Back to Journals » Neuropsychiatric Disease and Treatment » Volume 18
Working Conditions, Work Productivity, Quality of Life, and Depressive Symptoms in Undiagnosed Adults with and without Attention-Deficit/Hyperactivity Disorder (ADHD) Symptoms During the COVID-19 Pandemic
Authors Nakai T , Tsuji T , Tsuda H , Sotodate T, Namba Y, Uenishi T, Iwasaki K, Kokubo K, Tomita H
Received 18 February 2022
Accepted for publication 6 July 2022
Published 29 July 2022 Volume 2022:18 Pages 1561—1572
DOI https://doi.org/10.2147/NDT.S358085
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Taro Kishi
Toru Nakai,1,* Toshinaga Tsuji,1,* Hiroshi Tsuda,2– 5 Takuma Sotodate,5 Yuki Namba,1 Tatsuhiro Uenishi,6 Katsuhiko Iwasaki,6 Kinya Kokubo,7,8 Hiroaki Tomita9
1Medical Affairs Department, Shionogi & Co., Ltd, Osaka, Japan; 2Clinical Research, Innovation and Education Center, Tohoku University Hospital, Sendai, Japan; 3Department of Neurology, Faculty of Medicine, Juntendo University, Tokyo, Japan; 4Department of Neurology, Faculty of Medicine, Toho University, Tokyo, Japan; 5Japan Medical Office, Takeda Pharmaceutical Company Limited, Tokyo, Japan; 6Data Science Department, Medilead, Inc, Tokyo, Japan; 7Medilead, Inc, Tokyo, Japan; 8Department of International Business, Faculty of International Politics and Economics, Nishogakusha University, Tokyo, Japan; 9Department of Psychiatry, Graduate School of Medicine, Tohoku University, Sendai, Japan
*These authors contributed equally to this work
Correspondence: Toru Nakai, Medical Affairs Department, Shionogi & Co., Ltd, 4-7-6, Doshomachi, Chuo-ku, Osaka, 541-0045, Japan, Email [email protected]
Purpose: This study aims to evaluate the impact of the COVID-19 pandemic on employment status, work productivity, quality of life (QOL), and depressive symptoms in undiagnosed adults with and without attention-deficit/hyperactivity disorder (ADHD) symptoms in Japan.
Methods: An observational study used baseline data from a Japanese Medilead Healthcare Panel before the COVID-19 pandemic (October–December 2019). Eligible panel participants were then surveyed during the pandemic (March 2021). ADHD symptoms were screened using the Adult ADHD Self-Report Scale. Changes in QOL (EuroQol 5-Dimensions 5-Levels; EQ-5D-5L) and productivity impairment (Work Productivity and Activity Impairment scale; WPAI) from before to during the pandemic were analyzed in undiagnosed adults with and without ADHD symptoms. Unemployment rate and depressive symptoms (Patient Health Questionnaire; PHQ-9) during the pandemic were compared between groups.
Results: Participants with (N=949) and without (N=942) ADHD symptoms completed the survey. The unemployment rate was not significantly different between participants with and without ADHD symptoms. Participants with ADHD symptoms were more likely to change jobs or employers during the pandemic. PHQ-9 scores in participants with ADHD symptoms were significantly higher than in those without ADHD symptoms (8.96 vs 3.57, respectively) during the pandemic. Before the pandemic, WPAI scores were significantly higher and EQ-5D-5L scores lower in participants with ADHD symptoms than in those without. Productivity improved and QOL was not altered during the pandemic in both groups, but productivity and QOL remained poorer among participants with ADHD symptoms than in those without.
Conclusion: Productivity was improved among all participants during the COVID-19 pandemic, contrary to expectations. However, adults with ADHD symptoms consistently had lower productivity, poorer QOL, and more depressive symptoms than those without ADHD symptoms.
