Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 16
An Analysis of Post-Traumatic Stress Disorder and Quality of Life Among Adults Living with HIV in Western Uganda
Authors Kabunga A , Kigongo E , Udho S, Auma AG, Tumwesigye R, Musinguzi M, Acup W , Akello AR, Okalo P, Nabaziwa J, Shikanga EM, Halima N
Received 10 November 2023
Accepted for publication 27 February 2024
Published 5 March 2024 Volume 2024:16 Pages 73—82
DOI https://doi.org/10.2147/HIV.S449298
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Olubunmi Akindele Ogunrin
Amir Kabunga,1 Eustes Kigongo,2 Samson Udho,3 Anna Grace Auma,3 Raymond Tumwesigye,3 Marvin Musinguzi,4 Walter Acup,4 Anne Ruth Akello,2 Ponsiano Okalo,1 Jannat Nabaziwa,4 Enos Mwirotsi Shikanga,5 Namata Halima6
1Department of Psychiatry, Faculty of Medicine, Lira University, Lira City, Uganda; 2Department of Environmental Health and Disease Control, Faculty of Public Health, Lira University, Lira City, Uganda; 3Department of Midwifery, Faculty of Nursing and Midwifery, Lira University, Lira City, Uganda; 4Department of Community Health, Faculty of Public Health, Lira University, Lira City, Uganda; 5Department of Education Psychology, Moi University, Eldoret City, Kenya; 6Department of Mental Health, Makerere University, Kampala City, Uganda
Correspondence: Amir Kabunga, Department of Psychiatry, Faculty of Medicine, Lira University, P.O Box 1035, Lira City, Uganda, Tel +256777929576, Email [email protected]
Background: HIV/AIDS remains a significant global public health issue, profoundly impacting infected individuals. Living with HIV involves complex mental health dynamics, with post-traumatic stress disorder (PTSD) being a prevalent challenge. This study aims to examine the correlation between PTSD and quality of life among HIV-positive individuals in western Uganda.
Material and Methods: Conducted between May and July 2023, this facility-based cross-sectional study surveyed 439 participants from four HIV clinics in southwestern Uganda. Data were collected through interviewer-administered questionnaires, analyzed using descriptive statistics, simple linear regression, and multiple linear regression (p< 0.05).
Results: Respondents had a mean age of 40.6 years, with 68.3% female, 54.9% married, and 55.1% lacking formal education. The reported PTSD prevalence among HIV-positive individuals was 33.7%, significantly correlating with reduced overall quality of life (β = − 4.52; p< 0.001). The social quality of life had the highest mean score of 14.24 (± 3.45) while the environmental quality of life had the lowest mean score 11.89 (± 2.68).
Conclusion: Our study reveals a concerning prevalence of PTSD, affecting 1 in 3 individuals, emphasizing the pressing need for comprehensive mental health support within HIV care settings. We observed a significant negative impact of PTSD on overall quality of life, particularly in physical and social aspects. Integrating mental health screening into routine HIV care is crucial, using validated tools like the PSTD Checklist Civilian Version, alongside training for healthcare providers to recognize PTSD symptoms in the context of HIV diagnosis and treatment.
Keywords: HIV, mental health, post-traumatic stress disorder, quality of life
Background
HIV/AIDS is still a major global public health concern that has a profound effect on people who are infected.1 The World Health Organization (WHO) projects that, of the estimated 39.0 million (33.1 million–45.7 million) HIV-positive people globally, 630,000 (480,000–8880,00) died from AIDS-related illnesses in 2022.2 Sub-Saharan Africa remains the most affected region, with over two-thirds of all people living with HIV.2 However, living with HIV involves a complex interplay of mental health factors that affect an individual’s overall well-being. One of the most prevalent and debilitating psychological challenges experienced by people living with HIV is post-traumatic stress disorder (PTSD).3
A large body of research has demonstrated the correlation between PTSD and depression, substance abuse problems, poor HIV clinical outcomes, and nonadherence to medicinal interventions4 Moreover, data suggests that PTSD may contribute to HIV disease progression, which is marked by a notable decrease in CD4 cells.5 Additionally, PSTD adversely affects the quality of life of individuals living with HIV6 Quality of life is a broad term that encompasses several aspects of physical, mental, and social health.7 Quality of life is significantly impacted by the interplay of medical, psychological, and social aspects for individuals living with HIV.8 An individual experiencing PTSD may find their quality of life significantly reduced as a result of increased psychological distress, disruptions to daily routines, and a general decrease in life pleasure.
