Back to Journals » International Journal of Nephrology and Renovascular Disease » Volume 17
Acute Kidney Injury Prediction Model Using Cystatin-C, Beta-2 Microglobulin, and Neutrophil Gelatinase-Associated Lipocalin Biomarker in Sepsis Patients
Authors Susianti H , Asmoro AA, Sujarwoto, Jaya W, Sutanto H, Kusdijanto AY, Kuwoyo KP, Hananto K, Khrisna MB
Received 14 December 2023
Accepted for publication 12 March 2024
Published 28 March 2024 Volume 2024:17 Pages 105—112
DOI https://doi.org/10.2147/IJNRD.S450901
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Pravin Singhal
Hani Susianti,1 Aswoco Andyk Asmoro,2 Sujarwoto,3 Wiwi Jaya,2 Heri Sutanto,4 Amanda Yuanita Kusdijanto,1 Kevin Putro Kuwoyo,1 Kristian Hananto,5 Matthew Brian Khrisna1
1Clinical Pathology Department, Faculty of Medicine Brawijaya University/Saiful Anwar General Hospital, Malang, Indonesia; 2Anesthesiology and Intensive Therapy Department, Faculty of Medicine Brawijaya University/Saiful Anwar General Hospital, Malang, Indonesia; 3Faculty of Public Administration, Brawijaya University, Malang, Indonesia; 4Internal Medicine Department, Faculty of Medicine Brawijaya University/Saiful Anwar General Hospital, Malang, Indonesia; 5Faculty of Medicine, Brawijaya University, Malang, Indonesia
Correspondence: Hani Susianti, Clinical Pathology Department, Medicine Faculty of Universitas Brawijaya/Dr. Saiful Anwar General Hospital, Malang, Indonesia, Email [email protected]
Introduction: AKI is a frequent complication in sepsis patients and is estimated to occur in almost half of patients with severe sepsis. However, there is currently no effective therapy for AKI in sepsis. Therefore, the therapeutic approach is focused on prevention. Based on this, there is an opportunity to examine a panel of biomarker models for predicting AKI.
Material and Methods: This prospective cohort study analysed the differences in Cystatin C, Beta-2 Microglobulin, and NGAL levels in sepsis patients with AKI and sepsis patients without AKI. The biomarker modelling of AKI prediction was done using machine learning, namely Orange Data Mining. In this study, 130 samples were analysed by machine learning. The parameters used to obtain the biomarker panel were 23 laboratory examination parameters.
Results: This study used SVM and the Naïve Bayes model of machine learning. The SVM model’s sensitivity, specificity, NPV, and PPV were 50%, 94.4%, 71.4%, and 87.5%, respectively. For the Naïve Bayes model, the sensitivity, specificity, NPV, and PPV were 83.3%, 77.8%, 87.5%, and 71.4%, respectively.
Discussion: This study’s SVM machine learning model has higher AUC and specificity but lower sensitivity. The Naïve Bayes model had better sensitivity; it can be used to predict AKI in sepsis patients.
Conclusion: The Naïve Bayes machine learning model in this study is useful for predicting AKI in sepsis patients.
Keywords: machine learning, sepsis, AKI, Cystatin C, Beta-2 Microglobulin, NGAL
Introduction
Sepsis is defined as life-threatening organ dysfunction caused by dysregulation of the body’s response to infection. The Intensive Care Over Nations study mentioned, of 10,069 ICU patients worldwide, 29.5% of patients experienced sepsis. The mortality rate of sepsis in the ICU was 25.8%, and the mortality rate in the hospital was 35.3%. Research in the United States shows that approximately 1.7 million adults are hospitalised with sepsis, resulting in an enormous economic burden, as sepsis requires the highest cost of care in US hospitals.1 Sepsis patients have high morbidity and mortality, and the risk is further increased by the occurrence of AKI (acute kidney injury). AKI is a frequent complication in sepsis patients and is estimated to occur in almost half of patients with severe sepsis. AKI in sepsis is associated with poor outcomes, including more extended hospitalisation, higher mortality, and increased healthcare costs.2
AKI is a sudden decline in renal function (within hours), which includes structural damage and or loss of renal function. AKI patients generally have a mixed aetiology of sepsis, ischemia, and nephrotoxicity, which often occur together, complicating diagnosis and therapy.3 The prevalence of AKI in Indonesia in 2013 was estimated at 11%.4 However, there is currently no effective therapy for AKI in sepsis. Therefore, the therapeutic approach is focused on the prevention of AKI and supportive care, as well as the timely initiation of renal replacement therapy.5 Based on this, biomarkers to detect AKI early are needed.
