycystic ovary syndrome: a systematic review and multi effect size meta-analysis. Gynecol Endocrinol. 2019;35(3):190–197. doi:10.1080/09513590.2018.1536736
12. Spracklen CN, Chen P, Y J K, et al. Association analyses of East Asian individuals and trans-ancestry analyses with European individuals reveal new loci associated with cholesterol and triglyceride levels. Hum Mol Genet. 2017;26(9):1770–1784. doi:10.1093/hmg/ddx062
13. M A C, Duan Q, Hoffmann TJ, et al. Genome-wide characterization of shared and distinct genetic components that influence blood lipid levels in ethnically diverse human populations. Am J Hum Genet. 2013;92(6):904–916. doi:10.1016/j.ajhg.2013.04.025
14. Ho CY, Lee JI, Huang SP, et al. A genome-wide association study of metabolic syndrome in the Taiwanese population. Nutrients. 2023;16(1):77. doi:10.3390/nu16010077
15. Liu J, Yagi K, Nohara A, et al. High frequency of type 2 diabetes and impaired glucose tolerance in Japanese subjects with the angiopoietin-like protein 8 R59W variant. J Clin Lipidol. 2018;12(2):331–337. doi:10.1016/j.jacl.2017.12.011
16. Hou G, Tang Y, Ren L, et al. The ANGPTL8 rs2278426 (C/T) polymorphism is associated with prediabetes and type 2 diabetes in a Han Chinese population in Hebei Province. Int J Endocrinol. 2020;2020:1621239. doi:10.1155/2020/1621239
17. Alenad A, Alenezi MM, Alokail H, et al. Association of ANGPTL8 (betatrophin) gene variants with components of metabolic syndrome in Arab adults. Sci Rep. 2020;10(1):6764. doi:10.1038/s41598-020-63850-7
18. Rotterdam ES. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum Reprod. 2004;19(1):41–47.
19. Hoeger KM, Dokras A, Piltonen T. Update on PCOS: consequences, challenges, and guiding treatment. J Clin Endocrinol Metab. 2021;106(3):e1071–e83. doi:10.1210/clinem/dgaa839
20. Li Y, Chen C, Ma Y, et al. Multi-system reproductive metabolic disorder: significance for the pathogenesis and therapy of polycystic ovary syndrome (PCOS). Life Sci. 2019;228:167–175. doi:10.1016/j.lfs.2019.04.046
21. Ding H, Zhang J, Zhang F, et al. Resistance to the insulin and elevated level of androgen: a major cause of polycystic ovary syndrome. Front Endocrinol. 2021;12:741764. doi:10.3389/fendo.2021.741764
22. Chen J, Guan L, Liu H, et al. GALNT2 gene variant rs4846914 is associated with insulin and insulin resistance depending on BMI in pcos patients: a case-control study. Reprod Sci. 2021;28(4):1122–1132. doi:10.1007/s43032-020-00380-7
23. Yang C, Xi M, Liu H, et al. Association of polymorphisms of glutamate cysteine ligase genes GCLC C-129 T and GCLM C-588 T with risk of polycystic ovary syndrome in Chinese women. Reprod Sci. 2022;29(6):1790–1800. doi:10.1007/s43032-021-00764-3
24. Luo M, Peng D. ANGPTL8: an important regulator in metabolic disorders. Front Endocrinol. 2018;9:169. doi:10.3389/fendo.2018.00169
25. Liu D, Qu H, Wang H, et al. Relationship between serum betatrophin levels and the first-phase of glucose-stimulated insulin secretion. Obes Res Clin Pract. 2018;12(Suppl 2):9–15. doi:10.1016/j.orcp.2016.08.004
26. Zhang Z, Wu H, Dai L, et al. ANGPTL8 enhances insulin sensitivity by directly activating insulin-mediated AKT phosphorylation. Gene. 2020;749:144707. doi:10.1016/j.gene.2020.144707