PTSD is a trauma-related disorder that is characterized by reexperiencing, avoidance, negative cognition, mood, and arousal for at least one month.9 For people living with HIV, PTSD can be triggered by a variety of traumatic experiences, including the diagnosis of a life-threatening illness such as HIV, the stigma and discrimination associated with it, and the personal and economic challenges that often accompany the diagnosis. Following an HIV diagnosis, infected individuals may feel intrusive thoughts of disease or death and may try to avoid situations, persons, and locations that remind them of the disease.3 When compared to the general population, people living with HIV have a higher prevalence of PTSD10 The combined prevalence of PTSD in ten low-income nations was 22%, which was considerably greater than the 4% lifetime prevalence of PTSD found in 25 high-income countries.11 Studies show that pre-HIV trauma history, a lower perceived amount of support, a higher level of stigma, and physical symptoms linked to HIV are risk factors for PTSD symptomatology.3
Individuals living with HIV who also experience PTSD are at an elevated risk of somatisation and physical disorders.12 The impact of PTSD on the illness experience, characterized by persistent avoidance and re-experiencing of traumatic events, can further compromise the quality of life and lead to significant distress in people living with HIV.12 Consequently, untreated PTSD may exacerbate both PTSD symptoms and HIV progression.3 Moreover, evidence suggests that reductions in PTSD symptom severity correlate with improved HIV-related outcomes.12 Given the association between PTSD and elevated HIV risk behaviors, along with the increased likelihood of HIV transmission as the disease progresses, understanding and intervening with PLWH who suffer from PTSD is crucial.
In Uganda, where HIV stigma is still a major problem, people living with HIV may experience social marginalization, discrimination, and isolation. Feelings of hopelessness, anxiety, depression, and ultimately PTSD might result from these experiences.13 HIV and PTSD can coexist in a vicious loop that can seriously impair a person’s entire quality of life3 PTSD affects PWH in Uganda disproportionately. According to recent studies of people living with HIV in northern3 and southwestern Uganda, 65%3 and 28.3%,14 respectively, experienced PTSD symptoms. Notably, the prevalence of PTSD and coping mechanisms were the main emphasis of this research, rather than quality of life.
The diagnosis of HIV often serves as a traumatic event that can trigger or exacerbate symptoms of PTSD, including reexperiencing, avoidance, negative cognition, mood disturbances, and hyperarousal.3 Moreover, the pervasive stigma, discrimination, and social marginalization experienced by people living with HIV in Uganda13 further contribute to the development and maintenance of PTSD symptoms. This dual burden of HIV and PTSD can significantly impact an individual’s quality of life across multiple domains, including physical, psychological, social, and environmental well-being. Despite the recognition of the co-occurrence of HIV and PTSD in Uganda, there is a paucity of research specifically examining the relationship between these two conditions and their impact on quality of life among individuals living with HIV in western Uganda. Therefore, this study seeks to address this gap by conducting a comprehensive analysis of PTSD prevalence and its association with quality of life among people living with HIV in Western Uganda.
Materials and Methods
Study Setting
The present study was conducted in southwestern Uganda. The region is made up of Mbarara, Bushenyi, Ntungamo, Kanungu, Rukungiri, Kabale, Kisoro, Kirugura, and other districts. The participants were recruited from four HIV clinics (ranging between 5000 and 15,000 patients).14 A recent study in the region reported the prevalence of PTSD among people living with HIV.14
Research Design
A facility-based cross-sectional design using was employed in the present study. Data was collected from four HIV clinics (ranging between 5000 and 15,000 patients) between May and July, 2023.
Study Participant and Sample Size Estimation
All participants included in our study were individuals living with HIV who were receiving care at HIV clinics in southwestern Uganda. In our study, we focused on adults aged 18 years and above, and adolescents were not included in the sample. The sample size was estimated using a mathematical expression N = Z2 PQ/D2, where: N = sample size, Z = normal distribution at 1.96 that corresponds to a 95% confidence interval, P = 50% is the estimated proportion in the target population with PTSD, D = the margin of errors allowed, which corresponds to a 0.05 error, and Q = the estimated proportion of depression (1-P) = 50%. Based on the formula, the sample size is 384 participants. After adding 20% of the sample size for the non-response rate, the total sample was 460.
