Back to Journals » Research and Reports in Urology » Volume 15
Assessing the Variability of the Twelfth Rib as a Landmark for Percutaneous Nephrolithotomy Using Computed Tomography
Authors Tempo JA, Williams GM, Robertson IK, Rama DJ, Pascoe CEA, Cetti RJ
Received 9 March 2023
Accepted for publication 1 July 2023
Published 3 August 2023 Volume 2023:15 Pages 355—363
DOI https://doi.org/10.2147/RRU.S409414
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Panagiotis J Vlachostergios
Jake A Tempo,1 Georgina M Williams,1 Iain K Robertson,2,3 Darren J Rama,1 Claire EA Pascoe,1 Richard J Cetti1
1Department of Urology, Launceston General Hospital, Launceston, Tasmania, Australia; 2College of Health and Medicine, University of Tasmania, Hobart, Tasmania, Australia; 3Clifford Craig Foundation, Launceston General Hospital, Launceston, Tasmania, Australia
Correspondence: Jake A Tempo, Department of Urology, Launceston General Hospital, 3/182 Hawdon Street, Heidelberg, VIC, Launceston, Tasmania, 3084, Australia, Tel +61448438937, Email [email protected]
Background: The variability in length of the twelfth rib is mentioned in the literature but has never been formally studied. The highly variable rib length provides a challenge for urologists seeking a consistent landmark for Percutaneous Nephrolithotomy (PCNL). We set out to determine whether the twelfth rib is safe to use as a consistent landmark for surgery.
Methods: Single centre, cross-sectional retrospective observational study and analysis of CT scans of 100 adults who had imaging between 23rd March and 12th April 2020. The distance from the mid-sagittal line to the twelfth rib tip in the axial plane was measured as was the distance from the twelfth rib tip to the kidney, spleen and liver.
Results: Length from the mid-sagittal line to the right twelfth rib tip varied from 46 (percentile 95% CI 40 to 57) to 136mm (percentile 95% CI 133 to 138). On the left, the distances varied from 55 (percentile 95% CI 50 to 64) to 134mm (percentile 95% CI 131 to 135). Twenty-three percent of people had an organ lying between the tip of the twelfth rib and the kidney on the right and 11% on the left.
Conclusion: The twelfth rib is highly variable in length. Similar variability was recorded in the distance from the tip to intra-abdominal organs. Due to the frequency of organs lying between the tip of the rib and the kidney it should not be used as a landmark for accessing the kidney without prior knowledge of an individual patient’s anatomy as seen on imaging.
Keywords: percutaneous nephrolithotomy, rib, anatomical marker
Introduction
Percutaneous nephrolithotomy is the gold-standard procedure for removing large or complex renal stones.1,2 Despite this, PCNL carries the risk of significant morbidity, with contemporary series describing a complication rate of 20.5%.3 The use of the twelfth rib as a landmark for puncture during PCNL continues to be described in the surgical literature despite the twelfth rib being highly variable in its length.4–9 The use of an inconsistent landmark, which varies in its relationship to the target organ, and other nearby viscera, and as a result, PCNL and retroperitoneal access should not be performed without pre-operative imaging.4
Injury to abdominal viscera (liver, spleen, colon) is rare but potentially catastrophic complications of PCNL. The incidence of injury to intra-abdominal organs is low, often reported as case series in the literature and therefore difficult to accurately quantify. A 2016 literature review reported that colonic perforation occurred in <0.5% of PCNL operations.10 Nine cases of small bowel perforation have been published worldwide, 11 cases of splenic injury and one case of liver injury.10 A retro-renal colon was found in 1.9% of patients positioned in a supine position for PCNL.11 A study of 200 patients found that 1% of patients had a retro-renal colon on the left and in 9% of patients part of the colon passes posterior to the most posterior aspect of the kidney.12 Colonic perforation is more common in left-sided PCNL, lower calyceal punctures, horse-shoe kidneys, older patients, puncture posterior to the mid-axillary line and patients with colonic dilatation.11,13 Injuries to the colon are not always detected immediately and may necessitate parenteral nutrition, laparotomy and stoma formation.10 Injury to the liver and spleen may present with haemodynamic compromise, collapse, or sudden decrease in haemoglobin. Management may include the infusion of clotting factors, high-dependency care, embolization, prolonged nephrostomy placement, laparotomy, packing and splenectomy.14–16 Minimising the risk of injury to abdominal viscera is key to performing safe PCNL and retroperitoneal surgery. Percutaneous access can be achieved fluoroscopically or via ultrasound by a urologist or an interventional radiologist.17
