Back to Journals » Integrated Blood Pressure Control » Volume 16
Adherence to Lifestyle Modification Practices and Its Associated Factors Among Hypertensive Patients in Bahir Dar City Hospitals, North West Ethiopia
Authors Geremew G, Ambaw F, Bogale EK , Yigzaw ZA
Received 26 September 2023
Accepted for publication 23 November 2023
Published 29 November 2023 Volume 2023:16 Pages 111—122
DOI https://doi.org/10.2147/IBPC.S436815
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Gebeyaw Geremew,1 Fentie Ambaw,2 Eyob Ketema Bogale,2 Zeamanuel Anteneh Yigzaw2
1Department of Nursing, Tibebe Ghion Comprehensive Specialized Hospital, Bahir Dar, Ethiopia; 2Department of Health Promotion and Behavioral Science, School of Public Health, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
Correspondence: Zeamanuel Anteneh Yigzaw, (B.Sc., B.Th., B.A., MPH), Department of Health Promotion and Behavioral Science, School of Public Health, College of Medicine and Health Sciences, Bahir Dar University, P.O. Box: 79 (Bahir Dar University Ethiopia), Bahir Dar, Ethiopia, Tel +251918166551, Fax +251(8)202025, Email [email protected]
Background: Globally, hypertension affects 1.4 billion adults, accounting for 31% of the world population. The prevention and control of hypertension is not addressed only by pharmacological management. Even though the prevalence of uncontrolled hypertension and its complications is increasing every day, Adherence to lifestyle modification practice among diagnosed hypertensive individuals is low for a number of reasons. The study aims to assess adherence to lifestyle modification practices and associated factors among hypertensive patients at Bahir Dar city hospitals, in North West Ethiopia.
Methods: An institutional-based cross-sectional study design was conducted at Bahir Dar city from October 30 to November 30, 2022. A stratified sampling technique was used. For the data quality pre-test was done, the questionnaire was checked for completion, the assumption of binary logistic regression (VIF 1.8 and no outlier), and model fit using the Hosmer and Lemeshow’s test was checked. Binary logistic and multivariate logistic regression were used to find significant variables after the data were entered into EpiInfo and analyzed using SPSS version 23.
Results: The overall adherence to lifestyle modification practices was about 32.4%. From the independent factors, above secondary educational status (AOR = 0.201 95% CI (0.081– 0.499)), good knowledge (AOR = 3.323 95% CI (1.79– 6.168)), good self-efficacy (AOR = 3.553 95% CI (1.91– 6.613)), good social support (AOR = 8.339 95% CI (4.251– 16.357)), and good patient–physician relationship (AOR = 2.424 95% CI (1.309– 4.490)) were statistically significant predictors of adherence to lifestyle modification practices.
Conclusion: Only one-third of the participants had adhered to the recommended lifestyle modifications. Educational status, knowledge, self-efficacy, social support, and patient–physician relationships were significant factors. Healthcare organizations should develop programs to raise hypertension patients’ awareness and degree of self-efficacy that aid in adherence to advised lifestyle changes.
Keywords: adherence, lifestyle modification, hypertension, Bahir Dar
A Letter to the Editor has been published for this article.
Introduction
The term “hypertension” refers to a blood pressure reading of 140/90 mm Hg or greater. It is a significant important risk factor for cardiovascular illnesses. Hypertension has no specific causes but numerous potential causes are reliable indicators of the disease such as age, becoming overweight, tobacco use, alcohol dependence, hereditary factors, and a nutrient-dense diet of fried and calorie-dense foods.1,2
Globally, hypertension affects 1.4 billion adults, accounting for 31% of the world population.3,4 The number of persons with hypertension has increased by 90%, mostly in low- and middle-income nations, and over the previous 40 years, it has been a factor in almost 10.8 million fatalities. Hypertension is the leading cause of heart disease complications, including hemorrhagic (58%) and infarct (50%) stroke, coronary heart disease (55%), and other forms of cardiovascular disease. By 2025, there will be a 60% increase in the prevalence of high blood pressure, and about 25% of adults worldwide are predicted to have high blood pressure.1
The prevention and control of hypertension are not addressed only by pharmacological management; rather, pharmacological management has a great role in hypertension treatment. The Joint National Committee’s eighth report recommends that all hypertensive patients modify their lifestyles, including losing weight, consuming more fruits and vegetables, limiting their salt intake, engaging in physical activity, quitting smoking, and abstaining from alcohol, whether or not they are taking antihypertensive medication.5
The WHO Global Action Plan for the Prevention and Control of NCDs sets nine global NCD targets, including a 25% reduction in the prevalence of high blood pressure, a 30% reduction in the mean population intake of salt, and a 10% reduction in the prevalence of insufficient physical activity.6