Renal injury biomarkers are analogous to troponins released by myocardial cells after myocardial ischemia or infarction, so they are more sensitive early markers of kidney injury than creatinine.6 Currently, AKI is detected by an increase in serum creatinine levels and or a decrease in urine output. Still, creatinine has limitations because its levels will increase when kidney damage is ≥ 50%. Based on this, several low molecular weight proteins detected in the serum of AKI patients are thought to be early biomarkers of AKI. These promising biomarkers include Cystatin C, Beta-2 Microglobulin (Β2MG), and Neutrophil Gelatinase-Associated Lipocalin (NGAL).7
Cystatin C is a 13-kDa cysteine proteinase inhibitor produced by all nucleated cells, freely filtrated by the glomerulus, and reabsorbed but not secreted by the renal tubules.7 A meta-analysis showed elevated levels of Cystatin C in sepsis patients with AKI.8 In addition, Cystatin C also has a high predictive value for the incidence of AKI in elderly sepsis patients.9
NGAL is a kidney-secreted 24-kDa glycoprotein and was identified as a biomarker of AKI, as its concentration increases significantly after ischemic kidney injury.10 Research by Xie et al mentioned that NGAL is a superior examination compared to other biomarkers in detecting AKI and is considered a “renal troponin”.11
Beta-2 Microglobulin (β2MG) is a 12-kDA protein, a significant component of histocompatibility antigens. Β2MG is filtered in the glomerulus, and 99.9% is reabsorbed in the proximal tubule. Research by Barton et al in 2018 mentioned that serum Β2MG could identify AKI, and its increase is directly proportional to the severity of AKI.12 Based on the data above, further research on the role of these biomarkers in sepsis patients with AKI is still needed.
In addition to Cystatin C, Β2MG, and NGAL biomarkers, this study will add laboratory examination data routinely used in sepsis to develop the panel model. The examination data used was based on the complete blood count (haemoglobin level, hematocrit, total leukocyte count, neutrophil count, lymphocyte count, NLR, RDW, MCHC, PDW, and platelet count), blood sugar level, urea, creatinine, SGOT, SGPT, bilirubin, serum electrolytes (sodium, potassium, chloride), and albumin.
Based on the description above, there is an opportunity to examine a panel of biomarker models for predicting AKI that has never been done before; it is expected to be a novelty in this study using machine learning technology (artificial intelligence).
Materials and Methods
Study Design
This prospective cohort study analysed the differences in Cystatin C, Beta-2 Microglobulin, and NGAL levels in sepsis patients with AKI and sepsis patients without AKI. In addition, the diagnostic performance in AKI of these biomarkers was analysed. The data sources used in this study are primary data obtained from the measurement of Cystatin C, Beta-2 Microglobulin, and NGAL levels using the Enzyme-linked Immunosorbent Assay (ELISA) method and secondary data obtained from medical records to determine the diagnosis of sepsis, kidney injury (AKI), and sample characteristics. These data was then analysed and made into a biomarker model for predicting the occurrence of AKI using machine learning. This study was conducted in the ICU and HCU at Dr. Saiful Anwar Hospital Malang (RSSA) and RSSA Central Laboratory from January to September 2023. The participants of this test were 130 samples divided into healthy participant group, sepsis with AKI, and sepsis without AKI.
The inclusion criteria of this study were participants who are 18–60 years old, not pregnant, not suffering from autoimmune disease, and not an ESRD (end-stage renal disease) patient. The time of sepsis diagnosis was based on the patient’s SOFA score correlated with the patient’s clinical condition. The creatinine level was followed up until the seventh day after sepsis diagnosis, and those are the samples taken for the measurement of the biomarkers in this study.
