Back to Journals » International Journal of Women's Health » Volume 15
Women’s Involvement in Decision-Making and Associated Factors Among Women Who Underwent a Caesarean Section in Sidama Region, South Ethiopia: Cross-Sectional Study
Authors Getu Wondimu M , Dadhi AE, Gesisa HI, Feyisa GT , Yohannes Kassa Z
Received 26 November 2022
Accepted for publication 5 May 2023
Published 25 May 2023 Volume 2023:15 Pages 813—824
DOI https://doi.org/10.2147/IJWH.S399261
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Melkamu Getu Wondimu,1,2 Aberash Eifa Dadhi,1 Hana Israel Gesisa,2 Gizu Tola Feyisa,3 Zemenu Yohannes Kassa1,4
1Department of Midwifery, Hawassa University, Hawassa, Ethiopia; 2Department of Midwifery, Jimma University, Jimma, Ethiopia; 3Department of Midwifery, Metu University, Metu, Ethiopia; 4Centre for Midwifery, University of Technology Sydney, Sydney, Australia
Correspondence: Melkamu Getu Wondimu, Email [email protected]
Background: A caesarean delivery without maternal involvement in decision-making reduces the quality of health care and breaks women’s autonomy. However, the involvement of women in decision-making to have a caesarean delivery is minimal. Still, now paternalism is widely practised. The study aims to assess women’s involvement in decision-making and associated factors among women who underwent a caesarean delivery.
Methods: Institutional-based cross-sectional study was conducted in Sidama region Public hospitals from June 22/2022-August 5/2022, among women who underwent a caesarean delivery. The total sample size was 457. The collected data was exported from the ODK toolbox server to excel and then to SPSS version 26 for further data cleaning and analysis. The variables with a p-value ≤ 0.25 in the bivariable analysis were included in a multivariable ordinal logistic regression model to control possible confounders. The resulting odds ratio and 95% confidence interval were computed, and a p-value of less than 0.05 is considered statistically significant.
Results: Women’s agreed decision-making involvement to have a caesarean delivery is 165(37.9%). Women who had an scheduled caesarean delivery [AOR: 7.6; 95% CI: 3.3, 17.8], had adequate information about caesarean delivery [AOR: 5.7; 95% CI:3.3, 10.0], had adequate time for decision-making [AOR: 4.6; 95% CI:2.09, 6.4], language of consent [AOR: 1.9; 95% CI: 1.2, 3.1], and women-healthcare providers relationship [AOR: 5.2; 95% CI: 3.2, 8.6]are higher odds of being involved in decision-making, but women’s being primary school [AOR: 0.53; 95% CI: 0.3,0.97] are lower odds of involvement in decision-making to have a caesarean delivery.
Conclusion and recommendation: In this study, women’s agreed decision-making involvement to have a caesarean delivery is low compared with other studies. Women-healthcare providers’ relationship and an unscheduled caesarean delivery are highly affect their involvement in decision-making. Therefore, hospitals should translate and prepare the consent form in an understandable way for women and families, and healthcare providers should develop good relationship and encourage her involvement.
Keywords: caesarean delivery, women’s involvement, mode of decision-making, shared decision-making
Background
Caesarean delivery is a surgical procedure performed on mothers for obstetrics reasons for those unable to have vaginal childbirth.1 Now a day it is widely increased invasive obstetrics procedures for the birth of fetuses worldwide.2 However, a caesarean section performed without medical or obstetrics necessity can put women at risk of immediate and long-term health problems.3 The caesarean delivery might be scheduled or unscheduled, requiring urgent decision-making by the people involved, including the health care providers, the woman, and her family.4
There are three modes of decision-making: paternalistic, informed decision-making, and shared decision-making.5 The paternalistic decision-making style involves a one-way communication of the minimum amount of medical information required for informed consent (from the healthcare provider to the patient), and the choice is made solely by the healthcare provider.6
In the informed decision-making model, all medical information required for decision-making is transferred in one direction (from healthcare practitioners to patients), and the patient makes those decisions alone.7 Also, the shared decision-making approach represents a sharing and negotiation of treatment decisions between patients and healthcare professionals.8
Shared decision-making reflects the ethical principle that patients have the right make their own decisions about what is appropriate for them, taking into consideration their circumstances, beliefs, and priorities.9 It includes the freedom to accept or refuse certain health care offers and change that decision.10 For a patient to exercise this right to decide, they require the information that is relevant to them.11