Keywords: absenteeism, ADHD symptoms, ASRS, COVID-19, depression, Japan, presenteeism, quality of life, working from home, work productivity
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a neurodevelopmental disorder with symptoms such as inattention, hyperactivity, and impulsivity that affect life disproportionately to age or development.1 Adults with ADHD often experience restlessness, impatience, distractibility, poor organization, forgetfulness, and an inability to track time.2 Adults with ADHD report greater difficulties with social functioning, relationships, self-organization and planning, personal finances, and mood control than adults without ADHD.3 Mental illnesses like depression and anxiety have substantial comorbidity with ADHD, which may increase burden and further reduce quality of life (QOL).4 Adults with ADHD also experience substantial impacts on work performance.2–4
The COVID-19 pandemic has forced people to undergo major changes in their lives, particularly in the work environment. In Japan, the first national COVID-19 state of emergency (SOE) was declared in April 2020 and lasted until late May 2020. Additional COVID-19 SOE declarations for specific cities and prefectures were issued in January, April, July, and August 2021. The COVID-19 SOE declarations placed restrictions on residents and businesses, including school closures, partial business closures, and the encouragement to stay home as much as possible, including working from home (WFH). Mental health impacts of the COVID-19 pandemic in Japan include anxiety-related and trauma-related disorders,5 psychological distress,6,7 depression,7,8 and suicide.9,10
Given the adverse impacts of the pandemic, people with ADHD are likely to experience various effects on QOL, mental health, and work productivity. To date, the impact of COVID-19 on people with ADHD has been primarily studied in children and adolescents, with most studies showing some negative behavioural and/or psychological outcomes during the pandemic.11–16 The impact of the pandemic on children with ADHD has also affected their interactions with adult caregivers.12 Similarly, the few studies on adults with ADHD during the pandemic have generally shown negative consequences, including stress, anxiety, poorer physical and psychological QOL, psychological distress, and financial decline.17–19 Other studies have shown minimal mental health impact of the pandemic in adults with ADHD who maintained their medication regimen.20 However, the full impact of the COVID-19 pandemic on adults with ADHD, especially in the work environment, has not been well elucidated. Furthermore, there are potentially many undiagnosed adults with ADHD symptoms in addition to the population with diagnosed ADHD. The estimated prevalence of Japanese adults diagnosed with ADHD is just 1.7%,21 lower than the worldwide prevalence of 3.4%,22,23 suggesting a large number of adults with undiagnosed ADHD in Japan.
Due to poor awareness of ADHD in Japanese society, the needs of people with ADHD symptoms are often not considered, and thus the working environment can be difficult for adults with ADHD symptoms. This observational web-based survey study aimed to evaluate work productivity, QOL, and mental health in undiagnosed Japanese adults with ADHD symptoms before and during the COVID-19 pandemic, using established assessment scales. Participants were people with (and without) ADHD symptoms who voluntarily reported that they were not diagnosed with ADHD. There were two primary objectives of this study. The first was to compare the unemployment rate and depressive symptoms during the COVID-19 pandemic between adults with and without ADHD symptoms. The second was to measure change from before to during the COVID-19 pandemic in work productivity and QOL in adults with and without ADHD symptoms. In addition, an exploratory objective was to evaluate the relationship between scores in the Adult ADHD Self-Report Scale (ASRS) v1.124 and work productivity, QOL, and depressive symptoms using post hoc analyses.
Materials and Methods
Study Design
This observational study utilised baseline data from a Medilead Healthcare Panel (MHP; Medilead, Inc.) collected before the COVID-19 pandemic, followed by targeted surveying of eligible panel participants. Survey 1 (before the COVID-19 pandemic; October–December 2019; baseline data) measured demographics, QOL, and work productivity. Survey 2 (during the COVID-19 pandemic; March 2021) included a screening phase (Survey 2, Part 1) and QOL, mental health, and work productivity questions (Survey 2, Part 2). This research complied with the principles of the Japanese Ethical Guidelines for Medical and Health Research Involving Human Subjects. Study approval was obtained from the MINS Research Ethics Committee (MINS-REC-210210, approved March 4, 2021). Informed consent was obtained from respondents using a web form at the beginning of the survey; all responses were anonymized.
Survey Variables and Measurement Scales
Survey 1 included demographics, a Japanese translation of the EuroQol 5-dimensions 5-levels (EQ-5D-5L) scale,25,26 and a Japanese translation of the Work Productivity and Activity Impairment (WPAI) scale.27 Survey 2, Part 1 included demographics, employment status, hospitalization status within the past year, and the ASRS. Employment status was categorized as regular or non-regular (part-time, dispatch, or short-term contract). Survey 2, Part 2 included the WPAI, the EQ-5D-5L, and the Japanese-language version of the Patient Health Questionnaire (PHQ-9) for depressive symptoms.28,29
All measurement scales used in this study are well established and validated in English.25,27,28 The Japanese-language version of the PHQ-9 has been validated,29 and Japanese population norms have been established for the EQ-5D-5L.26 High PHQ-9 scores indicate more depressive symptoms,28 and low EQ-5D-5L index scores indicate poor QOL.25 The WPAI survey is used to calculate four scores: absenteeism (percentage of time absent from work), presenteeism (percentage of time affected while at work), total work productivity impairment (absenteeism plus presenteeism), and total activity impairment (percentage of time affected outside the workplace). WPAI scores are reported as the percentage of time affected by participants’ disease/disorder, and a high impairment percentage indicates low productivity.27
Study Population
Participants from an MHP who responded to work productivity and QOL questions in Survey 1 and met selection criteria were targeted for Survey 2 (Supplementary Figure 1). Eligible participants were employed adults (≥20 years of age) with no history of ADHD diagnosis or hospital treatment for ADHD within the previous year. Diagnosed and/or treated ADHD patients were excluded because this study focused on undiagnosed adults with ADHD symptoms.