Routine Laboratory Test to Diagnose Sepsis
All participants at the initial stage underwent a complete laboratory examination that is commonly requested in sepsis patients, namely DL, which includes white blood cell count (WBC), absolute neutrophil count (NE), absolute lymphocyte count, NLR, serum lactate, PH, PaCO2, PaO2, and PaO2/FiO2, procalcitonin (PCT), liver function tests (SGOT, SGPT), kidney function tests (urea, creatinine, eGFR), and electrolyte tests.
Biomarkers to Diagnose AKI
In addition to the above examinations, all samples will be examined for Cystatin C, Beta-2 Microglobulin, and NGAL levels using venous blood samples with ELISA. The principle of examination is to use specific antibodies attached to the bottom of the well, forming solid-phase antibodies. The sample is added to the well, followed by a second antibody labelled with a horseradish peroxidase (HRP) enzyme. If the sample contains Cystatin C or Beta-2 Microglobulin or NGAL, an enzyme-labeled antibody-antigen-antibody complex will form. The presence of this complex will cause a blue colour change. The concentration of Cystatin C, β2MG, or NGAL in the samples is determined by comparing the samples’ optical density (OD) with the standard curve.
Each participant was also tested for creatinine (using a Cobas c-501 chemical autoanalyser), and urine output was monitored daily for seven days to assess the presence of AKI according to KDIGO criteria.
Model Analysis
The biomarker modelling of AKI prediction was implemented using machine learning, specifically Orange Data Mining. The outcomes of these analyses are typically represented by performance metrics such as AUC, sensitivity, specificity, PPV, and NPV. As indicated by these metrics, the model with the highest overall performance will be selected.
A predictive biomarker model of AKI was created by combining the Cystatin C, Beta-2 Microglobulin, and NGAL biomarkers. The model was then expanded by incorporating several laboratory tests that are routinely examined in sepsis patients, including complete blood count, blood sugar, urea, creatinine, SGOT, SGPT, bilirubin, serum electrolytes, and albumin.
Statistical Analysis
This study employed descriptive analysis to determine the mean and standard deviation of Cystatin C, Beta-2 Microglobulin, and NGAL levels across the study groups. A one-way ANOVA test or Kruskal–Wallis test was performed to assess the comparison between the three research groups: the healthy participant group, the sepsis group with AKI, and the sepsis group without AKI, with a significance value of < 0.05, using SPSS software.
Results
Patients Characteristics
The study groups differed in age and creatinine levels. The mean age was 32.91 ± 6.40 years in healthy participants, 57.58 ± 13.30 years in sepsis patients with AKI, and 58.10 ± 17.00 years in sepsis patients without AKI. Haemoglobin was lower in sepsis groups compared to healthy participants. Creatinine was highest in sepsis patients with AKI, followed by sepsis patients without AKI, and lowest in healthy participants (Table 1).
 |
Table 1 Characteristics of Patient Included in This Study |
Biomarkers for AKI in Sepsis Patients
This study identifies three novel biomarkers for predicting AKI in sepsis patients. In this study, Beta-2 Microglobulin (7.83 ± 3.55) was higher than in the healthy participants group (1.64 ± 0.24) and in sepsis patients without AKI (7.27 ± 3.95). We found a significant difference among the three study groups in NGAL and Beta-2 Microglobulin. All the parameters used in this study are listed in Table 2. The comparison data for β2MG, Cystatin C, and NGAL are shown in Table 3.
 |
Table 2 List of Common Biomarkers Used in This Study |
 |
Table 3 Renal-Associated Biomarkers Result |
Diagnostic performance analysis using receiver operating curve (ROC) cut-off was done for the biomarkers. At the optimal cut-off value of 7.54 mg/dL for β2-microglobulin (β2MG), the sensitivity was 60.4% and the specificity was 73.2%. For Cystatin C (CysC) at a cut-off of 0.5315 mg/dL, the sensitivity and specificity were 54.2% and 51.2%, respectively. Using a 60.7065 ng/mL cut-off for Neutrophil Gelatinase-Associated Lipocalin (NGAL), the sensitivity was 66.7% and the specificity was 59.8% (Table 4).
 |
Table 4 Sensitivity, Specificity, PPV, and NPV of Each Parameter Using ROC Curve-Based Cut-off |
Diagnostic Performance for Predicting AKI Patients
This study employed machine learning algorithms, namely Support Vector Machine (SVM) and Naïve Bayes, to evaluate their effectiveness in predicting acute kidney injury (AKI). The performance of each model was assessed based on its sensitivity, specificity, negative predictive value (NPV), and positive predictive value (PPV).
