Back to Journals » Clinical Optometry » Volume 15
Accuracy of the SRK/T Formula in Pediatric Cataract Surgery
Authors Irfani I , Wahyu T, Oktarima P , Caesarya S, Sari M, Karfiati F
Received 11 October 2022
Accepted for publication 22 December 2022
Published 4 January 2023 Volume 2023:15 Pages 1—8
DOI https://doi.org/10.2147/OPTO.S390994
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Mr Simon Berry
Irawati Irfani,1,2 Tri Wahyu,1 Primawita Oktarima,1,2 Sesy Caesarya,1,2 Maya Sari,1,2 Feti Karfiati1,2
1Department of Ophthalmology, Faculty of Medicine Universitas Padjadjaran, Bandung, West Java, Indonesia; 2Pediatric Ophthalmology & Strabismus Division, Cicendo National Eye Hospital, Bandung, West Java, Indonesia
Correspondence: Irawati Irfani, Email [email protected]
Purpose: Determining IOL power is an important step in achieving the desired postoperative refractive target, but this determination remains challenging, as currently the used formulas were developed using IOL power calculations derived from adults.
Patients and Methods: This is a retrospective analytical study with the period of June 2018 to May 2019. All of the data were taken from medical records in referral tertiary eye hospital in Indonesia. All type of cataracts underwent uncomplicated surgeries and in-the-bag IOL implantation were included in this study, while aphakia, secondary IOL implantation, primary sulcus implantation, and history of ocular disorders were excluded. The data were analyzed using Wilcoxon sign-rank, paired t, and Kruskal–Wallis tests.
Results: Sixty-seven patients (106 eyes) were found to meet the inclusion criteria, average age was 7.35 ± 4.61 years (1.00 to 17.00 years). Average targeted refraction was 1.69 ± 2.06 D (− 0.38–+6.99 D), and spherical equivalent (actual postoperative refraction) was − 0.90 ± 1.45 D (− 4.38 to +2.75 D). There was statistically significant difference between preoperative targeted refraction and actual postoperative refraction (p < 0.001). Mean absolute prediction error (APE) in general was 1.34 ± 1.18 D, 1.22 ± 0.88 D (in short eyes), 1.52 ± 1.37 D (in moderate eyes), and 0.69 ± 0.52 D (in long eyes) (p = 0.202). Mean APE in age group < 7 years old was 1.27 ± 1.18 D and ≥ 7 years-old was 1.42 ± 1.19 D (p = 0.429).
Conclusion: SRK/T formula is fairly accurate in calculating IOL power in pediatric cataract surgery. Mean APE in this study was within the range of accurate mean APE in pediatric patients despite differentiated axial length and age.
Keywords: absolute prediction error, SRK/T formula, pediatric cataract
Introduction
Cataract remains the leading cause of blindness in children, especially in the developing countries, and is responsible for visual impairment in estimated 19 million children worldwide.1,2 Pediatric cataract is considered congenital if it occurs from birth through the first year of life and developmental if it occurs after the first year of life; it can also occur due to trauma. Congenital cataract is associated with ocular abnormalities in 27% of cases and with systemic abnormalities in 22% of cases.3,4 Early diagnosis and prompt treatment are important to prevent deprivation amblyopia. Cataract extraction surgery followed by primary intraocular lens (IOL) implantation, in children aged one year or more, has been considered as a safe and effective procedure in children.1–3,5,6
Primary IOL implantation in the posterior chamber following cataract extraction is the standard of care for pediatric cataract and is commonly performed by pediatric ophthalmologists.1,3,7 Determining IOL power is an important step in achieving the desired postoperative refractive target, but this determination remains challenging, as currently the used formulas were developed using IOL power calculations derived from adults.8 Calculation of post-operative hyperopic refractive target based on the age is commonly used by surgeons, thus allowing the myopic-shift occurred along with the axial length growth.8,9
SRK/T formula has considered as an accurate formula in determining refractive target in many previous studies.1,7–9 The usage of SRK/T formula in pediatric cataract surgeries remains controversy up to date, even though many prior studies have compared the SRK/T formula with alternative formulas such as SRK-II, Hoffer Q, and Holladay 1. The results of these studies were highly variable and seemingly conflicting. Therefore, the present study was conducted to further investigate the accuracy of biometry calculations using the SRK/T formula in pediatric cataract surgery and to analyze the predictive refractive error based on axial lengths and age.