Furthermore, searching for information regarding the procedure is one-way women are involved in decision-making.12 Health care providers must give appropriate information to the patient that they need to know and understand.13 This information may include the type of procedure, indication, options, risks, benefits, complications, alternatives, and outcomes, which may include the decision to do nothing.12 Involvement in decision-making has been linked to efficacy, empowerment, and autonomy.8,14 When decision sharing is evident, patients and healthcare providers will have improved connections and interactions.15 In addition, this compliance will be improved.13 Also, enhance satisfaction,4 and quality of care.7,16
However, caesarean delivery without involving women in decision-making compromise trust between health care providers and women.4 In addition, it breaks women’s autonomy (the right to accept and refuse),17 and women can feel disempowered. Also, they may be unable to achieve health goals and inability to recover.18 The studies show that the involvement of women in decision-making to have a caesarean delivery is minimal and it ranges from (23%)-(to 95%).1,19 A study in Ghana states that women in underdeveloped nations who make health-related decisions are not autonomous.20
According to American College of Obstetricians and Gynecologists committee of ethics, every woman should be involved in decision-making during the procedure, and the patient has the autonomy to have or not have a surgical procedure.21 In addition, the newly revised guideline on obstetric management in Ethiopian 2020 recommends that every pregnant woman has the right to receive adequate information about her health, be involved in the decision for any procedure, and express her opinions about the services that she received.10 But clients’ involvement in decision-making was not widely practised in most developing countries, including sub-Saharan Africa. It had not integrated the concept of patient-centred care into health systems.5,22,23 Still, paternalism is now widely practised in developing countries.5,6
Though it is limited, adequate evidence is very important for women’s, healthcare providers, hospitals and other concerned bodies to improve the quality of care, respect the autonomy (the right to accept or refuse) of women and increase cooperation of women’s during the procedure. So, this study was designed to assess women’s involvement in decision-making and associated factors among women who underwent a caesarean delivery in Sidama region Public hospitals.
Methods
Study Design and Settings
A hospital-based cross-sectional study was done in the Sidama region from June 22 to August 5, 2022, among a woman who underwent a caesarean delivery in Public hospitals. Sidama National Regional state is one of eleven regions in Ethiopia, and its administrative city is Hawassa, located 273 kilometers away from Addis Ababa, the country’s capital city. The region is bordered in northern and east by the Oromia region and south and west by the Oromia and south region. According to the 2007 Ethiopia central statics agency report estimation, the region’s total population was 4,369,214. According to the regional health bureau report of 2022, the region has a tertiary hospital, five general hospitals, and fourteen primary hospitals. Tertiary and all general hospitals provided caesarean delivery. Also, of fourteen primary hospitals, eleven fully provided caesarean delivery. The 2022 health bureau nine months report showed that 5239 caesarean sections were done.
Population
All selected women who underwent a caesarean delivery at selected hospitals during the study were included. However, women referred for better management before exiting the post-caesarean ward were excluded.
Sample Size and Sampling Procedure
The sample size was determined using the single population proportion formula by considering a 25.3% proportion (P) which was taken from research done at Jimma university,5 with a 95% confidence interval (1.96), α=0.05, and 5% margin of error. Considering 1.5 design effects and a 5% possible non-response rate, the final sample size was 457.
Two-stage sampling technique was employed. There were one comprehensive specialised teaching hospital, five general and fourteen primary hospitals in the Sidama region. Of fourteen primary hospitals, only eleven hospitals were fully functional to provide a caesarean section. Forty percent of general and primary hospitals and one comprehensive specialized teaching hospital were selected using simple random sampling. Each hospital was given a proportional share of the required sample size based on the number of women they served in one and a half months (45 days). Finally, the study participants were selected using a simple random sampling technique.