One of the most prevalent non-communicable diseases (NCDs) in Ethiopia is hypertension, which presents a significant public health and development challenge. An estimate of the economic expenses of NCDs reveals that they account for 31.3 billion birr annually, or 1.84% of Ethiopia’s GDP in 2017.7 One-third of hypertension is caused by high sodium intake, 20% by inadequate potassium intake, 30% by obesity, 20% by low fitness, and 5% by excessive alcohol consumption.8
The Ethiopian Federal Ministry of Health developed programs and put them into practice to lower the prevalence of behavioral risk factors like smoking, drinking too much alcohol, being inactive, and eating too much salt such as keeping an eye on cigarette use and preventative measures, hiking excise charges on alcoholic beverages, promoting public awareness and offering motivating messages for physical exercise.9,10
Only 10% of cases of hypertension are caused by other types of hypertensions; 90% of cases are primary hypertension, which is primarily caused by an unhealthy diet and a sedentary lifestyle. Pharmacological and non-pharmacological interventions are needed for proper management of hypertension. Non-pharmacological therapies include alterations to one’s way of life, such as cutting back on alcohol intake, exercising, avoiding stress, and changing one’s diet.11
Lifestyle changes help the patient by lowering blood pressure, improving anti-hypertensive drug efficacy, and minimizing heart disease risk.12 The American Institute for Health and Care Excellence’s (NICE) clinical guidebook on high blood pressure advises people with the condition to quit smoking, reduce their alcohol intake, limit their salt intake, and engage in regular cardiovascular exercise in addition to adhering to a low-calorie eating regimen.13
Patients with high blood pressure are better off doing moderate-intensity aerobic activity for thirty minutes each day, or at least 2.5 hours a week.14,15 This can result in a 4 mm Hg drop in systolic blood pressure and a 2.5 mm Hg drop in diastolic blood pressure. Patients who are overweight or obese must be prompted to lose some weight by integrating a low-calorie way of eating with much more exercise and lifestyle changes. Lowering alcohol consumption can noticeably decrease blood pressure.14
Adoption of a healthy diet should always be advised for patients with hypertension, and every hypertensive patient should be forcefully prompted to eat less fat and saturated fat.14,15 Each person should be aggressively encouraged to cut their routine salt intake by at least one-third and, if possible, to less than 5 g (or 90 mmol) of salt. Avoiding high-salt processed foods, snack foods, high-salt takeout items, and salt added during cooking or at the table are all ways to reduce salt intake.14 Patients with high blood pressure who smoke cigarettes have a 2–6-fold increased likelihood of a myocardial infarction and a 3-fold increased risk of stroke in hypertensive patients.14
Good lifestyle modification practices improve health status and reduce blood pressure, which prevents the effects of hypertension complications. A stage one hypertensive patient can do lifestyle modification practices for 6–12 months without cardiovascular complications or the use of medicine.16 About 70% of people with hypertension who simply get pharmaceutical treatment have uncontrollable blood pressure.17 According to a study conducted in the Amhara region of Dessie on adherence to lifestyle modification practices, the general adherence to lifestyle modification practices was only 23.6%.18
Despite being a government priority in Ethiopia, there are a variety of factors that contribute to the low overall lifestyle adherence among those who have been diagnosed with hypertension. There is not any research done in the study area, and there are not many studies done in Ethiopia in this regard. Therefore, we aimed to assess adherence to lifestyle modification practices and their associated factors among hypertensive patients at Bahir Dar city hospitals, in North West Ethiopia.
Methods and Materials
Study Area and Period
This study was carried out in Bahir Dar City administration from September 30 to October 30, 2022. Bahir Dar is the seat of government of the Amhara National Regional State and is located 565 kilometers northwest of Addis Ababa, Ethiopia. The town’s total population (excluding rural Kebeles) is estimated to be about 332,856.19 The city administration is made up of 18 kebeles. There are seven hospitals (three public referral hospitals and four private hospitals) named Tibebe Ghion and Felege Hiwot Comprehensive Specialized Hospitals, Addis Alem Primary Hospital, Gamby, Adinas, Afilas, and Dream Care Hospitals.
Study Design
An institutional-based cross-sectional study design was conducted in Bahir Dar City Hospitals in 2022.
Populations
Source Populations
All hypertensive patients attended the chronic follow-up unit.
Study Unit
All adults with hypertension who met the inclusion criteria took part in the study.
Eligibility Criteria
Inclusion Criteria
All patients with hypertension who were over the age of eighteen and had been receiving chronic follow-up for at least six months were included.
