Back to Journals » Patient Preference and Adherence » Volume 18
Association Between Persistence with Oral Atypical Antipsychotic Medications and Hospital and Emergency Department Utilization in Medicaid Patients with Schizophrenia
Authors Richards K , Johnsrud M, Zacker C, Sasané R
Received 29 September 2023
Accepted for publication 11 January 2024
Published 18 January 2024 Volume 2024:18 Pages 177—185
DOI https://doi.org/10.2147/PPA.S439081
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Kristin Richards,1 Michael Johnsrud,1 Christopher Zacker,2 Rahul Sasané2
1TxCORE, College of Pharmacy, The University of Texas at Austin, Austin, TX, USA; 2Cerevel Therapeutics, LLC, Cambridge, MA, USA
Correspondence: Kristin Richards, TxCORE, College of Pharmacy, The University of Texas at Austin, 2409 University Avenue, Mail Stop A1930, Austin, TX, 78712, USA, Tel +1 512 471 5607, Email [email protected]
Purpose: To examine 1-year persistence with oral atypical antipsychotics (OAAPs) for Medicaid patients with schizophrenia and assess the association between OAAP persistence and hospital and emergency department (ED) resource utilization.
Patients and Methods: Using 2016– 2020 multi-state Medicaid claims data, this retrospective study followed patients diagnosed with schizophrenia for 12 months after initiating OAAP therapy. Patients started on an OAAP with no evidence of antipsychotic use in the previous 6 months were included if they had a diagnosis of schizophrenia, were not dually enrolled in Medicaid and Medicare, did not switch to a long-acting injectable antipsychotic, and were continuously eligible 6 months before and 12 months after the initial OAAP prescription (index date). OAAP persistence was measured allowing for a < 60-day gap. All-cause and schizophrenia-related inpatient and emergency department (ED) resource utilization during the follow-up period were compared between OAAP persistent and non-persistent groups.
Results: The study sample of 13,007 had an average age of 39.1 years and 57.0% were male. Patients were persistent with their index OAAP for 135 days on average and 73.1% had a ≥ 60-day gap in antipsychotic therapy post-index. While 32.8% and 28.6% of patients who did not persist with their index OAAP restarted the index OAAP or switched to a different OAAP medication later in the year, respectively, a larger proportion (38.6%) had no further OAAP prescriptions. After adjustment for demographic and clinical variables, compared to non-persistent patients, persisting with OAAPs was significantly associated with fewer all-cause and schizophrenia-related hospitalizations (Incidence Rate Ratio [IRR]=0.742, p< 0.001; IRR=0.823, p< 0.001; respectively) and ED visits (IRR=0.759, p< 0.001; IRR=0.773, p< 0.001; respectively).
Conclusion: Non-persistence with OAAP medication is common among patients with schizophrenia and associated with negative outcomes including increased utilization of hospital and ED resources. Patient-centered interventions that improve antipsychotic persistence should be implemented to facilitate optimal outcomes in this population.
Keywords: antipsychotic medication, persistence, healthcare resource utilization, Medicaid, schizophrenia
Introduction
In studies of medication utilization, adherence to and persistence with prescribed medications are important outcomes to measure, as they are well recognized as contributors to the effectiveness of a drug in the real world, compared to the efficacy demonstrated in clinical trials. Adherence is a measure of the percentage of prescribed medication that a patient has presumably consumed.1 Medication possession ratios (MPRs) or proportions of days covered (PDC) are calculated and patients are often categorized as “adherent” at or above an 80% threshold for many disease states.2 Persistence is a measure of how long a patient stays on medication, providing a “chronology of adherence”.1 It is usually reported as the number of therapy days until discontinuation or a gap in refills of a specific period of time (eg, 30 days, 60 days).