At the time of Survey 2, essential workers employed by medical institutions (hospital/clinic, pharmacy) were excluded because of potential bias if medically knowledgeable participants identified that the ASRS measured ADHD symptoms. Participants were categorized as adults with ADHD symptoms (ASRS-positive; ASRS Part A score ≥4) or without ADHD symptoms (ASRS-negative; ASRS Part A score <4). The target number of respondents with ADHD symptoms was set to 1000, as a practical, achievable number, and inclusion of respondents was stopped once this target was reached. Participants without ADHD symptoms were matched 1:1 to those with ADHD symptoms by sex, age, and occupation once the target number of participants with ADHD symptoms was reached. Participants in both groups completed Survey 2, Part 2.
Statistical Analysis
Baseline demographic and work characteristics were analyzed using chi-square (categorical variables) or Wilcoxon rank sum (continuous variables) tests. Chi-square tests were used to compare the work situations of adults with and without ADHD symptoms during the COVID-19 pandemic. Wilcoxon rank sum tests were used to compare WPAI and EQ-5D-5L index scores between those with and without ADHD symptoms across employment types (regular/non-regular) before and during the COVID-19 pandemic and PHQ-9 scores between groups across employment types during the pandemic.
Post hoc analyses of Survey 2 data were Kendall rank correlations of ASRS scores with each outcome variable, and linear regression analyses, with each outcome as the objective variable and ASRS score as the explanatory variable.
All analyses were conducted with R, version 4.0.2. Significance was assumed at the p<0.05 level. All statistical tests were two-sided.
Results
Demographic and Baseline Clinical Characteristics
Among 47,900 individuals who completed the ASRS questionnaire, 1126 were identified as having ADHD symptoms (Supplementary Figure 1). These individuals were matched by sex, age, and occupation to 1116 individuals without ADHD symptoms; 10 participants with ADHD symptoms could not be matched. Of these 2242 individuals, 1891 (949 with and 942 without ADHD symptoms) completed Survey 2, Part 2 (Figure 1). Participants were predominantly male (with ADHD symptoms 70.8%; without ADHD symptoms 71.5%) with a mean age of 46.7 years (Table 1). Participants with ADHD symptoms were more likely than those without to have ever been married (65.5% vs 60.7%, p=0.034) and to be university graduates (60.6% vs 54.8%, p=0.012), but less likely to be engaged in discretionary work (61.4% vs 68.2%, p=0.003). Annual income, days per week worked, and days worked from home were similar in participants with and without ADHD symptoms.
 |
Table 1 Baseline Demographic Data and Work Characteristics |
Employment Status
During the COVID-19 pandemic (Survey 2), 1.2% of participants with and 1.7% of participants without ADHD symptoms were unemployed (Table 2), with no significant difference between groups (p=0.427). However, the work situation of participants with ADHD symptoms during the COVID-19 pandemic was significantly different from that of participants without ADHD symptoms (p=0.039): more participants with ADHD symptoms than participants without ADHD symptoms were furloughed (“waiting at home” due to temporary business closures; 3.6% vs 2.8%) or had reduced working hours (12.2% vs 8.7%). Among participants who were unemployed, furloughed, or working reduced hours, 73.3% reported that this work situation was due to the COVID-19 pandemic, with no difference between those with and without ADHD symptoms.
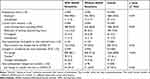 |
Table 2 Work Situation During the COVID-19 Pandemic |
Overall, 208 participants (11.2%) had changed employers or had a job transfer with the same employer since December 2019 (the end of Survey 1) (Table 2). More participants with than without ADHD symptoms changed employers or had a job transfer (6.4% vs 3.8% and 7.5% vs 4.6%, respectively; p<0.001). Of those who changed employers or had a job transfer, 35.4% of those with ADHD symptoms and 26.9% of those without ADHD symptoms reported that this was due to the COVID-19 pandemic; however, the difference between groups was not significant.