Exclusion Criteria
A patient with hypertension who was critically ill patient was excluded.
Sample Size Determination and Procedure
Sample Size Determination
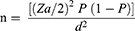
The sample size (n) required for the study was calculated using the single population proportion formula.
Where assumption: with the assumption of a 95% confidence interval, 46.4% of the adherence rate to lifestyle modifications among hypertensive patients in Yekatit 12 Hospital in Addis Ababa.20 With a 5% marginal error computed as follows:
n is the required sample size.
Za/2 is the critical value for normal distribution at a 95% confidence level, which is equal to 1.96.
d = 0.05 for absolute precision.
But when it uses associated variables to determine the sample size, the maximum sample size is expressed by duration with hypertension less than 5 years, which is 383; assuming a 10% non-response rate, the final sample size will be 383 + (38.30) = 422.
Sampling Procedure
In Bahir Dar, there are three public health hospitals and four private hospitals that provide chronic follow-up care. The study included all of the hospitals in Bahir Dar city. The study was carried out in chronic follow-up units across both public and private hospitals. The sample was selected using stratified sampling techniques by taking each hospital as strata and in each strata number of study units was allocated proportionally (depending on the number of patients reporting per month), and the participants who were part of the final sample size were chosen using systematic sampling techniques and proportionally allocated according to population size after determining the k value using the formula N/n, where N is the total population during the study period in the area and n is the sample size determined for the specific area and the first participants were drawn by random sampling technique.
Study Variables
Dependent Variable
Adherence to recommended lifestyle modifications.
Independent Variables
Socio-demographic factors: age, sex, marital status, occupation, level of education, and income
Personal factors: commodities, knowledge about the disease, and duration of HTN
Behavioral factors: self-efficacy
Social factors: support from families and non-family members of society and patient–physician relations
Operational Definitions
Aerobic activity:- is defined as any physical activity that creates a rise in heart rate, fast breathing, and core temperature, like strength training, or taking a walk.13
A normal healthy weight:-The participant is said to have a healthy body weight when the Body mass index of 18.5–24.9.13
Knowledge about lifestyle modification:- It was assessed using eight items. Respondents with sum scores above 6 items on the Hypertension Evaluation of Lifestyle and Management (HELM) scale were taken as having good knowledge about hypertension lifestyle modification.21
Co-morbidities:- a known hypertensive patient with other chronic diseases like heart disease, diabetes mellitus, and other diseases.22
Self-efficacy:- the patient’s belief in his or her capacity to carry out tasks. It is drawn from an eight-item scale. The computed mean from the item was 3.08 and respondents who scored above the mean were classified as having good self-efficacy, and those who scored below the mean were considered to have poor self-efficacy.23
Social support: is the assistance gained from family and friends. The Duke Social Support and Stress Scale item’s computed mean was 3.42. Participants with scores above the median were considered to have strong social support.24
Patient–physician relationship:- Participants who received a mean value of 0.43 and above from the 4-item scale prepared questions about the client interaction in the care and treatment of HTN patients will take this as a good relationship.
Adherent to the DASH diet and salt:- In this study, participants were categorized as not adhering to the DASH diet and salt if they stated that they did not eat a diet high in fruits, vegetables, grains, fish, and salt but instead consumed meals high in spices and saturated fat. The computed mean for the 5 items was 2.63; those who scored higher than the computed mean were considered adherents to dietary control.25
Exercise-related adherence:- participant who reported engaging in at least three times per week of moderate-intensity physical activity for a mean of more than 0.45 hours.25
Weight management adherence:- Six items were evaluated utilizing weight management strategies used in the diet, such as reducing portion sizes and substituting foods, as well as weight loss exercises. The six-item response’s computed mean was 2.47, and individuals who scored higher than the mean were considered to have good weight management habits.
Smoking-related adherence: who disclosed that they either never smoked or quit smoking.
Alcohol consumption-related adherence: Respondents who reported, that they either never consumed alcohol or male patients took less than two bottles female patients took less than one bottle in a day, and those whose overall mean score was greater than 2.3 were taken as adherents to moderation of alcohol consumption.26
Overall adherence to lifestyle modifications: It was evaluated utilizing the following five lifestyle change components: exercise, alcohol use, quitting smoking, food (DASH diet and salt reduction), and weight management. The computed mean from the five components of lifestyle modifications was 0.68. Participants with a score above 0.68 were considered adherents to lifestyle modification practices.
Data Collection Tools
The data was gathered using face-to-face interviewer-administered questions that were developed from multiple literature studies to evaluate total adherence to lifestyle adjustments and factors influencing lifestyle modification.