An abundance of published studies have evaluated adherence to antipsychotic (AP) medications in schizophrenia, including systemic reviews and meta-analyses.3–6 Most of these analyses demonstrate suboptimal adherence to APs, with a recent meta-analysis of studies conducted in Africa, Europe, and North America finding that 56% of patients with schizophrenia self-reported lack of adherence to AP medications.4 US studies, using Medicaid prescription claims data to assess adherence to oral and/or long-acting injectable (LAI) APs, report even higher non-adherence rates of 52–80%.6–9 AP non-adherence is associated with negative outcomes including higher rates of psychotic symptoms, schizophrenia relapse, high utilization of emergency department (ED) and hospital resources, and increased risk of early death.5,10–12
Studies of persistence with AP medication are equally important, but less frequently published compared to adherence studies. Recent persistence studies generally treat oral atypical APs (OAAPs) as a class and often compare persistence results to those of an LAI AP cohort. Medication discontinuation rates are usually higher among those taking OAAPs compared to LAI APs, and persistence with therapy favors LAI APs, though results are somewhat mixed.7,10,13,14
To lend further understanding to the medication-taking behaviors of people diagnosed with schizophrenia, we aimed to assess patients’ persistence with oral atypical APs (OAAPs) during the 1-year period after OAAP initiation using recent Medicaid administrative claims data. We selected these medications and this patient population because the majority of patients being treated with APs take an oral dosage form of a second-generation (atypical) product and 70% of non-institutionalized adults with schizophrenia are enrolled in state Medicaid programs.15 In addition, we aimed to assess a hypothesized association between OAAP persistence and utilization of hospital and ED resources in order to inform medical policy within Medicaid programs.
Materials and Methods
Study Design and Data Source
This retrospective cohort study used a blinded multi-state sample of de-identified Medicaid administrative healthcare claims data from January 1, 2016 to December 31, 2020. The patient sample has previously been described in detail.9 Medical and pharmacy claims were utilized, along with enrollment information for 344,751 patients with evidence of a schizophrenia diagnosis (International Classification of Disease, Tenth Revision (ICD-10): F20.xx). The first prescription for an OAAP medication between July 1, 2016 and December 31, 2019 served as the index date, and all patients were followed for 12 months. The 6-month period before the index date was the source for baseline study variables. All data fully complied with the 1996 US Health Insurance Portability and Accountability Act regulations. This study was deemed exempt by The University of Texas at Austin Institutional Review Board.
Inclusion Criteria
Inclusion in the study required the following: (1) evidence of a paid OAAP medication claim between 7/1/16 and 12/31/19; (2) no evidence of oral typical or OAAP medication utilization during the 6-month baseline period; (3) not dually eligible for Medicaid and Medicare pre- or post-index; (4) presence of a schizophrenia diagnosis associated with at least 1 inpatient or 2 outpatient claims during the pre- and/or post-index periods; (5) 18–63 years of age at index; (6) continuous Medicaid enrollment pre- and post-index; and (7) no evidence of pre- or post-index LAI AP utilization.
Study Variables
Baseline variables consisted of age at index, sex, race/ethnicity, and Quan-Charlson Comorbidity Index (CCI) score.16 Pre- and post-index periods were used to identify evidence of other severe mental illnesses and alcohol/substance abuse. The primary independent variable was persistence with OAAP medication during the 12-month post-index period. Persistence was determined by identifying the last consecutive day of OAAP medication possession during the post-index period, without a gap in therapy of 60 days or greater. This gap period has also been used in previous studies examining OAAP persistence in Medicaid beneficiaries with schizophrenia.13,14 Since we used a 60-day runout period to determine a gap in therapy, persistence was assessed through day 300 of the post-index period. Therefore, if the last day of persistence was between day 1 and day 300 (post-index), the patient was classified as non-persistent. Persistence was calculated for the index OAAP and for all OAAPs (treated as a class) dispensed during follow-up. From the cohort of patients who did not persist with their index OAAP, we identified those who later restarted their index OAAP or were prescribed a non-index OAAP after initial non-persistence.
Statistical Analyses
Study sample characteristics and outcomes were compared between patients who were and were not persistent with OAAP medications for one year after OAAP initiation. Wilcoxon-Mann–Whitney U and chi-square tests were used for bivariate analyses. Kaplan-Meier survival curves were generated to assess OAAP persistence. Multivariable analyses were conducted to evaluate the association of OAAP persistence with study outcomes, while controlling for baseline covariates. Logistic regression was used to assess hospitalization or ED visit outcomes and negative binomial regression was used to assess inpatient and ED visits, as well as for hospital length of stay. The level of significance was set a priori at p<0.05, with confidence intervals set at 95%. All analyses were performed using Stata Statistical Software, Release 17.