27. Abu-Farha M, Abubaker J, Tuomilehto J. ANGPTL8 (betatrophin) role in diabetes and metabolic diseases[J]. Diabetes Metab Res Rev. 2017;33(8). doi:10.1002/dmrr.2919
28. Bai Y, Du Q, Zhang L, et al. Silencing of ANGPTL8 alleviates insulin resistance in trophoblast cells. Front Endocrinol. 2021;12:635321. doi:10.3389/fendo.2021.635321
29. Ye J, Qin Y, Wang D, et al. The relationship between circulating ANGPTL8/betatrophin concentrations and adult obesity: a meta-analysis. Dis Markers. 2019;2019:5096860. doi:10.1155/2019/5096860
30. Keyif B, Goksever Celik H, Karamustafaoglu Balci B, et al. Serum betatrophin levels are significantly increased in obese patients compared to lean patients regardless to the presence of PCOS. Gynecol Endocrinol. 2020;36(8):678–681. doi:10.1080/09513590.2020.1725964
31. Luo P, Zhang C, He Y, et al. Several circulating biomarkers for PCOS diagnosis. Exp Clin Endocrinol Diabetes. 2021;129(10):705–712. doi:10.1055/a-1025-3711
32. Keikha F, Shahrokh Tehraninejad E, Rakhshkhorshid M, et al. The association of the betatrophin level with metabolic and inflammatory parameters in infertile females with polycystic ovary syndrome: a case-control study. Int J Reprod Biomed. 2022;20(1):29–36. doi:10.18502/ijrm.v20i1.10406
33. Quagliarini F, Wang Y, Kozlitina J, et al. Atypical angiopoietin-like protein that regulates ANGPTL3. Proc Natl Acad Sci U S A. 2012;109(48):19751–19756. doi:10.1073/pnas.1217552109
34. He Y, Hu W, Yang G, et al. Adipose insulin resistance and circulating betatrophin levels in women with PCOS. Biomed Res Int. 2020;
35. DING Y, Haoxiang LI, Mengjiao XU, et al. Association of betatrophin gene polymorphisms with type 2 diabetes mellitus[J]. J Jiang Univ. 2019;29(01):72–76.
36. El-Lebedy D. Interaction between endothelial nitric oxide synthase rs1799983, cholesteryl ester-transfer protein rs708272 and angiopoietin-like protein 8 rs2278426 gene variants highly elevates the risk of type 2 diabetes mellitus and cardiovascular disease. Cardiovasc Diabetol. 2018;17(1):97. doi:10.1186/s12933-018-0742-8
37. Guo T, Yin RX, Wu J, et al. Association of the angiopoietin-like protein 8 rs2278426 polymorphism and several environmental factors with serum lipid levels. Mol Med Rep. 2015;12(3):3285–3296. doi:10.3892/mmr.2015.3825
38. Ghasemi H, Karimi J, Khodadadi I, et al. Association between rs2278426 (C/T) and rs892066 (C/G) variants of ANGPTL8 (betatrophin) and susceptibility to type2 diabetes mellitus. J Clin Lab Anal. 2019;33(1):e22649. doi:10.1002/jcla.22649
39. Cannon ME, Duan Q, Wu Y, et al. Trans-ancestry fine mapping and molecular assays identify regulatory variants at the ANGPTL8 HDL-C GWAS locus. G3 (Bethesda). 2017;7(9):3217–3227. doi:10.1534/g3.117.300088
40. Oldoni F, Bass K, Kozlitina J, et al. Genetic and metabolic determinants of plasma levels of ANGPTL8. J Clin Endocrinol Metab. 2021;106(6):1649–1667. doi:10.1210/clinem/dgab120
41. Abu-Farha M, Melhem M, Abubaker J, et al. ANGPTL8/betatrophin R59W variant is associated with higher glucose level in non-diabetic Arabs living in Kuwaits. Lipids Health Dis. 2016;15:26. doi:10.1186/s12944-016-0195-6
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