The debate regarding ideal positioning is controversial and continues15 (Table 1). With regard to anatomy, the medial displacement of the bowel in the modified supine position has been postulated to reduce the risk of colonic injury. Studies have shown that there is a 1.9–6% chance of colon lying in the line of access supine, compared to 10–15% in the prone position.18,19
 |
Table 1 Supine versus Prone Positioning for Percutaneous Nephrolithotomy |
Anatomy and Embryology of the Twelfth Rib
The cartilage of the ribs begins development in the mesoderm in the sixth week of gestation and ossification begins in the eighth week.27 The head and tubercle secondary ossification begins at 15 years of age and is complete by 25.27 The twelfth rib has a single facet joint with the T12 vertebral body’s articular margins and curves anteriorly.27 The variation in morphology of the rib cage has been well defined; however, no specific study into the variability of the length of the twelfth rib has been performed.27–29 The twelfth rib attachments include quadratus lumborum, the costodiaphragmatic recess of the pleura, latissimus dorsi, the external oblique, iliocostalis, serratus posterior inferior, the lumbocostal ligament, and the inferior levator costae.30 Recent studies of rib anatomy have been taken from CT images which are readily available for analysis without the expense and time constraints of cadaver dissection.29,31 A study comparing CT measurements of rib geometry of cadaveric subjects to the “ground truth” histology of the ribs reported that the use of CT imaging can be used to define and compare geometric properties of ribs.32 The anatomy of the kidney does not appear to change significantly from the supine to the prone position as assessed on CT imaging.33
Multiple surgical textbooks and articles continue to suggest the use of the twelfth rib tip as a landmark for surgeons when performing the initial puncture at the start of a PCNL case.4–9 The use of an inconsistent surface landmark may provide surgeons false reassurance that they are at less risk of injuring nearby viscera. Advances in medical imaging have allowed scrutiny of anatomical landmarks which have been recited verbatim by medical students and clinicians for centuries.31
The aim of this study is to assess the variability in the length of the twelfth rib and its relationship to the kidney and other organs. For use as a reliable surgical landmark without prior imaging, a bony prominence must be fixed in its position to both the target organ and organs at risk of injury. We hope to highlight that the twelfth rib should only be used as a landmark for PCNL puncture when its relationship to other organs is confirmed with imaging.
Methods and Materials
Study Design and Selection Criteria
A cross-sectional retrospective observational study of CT scans of 100 adults who had imaging between 23rd March and 12th April 2020 in an Australian hospital. The study was approved by the University of Tasmania ethics committee to complete the study with no requirement for informed patient consent as no identifiable images or patient data were collected or stored. The software used for measurement was IntelliSpace PACS 4.4 Enterprise with ISyntax technology. All patients were in the supine position and were asked to be at full inspiration for the duration of the scan. Exclusion criteria included previous retroperitoneal surgery or spinal deformity.
Data Collection
Measurements were taken from each twelfth rib tip to the mid-sagittal line in the axial plane (Figure 1). In the same axial plane, measurements were taken from the twelfth rib tip to the colon, kidney and liver (on the right), and spleen (on the left). Note was taken if an organ lay between each twelfth rib tip and kidney in the axial plane (Figures 2 and 3).
 |
Figure 1 Method for measuring twelfth rib tip to mid-sagittal line. |
 |
Figure 2 Assessing the tract from the left twelfth rib tip to the left kidney. |
 |
Figure 3 Assessing the tract from the right twelfth rib tip to the right kidney. |
Power Analysis
A priori analysis was not performed. However, retrospective power analysis for 100 subjects using one-sample test of proportions (notional intervening organ rate of 0.05% compared to minimum sought rate of 1.2% compared to actual rate of 23% on right and 11% on left; alpha 0.05, power >80%), and using one-sample test of standard deviations (SD) of twelfth rib length (notional SD of 5mm compared to minimum sought SD of 7.5mm compared to actual SD of 19–21mm; alpha 0.05, power >80%) demonstrated that adequate numbers of participants were included in the study.