Sampling Criteria
We consecutively recruited 460 participants on clinic days to participate. All participants meeting the inclusion criteria and available during the clinic days were recruited. Adults aged 18 years and above were eligible for recruitment.
Study Instruments
Three interviewer-administered questionnaires were used in data collection: a questionnaire addressing sociodemographic information, the PSTD Checklist Civilian Version (PCL-C-5), and the World Health Organization Quality of Life Brief Version (WHOQOL-Brief). The sociodemographic data comprised age, gender, marital status, and educational attainment levels. In this study, PTSD was assessed using the PTSD Checklist Civilian Version (PCL-C-5). The PCL-C-5 is a well-established tool designed to measure PTSD symptoms in individuals who have experienced traumatic events. It consists of 17 items categorized into three domains: hyperarousal, avoidance, and reexperiencing. Each item is rated on a 5-point Likert scale, with higher scores indicating a higher level of PTSD symptomatology. PTSD is a trauma-related mental health condition characterized by symptoms such as reexperiencing traumatic events, avoidance of triggers related to the trauma, negative changes in mood and thinking, and heightened arousal. In the context of our study, PTSD specifically refers to the psychological distress experienced by individuals living with HIV due to various traumatic experiences associated with their diagnosis, including stigma, discrimination, and personal/economic challenges. We utilized a cutoff score of 44 on the PCL-C-5 to identify individuals with probable PTSD,15 as this threshold has been shown to enhance the sensitivity and specificity of the diagnosis.
The WHOQOL-Brief contains 26 items. Two items are on general quality of life, and the remaining items are divided into four domains: physical, psychological, social, and environmental. The WHOQOL-Brief is a 5-point Likert scale, with a higher score indicating a better quality of life. Each domain’s total score may range from 4 to 20, with higher scores signifying a higher quality of life. The Cronbach alpha for WHOQOL-Brief in this study was 0.93.
Procedures
Four research assistants with a background in social science and experience in research collected data. We visited the HIV clinics on clinic days and waited for potential participants. After permission from the officers in charge, participants were recruited after receiving their medical services. The aim of the study, the methods of data collection, and the time frame for the study were explained to the participants before data collection. Participation was voluntary, and those who consented were enrolled in the study and then completed an interviewer-administered questionnaire. There was a trained psychologist in case they needed help. It took between 25 and 30 minutes to complete the survey.
Statistical Analysis
Data entry and cleaning were performed in the statistical product and service solution (SPSS) software, after which they were exported to the Stata Statistical (2017) Software, StataCorp LLC, College Station, Texas, for formal analysis. The demographic data was presented as the mean with standard deviation (for continuous data) and frequencies and proportions (for categorical data). After careful assessment of the underlying assumptions, including linearity, normality, multi-collinearity, and homoscedasticity, we performed a simple linear regression to assess associations between quality of life and experience of PTSD at p<0.2. Multiple linear regression analyses were performed to report the adjusted analysis. The significance level was set at 5% (p<0.05).
Ethical Approval and Consent to Participation
The study adheres to the guidelines outlined in the Declaration of Helsinki. The research ethics committee of Lira University approved the study protocol (LUREC-2022-1). The participants filled out the questionnaire anonymously to ensure their privacy was protected and that it would only be used for this study. Confidentiality was ensured, and participation was entirely voluntary. The informed consent form was signed by participants who took part in the study. Additionally, we followed the recommendations for improving the reporting of observational studies in epidemiology when conducting this investigation (STROBE statement).
Results
Demographic Characteristics of the Participants
Of the 460 recruited participants, 439 accepted to be part of the study, giving a response rate of 94.4%. Results in Table 1 show that the mean age of respondents was 40.6 years (standard deviation of 13.3) with a minimum of 18 and maximum of 80 years. Majority of the respondents 265 (60.4%) were aged over 35 years and only 32 (7.3%) were young people aged below 25 years. Most of the respondents, 300 (68.3%), were female, and 241 (54.9%) were married. More than half of the respondents, 242 (55.1%) had no formal education.
 |
Table 1 Sociodemographic Characteristics of Participants (N = 439) |
Post-Traumatic Stress Disorder
In the present study (Table 2), the estimated prevalence of PTSD among people living with HIV in southwestern Uganda was 148 (33.7%).