Before being translated into the local tongue (Amharic), the questions are mostly developed in English. Interviews are conducted using the Amharic translation after which multilingual specialists translate it back into English to ensure uniformity. The questionnaire includes sociodemographic information, social support status, knowledge evaluation, self-efficacy, and characteristics related to lifestyle modification, such as regular physical activity, the DASH diet, weight management, moderate alcohol use, and quitting smoking. To assess both family and non-family support, seven factors from Duke’s stress and social support scale are employed.24 A modified 8-item scale was used to measure knowledge to assess lifestyle choices and hypertension management.21 Eight items with an internal reliability of 0.879 were used to measure self-efficacy. By using the Fast Alcohol Screening Test (FAST), which has an internal consistency value of Cronbach alpha of 0.783, moderate alcohol use was evaluated.27
Data Collection Procedure
A standardized interviewer-administrator questionnaire was used to gather the quantitative data. Weight, height, and other physical characteristics were measured. During the time of data collection, patients were only ever interviewed once, at their initial appointment. Getting the patient’s card number and asking if they were interviewed helped prevent a repeat visit. To foster a supportive and confident environment, the interview is held in a private space.
The skilled nurses employed in the chronic follow-up unit were chosen to gather data, with one BSc nurse acting as supervisor. A consensus was obtained with the participants on the specific nature of the research’s goal before any data was ever collected.
Data Quality Control
The questionnaire was developed in English, translated into Amharic, and then returned to English by multilingual experts to ensure the accuracy of the data. Each questionnaire was pre-tested and validated for accuracy, and the results of logistic regression showed that the chosen model fit, as indicated by the p-value of 0.8 for Hosmer and Lemeshow’s goodness of fit. The checked VIF for binary logistic regression was 1.8. The questionnaire responses should be reviewed by the research assistants to make sure the data is accurate and full.
Seven BSC nurses received training on the study’s purpose, applicability, significance of maintaining information confidentiality, and the value of respecting respondents’ rights as data collectors in preparation for the data collection process. The supervisor closely monitored the data collector while they conducted interviews with respondents and evaluated the information they had gathered for precision and clarity. To improve clarity and make the data-collecting instruments more effective, 5% of the entire sample was pre-tested at the questionnaire level in a chronic hypertension follow-up clinic before data collection.
Data Management and Analysis
Epi Info was used to enter, clean, and export the data for analysis in version 23.0 of SPSS. To verify correctness, consistency, and the lack of missing values, data was cleaned using frequency and cross-tabulation.
The descriptive summary measures mean and percentage for categorical variables were used to summarize the descriptive analysis findings for the independent and dependent (outcome) variables.
Binary logistic regression was used to ascertain the existence and strength of the association between the independent factors and the dependent variable. Candidates for the multiple logistic regression analysis included variables with a significance threshold of p = 0.2.
Furthermore, to account for potential confounding variables and assess the distinct effects of the significant influencing dependent variable, multiple logistic regression analysis was utilized.
An odds ratio with associated p-values and 95% confidence intervals was used to evaluate the existence and strength of the connection.
Results
Socio-Demographic Characteristics of the Study Participants
The study included 398 eligible hypertension patients with a response rate of 94.3% who were receiving care in the chronic follow-up unit of the Bahir Dar City Hospitals. The study included 239 (60.1%) male and 159 (39.9%) female participants. The mean age of participants was 48.1 years, while 49.7% of respondents were above 45 years old and 42.2% were between 30 and 45 years. From there, 132 (33.2%) respondents did not have formal education, 92 (23.1%) were able to read and write, 104 (26.1%), and 54 (13.6%) were educated up to college/diploma and secondary school, respectively. From the perspective of their job status, 128 (32.2%) were farmers, 88 (22.1%) were merchants, and 92 (25.6%) were employed. One hundred five (26.4%) of respondents have income below 1500 ETB, 141 (35.4%), and 57 (14.3%) have income above 7500 ETB (Table 1).
Personal Characteristics of the Study Participants
From 398 respondents, 229 (57.5%) had a mean atrial pressure above the normal range (above 100), which shows their blood pressure is not controlled, and about 169 (42.5%) had a mean atrial pressure in the normal range (70–100). And 96 (24.1%) of participants had a BMI level above the normal range (18.5–24.9 kg/m2), and one hundred sixty-two (40.7%) of respondents were hypertensive for more than 6 years, while 186 (46.7%) of them had hypertensive follow up for 2–5 years. Among the respondents, 249 (62.6%) had one or more comorbidities.