Outcome Measurements
The distance from the mid-sagittal line to the twelfth rib tip in the axial plane was measured, and only fully ossified bone was included. The recorded measurement is a surrogate for true rib length due to the absence of software that can accurately measure a curved structure across coronal and axial planes. Although this is not a true measurement, it is equally useful clinically. To highlight the variability in the relationship of the twelfth rib tip and adjacent viscera, the distance from the twelfth rib tip to the kidney, spleen and liver was also measured in the axial plane.
Statistical Analysis
The distribution of length of the twelfth rib, and its position in relation to other structures was analysed by estimating the mean, standard deviation, and centile values (1st, 5th, 10th, 25th, 50th, 75th, 90th, 95th, 99th) using bootstrapping estimates of those values from 1000 bootstrap samples. Bootstrap estimation methods allow estimation of distribution values without assuming normality of distribution, whilst also providing a better estimation of the underlying population that might be distorted by outliers. Estimates were made for all cases, and for each gender separately.
The association between the incidence of intervening organ between twelfth rib tip and kidney and the mid-sagittal line to twelfth rib tip (MSL-12RT) distance evaluated by estimating the incidence rate ratio using Poisson regression, adjusted for age and MSL-12RT distance: Z-scores [(patient value minus mean)/standard deviation] of age and gender-specific MSL-12RT distances were used as predictors in the regression models. The sensitivity and specificity of optimum risk score thresholds were estimated again using a bootstrap procedure. First, the mean coefficient values for the risk scores for the left and right kidneys were estimated using a Poisson model for prediction of an intervening organ as outcome and the midline to twelfth rib tip distance (MSL-12RT) and twelfth rib tip to kidney distance (12RT-K) z-scores. One thousand bootstrap samples were created; the Poisson regression model estimated; the mean values of the regression constants for the model from the 1000 samples were estimated; those coefficients were then applied to each of a new 1000 bootstrap samples with risk scores for the 100 cases in each of the 1000 samples calculated. Twenty-one possible threshold values ranging from −3.0 to −1.0 were then used to classify the risk scores, and 2-by-2 case-exposure tables for each of the thresholds in each of the 1000 samples were created. The mean values for the four cells in the 2-by-2 tables were calculated, and percentile 95% confidence intervals were estimated from the 1000 samples.
Results
Demographics
Data was collected from 48 men and 52 women with an average age of 63.5 years, one patient was under 25 years old (Table 2).
 |
Table 2 Demographics Table |
Twelfth Rib Length
Length from the mid-sagittal line to the right twelfth rib tip varied from 46mm (percentile 95% CI 40 to 57) to 136mm (percentile 95% CI 133 to 138) (Table 3). On the left, the distances varied from 55 (percentile 95% CI 50 to 64) to 134mm (percentile 95% CI 131 to 135). The mean distances were 101mm on the right (standard deviation 21; median 105; inter-quartile ranges were 25mm (92 to 117mm)) and 102mm on the left (SD 19; median 104; inter-quartile ranges were 27mm (90 to 117mm)).
 |
Table 3 Estimate of the Mean, Standard Deviation and Centile Values of the Position of the Twelfth Rib Tip in Relation to Other Structures: All Subjects, Axial View |
Relationship to Abdominal Viscera
The distance between the tip of the twelfth rib and abdominal organs was measured if the organ in question was visible on the same axial image as the tip of the twelfth rib. In 97% of CT series, the right kidney was visible in the same axial plane as the twelfth rib tip and 100% on the left. The length from the right twelfth rib tip to the kidney ranged from 5.1mm (percentile 95% CI 4.8 to 7.3) to 62mm (percentile 95% CI 48 to 64). The length from the left twelfth rib tip to the kidney ranged from 4.0mm (percentile 95% CI 3.5 to 5.0) to 52mm (percentile 95% CI 44 to 59).
On the left, the spleen was visible in 28% of patients in the same axial plane as the twelfth rib tip and 94% of patients had colon visible on the same plane (Table 4). The distance between the left twelfth rib tip and the spleen ranged from 3.3mm (percentile 95% CI 2.5 to 6.0) to 52mm (percentile 95% CI 42 to 58). The distance between the left twelfth rib tip and the colon ranged from 5.5mm (percentile 95% CI 3.8 to 9.4) to 138mm (percentile 95% CI 123 to 140). Eighty-two percent of patients had their liver visible in the same axial plane as the right twelfth rib tip and 58% of patients had the colon visible in the same plane as the twelfth rib tip. The distance between the right twelfth rib tip and the liver ranged from 3.1mm (percentile 95% CI 2.7 to 15) to 102mm (percentile 95% CI 82 to 105). The distance between the right twelfth rib tip and the colon ranged from 3.1mm (percentile 95% CI 2.7 to 5.0) to 144mm (percentile 95% CI 120 to 156).