Materials and Methods
Study Design and Patient Cohort
This was a retrospective study from medical records during the period of June 2018 to May 2019 in the Pediatric Ophthalmology & Strabismus Division, Cicendo National Eye Hospital, Bandung, Indonesia. The study adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board (IRB) of the Cicendo National Eye Hospital. Patient informed consent was not required by the IRB, as the data were collected retrospectively, and patient data were de-identified to protect patient privacy. Inclusion criteria were all pediatric patients who underwent uncomplicated cataract surgery and primary IOL implantation with biometry calculations using the SRK/T formula. Exclusion criteria included aphakic patients or secondary IOL implantation, patients with previous history of ocular disorders (corneal or vitreous opacity, microcornea, uveitis, aniridia, glaucoma, persistent fetal vasculature, retinal detachment or retinopathies, maculopathies, optic neuropathies, microphthalmia), and history of prior ocular surgeries. Ciliary sulcus intraocular lens implantation was also excluded.
All patients underwent examination in the clinic, including visual acuity examination using the Snellen chart, Cardiff cards, cake decoration, toys, or pen light. Non-contact tonometry; autokeratorefractometry (TONOREFTM III; Nidek Co. Ltd., Japan); biomicroscopy and indirect funduscopy examination; and contact A-scan biometry (Biometer AL-100; Tomey, Germany) were performed in cooperative patients. The uncooperative patients were examined under general anesthesia prior surgery to obtain keratometry readings (Autokeratometry KM-500; Nidek Co. Ltd., Japan) and biometry parameters (Biometer AL-100).
Demographic data included age, sex, cataract type, and laterality. Biometry data included axial length, keratometry, A-constant, IOL power, and location of implantation. For analysis purpose, the eyes were also divided into the following subgroups depending on the axial length (AXL): short (≤22.0 mm), moderate (>22.0 mm and <24.5 mm); and long (≥24.5 mm).
Determination of Refractive Target
Refractive target was determined using two methods: (1) Enyedi’s Rule of Seven for children under 7 years (+7.00 D – age at time of surgery) and (2) plano for children above 7 years with bilateral cataract at the first visit or adjusted target according to the refractive error of the fellow eye (in case of unilateral cataract or pseudophakia).
Prediction of Refractive Error
Preoperative refractive error was examined with autorefractometry in cooperative patients with clear lens or IOL in the fellow eye (in cases of unilateral cataract). For uncooperative patients, streak retinoscopy was performed. Post-operative refractive error was examined with the same methods in the pseudophakic eye during follow-up visits. The final refractive error was that prescribed for corrective spectacles or contacts at the end of the study. Refractive error was then converted to spherical equivalent (SE).
Prediction error (PE) was calculated using this following formula: [prediction error = predicted refraction – actual postoperative refraction], and absolute prediction error (APE) was obtained by converting PE into an absolute value.
Surgical Procedures
All patients underwent irrigation-aspiration of cataract and primary IOL implantation under general anesthesia. Additional procedures, such as primary posterior capsulotomy and anterior vitrectomy were performed in patients under 5 years of age or considered to be uncooperative for Nd:Yag laser capsulotomy in the case of post-surgery visual axis opacification. Membranectomy was required in some certain cases, and synechiolysis was primarily performed in traumatic or complicated cataracts.
Irrigation-aspiration was performed according to standardized procedures. The lens mass was aspirated, and intraocular lens (IOL) was implanted in-the-bag with a foldable single-piece IOL (Neo Eye®; Rohto Laboratories Indonesia) or a foldable three-piece IOL (Sensar®, Johnson & Johnson Vision, Abbott Medical Optics). The incision wound was sutured using non-absorbable 10–0 nylon (Ethilon®, Ethicon, LLC).
All the procedures were performed by five experienced pediatric ophthalmology surgeons (FK, MS, II, PA, and SCA).
Follow-Up
Uncorrected visual acuity (UCVA) and best-corrected visual acuity (BCVA) were examined in 1 day, 1 week, and 1 month postoperatively using a Snellen chart, Cardiff cards, cake decoration, toys, or pen light. Refractive error was examined in the clinic and subsequently corrected using spectacles in 1 month postoperatively. Postoperative SEs were obtained from final spectacles prescription for the patients.