Depressive Symptoms
During the COVID-19 pandemic, depressive symptoms were greater in participants with ADHD symptoms than in participants without ADHD symptoms (Figure 2A; p<0.001). This pattern was observed both overall and within the employment subgroups. PHQ-9 scores were positively correlated with ASRS scores, suggesting there were more depressive symptoms in participants with more ADHD symptoms (Supplementary Figure 2A; p<0.001).
Longitudinal Changes in Work Productivity and QOL
All WPAI scores were lower during the COVID-19 pandemic than before the pandemic (Figure 2B), indicating improved productivity in work and daily life in participants both with and without ADHD symptoms. During the COVID-19 pandemic, all WPAI scores were significantly positively correlated with ASRS scores, which may indicate that people with more ADHD symptoms had lower productivity (Supplementary Figure 2B–E; p<0.001 for all correlations; Kendall rank correlation coefficients ~0.12–0.24 and r2 values ~0.01–0.08). The changes in WPAI scores between surveys were not different between participants with and without ADHD symptoms (Figure 2C). The data analyzed by employment type were consistent with this pattern: WPAI scores were significantly lower during the COVID-19 pandemic than before the pandemic in participants with and without ADHD symptoms in both regular and non-regular employment (Figure 3A), and the changes in WPAI scores were not different between participants with and without ADHD symptoms in both regular and non-regular employment (Figure 3B).
QOL scores were not affected by the COVID-19 pandemic. No differences in EQ-5D-5L scores were observed between surveys in participants with or without ADHD symptoms (Figure 2B), including when employment type was considered (Figure 3A).
Cross-Sectional Differences in Work Productivity and QOL
Both before and during the COVID-19 pandemic, participants with ADHD symptoms had significantly higher WPAI scores than participants without ADHD symptoms (Figure 2B, p<0.001 for all between-group comparisons), regardless of whether in regular employment or non-regular employment (Figure 3A, p<0.001 for all between-group comparisons except absenteeism during the pandemic in non-regular employment, for which p=0.023). Mean EQ-5D-5L scores were significantly lower in participants with ADHD symptoms than those without ADHD symptoms (Figure 2B, p<0.001), regardless of employment type (Figure 3A, p<0.001), indicating poorer QOL in the group with ADHD symptoms. EQ-5D-5L scores were weakly but significantly negatively correlated with ASRS scores (Supplementary Figure 2F; p<0.001; Kendall rank correlation coefficient −0.24, r2 value 0.07).
Discussion
This study describes work productivity, QOL, and mental health of Japanese adults without an ADHD diagnosis but with and without ADHD symptoms and the impact of changes in working conditions due to the COVID-19 pandemic. In many countries, the COVID-19 pandemic has been associated with substantial unemployment, accompanied by detrimental effects on mental health.9,30 In Japan, despite decreased employment during the COVID-19 pandemic,31 population unemployment was only 2.7% in March 2021, when Survey 2 was conducted.32 In this study, the unemployment rate was not different between undiagnosed participants with ADHD symptoms (1.2%) and participants without ADHD symptoms (1.7%). However, there was a significant difference between adults with and without ADHD symptoms with respect to overall changes in their work situation during the pandemic: more people with ADHD symptoms were working fewer hours or were furloughed. In addition, a greater percentage of participants with than without ADHD symptoms changed employers or transferred jobs during the pandemic. It has been suggested that individuals with ADHD experience internal restlessness and frustration that may lead to frequent job changes even in non-pandemic times,33 and it seems plausible that the COVID-19 pandemic may have exacerbated the existing employment instability of undiagnosed Japanese people with ADHD symptoms. Although these changes in jobs or employers may sometimes reflect increased success, the Japan Ministry of Health Labour and Welfare reported that “bad working conditions” and “unfavourable relationships in the workplace” are more common reasons to change jobs than career advancement among Japanese workers, based on the Employment Trend Survey conducted in 2018.34 The relationship between workplace social factors and job changes in Japanese adults with ADHD symptoms may need further investigation.