The SVM model exhibited a sensitivity of 50%, indicating its ability to correctly identify 50% of actual AKI cases. On the other hand, its specificity was 94.4%, implying that it accurately ruled out 94.4% of non-AKI cases. The NPV and PPV of the SVM model were 71.4% and 87.5%, respectively. These values suggest that the model was more effective in identifying true negatives (non-AKI cases) than true positives (AKI cases).
The Naïve Bayes model demonstrated a sensitivity of 83.3%, outperforming the SVM model in correctly detecting AKI cases. Its specificity, however, was slightly lower at 77.8%. The NPV and PPV of the Naïve Bayes model were 87.5% and 71.4%, respectively. The diagnostic test parameters of both SVM and Naïve Bayes are shown in Table 5.
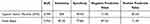 |
Table 5 Diagnostic Test Parameters for the Machine-Learning Parameters of Acute Kidney Injury |
Discussion
Our study investigates the AUC, sensitivity, specificity, PPV, and NPV values of machine learning that combines the predictive biomarker values of AKI in sepsis patients namely Cystatin C, Beta-2 Microglobulin, and NGAL, and combined with several laboratory tests routinely examined in sepsis patients such as complete blood count (haemoglobin level, total leukocyte count, neutrophil count, lymphocyte count, NLR, RDW, PDW, and platelet count), blood sugar, urea, creatinine, SGOT, SGPT, bilirubin, serum electrolytes (sodium, potassium, chloride), and albumin. There is evidence that the incidence of AKI is associated with outcomes in critically ill sepsis patients, so laboratory tests in sepsis patients were also included in this machine learning.13
In our study, the healthy participants had normal creatinine, whereas creatinine is increased and abnormal both in the group of sepsis with no AKI but to a lesser extent than in the group of sepsis with AKI. Sepsis can increase creatinine through inflammatory effects on renal microvasculature; therefore, increased creatinine is not necessarily caused by AKI.14
One hundred thirty samples were analysed in our study by machine learning. The parameters used to obtain the biomarker panel are 23 laboratory examination parameters. This study used biomarkers such as NGAL, Cystatin C, and Beta-2 Microglobulin, which can be used to diagnose AKI patients.7 The levels of the biomarkers and some of the routine laboratory parameters are time-related. Because of this, the participant’s samples were taken when the diagnosis of sepsis was made to mitigate the influence of sample collection time on the results of the biomarker examination.
To select an appropriate diagnostic test, it is recommended that the most specific test be used to confirm the positivity of a test (ruling in) and the most sensitive test be used to establish that a disease is unlikely (ruling out). A highly sensitive test will correctly identify most diseased individuals as positive, thus ruling out negative results. A highly specific test will confirm the disease in those with positive results, thus ruling in disease with a positive test.15 In our study, compared to the SVM model, Naïve Bayes had a lower AUC, specificity, NPV, and PPV but a higher sensitivity, making it more suitable for AKI rule-out modalities. The SVM model has a higher specificity, making it more suitable for use as a rule-in AKI modality.