Data Processing and Statistics
Basic data were processed using Microsoft® Excel and analyzed with Statistical Package for the Social Sciences (SPSS) version 23.0 (IBM Corporation, New York, USA). A Wilcoxon sign-rank test was used to compare pre-operative versus post-operative vision categories; a paired t-test was used to compare targeted refraction vs actual refraction; and a Kruskal–Wallis test was used to compare mean APE among AXLs and age categories.
Results
During the period of June 2018 to May 2019, 67 patients (106 eyes) met the inclusion criteria. Mean patient age was 7.35 ± 4.61 years (1.00 to 17.00 years). Patients consisted of 36 boys (53.73%) and 31 girls (46.27%). Developmental cataract was the most common cataract type, found in 70 eyes (66.03%), followed by congenital cataract in 32 eyes (30.19%), traumatic cataract in two eyes (1.89%), and complicated cataract in two eyes (1.89%).
Most of the patients could be classified according to the Visual Impairment Classification of the World Health Organization (WHO), while toddlers and preschool-age children that did not understand the Snellen chart were categorized into fix and follow the light (FFTL) or the object (FFTO) or cake decoration. Table 1 shows the comparison of preoperative and postoperative UCVA. In preoperative examination, most of the patients presented a visual acuity of <6/18–6/60 (32 eyes, 30.19%), <3/60 (28 eyes, 26.42%), and fix and follow the object (20 eyes, 18.87%). One month postoperatively, visual acuities were improved. Postoperative examination showed that visual acuity of 6/18 increased to ≥6/12 in 18 eyes (16.98%) and <6/12–6/18 increased in 23 eyes (21.70%). The difference between pre- and postoperative UCVA was statistically significant.
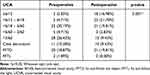 |
Table 1 Comparison of Preoperative and Postoperative UCVA and BCVA (n = 106 Eyes) |
Preoperative BCVA was not included in the study due to the variable cataract densities, so the refractive corrections in preoperative visits were therefore undetermined. Forty eyes (37.74%) achieved postoperative BCVA of ≥6/12 (Figure 1). Mean spherical power was −0.18 ±1.41 D (−3.25 to +3.50 D), mean cylindrical power was −1.45 ± 0.74 D (−0.50 to −3.50 D), and mean SE (or actual postoperative refraction) was −0.90 ± 1.45 D (−4.38 to +2.75 D).
Biometry revealed that mean AXL was 22.56 ± 1.57 mm (18.70 to 26.20 mm), and mean implanted IOL power was 20.31 ± 4.42 D (+10.00 to +30.00 D). Comparison of mean preoperative targeted refraction and actual postoperative refraction is shown in Table 2. Average targeted refraction and actual postoperative refraction were significantly different (p < 0.01). Comparison between preoperative targets and actual postoperative refraction results based on AXL and age was also significantly different (p < 0.01).
 |
Table 2 Comparison of Mean Targeted Refraction and Actual Refraction Postoperatively |
The accuracy of biometry calculation using the SRK/T formula was determined by average APE. Average APE in all groups was 1.34 ± 1.18 D (0.00–5.81 D). Average APE in short eyes was 1.22 ± 0.88 D, APE in moderate eyes was 1.52 ± 1.37 D, and APE in long eyes was 0.69 ± 0.52 D (Figure 2A; p = 0.202 using Kruskal–Wallis test). Average APE in patients <7 years was 1.27 ± 1.18 D, and average APE in patients ≥7 years was 1.42 ± 1.19 D (Figure 2B; p = 0.429 using Kruskal–Wallis test).