Knowledge About Hypertension of the Study Participants
To determine the level of the respondent’s knowledge regarding hypertension, an 8-item Hypertension Evaluation of Lifestyle and Management (HELM) scale was used. We used the sum score of six as the cut-off point from the total participants, 228 (57.3%) had a poor knowledge level, which is below the cutoff point, while 170 (42.7%) had a good knowledge level.
Behavioral Characteristics of the Study Participants
The self-efficacy of respondents was assessed using the 7-item Chronic Disease Self-Efficacy Scale, which had 5 choices, and the mean score was 3.128 with a standard deviation of 0.986. One hundred and sixty-one (40.5%) of the study’s participants exhibited high self-efficacy, according to the mean value.
Social Characteristics of the Study Participants
To measure the social support status of participants, seven items of the Duke Social Support and Stress Scale were used to assess support gained from family, friends, or significant others. The total computed mean score of the respondent’s social support on this modified scale was 3.42+0.879. Using this mean score as a cutoff point, it was determined that 137 (34.4%) of respondents had good social support from family, friends, or significant others, whereas 261 (65.6%) had poor support and approximately 219 (55%) had poor patient-to-physician communication.
Adherence to Lifestyle Modification Practices of the Study Participants
About 191 (48.0%) of the respondents included fruits, vegetables, grains, and beans in their diet since their hypertension diagnosis, which adheres to dietary management, and 207 (52.2%) of the respondents were not adherent to dietary management.
Physical exercise adherence patients who were doing regular physical exercise was about 190 (47.7%); among these, 44.3% were doing regular physical exercise for more than 30 minutes for more than three days, and the most common types of exercise were walking (23.1%) and jogging (19.6%).
Related to weight management adherence of a patient nearly half of the 200 (51.1%) respondents were careful about the content of the food they ate and cut out drinking sugary food and sweet tea more than usual 183 (46%), and overall adherence was about 190 (47.7%) of the participants who performed weight management activities.
About 19.3% of the patients had ever used tobacco; of these, 11.3% were still smokers. Among the 45 respondents who still smoked cigarettes, 24 had tried to quit smoking. Among participants, 155 (38.9%) used alcohol after the diagnosis of hypertension; 92 male patients took more than two bottles and 44 female patients took more than one bottle in a day, and the overall adherence to alcohol moderation was 252 (63.3%) (Table 2).
 |
Table 2 Adherence to Recommended Lifestyle Modifications Among Hypertensive Patients Who Attended Chronic Follow-Up Units at Bahir Dar City Hospitals, North West Ethiopia, 2022 |
Overall Adherence to Lifestyle Modification Practices
The overall adherence to lifestyle modification practices, including exercise, diet, smoking cessation, weight management, and moderation of alcohol, in the study was about 32.4% (Figure 1).
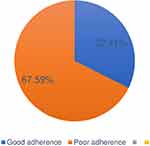 |
Figure 1 The overall adherence of hypertension lifestyle modification practices among Bahir Dar city hospitals, North West Ethiopia, 2022. |
Factors Associated with Lifestyle Modification Practices of the Study Participants
Bivariate and multivariable logistic regression models were used to examine the relationship between dependent and independent variables. With a p-value of 0.2, binary logistic regression analysis showed that gender, educational level, income, time since diagnosis of hypertension, knowledge, social support, self-efficacy, patient–physician relationship, and presence of comorbidity were significantly associated with lifestyle modification practices.
Education-level, self-efficacy, knowledge, social support, and patient-to-physician relationships were statistically significant predictors of adherence to lifestyle modification activities at p 0.05 after adjusting for the confounding factor in multiple logistic regression.
When we compare the educational status of hypertensive patients, participants with secondary education were 79.9% less likely to adhere to recommended lifestyle practices than those with diplomas and above [AOR = 0.201; 95% CI (0.081–0.499)].
Patients with good knowledge status were 3.32 times more adherent to lifestyle modification practice than those who were poorly knowledgeable [AOR = 3.323; 95% CI (1.790–6.1680)].
Respondents with good self-efficacy were almost four times more likely to adhere to lifestyle modification practices than those with poor self-efficacy [AOR = 3.553; 95% CI (1.910–6.613)].
A participant with good social support was eight times more likely to adhere to lifestyle modification practices than a participant with poor social support [AOR = 8.339; 95% CI (4.251–16.357)]. Those with a good patient-physician relationship were almost 2 times more adherent than those who had a poor relationship with their physician [AOR = 2.424; 95% CI (1.309–4.490)] (Table 3).
 |
Table 3 Factors Associated with Adherence to Recommended Lifestyle Modifications Among Hypertensive Patients Attending Chronic Follow-Up Units at Bahir Dar City Hospitals, North West Ethiopia, 2022 |
Discussion
The study investigates adherence to lifestyle modifications and its associated factors among patients with hypertension. The overall good adherence to lifestyle modification among hypertensive patients was 32.4% and factors like educational status, knowledge of respondents, self-efficacy, relationship support, and patient–physician relation were significantly associated with lifestyle modification adherence.