Results
A total of 13,007 patients met the criteria for inclusion in the study. The mean age was 39.1 years (sd=12.8; median=38) at index and 41.6% were between 18 and 34 years of age. Males comprised a larger proportion of the sample than females (57% vs 43%) and 36.1% were Black, 31.8% were White, and 9.7% were Hispanic. Approximately 40% of patients had claims evidence of bipolar disorder (39.2%) and schizoaffective disorder (40.1%), while 26.5% had evidence of major depressive disorder. Sixty percent had evidence of alcohol/substance abuse. The top four index OAAPs were quetiapine (25.6%), risperidone (24.8%), olanzapine (19.7%), and aripiprazole (13.7%). Overall sample characteristics are detailed in Table 1.
 |
Table 1 Sample Characteristics by Persistence Status |
OAAP Persistence
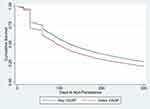
Nearly three in four patients (73.1%) were non-persistent with OAAP medication, with Figure 1 displaying a pronounced drop in persistence rates with both the index and any OAAP at 30 days, followed by a smaller decline at 60 days. Age, race/ethnicity, evidence of other severe mental illness, and index OAAP medication were significantly different (p<0.001) between the persistent and non-persistent groups. (Table 1) Unadjusted analysis results showed that persistent patients were slightly older (1.5 years; p<0.001) than their non-persistent counterparts and less likely to initiate aripiprazole as the index OAAP therapy (p<0.001). They were less likely to have evidence of bipolar disorder (p<0.001) and alcohol/substance abuse (p<0.001), but more likely to have schizoaffective disorder diagnoses (p=0.001). A greater percentage of Black patients (78.4%) did not persist with OAAP treatment compared to Hispanic and White patients (67.9% and 69.4%, respectively). Figure 2 shows persistence curves for Black, Hispanic, and White patients for the index and any OAAP medication.
Overall, patients were persistent with their index OAAP therapy for an average of 135.1 days (sd=107.2, median=95) and, when including non-index OAAPs, mean persistence increased to 155.4 days (sd=109.3, median=125). (Table 2) Among 73.1% of patients who were classified as non-persistent to OAAPs overall, the average days of persistence with the index and any OAAP medications were 89.6 (sd=72.3, median=63) and 102.0 (sd=76.0, median=82), respectively.
 |
Table 2 Patterns of Antipsychotic Medication Persistence |
For those patients meeting the criteria for non-persistence with their index OAAPs, 3370 patients (32.8% of 10,275 index OAAP non-persistent patients) restarted their index OAAP after an average of 130.3 days (sd=67.7, median=107). Nearly 29% (n=2937, 28.6%) were prescribed an alternative OAAP at a mean of 86.7 days (sd=94.0, median=53) after index OAAP non-persistence and 6.2% (n=635) were prescribed a first-generation antipsychotic. The remaining 32.4% (n=3333) had no evidence of typical or atypical AP utilization during the study period after discontinuing their index OAAP.
Hospital and Emergency Department Utilization
Table 3 presents overall all-cause and schizophrenia-related hospital and ED utilization, as well as results for persistent and non-persistent patients. Nearly 40% of all patients (39.8%) were hospitalized during the 1-year follow-up period with a mean of 0.97±2.04 visits per patient, and 23.3% of all patients had a schizophrenia-related hospitalization (0.54±2.56 per patient). All-cause and schizophrenia-related hospital days averaged 17.0±22.3 and 11.3±14.3, respectively. Nearly 70% of the sample had at least one ED visit, with a mean of 3.5±6.4 visits.