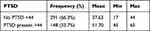 |
Table 2 Post-Traumatic Stress Disorder (N=439) |
Overall Quality of Life
Table 3 indicates that the mean for the overall quality of life was 9.73 with a standard deviation of 6.40, signifying an overall low quality of life. The social quality of life had the highest mean score of 14.24 (±3.45) while the environmental quality of life had the lowest mean score 11.89 (±2.68). Social quality of life refers to the subjective perception of an individual’s social relationships, interactions, and integration into their community or society. It encompasses factors such as social support, interpersonal relationships, and community participation. Table 3 also indicates that the overall quality of life (p<0.001), physical quality of life (p<0.001) and environmental quality of life (p<0.001) were associated with post-traumatic stress disorder.
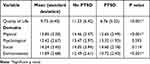 |
Table 3 Overall Quality of Life and Quality of Life Domains (N=439) |
Relationship Between Quality of Life and Post-Traumatic Stress Disorder
We performed a multiple linear regression analysis and adjusted for age and marital status. Table 4 indicates that PTSD was negatively associated with the overall quality of life (β=−4.52; p<0.001), physical quality of life (β=−1.83; p<0.001), and environmental quality of life (β=−1.78; p<0.001). The overall quality of life score was reduced by 4.52 for participants who had PTSD compared to those who did not have PTSD. The physical quality of life score was reduced by 1.83 for participants who had PTSD compared to those who did not. The social quality of life score was reduced by 1.78 for participants who had PTSD compared to those who did not. Also, the result indicates that secondary education increased the physical quality of life score by 1.09 (β = 1.09; p = 0.016), the psychological quality of life score by 0.94 (β = 0.94; p = 0.005), and the social quality of life score by 1.69 (β = 1.69; p = 0.002) as compared to having no formal education. Having primary education increased the social quality of life score by 0.88 (β = 0.88; p = 0.016) compared to having no formal education. Being a female reduced the psychological quality of life score by 0.56 (β = 0.56; p = 0.044) compared to being a male.
 |
Table 4 Relationship Between Quality of Life and PTSD After Adjusting for Demographic Factors |
Discussion
The study conducted in southwestern Uganda revealed a notable prevalence PTSD among people living with HIV, with 33.7% experiencing PTSD symptoms. Furthermore, the analysis showed a significant negative association between PTSD and overall quality of life, as well as specific domains of quality of life such as physical and environmental well-being. Adjusted analyses demonstrated that individuals with PTSD scored lower on overall quality of life, physical quality of life, and environmental quality of life compared to those without PTSD.
The estimated prevalence of post-traumatic stress disorder (PTSD) among people living with HIV in southwestern Uganda, reported at 33.7%, aligns with prior research indicating a high prevalence of PTSD within HIV-positive populations globally.16 This finding underscores the significant mental health burden faced by individuals living with HIV in resource-limited settings, where factors such as poverty, social stigma, and limited access to mental health services exacerbate psychological distress. Studies in similar contexts have consistently highlighted the adverse impact of trauma and chronic stressors on the mental well-being of HIV-positive individuals.6 The implications of this high prevalence of PTSD among people living with HIV in western Uganda are profound, highlighting the urgent need for targeted interventions to address trauma and promote psychological resilience within this population. Effective mental health support not only improves the quality of life for individuals living with HIV but also enhances the overall effectiveness and sustainability of HIV care and treatment programs in the region.
The findings of this study highlight a significant negative association between PTSD and the overall quality of life among individuals living with HIV in western Uganda. This result resonates with previous research that has demonstrated similar detrimental impacts of PTSD on quality of life in various populations.17 The results also, aligns with previous research indicating that PTSD symptoms significantly impact various aspects of quality of life, including physical, social, and environmental domains.17 Studies in different contexts, such as among veterans or survivors of natural disasters, have consistently shown that PTSD symptoms are linked to lower quality of life scores.18 Additionally, research focusing specifically on individuals living with HIV has also indicated a correlation between PTSD and poorer quality of life outcomes.19 The highest mean score in the social quality of life domain suggests that while individuals may still maintain some level of social connection, their overall quality of life is substantially affected by PTSD symptoms. The lowest mean score in the environmental quality of life domain highlights potential challenges related to living conditions and access to resources. These findings highlight the importance the urgent need for targeted interventions addressing both mental health and social determinants of health for people living with HIV and PTSD in Uganda and similar resource-constrained settings.