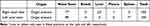 |
Table 4 Raw Number of Cases Where an Organ Was Seen Between the Twelfth Rib-Tip and Kidney on CT Scan Axial and Coronal Views |
Twenty-three percent of people (95% CI 15% to 32%) had an organ lying between the tip of the twelfth rib and the kidney on the right, in 22 cases this was the liver and in one was the pleura. Eleven percent of people (95% CI 5.6% to 19%) had an organ lying between the tip of the twelfth rib and the kidney on the left. Seven percent had a spleen between the twelfth rib tip and the kidney, and four patients had colon between the rib-tip and the kidney.
Discussion
Percutaneous nephrolithotomy is a potentially morbid procedure. Large international series shows that the majority are undertaken with fluoroscopy (85.7%) and by a urologist (93%).3 The learning curve has been quoted up to 60 cases to achieve competency.34 The use of the twelfth rib as a landmark for percutaneous access continues to be described in the surgical literature.4–9
Our study demonstrates that the twelfth rib is highly variable in its length. Similar variability was recorded in the distance from the tip to intra-abdominal organs. Due to the high likelihood of organs lying between the tip of the twelfth rib and the kidney, the tip of the twelfth rib should not be used as a puncture point landmark for percutaneous access without confirmation, with imaging, that the tract is safe. We demonstrate that 23% of our cohort would risk liver or pleura injury when accessing the right kidney using the twelfth rib tip as the location for puncture if the needle passes in the same axial plane towards the kidney. Eleven percent of patients would risk splenic or bowel injury as the needle passed from the twelfth rib tip to the kidney on the left in the same axial plane.
Our study, as well as being the first to objectively measure the variability in twelfth rib anatomy, also emphasises that scrutiny of individual patients’ cross-sectional imaging is mandatory prior to any retroperitoneal percutaneous approach. The urologist should assess individual patient anatomy, stone burden and plan a route to access a favourable calyx for stone extraction, avoiding nearby structures. The twelfth rib should be used as a landmark, but only in conjunction with cross-sectional imaging, to guide safe puncture of the kidney. Future literature needs to reflect this.
Limitations
The use of CT imaging in our study, compared to studying cadavers is justified both due to the time and expense of using cadavers. Using CT imaging rather than cadavers allows visualisation of the relationships between anatomical structures in living subjects without post-mortem changes in anatomical relationships. The rib length using our surrogate measure (mid-sagittal line to rib tip) is as useful to describe variability as the true length.
The line to the kidney from the twelfth rib tip was measured in only one axial plane, whereas retroperitoneal surgery and PCNL are three-dimensional procedures and surgeons may avoid intervening viscera by targeting a calyx for puncture that is in a separate plane. The length between the twelfth rib tip and the kidney will be affected by the extent of muscularity or obesity of patients, and in this study, this will be specific to this Australian population. Tasmanian adults, from which the cohort was selected, had a 32.3% obesity rate between 2014 and 15 compared with 39.6% of US adults between 2015 and 16.35,36 All patients in this study were in the supine position during their CT, and therefore the anatomical relationships may differ in prone and lateral PCNL positions. Analysis of the surrogate rib length in the supine position has demonstrated the variability in its length and relationship to viscera in the supine position and future studies could analyse the relationship between the twelfth rib tip and viscera in prone positions.
Images of the participants were taken at full inspiration, as per the local CT imaging protocol. As all the patients in the scan were under the same conditions, it is unlikely to affect analysis of variability between participants; however, we did not have record of patient adherence to breath holding during imaging. Patients undergoing PCNL puncture typically are not at maximal inhalation, and therefore the incidence of organs lying between the twelfth rib tip and the kidney may be different to our findings based on CT imaging. We did not have access to the individual patients’ ethnicity data; however, our rib length variability is likely to be similar amongst individuals of all ethnicities.