Undiagnosed adults with ADHD symptoms experienced more depressive symptoms during the COVID-19 pandemic than adults without ADHD symptoms. The highest mean PHQ-9 score (9.5) was in participants with ADHD symptoms in non-regular employment (Figure 2A), which was slightly lower than that (10.9) reported by British adults with diagnosed ADHD during the COVID-19 lockdown.20 Overall, PHQ-9 scores in adults with ADHD symptoms were in the mild to moderate range (~9–10), compared with the minimal range scores (<4) of participants without ADHD symptoms, indicating that adults with ADHD symptoms need mental health support. In an earlier study from the United States (US), undiagnosed adults with ADHD symptoms were more likely to have experienced depression in the previous 12 months than a matched cohort with diagnosed ADHD.35 The diagnosed cohort also experienced better QOL, work productivity, and self-esteem than the undiagnosed group.35 Possible interventions to improve mental health and workplace productivity in people with ADHD symptoms could include public health messaging promoting awareness of both adult ADHD and depression and collaboration between occupational physicians and psychiatrists to promote appropriate diagnosis and treatment of adult ADHD.
Before the COVID-19 pandemic, adults with ADHD symptoms had poorer productivity and work QOL than those without ADHD symptoms (Figure 2B), consistent with British and Japanese adults with diagnosed ADHD.2,4 For participants with ADHD symptoms, 16.9% of work time was lost to absenteeism before the COVID-19 pandemic, similar to the 17.8% reported in Japanese adults with diagnosed ADHD.4 The current cohort of people with ADHD symptoms had less presenteeism impairment (32.3%), total work impairment (41.7%), and total activity impairment (32.8%) than Japanese adults with diagnosed ADHD (58.2%, 64.7%, and 59.2%, respectively).4 The lower impairment scores in the current study may reflect the fact that our study targeted adults with ADHD symptoms who had not been diagnosed with ADHD; therefore, adults with more severe ADHD symptoms may have been excluded from the study. However, in US adults with ADHD symptoms, although absenteeism scores were similar (16.7%), impairment scores were higher than in the present study (44.5%, 49.2%, and 53.0% for presenteeism, total work impairment, and total activity impairment, respectively).35 In the current study, before the COVID-19 pandemic, EQ-5D-5L index scores were 0.80 and 0.89 in participants with and without ADHD symptoms, respectively, consistent with 0.74 for adults with diagnosed ADHD in the UK and the UK population norm of 0.86.2 However, US adults with ADHD symptoms had a lower average EQ-5D-5L index score of 0.70.35 Of note, baseline characteristics differed between the two studies, including age, sex, race, highest educational level, and socioeconomic factors. In addition, the definition of adults with ADHD symptoms differs between this study (ASRS Part A score ≥4) and the US study (ASRS score ≥5 among either the 9 inattentive symptoms or 9 hyperactive/impulsive symptoms),36 which may have contributed to differences in WPAI and QOL results.
In the current study, regardless of employment type (regular or non-regular), productivity improved during the COVID-19 pandemic and QOL was unaffected in adults with ADHD symptoms (Figure 3A). Improvement in productivity during the pandemic was unexpected. However, it is consistent with qualitative descriptions of the impact of the first SOE period on four Japanese adults with diagnosed ADHD, in which all interviewees used at least some productivity-based language (eg, “effortless time management”, “successful assignment”, “my own pace”) to describe positive aspects of working during the pandemic.37 In a survey of Japanese workers generally (ie, not specifically those with diagnosed ADHD or ADHD symptoms) later in the pandemic (November–December 2020), many found it easier to concentrate at work and to refresh after work when WFH than when working in an office.38 Therefore, improved productivity during the pandemic in our study may have been influenced by WFH. Productivity also increased in people without ADHD symptoms, with no difference in the change in productivity between those with and without ADHD symptoms (Figures 2C, 3B). Thus, adults with ADHD symptoms still experienced substantial work-related burdens during the pandemic.
In the current study, people with ADHD symptoms showed some demographic features (eg, education level and marital status) different from previous studies of adults diagnosed with ADHD.4,39 One possible reason is that because people with a confirmed diagnosis of ADHD were excluded, the ASRS-positive group may have included an overrepresentation of people with high scores for ADHD symptoms but low functional impairment. If this is the case, then it is possible that people diagnosed with ADHD, who presumably have greater functional impairment, may have been more affected by the pandemic than the results of our study suggest.