Operational Definitions
Women’s Involvement in Decision-Making
Refers involvement of the women’s/patients in decision-making or expressing opinions about different treatment methods, which include sharing information, feelings, and signs and accepting health team instructions. Shared decision-making question nine (SDMQ9) contains nine items. The nine-item of SDMQ, a 5-point Likert scale, was recorded into agreeing, neutral, and disagree. Those whose response was “agree” were considered as women adequately involved in decision-making, and those whose response was “disagree” were not adequately engaged in decision-making. Those whose response was “neutral” were neither involved nor not involved in decision-making.8,24–26
Patient-Doctor/Healthcare Providers Relationship
Refers to the perception of the patient concerning the caring shown by the healthcare providers and the attitude and behaviour of the healthcare providers towards the patient. The patient-doctor relationship questionnaire (PDRQ) contains nine items with a yes/no option. When the patients answered greater than seven7 items with a yes response, it was considered good PDR, and below seven,7 it was regarded as poor PDR.27
Data Collection Tools and Procedure
After reviewing relevant literature from previous related studies and other adopted standardised materials/tools,8,19,20,25,27 the questionnaire was prepared in English and translated to Sidaamu Afoo by language experts. The questionnaire was administered with Sidaamu Afoo to facilitate understanding. The questionnaire contains socio-demographic characteristics, obstetrics factors, SDMQ-9, service-related factors, and patient-to-healthcare provider relationships.
Trained seven-degree midwives collected the data. The trained data collectors preceded face-to-face interview techniques with those women who were willing to participate in the study during the participants post a caesarean ward at the exit time. The interviewer-administered and a chart review technique were used. The study participants were encouraged to fill out the questionnaire with the help of data collectors by reading and explaining the question in easy-to-understand language. Two supervisors were trained to supervise the data collection process closely. The principal investigator oversaw the entire data collection process and worked closely with the supervisors.
Data Quality Assurance
A properly designed data collection instrument was developed and pretested before the actual data collection period in a comparable setting in Yirgalem General Hospital on 5% (23 cases) of the calculated sample size to check whether the questioner were simple, clear and easily understandable. Based on the pretest, some necessary modifications were made before the actual accordingly. One day of training was given to data collectors and supervisors concerning data collection processes and handling. Close supervision was done regularly by the supervisors and the principal investigator. Every day the collected data was reviewed and checked for completeness and consistency by the principal investigator. Problems encountered were reported to supervisors and the principal investigator for immediate action.
Data Processing and Analysis
The collected data were checked, reviewed for completeness, and exported from the ODK toolbox server to excel and then to SPSS version 26 for analysis. Cross-tabulation was done to explore data, clean missing values, and determine the expected count per cell. Descriptive statistics were generated to describe the findings. Then bivariable and multivariable ordinal logistic regression analysis were fitted to identify factors associated with women involvement in decision-making. Before fitting the ordinal logistic regression model, the normality of continuous data was checked by plotting histogram. And the assumption of multicollineartity was checked by variance inflation factor (VIF) and tolerance test (VIF=2.14). The model fitness was checked by Goodness-of-fit of overall model (Pearson (p-value=0.109) and (deviance (p-value=1.000)), Nagelkerke’s (p-vale=0.628) and Test of Parallel Lines (p-value=0.299). The variables found with their p-value ≤ 0.25 in bivariabele ordinal regression analysis were fitted into the multivariable ordinal logistic regression model. Adjusted odds ratio (AOR) at a 95% confidence interval (CI) was used to indicate the degree to which the independent variables explained the outcome variable. Variables with a p-value less than 0.05 in multivariable ordinal logistic regression were reported as having a statistically significant association with the outcome. Finally, the result of the study was presented in tables, figures and texts based on the data obtained.
Ethics Approval and Consent to Participate
Ethical approval was obtained from the Internal Review Board (IRB) of Hawassa University College of Medicine and Health Science (IRB/189/14). The department of midwifery was written a letter of cooperation to the Sidama region health bureau, and the health bureau again wrote a letter to Sidama region Public hospitals’ chief clinical service officers. All the information obtained from study participants was confidential and used only for the intended purpose. After informing the purpose of the study, informed written consent was obtained from mothers. Any refusal of the women’s parents/family to participate in the study their right was respected. This study conforms the principles outlined in the Declaration of Helsinki.
Results
Socio-Demographic Characteristics of Respondents
Of the total 457 mothers who had given birth by a caesarean delivery, 435 mothers were interviewed, resulting in a response rate of 95.2%. Of the respondents, 305(66.7%) mothers were 20 to 30 years old, with a mean age of 25.03(SD=4.9) years. Most of the mothers were married; 422(97.0%) and 244(56.1%) were rural residents. Of mothers, 187(43.0%) were Protestant, and 43(9.9%) were Catholic. Regarding the educational status of mothers, only 94(21.6%) of mothers were unable to read and write, while 165(37.9%) of mothers had a secondary school and above. Among respondents, 128(29.4%) mothers were housewives (do not have independent work), and 40(9.2%) were private employees (Table 1).