 |
Table 3 Unadjusted and Adjusted Comparisons of Hospital and Emergency Department Utilization by Persistence Status |
Unadjusted comparisons of hospital and ED utilization showed that patients who were persistent to OAAP therapy, compared to their non-persistent counterparts, had lower rates of hospitalizations (31.0% vs 43.0%; p<0.001) and ED visits (58.0% vs 72.2%; p<0.001). (Table 3) The persistent group also had lower mean numbers of all-cause and schizophrenia-related ED and hospital visits, and spent fewer days (all-cause) in the hospital (all p<0.001). The adjusted analyses demonstrated that being persistent with OAAPs was associated with 25.8% and 17.7% fewer all-cause (IRR: 0.742, 95% CI: 0.691–0.797) and schizophrenia-related (IRR: 0.823, 95% CI: 0.742–0.914) hospitalizations, respectively; 31.7% shorter all-cause (IRR: 0.683, 95% CI: 0.618–0.755) and 27.3% shorter schizophrenia-related (IRR: 0.727, 95% CI: 0.631–0.836) inpatient lengths of stay; and 24.1% and 22.7% fewer all-cause and schizophrenia-related ED visits (IRR: 0.759, 95% CI: 0.720–0.801; IRR: 0.773, 95% CI: 0.691–0.864, respectively).
Discussion
Poor persistence with oral AP therapy among people diagnosed with schizophrenia is a long-standing trend that has been documented in the literature. Studies using multi-state Medicaid claims data between 2004 and 2015 and allowing for a <60-day gap between medication refills have reported that approximately 30–50% of patients with schizophrenia persist with their index oral AP over a 12-month period.7,10,13,14 Our study, based on more recent data (2016–2020), found that only 21% of the sample persisted with the index medication, and 27% persisted when allowing for a switch to a different OAAP medication. We found that patients filled their index OAAP prescription consistently (without a >60-day gap) for an average of only 4.5 months (135 days) before discontinuation. Shah et al reported similar findings (135.6 days to oral AP discontinuation), though they used a more conservative gap (15 days) in their persistence definition.7 The pattern of suboptimal persistence with oral AP medications has not improved over time.
Kaplan-Meier curves provide a valuable visualization of medication discontinuation in this population. Figure 1 shows a precipitous drop in persistence rates at 30 days, with nearly 30% of the sample discontinuing their index OAAP during the first month of therapy. At 60 days, nearly 40% of the sample had discontinued the index medication and more than half discontinued within 100 days of initiation of the medication. Prior studies have produced similar patterns of use.7,14 Sharp drops in medication persistence so early in the course of therapy are concerning, and even more troublesome when comparing these patterns by patient race/ethnicity. Our study found that 32% of Black patients discontinued their index OAAP medication during the first month of treatment, compared to 25% and 27% of Hispanic and White patients, respectively. Though persistence was poor for all groups, the Kaplan-Meier curves (Figure 2) show a clear disparity in OAAP persistence for Black patients throughout the follow-up period. These findings point to potential inequity in access or tolerance issues being experienced by Black patients that impact persistence to OAAP therapy. Identifying direct causes for these differences was beyond the scope of our objectives; however, we suggest this as an opportunity to investigate potential predictors of non-persistence using more comprehensive data sources that include non-medical drivers of health information.
Medication re-initiating patterns after AP discontinuation are infrequently reported in the literature. On a positive note, though the majority of our sample had a gap in AP therapy of at least 60 days, approximately 60% of those who initially discontinued their index OAAP resumed the same medication (~33%) or initiated a different OAAP (~29%) 3–4 months later, on average. Still, more than 30% had no evidence of any AP re-initiation after discontinuing their index medication. These results demonstrate the heterogeneity of schizophrenia treatment patterns during a 12-month period and point to the need to better understand the medication-related decisions made by patients and prescribers which future studies could explore.