 |
Figure 2 Mean APE based on (A) AXL (short, moderate, long); and (B) age (<7 and ≥7 years of age). Abbreviations: APE, absolute prediction error; AXL, axial length. |
Discussion
The primary goal of cataract surgery, especially in children, is to minimize refractive predicted error. Measurement of postoperative refraction target is the main factor determining better visual acuity and decreasing likelihood of amblyopia. However, this measurement depends on several factors in pediatric cataract patients, including shorter AXL, use of devices calibrated and normalized for an adult population, formulas calculated using adult eyes, steeper curvature of the pediatric cornea, and shallow anterior chamber in pediatric patients.8,10,11 This might be the first study reporting the accuracy of the SRK/T formula in pediatric cataract surgery in Indonesian population. All the patients in this study underwent biometry examinations using contact A-scan biometry under general anesthesia, using the SRK/T formula. Trivedi et al and Ben-Zion et al reported that there was no significant difference in PE accuracy between immersion and contact A-scan biometry techniques.8,12 Even though accurateness of contact A-scan biometry technique could be decreased due to inadvertent indentation of the cornea by the ultrasound probe, thus shortening the measured AXL.8,9
Visual acuity measured one month postoperatively was significantly improved (p < 0.001). However, visual rehabilitation of these children was still not complete, even though 40 eyes (37.74%) gained postoperative visual acuity ≥6/12. Muppidi et al reported that 81% of pediatric cataract patients attained good visual outcome (6/12 Snellen equivalent or better), while Gogate et al reported 24.7% of eyes had visual acuity >6/18.13,14 Visual acuity results may be more accurate if measured 1–2 years postoperatively, as AXL and corneal curvature change over time in pediatric eyes.
Prediction error reflects the accuracy of postoperative targeted refraction measurement, which is an important indicator to evaluate outcomes of pediatric cataract surgery with primary IOL implantation. Average APE in the present study was 1.34 ± 1.18 D. This was within the range of accurate mean APE in pediatric patients that was reported by various studies, which ranged between 1.08 and 1.40.8,15–17 This accuracy range differs from that of adult cataract surgery, in which modern theoretical formulas are accurate within approximately 0.5 D. The present study revealed that mean APE in general was within the range reported in previous studies (1.34 D), although mean APE in moderate and long eyes was outside of the benchmark value (1.52 D and 0.69 D, respectively). Mean APE in long eyes could have been lower than the benchmark values because this group had the fewest eyes of the three groups, so the results might not have been as reliable.
The predictive formula has considered to be of vital importance for determining and calculating IOL power and postoperative refractive target. Various studies reported that the accuracies of numerous formulas (SRK/T, Holladay 1, Hoffer Q) were similar in predicting refractive error of pediatric cataract surgeries. In the present study, the SRK/T formula was applied to all the patients.1,7,9,10,18,19 O’Gallagher et al and Thanapaisal et al reported that SRK/T is more accurate than SRK-II, while Joshi et al reported that Hoffer Q is more sensitive.1,9
In-the-bag IOL implantation is the most recommended procedure in cataract surgery. However, in some cases, the IOL might be implanted in the ciliary sulcus, such as in cases of Zinni zonule rupture, posterior capsule rupture, or secondary IOL implantation. IOL power in the ciliary sulcus could require adjustment, decreasing by 0.5 D for 9≤17 D; 1.0 D for 17< IOL ≤28 D; and 1.50 D for power >28 D. The purpose of power adjustment is to achieve a similar PE to that of in-the-bag.20,21 The present study did not include ciliary sulcus IOL implantation to minimize the bias or IOL power maladjustment.
Based on the AXL measurements, we found significant differences between mean preoperative targeted refraction and actual postoperative refraction in the short AXL group (p ≤ 0.001), even though mean APE was within accuracy range (1.22 ± 0.88 D). Many studies have reported that a relatively large PE is common in short AXL, which is inconsistent with the results of the present study. Vasavada et al reported that the SRK/T formula had the least PE, even in eyes with AXL of <20 mm.7 Nihalani et al reported that Hoffer Q provided the best prediction most of the time in younger children and in eyes with short AXL.18 The long AXL group in the present study might not be reflective of the overall pediatric cataract population, as the number of the subjects in this subgroup was only 10 eyes. The Holladay and SRK/T formulas were recommended by the Infant Aphakia Treatment Study (IATS) for short AXL.22 O’Gallagher et al suggested that SRK/T was more accurate in predicting postoperative refraction in pediatric patients undergoing cataract surgery.9
The mean APE between two age subgroups was also not statistically different. This study had similar results with Kou et al, but their study divided the groups based on age ≤2 years, >2 and <5 years, and ≥5 years. Kou et al reported that SRK/T formula had smaller APE in each group (1.13 ± 1.27 D, 1.018 ± 0.70 D, and 0.80 ± 0.70 D respectively).23 The smallest APE was found in group ≥5 years, while the present study found that APE in group ≥7 years was higher (1.42 ± 1.19 D). Kou et al did not analyze the difference among these groups, but Chang et al reported that prediction errors were not significantly associated with different ages in most formulas, including SRK/T.23,24 Lee et al stated that age at IOL implantation has significant correlation with PE calculated by SRK/II, SRK/T, and Hoffer-Q formula.25 The discordance between the present study results and several previous studies can be attributed to age distribution.