Conclusion
The twelfth rib is highly variable in its length, and in its relationship to intra-abdominal viscera. Therefore, as an inconsistent landmark, it is not safe to rely on the twelfth rib tip as a puncture site for retroperitoneal and percutaneous renal surgery without first assessing the nearby anatomy with imaging. Our study reinforces the need to plan individualised access, with cross-sectional or ultrasound imaging, and for surgeons not to rely solely on the twelfth rib as a landmark.
Funding
No funding to declare.
Disclosure
Dr Iain K Robertson is an employee of Clifford Craig Foundation, during the conduct of the study. The authors report no other conflicts of interest in this study. The interim findings of this study were presented at the 2020 Societe Internationale d’Urologie congress and the 2022 International Conference on Urology with corresponding abstract published in World Academy of Science, Engineering and Technology International Journal of Medical and Health Sciences. This study complies with The Declaration of Helsinki.
References
1. Preminger GM, Assimos DG, Lingeman JE, Nakada SY, Pearle MS, Wolf JS. Chapter 1: AUA guideline on management of staghorn calculi: diagnosis and treatment recommendations. J Urol. 2005;173(6):1991–2000. doi:10.1097/01.ju.0000161171.67806.2a
2. Türk C, Knoll T, Petrik A, Sarica K, Straub M, Seitz C. Guidelines on urolithiasis. Eur Assoc Urol. 2011;3(4):193–198. doi:10.1177/1756287211418725
3. Labate G, Modi P, Timoney A, et al. The percutaneous nephrolithotomy global study: classification of complications. J Endourol. 2011;25(8):1275–1280. doi:10.1089/end.2011.0067
4. Ganpule AP, Vijayakumar M, Malpani A, Desai MR. Percutaneous nephrolithotomy (PCNL) a critical review. Int J Surg. 2016;36:660–664. doi:10.1016/j.ijsu.2016.11.028
5. Novick AC, Jones JS. Operative Urology at the Cleveland Clinic. Totowa, New Jersey: Humana Press; 2006.
6. Joseph J, Patel H. Retroperitoneal, Robotic and Laparoscopic Surgery. London: Springer-Verlag; 2011.
7. Panaiyadiyan S, Singh P, Kumar R. Laparoscopic stone surgery. In: Practical Management of Urinary Stone. Springer; 2021:203–215.
8. Deng R, Huang X, Xiao Y, Meng L, Wang J. A percutaneous nephrolithotripsy performed in the oblique supine lithotomy position: a better choice. Surg Innov. 2021;29(3):360–366.
9. Haider A, Mahmud SM. Supracostal percutaneous nephrolithotomy, a safe and effective approach: a clinical audit. JPMA. 2022;72(2):287–291.
10. Kallidonis P, Panagopoulos V, Kyriazis I, Liatsikos E. Complications of percutaneous nephrolithotomy: classification, management, and prevention. Curr Opin Urol. 2016;26(1):88–94. doi:10.1097/MOU.0000000000000232
11. Traxer O. Management of injury to the bowel during percutaneous stone removal. J Endourol. 2009;23(10):1777–1780. doi:10.1089/end.2009.1553
12. Sherman JL, Hopper KD, Greene AJ, Johns TT. The retrorenal colon on computed tomography: a normal variant. J Comput Assist Tomogr. 1985;9(2):339–341. doi:10.1097/00004728-198503000-00021
13. Mousavi-Bahar SH, Mehrabi S, Moslemi MK. Percutaneous Nephrolithotomy Complications in 671Consecutive Patients: a Single-Center Experience. Urol J. 2011;8(4):271–276.
14. Knoedler JJ, Gettman MT, Fleming CJ. Bowel and other organ injuries with percutaneous nephrolithotomy. In: Smith’s Textbook of Endourology. Wiley Backwell; 2019:422–426.