The findings of this study indicate that about 129 (32.4%) of the participants adhered to lifestyle modification practices. This result is much lower than the previous study done in the Amhara region of the Oromia special zone (52.7%),28 and Addis Ababa Yekatite 12 Hospital 46.4%.20 But higher in a study done in Addis Ababa public hospital 23%,29 Dessie specialized hospital 23.6%,18 and Nigeria (16.4%).30 The possible discrepancy may be due to socio-cultural differences, sample size variation, exposure to lifestyle information, and different lifestyle modification styles.
The current study shows about 46.2% of participants adhered to regular physical exercise activity, which was held 3 times a week for a 30-minute duration. This finding resembles the study in the Amhara region of the Oromia special zone 51.0%.28 This could be a result of the research design being employed and some typical tool components being identical. But there was a lower finding in the Addis Ababa public hospital, which was 39.9%,29 Yekatit 12 hospital at 33.9%,20 and Nigeria was 16.3%.30 There may not be enough open spaces for physical activity as a result of Addis Ababa’s urbanization, which could account for this mismatch.
In this study, dietary management was explained by providing more vegetables, fruits, legumes, and grains along with dishes that were lower in salt, fat, and spice. In this study, 48% of the participants were adhering to dietary management. This finding was similar to the study in the Oromia Special Zone, Amhara Region, which was 47.1%.28 But this finding was lower than the study conducted in the Addis Ababa public health hospitals 76.4%,29 and Nigeria 94.4%.30 This discrepancy may be due to differences in dietary habits and knowledge about the effect of a salt diet on blood pressure management.
Adherence to smoking cessation and alcohol abstinence, the most widely practiced activities among other lifestyle modification practices, was 87.9% and 63.3%, respectively. This finding is in line with the Oromia special zone, which is 81.3%.28
And other studies in Addis Ababa’s public hospitals 94%.29 In Nigeria, alcohol consumption adherence was 90.7%, and smoking cessation adherence was 100%.30 This high adherence rate to smoking cessation could be due to socio-cultural norms that discourage smoking.
In this study, 47.7% of participants used weight management practices to control high blood pressure by modifying their lifestyle practices. This finding was similar to that of the study conducted in the Dessie referral hospital, which was 46.7%.18 The possible reason for similarity might be a methodological similarity.
According to the multivariable analysis, educational status, knowledge, patient self-efficacy, patient social support, and physician–physician relationship was strongly associated with adherence to recommended lifestyle modification practices.
Patient educational status was significantly associated with lifestyle modification practices. Participants with secondary education were 79.9% less likely to practice the recommended lifestyle modification when compared with participants who have a diploma and above. In the study done on dietary adherence in Bahir Dar City Hospital, respondents who had college and above educational levels were three times more likely to adhere to the recommended diet intake.31 This may be because higher education levels help patients understand educational information about the disease and have a better chance of coming across considerable information about the disease from different educational sources.
Patients who have good knowledge are 3 times more likely to adhere to lifestyle modification practices than those with poor knowledge. This finding was supported by a study in Dessie,18 and Jordan patients who got high scores in knowledge assessment were 2.9 times more adherent than those who got low scores.32 This is because knowledge of hypertension lifestyle modification practices helps have a positive impact on individual patients’ access, utilization, and outcomes of the recommended lifestyle practices. But much lower than the finding in Addis Ababa public hospitals, where good-knowledge respondents were 13 times more likely to be adherent compared to the poor-knowledge respondents.29 This discrepancy may be due to better information and living standards in Addis Ababa.
When compared to participants who had low self-efficacy, individuals with high self-efficacy were nearly four times more likely to stick with their lifestyle changes. This finding was similar to a study conducted in Addis Ababa, where participants with high self-efficacy were found to be four times more likely to be adherent than those with low self-efficacy.29 The reason could be that more self-assured patients will be inspired to alter their lifestyle in response to the advice.
Participants who had good social support from their families, neighbors, and friends were 8 times more likely to adhere than those with poor social support. These findings were in line with a study in Addis Ababa showing that having good social support made you 11 times more likely to be adherent.29 This might be good social support that can improve emotional well-being and practical help by giving money, encouraging family commitment to prepare a salt-free diet as well as the recommended diet, and decreasing unnecessary external influence, including false beliefs and attitudes, on patient lifestyle recommendations.