In children less than 2 years of age, AXL and keratometry change rapidly as compared to age of more than 2-year-old. AXL, corneal curvature, and lens thickness change over time to maintain the eye in an emmetropic state. Therefore, there is an inevitable trend towards myopic shift after cataract surgery because of ongoing axial elongation. There is no IOL calculation formula specifically designed for pediatric eyes. In the present study, average APE among AXLs was not different statistically. Previous studies reported the APE on different AXLs, but each study had different AXL categories.7,16,24 The present study divided axial lengths into three subgroups and had the least APE in long eye subgroup even though this group had the fewest number of eyes. This study revealed average APE in short eyes (≤22.0 mm) was 1.22 ± 0.88 D, slightly higher than the study by Nihalani and VanderVeen (1.0 ± 0.8 D).16 Gupta et al reported greater absolute mean PE (2.09 ± 2.73) in shorter eyes (<22 mm), but their study focused only in children less than 2 years of age.26 The present study found that there is no statistically difference in mean APE among AXLs. Previous studies reported that age, AXL, and keratometry values did not influence predictive accuracy using SRK/T.7,24
The limitations of this study include the inherent limitations of its retrospective design, with potential confounding factors of bias, wide range of age at surgery, and short follow-up period. Variations in the techniques of optometrists, refractionists, or physicians that examined postoperative RE were not considered. The strength of this study is the large number of eyes, which were treated by multiple surgeons with varying degrees of experience.
Conclusion
Measurement of IOL power in pediatric cataract surgery to yield minimum APEs remains challenging. SRK/T formula is fairly accurate in calculating IOL power in pediatric cataract surgery. Mean APE in this study was within the range of accurate mean APE in pediatric patients, despite differentiated AXL and age.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Thanapaisal S, Wongwai P, Phanphruk W, Suwannaraj S. Accuracy of intraocular lens calculation by SRK/T formula in pediatric cataracts. J Med Assoc Thai. 2015;98(Suppl 7):S198–S203.
2. Lenhart DP, Courtright P, Wilson ME, et al. Global challenges in the management of congenital cataract: proceedings of the 4th International Congenital Cataract Symposium held on March 7, 2014, New York, New York. J AAPOS. 2015;19(2):1–8. doi:10.1016/j.jaapos.2015.01.013
3. Medsinge A, Nischal KK. Pediatric cataract: challenges and future directions. Clin Ophthalmol. 2015;9:77–90. doi:10.2147/OPTH.S59009
4. Khokhar SK, Pillay G, Dhull C, Esha A, Mahabir M, Aggarwal P. Pediatric cataract. Indian J Ophthalmol. 2017;65(12):1340–1349. doi:10.4103/ijo.IJO_1023_17
5. Nischal KK. Practice patterns in pediatric cataract management: time for real world data. Indian J Ophthalmol. 2017;65(9):779–781. doi:10.4103/ijo.IJO_816_17
6. Valera DA, Cornejo BAF. Relationship between preoperative axial length and myopic shift over 3 years after congenital cataract surgery with primary intraocular lens implantation at the National Institute of Ophthalmology of Peru, 2007–2011. Clin Ophthalmol. 2018;12:395–399. doi:10.2147/OPTH.S152560
7. Vasavada V, Shah SK, Vasavada VA, et al. Comparison of IOL power calculation formulae for pediatric eyes. Eye. 2016;30:1242–1250. doi:10.1038/eye.2016.171
8. Ben-Zion I, Neely DE, Plager DA, Ofner S, Sprunger DT, Roberts GJ. Accuracy of IOL calculations in children: a comparison of immersion versus contact A-scan biometery. J AAPOS. 2008;12(5):440–444. doi:10.1016/j.jaapos.2008.03.016