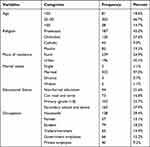 |
Table 1 Socio-Demographic Characteristics of Mothers Who Underwent a Caesarean Delivery in Sidama Region Public Hospitals, Sidama, South Ethiopia 2022 (n=435) |
Source of Information
Concerning the source of information of respondents, 261(60.0%) of mothers participated in the women’s development team, and 224(51.5%), 254(58.4%), 155(35.6%) of mothers had an android Mobile, Radio, and TV respectively. Among respondents, 118(27.1%), 183(42.1), and 68(15.6%) mothers got health information through medical consultation, watching/listening to mass media, and reading books/magazines related to obstetrics. Of the total respondents, 204(46.9%) mothers had a coffee ceremony in their neighbourhood (Table 2).
 |
Table 2 Source Information of Mothers Who Underwent a Caesarean Delivery in Sidama Region Public Hospitals, Sidama, South Ethiopia 2022 (n=435) |
Obstetric Characteristics
Among respondents of the study, 280(64.4%) of the mothers were multipara, and 378(86.9%) of them had ANC follow-up, out of which 158(36.30%) of them had four and above ANC follow-up. Of 378 ANC followers, 157(36.1%) had information about shared decision-making during labour for a mode of delivery. Of the respondents, 96(22.1%) women had a previous caesarean delivery history, and 357(82.1%) of current caesarean delivery were the unscheduled type (Table 3).
 |
Table 3 Obstetrics Characteristics of Mothers Who Underwent a Caesarean Delivery in Sidama Region Public Hospitals, Sidama, South Ethiopia 2022 (n=435) |
Service-Related Factors
According to this study finding, regarding health services respondents got, 184(42.3%) women’s signed the consent after explaining in easy language/mother language, and 139(32.0%) women’s had adequate information about a caesarean delivery. Of 435 respondents, 240(55.2%) women signed their consent immediately before surgery. Among respondents, 184(42.3%) mothers were requested consent from midwives/nurses, and 207(47.6%) women had adequate time to decide to have a caesarean delivery (Table 4).
 |
Table 4 Service-Related Factors of Consent Disclosure of Mothers Who Underwent a Caesarean Delivery in Sidama Region Public Hospitals, Sidama, South Ethiopia 2022 (n=435) |
Patient Healthcare Provider’s Relationship Factors
Of 435 respondents, 181(41.6%) mothers had a good relationship with care providers, and 254(58.4%) mothers had a poor relationship with healthcare providers (Figure 1).
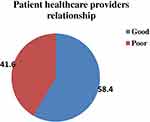 |
Figure 1 Health care providers’ relationship with mothers who underwent a caesarean delivery in Sidama region Public hospitals, Sidama, South Ethiopia 2022 (n=435). |
Shared Decision-Making
Responses of women on the nine questions on shared decision-making. Among 435 mothers, 195(44.8%) and 207(47.6%) agreed that “healthcare providers explain the benefits and risks of a CS” and “reach an agreement on how to precede the procedure”, respectively. However, 217(49.9%) and 208(47.8%) of mothers disagree with “care providers tell about CS/indication” and “explain about different modes of birth for treating obstetrics condition”. Among respondents, 83(19.1%) mothers had neither agreed nor disagreed with healthcare providers asking their thought about a caesarean delivery (Table 5).
 |
Table 5 Shared Decision-Making Among Mothers Who Underwent a Caesarean Delivery in Sidama Region Public Hospitals, Sidama, South Ethiopia 2022 (n=435) |
Shared Decision-Making
Of 435 respondents (women) 165(37.9%) had been adequately involved (agreed) in decision-making during a caesarean delivery, 85(19.5%) intermediate (neutral) and 185(42.5%) women were not adequately involved (disagreed) in decision-making during the procedure (Figure 2).
 |
Figure 2 Involvement in decision-making among mothers who underwent a caesarean delivery in Sidama region Public hospitals, Sidama, South Ethiopia 2022 (n=435). |
Factors Associated with Women’s Involvement in Decision-Making During a Caesarean Delivery
In the bivariable ordinal logistic analysis, the variables p-value ≤ 0.25 became a candidate of multivariable ordinal logistic regression, those are: age, educational status, watching/listening to mass media, ANC follow-up, the current type of caesarean delivery, consenting in easily understandable language, women who felt that they had adequate information about a caesarean delivery, women who felt that they had adequate time for decision-making, and had good mother-health care providers relationship.