A study by Luo et al obtained an AUC of 0.76 (95% CI 0.73–0.78) with sensitivity and specificity of 63% and 76%, respectively. The machine learning model in this study had a higher AUC and specificity but lower sensitivity, and the parameters used were more diverse than in the previous study.16 That study also used a similar sample size to our study. A study conducted by He et al obtained an AUC of 0.728, which is lower than the value obtained in our study. The study by He et al used sepsis patients as subjects, while our study used a population of sepsis and non-sepsis patients with more parameters.17
In another recent study on machine learning in AKI screening in sepsis, the AUC values predicted by the model 12–48 hours before the onset of AKI were between 0.774–0.788 and 0.756–0.813, which were lower than the AUC in this study. However, this study used a larger sample of around 21 thousand samples, ie, it was more representative of the sepsis patient population.18 In some of the above studies, the criteria for AKI patients were obtained from observations for 12 to 48 hours, and retrospective data was used. In contrast, the AKI criteria were obtained in our study after observing sepsis patients for seven days according to the KDIGO criteria.19
In our study, the AUC value with the SVM model was higher than other models in several studies regarding sepsis in AKI, so the true positives and true negatives of using machine learning in this study are expected to be better. The SVM model of machine learning had higher AUC and specificity but low sensitivity. The Naïve Bayes model had better sensitivity, which therefore can be used to predict AKI in sepsis patients.
In our study, the number of biomarker parameters used was more than in previous studies, so more accurate results are expected to predict AKI. The parameters used in machine learning are commonly found in various clinical settings, which means that the results of these parameters can be easily obtained, and the application of machine learning models will not be limited to parameters that are difficult to detect.20
In addition, many studies have conventionally examined one-parameter correlations to predict AKI in sepsis. However, few have incorporated it into a single prediction model and successfully measured its ability to predict AKI in sepsis patients.18 Machine learning has been widely applied to solve medical and clinical problems. For that reason, it has become a popular research topic. It is expected to predict better the prognosis in sepsis patients, one of which is the incidence of AKI.21 Even so, this study has a weakness, namely the number of samples used is less than in other studies.
Conclusion
Sepsis patients have high morbidity and mortality, and the risk is further increased by the occurrence of AKI (acute kidney injury). Several low molecular weight proteins detected in the serum of AKI patients are thought to be early biomarkers of AKI. These promising biomarkers include Cystatin C, Beta-2 Microglobulin (Β2MG), and Neutrophil Gelatinase-Associated Lipocalin (NGAL). This study’s SVM model of machine learning has higher AUC and specificity but low sensitivity. The Naïve Bayes model has better sensitivity, so it has the potential to be used to predict AKI in sepsis patients.
Acknowledgments
We would like to thank the Dean of the Medical Faculty of Universitas Brawijaya, the Director of Dr. Saiful Anwar Hospital, and all participants for supporting this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation; took part in drafting, revising, or reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received funding from the Medical Faculty of Universitas Brawijaya with grant number DPA-FK-271101/2023-0.
Disclosure
No potential conflict of interest.
References
1. Belsky JB, Wira CR, Jacob V, Sather JE, Lee PJ. A review of micronutrients in sepsis: the role of thiamine, l-carnitine, Vitamin C, selenium and Vitamin D. Nutr Res Rev. 2018;31(2):281–290. doi:10.1017/S0954422418000124
2. Odum JD, Wong HR, Stanski NL. A precision medicine approach to biomarker utilization in pediatric sepsis-associated acute kidney injury. Front Pediatr. 2021;9. doi:10.3389/fped.2021.632248
3. Acosta-Ochoa I, Bustamante-Munguira J, Mendiluce-Herrero A, Bustamante-Bustamante J, Coca-Rojo A. Impact on outcomes across KDIGO-2012 AKI criteria according to baseline renal function. J Clin Med. 2019;8(9). doi:10.3390/jcm8091323
4. Indonesian Renal Registry. 7th report of Indonesian Renal Registry; 2014. Available from: https://www.indonesianrenalregistry.org/data/INDONESIAN%20RENAL%20REGISTRY%202014.pdf.
5. Odum JD, Standage S, Alder M, Zingarelli B, Devarajan P, Wong HR. Candidate biomarkers for sepsis-associated acute kidney injury mechanistic studies. Shock. 2022;57(5):687–693. doi:10.1097/SHK.0000000000001916
6. Edelstein CL. Chapter Six - biomarkers in acute kidney injury. In: Edelstein CL, editor. Biomarkers of Kidney Disease.