When analyzed as a continuous variable, ASRS scores significantly correlated with WPAI productivity scores, QOL, and PHQ-9 (Supplementary Figure 2). However, the associations between ASRS and QOL and between ASRS and WPAI scores were relatively weak, with low correlation coefficients and small r2 values. By contrast, the relationship between ASRS and PHQ-9 scores was stronger, with a Kendall rank correlation coefficient of 0.353 and an r2 of 0.194; this was consistent with the reported correlation between the Beck Depression Inventory scale and the ASRS.40 Correlations between ASRS scores and depression scales suggest physicians could potentially start supporting adults with ADHD symptoms earlier by paying attention to their scores in other clinical scales, such as the PHQ-9, and considering whether adult ADHD may be contributing to higher depression scale scores.
The COVID-19 pandemic offered a unique opportunity to study how changes in working conditions affect people with and without ADHD symptoms. To our knowledge, this was the first study to investigate the impact of the pandemic on the work and mental health domains of undiagnosed Japanese adults with self-reported ADHD symptoms. While this study was characterized by strengths, including the large sample size and the use of well-established scales for work productivity, depressive symptoms, and QOL, there were also several limitations. Because a web-based panel was used to recruit participants, there was a selection bias toward people with access to computers and smartphones; the panel members may also have had higher health awareness than the general Japanese population. Furthermore, survey questions relating to past events may have been subject to recall bias. The analysis included multiple comparisons without multiplicity adjustments, leading to the possibility of type 1 errors. The study did not exclude the possibility that comorbidities with ADHD symptoms may have contributed to measured outcomes. For example, symptoms of inattention and hyperactivity measured by the ASRS may be associated with untreated depression, insomnia, and other disorders, which may have been exacerbated or newly experienced during the COVID-19 pandemic. Thus, the burdens discussed in this article may have been influenced by other disorders. However, the data still provide insights into the pandemic’s impact on people who experienced inattention or hyperactivity symptoms during this time. Finally, the study design included only one survey during the COVID-19 pandemic. Additional surveys in other phases of the COVID-19 pandemic might have provided additional insights into how adults with ADHD symptoms adjust to a changed working situation.
Conclusions
In conclusion, undiagnosed Japanese adults with ADHD symptoms were more likely than those without ADHD symptoms to be furloughed or have reduced working hours. Although there was no difference in unemployment rates between people with and without ADHD symptoms, those with ADHD symptoms were more likely to change employers or transfer jobs during the COVID-19 pandemic. Adults with ADHD symptoms had lower work productivity, poorer QOL, and more depressive symptoms than adults without ADHD symptoms, both before and during the COVID-19 pandemic. Adults with and without ADHD symptoms improved their work productivity and had no change in QOL during the pandemic, but adults with ADHD symptoms continued to experience more work-related burdens during the pandemic. The results of this study suggest that people with ADHD symptoms potentially require additional support to reduce their work-related burdens.
Abbreviations
ADHD, attention-deficit/hyperactivity disorder; ASRS, Adult ADHD Self-Report Scale; EQ-5D-5L, EuroQol 5-Dimensions 5-Levels; MHP, Medilead Healthcare Panel; PHQ-9, Patient Health Questionnaire; QOL, quality of life; SOE, state of emergency; WFH, working from home; WPAI, Work Productivity and Activity Impairment.
Data Sharing Statement
Deidentified participant data collected during the current study are available from the corresponding author upon reasonable request.
Acknowledgments
The authors would like to thank all study participants. Medical writing assistance was provided by Koa Webster, PhD, and Rebecca Lew, PhD, CMPP, of ProScribe – Envision Pharma Group, and was funded by Shionogi & Co., Ltd. and Takeda Pharmaceutical Company Limited. ProScribe’s services complied with international guidelines for Good Publication Practice (GPP3).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was sponsored by Shionogi & Co., Ltd. and Takeda Pharmaceutical Company Limited. Shionogi & Co., Ltd. and Takeda Pharmaceutical Company Limited were involved in the study design, data collection, data analysis, and preparation of the manuscript. Medilead, Inc. was involved in the data collection.