A good patient–physician relationship was 2 times as adherent as a poor patient–physician relationship. This might be due to good patient–physician relations increasing trust in health care providers, developing their self-esteem, and patients wanting to wait with the provider for a detailed understanding of lifestyle practices. This finding of physician–patient relations was supported in a study done at Jimma University good relationships with health professionals were 2.01 times more likely to practice the recommended lifestyle modification practices.33
Conclusion
Only one-third of the participants had adhered to the recommended lifestyle modifications. Independent predictors like educational status, knowledge, self-efficacy, social support, and patient–physician relationship were statistically significant predictors of adherence to lifestyle modification practice. Healthcare organizations should create programs to increase hypertensive patients’ awareness and their self-efficacy level that helps adherence to lifestyle modification recommendations.
Abbreviations
ACC, American College of Cardiology; AHA, American Heart Association; AOR, Adjusted Odd Ratio; BMI, Body Mass Index; BP, Blood Pressure, COR, Crude Odd Ratio; CVD, Cardio Vascular Disease; DASH, Dietary Approach to Stop Hypertension; HTN; Hypertension; HELM, Hypertension Evaluation of Life Style Modification; PIH, Pregnancy Induced Hypertension; WH O, World Health Organization.
Data Sharing Statement
The data were available on the corresponding author Zeamanuel Anteneh Yigzaw ([email protected]) upon request.
Ethics Approval and Consent to Participate
The Bahir Dar University College of Medicine and Health Sciences Institutional Review Board (IRB) approved the protocol on the ethical principles of the Helsinki Declaration and assigned it reference number 551/2022. APHI also provided a letter granting permission for the hospitals to take part in the study, with letter number ///-03/1643. For the patients’ willingness to participate, written informed consent was obtained from them.
Acknowledgment
We would like to acknowledge Bahir Dar University College of Medicine and Health Sciences, School of Public Health, hospital admins, data collectors, and patients who participated in the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or all these areas, have drafted or written, or substantially revised or critically reviewed the article, have agreed on the journal to which the article will be submitted, reviewed and agreed on all versions of the article before submission, during revision, the final version accepted for publication, and any significant changes introduced at the proofing stage, agree to take responsibility and be accountable for the contents of the article.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organisation. A Global Brief on Hypertension: Silent Killer, Global Public Health Crisis: World Health Day 2013. World Health Organization; 2013.
2. DK Arnett. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American college of cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation. 2019;140(11):e563–e595.
3. Forouzanfar MH, Liu P, Roth GA. Global burden of hypertension and systolic blood pressure. JAMA. 2017;317(2):165–182. doi:10.1001/jama.2016.19043
4. Mills AE, Bundy JD, Kelly TN. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circul. 2016;134(6):441–450. doi:10.1161/CIRCULATIONAHA.115.018912
5. Ukpabi OJ, Ewelike ID. The Eighth Joint National Committee on the Prevention, detection, evaluation, and treatment of high blood pressure (joint national committee-8) report: matters arising. Nga J Cardiol. 2017;14(1):15. doi:10.4103/0189-7969.201909
6. World Health.Organization. Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020. World Health Organization; 2013.
7. Dombrovskiy VA, Workneh A, Shiferaw F, Small R, Banatvala N. Prevention and control of noncommunicable diseases in Ethiopia: the case for investment, including considerations on the impact of khat. BMC. 2019;1:58.
8. Gurven M, Blackwell AD, Rodríguez DE, et al. Does blood pressure inevitably rise with age? Longitudinal evidence among forager-horticulturalists. Hypertension. 2012;60(1):25–33. doi:10.1161/HYPERTENSIONAHA.111.189100
9. Getachew H, Chanie A, Gebru A. Appraisal of nutrition communication strategies in Ethiopia: efficacy and barriers in the national nutrition program in East Gojjam zone, Amhara region. East Afr J Soc Sci Humaniti. 2022;7:1–14.
10. Non-Communicable Organisation. National strategic action plan (nsap) for prevention & and control of non-communicable diseases in Ethiopia. Google Scholar. 2016;2016:1.
11. Oliveira AE. Potential impact of the new American high blood pressure guidelines on hypertension prevalence in a primary health care Unit in Rio de Janeiro–the Laparc study. Int J Cardio Sci. 2021;34:284–293.