In multivariable ordinal logistic regression analysis, six variables namely educational status (being primary school), scheduled caesarean delivery, women who felt that they had adequate information about a caesarean delivery, women who felt that they had adequate time for decision-making, consented to easily understandable language, and good mother-healthcare provider relationship are significantly associated with women’s involvement in decision-making to have a caesarean delivery (Table 6).
Discussion
The study aims to assess women’s involvement in decision-making and associated factors among women who underwent a caesarean delivery in Sidama region Public hospitals.
In this study, women’s agreed decision-making involvement in having a caesarean delivery is 37.9% (95% CI: 33.3–42.5%).
This finding is inconsistent with studies conducted in Pakistan (92.5%) and Nigeria (88.4%).4,28 This discrepancy could be related to the sample size, study settings, demographic characteristics, and sampling technique. Also, private tertiary care centres and women’s had better educational and economic statuses were included in Pakistan. However, it is higher compared with a study conducted in Saudi Arabia (23%) and Jimma (25.3%).5,19 This disparity might be due to sampling size, study settings, and demographic characteristics of participants; in addition, a non-probability type of consecutive sampling was used in Saudi Arabia, and in Jimma, gynecological cases were included.
This finding indicates that maternal educational status is a significant indicator of women’s involvement in decision-making to have a caesarean delivery. Women who had primary school are 47% times lower odds of being involved in decision–making than those who had secondary and above educational status (AOR: 0.53; 95% CI: 0.3,0.97). This result is different from research done in Pakistan.28 This might be due to sampling technique, study area, and population; they used a non-probability convenience sampling technique and a tertiary private care centre.
The finding shows that the current caesarean delivery being scheduled is significantly associated with women’s involvement in decision-making than in an unscheduled. Women had scheduled caesarean delivery are 7.6 times higher odds of being involved in decision-making than an unscheduled caesarean delivery (AOR: 7.5; 95% CI: 3.3, 17.8). This result is supported by a study conducted in Pakistan.29 The reason might be that during scheduled cases, a mother feels free and has enough time to think and communicate with health care providers.
The study revealed that the women who felt they had adequate information about a caesarean delivery are 5.7 times more likely to be involved in decision-making than those without information (AOR: 5.7; 95% CI: 3.3, 10.0). This result is in line with a different study conducted in Sweden, Nigeria, and Uganda.4,8,30 This might be well-informed women easily develop self-confidence to decide on intervention.
In this study, there is a significant association between the women who felt that they had adequate time to decide to have a caesarean delivery and women’s involvement in the decision-making (AOR: 4.6; 95% CI: 2.8, 7.6). This finding is supported by studies conducted in Sweden and Jimma.5,30 The reason might be women who have enough time to search for information about the operation from various sources easily, would be able to contact and communicate with health professionals effectively and grow confident.
In this study finding, consenting/explaining the procedure in the mother tongue or the easily understandable language is significantly associated with women’s involvement in decision-making during the process (AOR: 1.9; 95% CI: 1.2, 3.1). This study is in line with the finding in Dessie.31 Reducing the language barrier might be that providing health information in understandable language might increase interaction and communication between health care providers. In addition, women can understand the situation.
Mothers-healthcare providers’ good relationship is a significant predictor of women’s involvement in decision-making during a caesarean delivery; women who have a good relationship with healthcare providers are 5.2 times more odds of getting involved than women who have poor relationships (AOR: 5.2; 95% CI: 3.2, 8.6). This result is in line with studies conducted in Bangladesh, Saudi Arabia, Nigeria, and Jimma.1,5,15,29 This reason could be positive healthcare providers’ interaction where the mothers felt comfortable sharing their worries, emotions, and adequate information delivered from care providers to the women. Additionally, they create amiable and trustworthy connections.
Limitation of the Study
Recall bias; mothers might have forgotten information that was told during (before) the surgery since they were interviewed after the procedure.
Conclusion
In this study, women’s agreed decision-making involvement to having a caesarean delivery is low compared with other studies. The factors those women’s had scheduled caesarean delivery, women being primary school, women who felt they had adequate information about a caesarean delivery, women who felt that they had adequate time for decision-making, consenting in easily understandable language, and good women’s-healthcare providers’ relationships are significantly associated with women’s involvement in decision-making to have a caesarean delivery. Having an unscheduled caesarean delivery and primary school educational status are negatively affect women’s involvement in decision-making. A good relationship between healthcare providers and women is vital for shared decision-making.