Disclosure
TN and YN are employees of Shionogi & Co., Ltd. and own shares in the company. TT was an employee of Shionogi & Co., Ltd. at the time the study was conducted and owns shares in both Shionogi & Co., Ltd. and Takeda Pharmaceutical Company Limited. HTs is a former employee of Takeda Pharmaceutical Company Limited. TS is an employee of and owns shares in Takeda Pharmaceutical Company Limited. TU and KI are employees of Medilead, Inc, which received payment for study design and data analysis from Shionogi & Co., Ltd. KK sits on the board of directors of Medilead, Inc. HTo reports grant funding (paid to Tohoku University) from Daiichi Sankyo Company, Limited, Eisai Co., Ltd., Otsuka Pharmaceutical Co., Ltd., and Sumitomo Dainippon Pharma Co., Ltd.; and has also received personal payment or honoraria from Daiichi Sankyo Company, Limited, EA Pharma Co., Ltd., Eisai Co., Ltd., Janssen Pharmaceutical K.K., Lundbeck, Meiji Seika Pharma Co., Ltd., Mochida Pharmaceutical Co., Ltd., MSD K.K., Mylan EPD G.K., Otsuka Pharmaceutical Co., Ltd., Pfizer Japan Inc., Sumitomo Dainippon Pharma Co., Ltd., Takeda Pharmaceutical Company Limited, and Viatris Inc. The authors report no other conflicts of interest in this work.
References
1. American Psychiatric Association, DSM-5 Task Force. Diagnostic and Statistical Manual of Mental Disorders: DSM-5™.
2. Joseph A, Kosmas CE, Patel C, Doll H, Asherson P. Health-related quality of life and work productivity of adults with ADHD: a U.K. web-based cross-sectional survey. J Atten Disord. 2019;23(13):1610–1623.
3. Pitts M, Mangle L, Asherson P. Impairments, diagnosis and treatments associated with attention-deficit/hyperactivity disorder (ADHD) in UK adults: results from the lifetime impairment survey. Arch Psychiatr Nurs. 2015;29(1):56–63.
4. Kirino E, Imagawa H, Goto T, Montgomery W. Sociodemographics, comorbidities, healthcare utilization and work productivity in Japanese patients with adult ADHD. PLoS One. 2015;10(7):e0132233.
5. Shigemura J, Kurosawa M. Mental health impact of the COVID-19 pandemic in Japan. Psychol Trauma. 2020;12(5):478–479.
6. Nagasu M, Muto K, Yamamoto I. Impacts of anxiety and socioeconomic factors on mental health in the early phases of the COVID-19 pandemic in the general population in Japan: a web-based survey. PLoS One. 2021;16(3):e0247705.
7. Yamamoto T, Uchiumi C, Suzuki N, Yoshimoto J, Murillo-Rodriguez E. The psychological impact of ‘mild lockdown’ in Japan during the COVID-19 pandemic: a nationwide survey under a declared state of emergency. Int J Environ Res Public Health. 2020;17(24):9382.
8. Ueda M, Stickley A, Sueki H, Matsubayashi T. Mental health status of the general population in Japan during the COVID-19 pandemic. Psychiatry Clin Neurosci. 2020;74(9):505–506.
9. Nomura S, Kawashima T, Yoneoka D, et al. Trends in suicide in Japan by gender during the COVID-19 pandemic, up to September 2020. Psychiatry Res. 2021;295:113622.
10. Ueda M, Nordström R, Matsubayashi T. Suicide and mental health during the COVID-19 pandemic in Japan. J Public Health. 2021;1:548.
11. Zhang J, Shuai L, Yu H, et al. Acute stress, behavioural symptoms and mood states among school-age children with attention-deficit/hyperactive disorder during the COVID-19 outbreak. Asian J Psychiatr. 2020;51:102077.
12. Shah R, Raju VV, Sharma A, Grover S. Impact of COVID-19 and lockdown on children with ADHD and their families—an online survey and a continuity care model. J Neurosci Rural Pract. 2021;12(1):71–79.
13. Melegari MG, Giallonardo M, Sacco R, Marcucci L, Orecchio S, Bruni O. Identifying the impact of the confinement of Covid-19 on emotional-mood and behavioural dimensions in children and adolescents with attention deficit hyperactivity disorder (ADHD). Psychiatry Res. 2021;296:113692.
14. Bobo E, Lin L, Acquaviva E, et al. Comment les enfants et adolescents avec le trouble déficit d’attention/hyperactivité (TDAH) vivent-ils le confinement durant la pandémie COVID-19? [How do children and adolescents with Attention Deficit Hyperactivity Disorder (ADHD) experience lockdown during the COVID-19 outbreak?]. L’Encéphale. 2020;46(Supplement 3):S85–92.
15. Breaux R, Dvorsky MR, Marsh NP, et al. Prospective impact of COVID-19 on mental health functioning in adolescents with and without ADHD: protective role of emotion regulation abilities. J Child Psychol Psychiatry. 2021;62:1132–1139.
16. Behrmann JT, Blaabjerg J, Jordansen J. Jensen de López KM. Systematic review: investigating the impact of COVID-19 on mental health outcomes of individuals with ADHD. J Atten Disord. 2022;26(7):959–975.