12. Ghezelbash S, Ghorbani A. Lifestyle modification and hypertension prevention. ARYA Atherosc J. 2012;8:1.
13. Nicoll R, Henein MY. Hypertension and lifestyle modification: how useful are the guidelines? Br J Gen Pract. 2010;60(581):p.879–80. doi:10.3399/bjgp10X544014
14. Rakugi H, Kario K, Yamaguchi M, Sasajima T, Gotou H, Zhang J. Efficacy of sacubitril/valsartan versus olmesartan in Japanese patients with essential hypertension: a randomized, double-blind, multicenter study. Hyper Res. 2022;45(5):824–833. doi:10.1038/s41440-021-00819-7
15. Jindal D, Gupta P, Jha D. Development of WellCare: a mHealth intervention for integrated management of hypertension and diabetes in low-resource settings. Global Health Action. 2018;11(1):1517930. doi:10.1080/16549716.2018.1517930
16. Mahmood AE, Shah KU, Khan TM. Non-pharmacological management of hypertension. Irish J Med Sci. 2019;188(2):437–452. doi:10.1007/s11845-018-1889-8
17. Selçuk KT. Hypertensive patients’ adherence to pharmacological and non-pharmacological treatment methods, in Turkey. Int J Community Med Public Health. 2017;4(8):2648–2657. doi:10.18203/2394-6040.ijcmph20173308
18. Andualem A, Gelaye H, Damtie Y. Adherence to lifestyle modifications and associated factors among adult hypertensive patients attending chronic follow-up units of Dessie Referral Hospital, North East Ethiopia, 2020. Integrated Blood Pressure Control. 2020;13:145–156. doi:10.2147/IBPC.S275575
19. wikipedia. Bahir Dar city population estimate; 2022.
20. Aynalem GA, Bekele TA, Berhe TT, Endazenew G. Factors affecting adherence to lifestyle modification among patients with hypertension at Yekatit 12 Hospital Medical College, Addis Ababa, Ethiopia, 2019. SAGE Open Med. 2021;9:205031212110125. doi:10.1177/20503121211012523
21. Schapira MM, Fletcher KE, Hayes A. The development and validation of the hypertension evaluation of lifestyle and management knowledge scale. J Clin Hyper. 2012;14(7):461–466. doi:10.1111/j.1751-7176.2012.00619.x
22. Program NHBPE. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure; 2004.
23. Warren-Findlow J, Seymour RB, Brunner Huber LR. The association between self-efficacy and hypertension self-care activities among African American adults. J Commun Health. 2012;37(1):15–24. doi:10.1007/s10900-011-9410-6
24. Parkerson J, Broadhead WE, Tse CK. Validation of the Duke social support and stress scale. Family Med. 1991;23(5):357–360.
25. Warren-Findlow J, Seymour RB. Prevalence rates of hypertension self-care activities among African Americans. J Natl Med Assoc. 2011;103(6):503–512. doi:10.1016/S0027-9684(15)30365-5
26. Khavari KA. A scale for the indirect assessment of alcohol intake. The alcohol use predictor scale. J Stud Alcohol. 1979;40(7):683–692. doi:10.15288/jsa.1979.40.683
27. Hodgson R. The FAST alcohol screening test. Alcohol Alcohol. 2002;37(1):61–66. doi:10.1093/alcalc/37.1.61
28. Ahmed T. Lifestyle Modification Practice and Associated Factors Among People with Hypertension Attending Chronic Follow-Up Units in Oromiya Special Zone Public Hospitals, Amhara, Ethiopia; 2020.
29. Tibebu A, Mengistu D, Negesa L. Adherence to recommended lifestyle modifications and factors associated with hypertensive patients attending chronic follow-up units of selected public hospitals in addis ababa, Ethiopia. Patient Prefer Adherence. 2017;11:323–330. doi:10.2147/PPA.S126382
30. Iloh GUP. Adherence to lifestyle modifications among adult hypertensive Nigerians with essential hypertension in a primary care clinic of a tertiary hospital in resource-poor environment of Eastern Nigeria. Br J Med Med Res. 2014;4(18):3478. doi:10.9734/BJMMR/2014/9439
31. Feleke AE. Dietary adherence and associated factors among hypertensive patients in Bahir Dar city administration, Ethiopia, 2020. Int J Afr Nur Sci. 2022;7:17.
32. Alefan Q, Huwari D, Alshogran OY, Jarrah MI. Factors affecting hypertensive patients’ compliance with healthy lifestyle. Patient Prefer Adherence. 2019;13:577–585. doi:10.2147/PPA.S198446
33. Lemessa F, Lamessa M. Uncontrolled hypertension and associated factors among hypertensive adults in Bale zone public hospitals, Ethiopia. J Hypertens Manag. 2021;7(1):185–190.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.