The findings that participants with secondary education have, on average, higher scores in both physical and psychological quality of life compared to those with no formal education resonate with existing literature that shows the significant impact of education on health outcomes, particularly in populations affected by chronic conditions like HIV.20 A low quality of life was mostly linked to a lower educational level in other studies conducted in Burkina Faso,21 Brazil,22 and Ethiopia.23 Education not only enhances knowledge about HIV prevention and treatment but also fosters greater self-efficacy and coping skills, which are crucial in managing the psychological challenges associated with the condition.24 These findings highlight the importance of implementing educational initiatives targeted at improving the overall well-being of individuals living with HIV in western Uganda. Moreover, addressing educational disparities may help alleviate the burden of comorbidities and promote holistic approaches to HIV care and management in resource-limited settings.
Our results also showed that being female is associated with a reduction in psychological quality of life scores compared to being male. This implies that, on average, females in this study have a lower psychological quality of life compared to males. This gender disparity may be attributed to various factors such as social and economic inequalities, gender-based violence, and differential access to healthcare and support services The finding that being female is associated with a reduction in psychological quality of life scores compared to being male aligns with existing literature indicating gender disparities in mental health outcomes among people living with HIV.25,26 It is currently unknown what variables contribute to these gender disparities in quality of life. However, the findings show the importance of addressing gender-specific mental health needs within HIV care and support programs in western Uganda and similar contexts. Tailored interventions that consider the unique psychosocial challenges faced by women living with HIV, including those related to PTSD, are essential for improving their overall quality of life and treatment outcomes.
Strengths and Limitations of the Study
The results of the present study provide evidence of the relationship between PTSD and quality of life among people living with HIV in western Uganda. However, the results relied on self-reported information, which could have been influenced by recall bias. The cross-sectional nature of this study makes it difficult to determine causality between PTSD and quality of life. There is a need for a longitudinal study to establish a causal relationship between the variables.
Conclusion
Our study reveals a concerning prevalence of PTSD, affecting one in three individuals, emphasizing the pressing need for comprehensive mental health support within HIV care settings. We observed a significant negative impact of PTSD on overall quality of life, particularly in physical and social aspects. Integrating mental health screening into routine HIV care is crucial, using validated tools like the PCL-C-5, alongside training for healthcare providers to recognize PTSD symptoms in the context of HIV diagnosis and treatment.
Data Sharing Statement
The datasets used and /or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgment
The authors wish to acknowledge the participants in this study.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit it to the current journal; gave final approval for the version to be published; and agreed to be accountable for all aspects of work.
Funding
The authors received no funding for this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bekker L-G, Beyrer C, Mgodi N, et al. HIV infection. Nat Rev Dis Primers. 2023;9(1):42. doi:10.1038/s41572-023-00452-3
2. Reliefweb. Global HIV & AIDS statistics — fact sheet 2023; 2023. Available from: https://reliefweb.int/report/world/global-hiv-aids-statistics-fact-sheet-2023.
3. Arebo B, Ewach GF, Omara J, et al. Post-traumatic stress disorder and coping strategies among people with HIV in Lira District, Uganda: a cross-sectional study. HIV/AIDS - Research and Palliative Care. 2022;Volume 14:255–264. doi:10.2147/HIV.S358575
4. McLean CP, Fitzgerald H. Treating posttraumatic stress symptoms among people living with HIV: a critical review of intervention trials. Curr Psychiatry Rep. 2016;18(9):1–9. doi:10.1007/s11920-016-0724-z
5. Neigh GN, Rhodes ST, Valdez A, Jovanovic T. PTSD co-morbid with HIV: separate but equal, or two parts of a whole? Neurobiol Dis. 2016;92:116–123. doi:10.1016/j.nbd.2015.11.012