AP non-adherence is strongly associated with negative outcomes (eg, schizophrenia relapse) that may result in the increased utilization of costly resources including hospitals and EDs.17,18 Similar results would be expected regarding AP non-persistence. We found that patients who persistently took OAAP medication had significantly fewer all-cause ED visits and hospitalizations, as well as significantly shorter hospital stays compared with the non-persistent cohort. The same patterns were observed for schizophrenia-related visits, and these findings are aligned with previous findings of studies examining AP persistence and healthcare resource utilization.13,18
In summary, the current study provides updated findings on persistence with OAAP medication, the mainstay of treatment, among patients with schizophrenia. Furthermore, it strengthens the evidence regarding the importance of AP medication persistence in this population. Persisting with AP medication is associated with improved clinical outcomes and fewer hospitalizations and ED visits, which has a positive impact on patient quality of life and an economic benefit for state Medicaid programs. The study also provides insight into medication treatment patterns after initial discontinuation, with most patients resuming AP therapy a few months later. Patients discontinue AP medication for a variety of reasons, including negative attitudes regarding medication, drug side effects, and impaired insight into their illness.19,20 Thus, efforts to better understand and address these issues at the point of prescribing should be encouraged in order to improve medication persistence among patients with schizophrenia. Furthermore, AP medication persistence should continue to be evaluated as the study of schizophrenia expands (eg, exosome biomarkers for diagnosis and treatment)21 and therapies for schizophrenia evolve and improve.
Limitations
This study has several limitations that should be considered when interpreting results. Duration of illness could not be determined and heterogeneity of this variable in our sample could impact our results. We assume that these patients were newly started on an OAAP after at least a 6-month period with no evidence of AP utilization, but we had no insight into any previous AP utilization that could play a role in patients’ medication-taking behavior. We used claims data compiled for administrative purposes which comes with inherent limitations. For example, evidence that an OAAP was dispensed does not guarantee consumption. We were limited to only those variables provided in the dataset and could not account for services that may have occurred outside of the Medicaid system. Data miscoding is a possibility and could not be identified. Finally, as we were blinded to the number and identity of the states included in our dataset, we advise caution in the generalization of results to the entire US Medicaid population of patients with schizophrenia.
Conclusion
This study adds to the literature by contributing updated insight into the issue of persistence with AP medications among Medicaid patients with schizophrenia. Persistence findings, which provide valuable temporal information regarding medication discontinuation, are not as abundantly available in the literature as adherence results. Our findings confirmed that medication persistence is poor during the first 12 months after OAAP initiation, and a substantial proportion of patients discontinue their medication within the first 2 months of treatment. Moreover, discontinuation of these drugs is associated with increased hospital and ED resource utilization. Opportunities for future research include investigations of non-medical drivers of health that contribute to medication non-persistence using primary data sources that build on our findings of differences in treatment utilization among racial/ethnic groups. To achieve better outcomes among patients with schizophrenia, efforts to improve and sustain persistence with AP medications are warranted and should address patient-reported barriers to persistent medication use.
Disclosure
Kristin Richards and Michael Johnsrud are employees of The University of Texas at Austin and conducted the research through a grant from Cerevel Therapeutics. Christopher Zacker and Rahul Sasané are employees of Cerevel Therapeutics.
References
1. Menditto E, Cahir C, Malo S, et al. Persistence as a robust indicator of medication adherence-related quality and performance. Int J Environ Res Public Health. 2021;18(9):4872. doi:10.3390/ijerph18094872