17. Hollingdale J, Adamo N, Tierney K. Impact of COVID-19 for people living and working with ADHD: a brief review of the literature. AIMS Public Health. 2021;8(4):581–597.
18. Engel-Yeger B. Emotional status and quality of life in women with ADHD during COVID-19. OTJR (Thorofare N J). 2022. doi:10.1177/15394492221076516
19. Pollak Y, Shoham R, Dayan H, Gabrieli-Seri O, Berger I. Symptoms of ADHD predict lower adaptation to the COVID-19 outbreak: financial decline, low adherence to preventive measures, psychological distress, and illness-related negative perceptions. J Atten Disord. 2022;26(5):735–746.
20. Adamou M, Fullen T, Galab N, et al. Psychological effects of the COVID-19 imposed lockdown on adults with attention deficit/hyperactivity disorder: cross-sectional survey study. JMIR Form Res. 2020;4(12):e24430.
21. Nakamura S, Ohnishi M, Uchiyama S. Epidemiological survey of adult attention deficit hyperactivity disorder (ADHD) in Japan. Jpn J Psychiatr Treat. 2013;28:155–162.
22. Fayyad J, De Graaf R, Kessler R, et al. Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Br J Psychiatry. 2007;190:402–409.
23. Corominas-Roso M, Palomar G, Ferrer R, et al. Cortisol response to stress in adults with attention deficit hyperactivity disorder. Int J Neuropsychopharmacol. 2015;18(9):pyv027.
24. Kessler RC, Adler L, Ames M, et al. The World Health Organization adult ADHD self-report scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35(2):245–256.
25. Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727–1736.
26. Shiroiwa T, Fukuda T, Ikeda S, et al. Japanese population norms for preference-based measures: EQ-5D-3L, EQ-5D-5L, and SF-6D. Qual Life Res. 2016;25(3):707–719.
27. Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. PharmacoEconomics. 1993;4(5):353–365.
28. Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613.
29. Muramatsu K, Kamijima K, Yoshida M, et al. The patient health questionnaire, Japanese version: validity according to the mini-international neuropsychiatric interview-plus. Psychol Rep. 2007;101(3 Pt 1):952–960.
30. Kawohl W, Nordt C. COVID-19, unemployment, and suicide. Lancet Psychiatry. 2020;7(5):389–390.
31. Fukai T, Ichimura H, Kawata K. Describing the impacts of COVID-19 on the labor market in Japan until June 2020. Jpn Econ Rev. 2021;72(3):439–470.
32. Statistics Bureau of Japan. Tokyo: Labour Force Survey; 2021. Available from: https://www.stat.go.jp/english/data/roudou/index.html.
33. Montano B. Diagnosis and treatment of ADHD in adults in primary care. J Clin Psychiatry. 2004;65:18–21.
34. Japan Ministry of Health Labour and Welfare. Overview of 2018 Employment Trend Survey Results. https://www.mhlw.go.jp/toukei/itiran/roudou/koyou/doukou/19-2/dl/gaikyou.pdf2018.
35. Pawaskar M, Fridman M, Grebla R, Madhoo M. Comparison of quality of life, productivity, functioning and self-esteem in adults diagnosed with ADHD and with symptomatic ADHD. J Atten Disord. 2020;24(1):136–144.
36. Cossrow N, Pawaskar M, Witt EA, et al. Estimating the prevalence of binge eating disorder in a community sample from the United States: comparing DSM-IV-TR and DSM-5 criteria. J Clin Psychiatry. 2016;77(8):e968–974.
37. Ando M, Takeda T, Kumagai K. A qualitative study of impacts of the COVID-19 pandemic on lives in adults with attention deficit hyperactive disorder in Japan. Int J Environ Res Public Health. 2021;18(4):2090.
38. Umishio W, Kagi N, Asaoka R, Hayashi M, Sawachi T, Ueno T. Work productivity in the office and at home during the COVID-19 pandemic: a cross-sectional analysis of office workers in Japan. Indoor Air. 2021.
39. Kuriyan AB, Pelham WE, Molina BS, et al. Young adult educational and vocational outcomes of children diagnosed with ADHD. J Abnorm Child Psychol. 2013;41(1):27–41.
40. Ishizuka K, Ishiguro T, Nomura N, Inada T. Depressive mood changes are associated with self-perceptions of ADHD characteristics in adults. Psychiatry Res. 2021;300:113893.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