7. Pei Y, Zhou G, Wang P, Shi F, Ma X, Zhu J. Serum cystatin C, kidney injury molecule-1, neutrophil gelatinase-associated lipocalin, klotho and fibroblast growth factor-23 in the early prediction of acute kidney injury associated with sepsis in a Chinese emergency cohort study. Eur J Med Res. 2022;27(1). doi:10.1186/s40001-022-00654-7
8. Linné E, Elfström A, Åkesson A, et al. Cystatin C and derived measures of renal function as risk factors for mortality and acute kidney injury in sepsis – a post-hoc analysis of the FINNAKI cohort. J Crit Care. 2022;72:154148. doi:10.1016/j.jcrc.2022.154148
9. Bian Z, Zhu R, Chen S. The predict value of serum/urocystatin C on acute kidney injury in elderly patients with sepsis. Exp Gerontol. 2021;155:111576. doi:10.1016/J.EXGER.2021.111576
10. Zhou H, Cui J, Lu Y, Sun J, Liu J. Meta-analysis of the diagnostic value of serum, plasma and urine neutrophil gelatinase-associated lipocalin for the detection of acute kidney injury in patients with sepsis. Exp Ther Med. 2021;21(4). doi:10.3892/etm.2021.9817
11. Xie Y, Huang P, Zhang J, et al. Biomarkers for the diagnosis of sepsis-associated acute kidney injury: systematic review and meta-analysis. Ann Palliat Med. 2021;10(4):4159–4173. doi:10.21037/apm-20-1855
12. Barton KT, Kakajiwala A, Dietzen DJ, Goss CW, Gu H, Dharnidharka VR. Using the newer Kidney Disease: improving global outcomes criteria, beta-2-microglobulin levels associate with severity of acute kidney injury. Clin Kidney J. 2018;11(6):797–802. doi:10.1093/ckj/sfy056
13. der Slikke EC V, Star BS, van Meurs M, Henning RH, Moser J, Bouma HR. Sepsis is associated with mitochondrial DNA damage and a reduced mitochondrial mass in the kidney of patients with sepsis-AKI. Crit Care. 2021;25(1). doi:10.1186/s13054-020-03424-1
14. Manrique-Caballero CL, Del Rio-Pertuz G, Gomez H. Sepsis-associated acute kidney injury. Crit Care Clin. 2021;37(2):279–301. doi:10.1016/j.ccc.2020.11.010
15. Baeyens JP, Serrien B, Goossens M, Clijsen R. Questioning the “SPIN and SNOUT” rule in clinical testing. Arch Physiother. 2019;9(1). doi:10.1186/s40945-019-0056-5
16. Luo XQ, Yan P, Zhang NY, et al. Machine learning for early discrimination between transient and persistent acute kidney injury in critically ill patients with sepsis. Sci Rep. 2021;11(1). doi:10.1038/s41598-021-99840-6
17. He J, Lin J, Duan M. Application of machine learning to predict acute kidney disease in patients with sepsis associated acute kidney injury. Front Med. 2021;8. doi:10.3389/fmed.2021.792974
18. Zhang L, Wang Z, Zhou Z, et al. Developing an ensemble machine learning model for early prediction of sepsis-associated acute kidney injury. iScience. 2022;25(9). doi:10.1016/j.isci.2022.104932
19. Wiersema R, Jukarainen S, Eck RJ, et al. Different applications of the KDIGO criteria for AKI lead to different incidences in critically ill patients: a post hoc analysis from the prospective observational SICS-II study. Crit Care. 2020;24(1). doi:10.1186/s13054-020-02886-7
20. Sukmark T, Lumlertgul N, Praditpornsilpa K, Tungsanga K, Eiam-Ong S, Srisawat N. Thai-ICU score as a simplified severity score for critically ill patients in a resource limited setting: result from SEA-AKI study group. J Crit Care. 2020;55:56–63. doi:10.1016/j.jcrc.2019.10.010
21. Yue S, Li S, Huang X, et al. Machine learning for the prediction of acute kidney injury in patients with sepsis. J Transl Med. 2022;20(1). doi:10.1186/s12967-022-03364-0
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