Recommendation
Hospitals should translate the consent format and the consent language into different (various) languages and assign the healthcare providers who could talk that language. Healthcare providers should develop intimate (close) relationships with mothers and her families, provide enough information about the procedure, give adequate time for the mothers and encourage the involvement of the women in decision-making before the procedure and take the consent after explaining all the information on consent format.
Abbreviations
ACOG, American College of Obstetricians and Gynecologists; ANC, Antenatal Care; CD, Caesarean delivery; DM, decision-making; HCP, Health care providers; IESOs, Integrated Emergency Surgery Officers; OB/Gym, Obstetrics and gynecology; ODK, Open-Data-Kit; PDRQ, Patient-doctor relationship questions; SDM, Shared decision-making; SDM-Q-9, Shared decision-making questions nine; SPSS, Statistical Package for Social Sciences; WHO, World Health Organization.
Acknowledgment
The author would like to thank Sidama region Public health institute and Public hospitals. Authors would like to express appreciation to data collectors, supervisors, and the mothers who participated in this study. Also thankful to Hawassa and Jimma university for financial support.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Hawassa University College of Medicine and Health Sciences.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Azikiwe N, Teaching U, Hospital G. Original article women’ s involvement in the decision to be delivered by caesarean section in Sub Saharan Africa. Table 1 distribution of respondents among the hospitals hospitals St Charles Borromeo specialist hospital, Onitsha general hospital. Niger J Med. 2012;21(2):150–156.
2. Asfaw T, Tesema A. Determinant factors, trend and outcomes of cesarean delivery in Debre Berhan referral hospital, North Shewa Zone, Ethiopia. Pediatr Rep. 2020;12(2):8430. doi:10.4081/pr.2020.8430
3. Betran AP, Torloni MR, Zhang JJ, Gülmezoglu AM. WHO statement on caesarean section rates. BJOG. 2016;123(5):667–670. doi:10.1111/1471-0528.13526
4. Ohaeri BM, Aideloje F, Ingwu JA. Women’s involvement in decision-making before caesarean section and its influence on their satisfaction with procedure in a tertiary health institution Edo State - Nigeria. Int J Nurs. 2019;6(1):197–205.
5. Biyazin T. Mode of decision making’ s approach in surgical procedures. J Eval Clin Pract. 2021;2021:1–7.
6. Norman I. Blind trust in the care-giver: is paternalism essential to the health-seeking behavior of patients in Sub-Saharan Africa? Adv Appl Sociol. 2015;5(2):94–104. doi:10.4236/aasoci.2015.52008
7. Truglio-londrigan M, Slyer JT, Singleton JK, Worral P. A qualitative systematic review of internal and external influences on shared decision-making in all health care settings. JBI Lib Syst Rev. 2012;10(58):4633–4646. doi:10.11124/jbisrir-2012-432
8. Nuwagaba J, Olum R, Bananyiza A, et al. Patients’ Involvement in Decision-Making During Healthcare in a Developing Country: A Cross- Sectional Study. Dovepress; 2021.
9. Barnett G, Swart M. Shared decision making for high-risk surgery. BJA Educ. 2021;21(8):667. doi:10.1111/1471-0528.13526
10. Ethiopia M. Obstetrics management protocol for hospitals. 2021.
11. Sketcher-Baker K. Guide to Informed Decision-Making in Health Care.
12. Chen SW, Hutchinson AM, Nagle C, Bucknall TK. Women’s decision-making processes and the influences on their mode of birth following a previous caesarean section in Taiwan: a qualitative study. BMC Pregnancy Childbirth. 2018;18(1):1–13. doi:10.1186/s12884-018-1661-0