15. Ghani KR, Andonian S, Bultitude M, et al. Percutaneous nephrolithotomy: update, trends, and future directions. Eur Urol. 2016;70(2):382–396. doi:10.1016/j.eururo.2016.01.047
16. Coccolini F, Coimbra R, Ordonez C, et al. Liver trauma: WSES 2020 guidelines. World J Emerg Surg. 2020;15:1–15. doi:10.1186/s13017-020-00302-7
17. Armitage JN, Withington J, Fowler S, et al. Percutaneous nephrolithotomy access by urologist or interventional radiologist: practice and outcomes in the UK. BJU Int. 2017;119(6):913–918. doi:10.1111/bju.13817
18. Tuttle DN, Yeh BM, Meng MV, Breiman RS, Stoller ML, Coakley FV. Risk of injury to adjacent organs with lower-pole fluoroscopically guided percutaneous nephrostomy: evaluation with prone, supine, and multiplanar reformatted CT. J Vasc Intervent Radiol. 2005;16(11):1489–1492. doi:10.1097/01.RVI.0000175331.93499.44
19. Hopper K, Yakes W. The posterior intercostal approach for percutaneous renal procedures: risk of puncturing the lung, spleen, and liver as determined by CT. AJR Am J Roentgenol. 1990;154(1):115–117. doi:10.2214/ajr.154.1.2104692
20. Yuan D, Liu Y, Rao H, et al. Supine versus prone position in percutaneous nephrolithotomy for kidney calculi: a meta-analysis. J Endourol. 2016;30(7):754–763. doi:10.1089/end.2015.0402
21. Zhang X, Xia L, Xu T, Wang X, Zhong S, Shen Z. Is the supine position superior to the prone position for percutaneous nephrolithotomy (PCNL)? Urolithiasis. 2014;42(1):87–93. doi:10.1007/s00240-013-0614-3
22. Duty B, Waingankar N, Okhunov Z, Levi EB, Smith A, Okeke Z. Anatomical variation between the prone, supine, and supine oblique positions on computed tomography: implications for percutaneous nephrolithotomy access. Urology. 2012;79(1):67–71. doi:10.1016/j.urology.2011.06.019
23. Edgcombe H, Carter K, Yarrow S. Anaesthesia in the prone position. Br J Anaesth. 2008;100(2):165–183. doi:10.1093/bja/aem380
24. Karami H, Mohammadi R, Lotfi B. A study on comparative outcomes of percutaneous nephrolithotomy in prone, supine, and flank positions. World J Urol. 2013;31(5):1225–1230. doi:10.1007/s00345-012-0889-y
25. Jones MN, Ranasinghe W, Cetti R, et al. Modified supine versus prone percutaneous nephrolithotomy: surgical outcomes from a tertiary teaching hospital. Invest Clin Urol. 2016;57(4):268–273. doi:10.4111/icu.2016.57.4.268
26. Mak DK-C, Smith Y, Buchholz N, El-Husseiny T. What is better in percutaneous nephrolithotomy–Prone or supine? A systematic review. Arab J Urol. 2016;14(2):101–107. doi:10.1016/j.aju.2016.01.005
27. McMinn R. Last’s Anatomy. Regional and Applied.
28. Holcombe SA, Wang SC, Grotberg JB. The effect of age and demographics on rib shape. J Anat. 2017;231(2):229–247. doi:10.1111/joa.12632
29. Weaver AA, Schoell SL, Stitzel JD. Morphometric analysis of variation in the ribs with age and sex. J Anat. 2014;225(2):246–261. doi:10.1111/joa.12203
30. Cranfield KA, Buist RJ, Nandi PR, Baranowski AP. The twelfth rib syndrome. J Pain Symptom Manage. 1997;13(3):172–175. doi:10.1016/S0885-3924(96)00271-0
31. Ali Mirjalili S, McFadden SL, Buckenham T, Stringer MD. A reappraisal of adult abdominal surface anatomy. Clin Anatomy. 2012;25(7):844–850. doi:10.1002/ca.22119
32. Holcombe SA, Kang Y-S, Wang SC, Agnew AM. The accuracy of local rib bone geometry measurement using full body CT images.
33. Sengupta S, Donnellan S, Vincent J, Webb D. CT analysis of caliceal anatomy in the supine and prone positions. J Endourol. 2000;14(7):555–557. doi:10.1089/08927790050152131
34. de La Rosette JJ, Laguna MP, Rassweiler JJ, Conort P. Training in percutaneous nephrolithotomy—a critical review. Eur Urol. 2008;54(5):994–1003. doi:10.1016/j.eururo.2008.03.052
35. Huse O, Hettiarachchi J, Gearon E, Nichols M, Allender S, Peeters A. Obesity in Australia. Obes Res Clin Pract. 2018;12(1):29–39. doi:10.1016/j.orcp.2017.10.002
36. Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007–2008 to 2015–2016. JAMA. 2018;319(16):1723–1725. doi:10.1001/jama.2018.3060
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