2. Hartman L, Lems WF, Boers M. Outcome measures for adherence data from a medication event monitoring system: a literature review. J Clin Pharm Ther. 2019;44(1):1–5. doi:10.1111/jcpt.12757
3. Lin D, Thompson-Leduc P, Ghelerter I, et al. Real-world evidence of the clinical and economic impact of long-acting injectable versus oral antipsychotics among patients with schizophrenia in the United States: a systematic review and meta-analysis. CNS Drugs. 2021;35(5):469–481. doi:10.1007/s40263-021-00815-y
4. Semahegn A, Torpey K, Manu A, et al. Psychotropic medication non-adherence and its associated factors among patients with major psychiatric disorders: a systemic review and meta-analysis. Syst Rev. 2020;9(1):17. doi:10.1186/s13643-020-1274-3
5. García S, Martínez-Cengotitabengoa M, López-Zurbano S, et al. Adherence to antipsychotic medication in bipolar disorder and schizophrenia patients: a systematic review. J Clin Psychopharmacol. 2016;36(4):355–371. doi:10.1097/JCP.0000000000000523
6. Sendt K-V, Tracy DK, Bhattacharyya S. A systematic review of factors influencing adherence to antipsychotic medication in schizophrenia-spectrum disorders. Psychiatry Res. 2015;225(1–2):14–30. doi:10.1016/j.psychres.2014.11.002
7. Shah A, Xie L, Kariburyo F, et al. Treatment patterns, healthcare resource utilization and costs among schizophrenia patients treated with long-acting injectable versus oral antipsychotics. Adv Ther. 2018;35(11):1994–2014. doi:10.1007/s12325-018-0786-x
8. Pesa JA, Doshi D, Wang L, et al. Health care resource utilization and costs of California Medicaid patients with schizophrenia treated with paliperidone palmitate once monthly or atypical oral antipsychotic treatment. Curr Med Res Opin. 2017;33(4):723–731. doi:10.1080/03007995.2016.1278202
9. Richards K, Johnsrud M, Zacker C, Sasané R. One-year medication treatment patterns, healthcare resource utilization, and expenditures for Medicaid patients with schizophrenia starting oral atypical antipsychotic medication. Adm Policy Ment Health. 2023;1–10. doi:10.1007/s10488-023-01327-1
10. Pilon D, Joshi K, Tandon N, et al. Treatment patterns in Medicaid patients with schizophrenia initiated on a first- or second-generation long-acting injectable versus oral antipsychotic. Patient Prefer Adherence. 2017;11:619–629. doi:10.2147/PPA.S127623
11. Cahaya N, Kristina SA, Widayanti AW, Green J. Interventions to improve medication adherence in people with schizophrenia: a systematic review. Patient Prefer Adherence. 2022;16:2431–2449. doi:10.2147/PPA.S378951
12. Phan SV. Medication adherence in patients with schizophrenia. Int J Psychiatry Med. 2016;51(2):211–219. doi:10.1177/0091217416636601
13. Panish J, Karve S, Candrilli SD, Dirani R. Association between adherence to and persistence with atypical antipsychotics and psychiatric relapse among US Medicaid-enrolled patients with schizophrenia. J Pharm Health Serv Res. 2013;4(1):29–39. doi:10.1111/jphs.12004
14. Greene M, Yan T, Chang E, et al. Medication adherence and discontinuation of long-acting injectable versus oral antipsychotics in patients with schizophrenia or bipolar disorder. J Med Econ. 2018;21(2):127–134. doi:10.1080/13696998.2017.1379412
15. Geissler KH, Ericson KM, Simon GE, et al. Differences in insurance coverage for individuals with schizophrenia after implementation of the Patient Protection and Affordable Care Act. JAMA. 2023;80(3):278–279. doi:10.1001/jamapsychiatry.2022.4628
16. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. doi:10.1097/01.mlr.0000182534.19832.83
17. Dilla T, Ciudad A, Alvarez M. Systematic review of the economic aspects of nonadherence to antipsychotic medication in patients with schizophrenia. Patient Prefer Adher. 2013;7:275–284. doi:10.2147/PPA.S41609
18. Jiang Y, Ni W. Estimating the impact of adherence to and persistence with atypical antipsychotic therapy on health care costs and risk of hospitalization. Pharmacotherapy. 2015;35(9):813–822. doi:10.1002/phar.1634
19. Velligan DI, Sajatovic M, Hatch A, et al. Why do psychiatric patients stop antipsychotic medication? A systematic review of reasons for nonadherence to medication in patients with serious mental illness. Patient Prefer Adherence. 2017;11:449–468. doi:10.2147/PPA.S124658
20. Joseph B, Narayanaswamy JC, Venkatasubramanian G. Insight in schizophrenia: relationship to positive, negative and neurocognitive dimensions. Indian J Psychol Med. 2015;37(1):5–11. doi:10.4103/0253-7176.150797
21. Du Y, Chen L, X-S L, et al. Metabolomic identification of exosome-derived biomarkers for schizophrenia: a large multicenter study. Schizophr Bull. 2021;47(3):615–623. doi:10.1093/schbul/sbaa166
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.