13. Making SD. The role of shared decision making in patient-centered care and orthopaedics. Orthop Nurs. 2016;35(3):1.
14. Slim K, Bazin JE. From informed consent to shared decision-making in surgery. J Visc Surg. 2019;156(3):181–184. doi:10.1016/j.jviscsurg.2019.04.014
15. Doraiswamy S, Billah SM, Karim F, Siraj MS, Buckingham A, Kingdon C. Physician–patient communication in decision-making about Caesarean sections in eight district hospitals in Bangladesh: a mixed-method study. Reprod Health. 2021;18(1):1–14. doi:10.1186/s12978-021-01098-8
16. Declercq ER, Cheng ER, Sakala C. Does maternity care decision-making conform to shared decision- making standards for repeat cesarean and labor induction after suspected macrosomia? Birth. 2018;45(3):236–244. doi:10.1111/birt.12365
17. Page AE. Safety in surgery: the role of shared decision-making. Patient Saf Surg. 2015;9(1):1–4. doi:10.1186/s13037-015-0068-3
18. Krist AH, Tong ST, Aycock RA, Longo DR. Engaging patients in decision-making and behavior change to promote prevention. HHS Public Access. 2020;2020:284–302.
19. El Amir H, El Zewawi N, Al Jaroudi D. Involvement of women with the decision of caesarean section and their degree of satisfaction for post-operative care and pain management. J Womens Health Care. 2017;6(5):2167–0420.
20. Bam V, Lomotey AY, Kusi-Amponsah Diji A, Budu HI, Bamfo-Ennin D, Mireku G. Factors influencing decision-making to accept elective caesarean section: a descriptive cross-sectional study. Heliyon. 2021;7(8):e07755. doi:10.1016/j.heliyon.2021.e07755
21. Ryan GL, Brandi K. Informed consent and shared decision making in obstetrics and gynecology. Obstet Gynecol. 2021;137(2):392–393. doi:10.1097/AOG.0000000000004248
22. Qidwai K. Senior specialist family physician & supervisor in the residency program of the Arab board for health specializations, manager of Continuing Professional Development (CPD), Continuing medical education (CME) & Member of the executive board of Iraqi Fami. Eur J Pers Cent Healthc. 2012;1(2):394–404. doi:10.5750/ejpch.v1i2.679
23. Alsulamy N, Lee A, Thokala P, Alessa T. Views of stakeholders on factors influencing shared decision-making in the eastern Mediterranean region: a systematic review. East Mediterr Health J. 2021;27(3):300–311. doi:10.26719/emhj.20.139
24. Rencz F, Tamási B, Brodszky V, Gulácsi L, Wesz M, Márta P. Validity and reliability of the 9-item Shared Decision Making Questionnaire (SDM-Q-9) in a national survey in Hungary. Eur J Health Econ. 2019;20(S1):43–55. doi:10.1007/s10198-019-01061-2
25. Rodenburg-vandenbussche S, Pieterse AH, Kroonenberg PM. Dutch translation and psychometric testing of the 9-item Shared Decision Making Questionnaire (SDM-Q-9) and Shared Decision Making Questionnaire-Physician Version (SDM-Q-Doc) in primary and secondary care. PLoS One. 2015;10(7):e0132158. doi:10.1371/journal.pone.0132158
26. Grüne B, Köther AK, Büdenbender B, Michel MS, Kriegmair MC, Alpers GW. Patients’ perspective on shared decision-making in urology: a prospective study at a university hospital. World J Urol. 2021;39(12):4491–4498. doi:10.1007/s00345-021-03794-3
27. Zenger M, Schaefert R, van der Feltz-Cornelis C, Brähler E, Häuser W, Assassi S. Validation of the Patient-Doctor-Relationship Questionnaire (PDRQ-9) in a representative cross- sectional German population survey. PLoS One. 2014;9(3):1–8. doi:10.1371/journal.pone.0091964
28. Anjum S, Husain A, Naseem A. Women involvement in decision making to have cesarean section and their postpartum satisfaction. J Dow Univ Health Sci. 2018;12(2):48–52. doi:10.36570/jduhs.2018.2.584
29. Shoaib T, Memon S, Javed I, Pario S, Bhutta SZ. Decision-making and involvement of women with previous C-section in choosing their mode of delivery. J Pak Med Assoc. 2012;62(10):1038–1041.
30. Rn AA, Registered M, Rn MV, Registered M. Patient involvement in surgical care – healthcare personnel views and behaviour regarding patient involvement. Scand J Caring Sci. 2021;35(1):96–103. doi:10.1111/scs.12823
31. Gebrehiwot H, Estifanos N, Zenebe Y, Anbesaw T. Patient perception of informed consent and its associated factors among surgical patients attending public hospitals in Dessie City administration, Northeast Ethiopia. Crit Care Res Pract. 2022;2022. doi:10.1155/2022/6269921
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