9. O’Gallagher MK, Lagan MA, Mulholland CP, Parker M, McGinnity G, McLoone EM. Pediatric intraocular lens implants: accuracy of lens power calculations. Eye. 2016;30:1215–1220. doi:10.1038/eye.2016.163
10. Joshi P, Mehta R, Ganesh S. Accuracy of intraocular lens power calculation in pediatric cataracts with less than a 20 mm axial length of the eye. Nepal J Ophthalmol. 2014;6(11):56–64. doi:10.3126/nepjoph.v6i1.10773
11. Al Shamrani M, Turkmani S. Update of intra-ocular lens implantation in children. Saudi J Ophthalmol. 2012;26:271–275. doi:10.1016/j.sjopt.2012.05.005
12. Trivedi RH, Wilson ME. Prediction error after pediatric cataract surgery with intraocular lens implantation: contact versus immersion A-scan biometry. J Cataract Refract Surg. 2011;37:501–505. doi:10.1016/j.jcrs.2010.09.023
13. Muppidi MR, Karanam S, Bevara A. A retrospective analysis of refractive changes in pediatric pseudophakia. Delhi J Ophthalmol. 2019;29:43–47. doi:10.7869/djo.417
14. Gogate P, Parbhoo D, Ramson P, et al. Surgery for sight: outcomes of congenital and developmental cataracts operated in Durban, South Africa. Eye. 2016;30:406–412. doi:10.1038/eye.2015.211
15. Moore DB, Zion IB, Neely DE, et al. Accuracy of biometry in pediatric cataract extraction with primary intraocular lens implantation. J Cataract Refract Surg. 2008;34:1940–1947. doi:10.1016/j.jcrs.2008.07.019
16. Nihalani BR, VanderVeen DK. Benchmarks for outcome indicators in pediatric cataract surgery. Eye. 2017;31:417–421. doi:10.1038/eye.2016.240
17. McClatchey SK. Choosing IOL power in pediatric cataract surgery. Int Ophthalmol Clin. 2010;50(4):115–123. doi:10.1097/IIO.0b013e3181f0f2e0
18. Indaram M, VanderVeen DK. Postoperative refractive errors following pediatric cataract extraction with intraocular lens implantation. Semin Ophthalmol. 2017;33:1–8.
19. Nihalani BR, Vanderveen DK. Comparison of intraocular lens power calculation formulae in pediatric eyes. Ophthalmology. 2010;177(8):1493–1499. doi:10.1016/j.ophtha.2009.12.031
20. Nakhli FR, Emarah K, Jeddawi L. Accuracy of formulae for secondary intraocular lens power calculations in pediatric aphakia. J Current Ophthalmol. 2017;29:199–203. doi:10.1016/j.joco.2017.05.007
21. Zhao Y, Gong X, Zhu X, et al. Long-term outcomes of ciliary sulcus versus capsular bag fixation of intraocular lenses in children: an ultrasound biomicroscopy study. PLoS One. 2017;12(3):1–13.
22. VanderVeen DK. The infant aphakia treatment study. Predictability of intraocular lens calculation and early refractive status. Arch Ophthalmol. 2012;130(3):293–299. doi:10.1001/archophthalmol.2011.358
23. Kou J, Chang P, Lin L, Li Z, Fu Y, Zhao Y. Comparison of the accuracy of IOL power calculation formulas for pediatric eyes in children of different ages. Hindawi J Ophthalmol. 2020;2020:1–6.
24. Chang P, Lin L, Li Z, Wang L, Huang J, Zhao Y. Accuracy of 8 intraocular lens power calculation formulas in pediatric cataract patients. Graefes Arch Clin Exp Ophthalmol. 2020;258:1123–1131. doi:10.1007/s00417-020-04617-8
25. Lee BJ, Lee SM, Kim HJ, Yu YS. Predictability of formulae for intraocular lens power calculation according to the age of implantation in paediatric cataract. Br J Ophthalmol. 2018;103:1–6.
26. Gupta R, Ganesh S, Singh C, Khurana AK. Prediction error after lens implantation in children with axial length less than 22 mm below 2 yrs. Del J Ophthalmol. 2016;26(4):250–255. doi:10.7869/djo.184
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