6. Onu DU, Ugwu SS, Nnadozie EE, Orjiakor CT. Stigma affects the health-related quality of life of people living with HIV by activating posttraumatic stress symptoms. J Clin Psychol Med Settings. 2023;30(3):561–569. doi:10.1007/s10880-022-09928-y
7. Karimi M, Brazier J. Health, health-related quality of life, and quality of life: what is the difference? Pharmacoeconomics. 2016;34(7):645–649. doi:10.1007/s40273-016-0389-9
8. Mendonca CJ, Newton-John TRO, Alperstein DM, et al. Quality of life of people living with HIV in Australia: the role of stigma, social disconnection and mental health. AIDS Behav. 2023;27(2):545–557. doi:10.1007/s10461-022-03790-7
9. Compean E, Hamner M. Posttraumatic stress disorder with secondary psychotic features (PTSD-SP): diagnostic and treatment challenges. Prog Neuro Psychopharmacol Biol Psychiatry. 2019;88:265–275. doi:10.1016/j.pnpbp.2018.08.001
10. Verhey R, Chibanda D, Brakarsh J, Seedat S. Psychological interventions for post-traumatic stress disorder in people living with HIV in resource poor settings: a systematic review. Trop Med Int Heal. 2016;21(10):1198–1208. doi:10.1111/tmi.12756
11. Ng LC, Stevenson A, Kalapurakkel SS, et al. National and regional prevalence of posttraumatic stress disorder in sub-Saharan Africa: a systematic review and meta-analysis. PLoS Med. 2020;17(5):e1003090. doi:10.1371/journal.pmed.1003090
12. Tang C, Goldsamt L, Meng J, et al. Global estimate of the prevalence of post-traumatic stress disorder among adults living with HIV: a systematic review and meta-analysis. BMJ Open. 2020;10(4):e032435. doi:10.1136/bmjopen-2019-032435
13. Jolle J, Kabunga A, Okello TO, et al. HIV-related stigma experiences and coping strategies among pregnant women in rural Uganda: a qualitative descriptive study. PLoS One. 2022;17(10):e0272931. doi:10.1371/journal.pone.0272931
14. Kekibiina A, Adong J, Fatch R, et al. Post-traumatic stress disorder among persons with HIV who engage in heavy alcohol consumption in southwestern Uganda. BMC Psychiatry. 2021;21(1):1–9. doi:10.1186/s12888-021-03464-z
15. Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD checklist (PCL). Behav Res Ther. 1996;34(8):669–673. doi:10.1016/0005-7967(96)00033-2
16. Beckerman NL, Auerbach C. Post-traumatic stress disorder and HIV: a snapshot of co-occurrence. Soc Work Health Care. 2010;49(8):687–702. doi:10.1080/00981389.2010.485089
17. Leserman J, Whetten K, Lowe K, et al. How trauma, recent stressful events, and PTSD affect functional health status and health utilization in HIV-infected patients in the south. Psychosom Med. 2005;67(3):500–507. doi:10.1097/01.psy.0000160459.78182.d9
18. Kabunga A, Okalo P, Nalwoga V, Apili B. Landslide disasters in eastern Uganda: post-traumatic stress disorder and its correlates among survivors in Bududa District. BMC Psychol. 2022;10(1):287. doi:10.1186/s40359-022-01001-5
19. Gore-Felton C, Ginzburg K, Chartier M, et al. Attachment style and coping in relation to posttraumatic stress disorder symptoms among adults living with HIV/AIDS. J Behav Med. 2013;36(1):51–60. doi:10.1007/s10865-012-9400-x
20. Rwegerera GM, Moshomo T, Gaenamong M, et al. Health-related quality of life and associated factors among patients with diabetes mellitus in Botswana. Alexandria J Med. 2018;54(2):111–118. doi:10.1016/j.ajme.2017.05.010
21. Bakiono F, Ouédraogo L, Sanou M, et al. Quality of life in people living with HIV: a cross-sectional study in Ouagadougou, Burkina Faso. Springerplus. 2014;3(1):1–11. doi:10.1186/2193-1801-3-372
22. da Silva J, Bunn K, Bertoni RF, Neves OA, Traebert J. Quality of life of people living with HIV. AIDS Care. 2013;25(1):71–76. doi:10.1080/09540121.2012.686594
23. Tesfay A, Gebremariam A, Gerbaba M, Abrha H. Gender differences in health related quality of life among people living with HIV on highly active antiretroviral therapy in Mekelle Town, Northern Ethiopia. BioMed Res Int. 2015;2015:1–9. doi:10.1155/2015/516369
24. Millard T, Elliott J, Girdler S. Self-management education programs for people living with HIV/AIDS: a systematic review. AIDS Patient Care STDS. 2013;27(2):103–113. doi:10.1089/apc.2012.0294
25. Liang J, Bennett JM, Sugisawa H, Kobayashi E, Fukaya T. Gender differences in old age mortality: roles of health behavior and baseline health status. J Clin Epidemiol. 2003;56(6):572–582. doi:10.1016/S0895-4356(03)00060-X
26. Orfila F, Ferrer M, Lamarca R, et al. Gender differences in health-related quality of life among the elderly: the role of objective functional capacity and chronic conditions. Soc Sci Med. 2006;63(9):2367–2380. doi:10.1016/j.socscimed.2006.06.017
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
